Fill Out Your 8584 Form
The 8584 form, developed by the Texas Department of Aging and Disability Services, serves as a vital tool for healthcare professionals conducting comprehensive nursing assessments. Designed to be filled out by registered nurses, it gathers essential information about an individual’s health status and medical history. This form encompasses various components, beginning with a review of the individual's healthcare team, including details about their primary care physician and specialists, as well as any medications they are currently taking, whether prescription or over-the-counter. It also prompts a thorough analysis of the individual’s health history, including any major medical or surgical occurrences and their current health status. Important assessments, such as vital signs and a fall risk evaluation, are included, allowing for a well-rounded picture of the patient's condition. The review of systems section addresses neurological, cardiovascular, and sensory health, ensuring that practitioners have a comprehensive view of the individual's overall well-being. Through structured prompts and sections, the 8584 form aims to capture real-time health information while considering the expressed needs of the individual, their legally authorized representative, or their responsible adult.
8584 Example
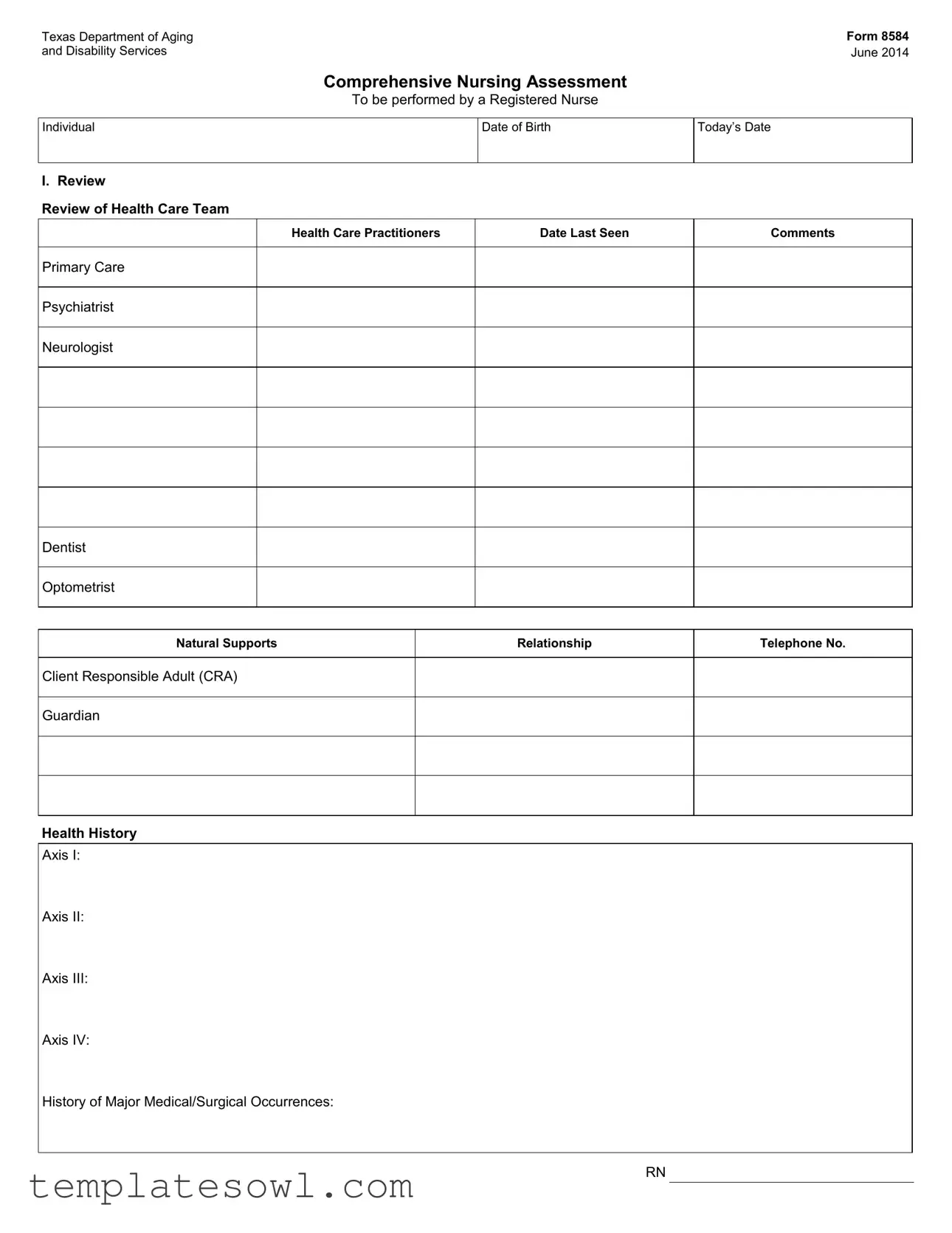
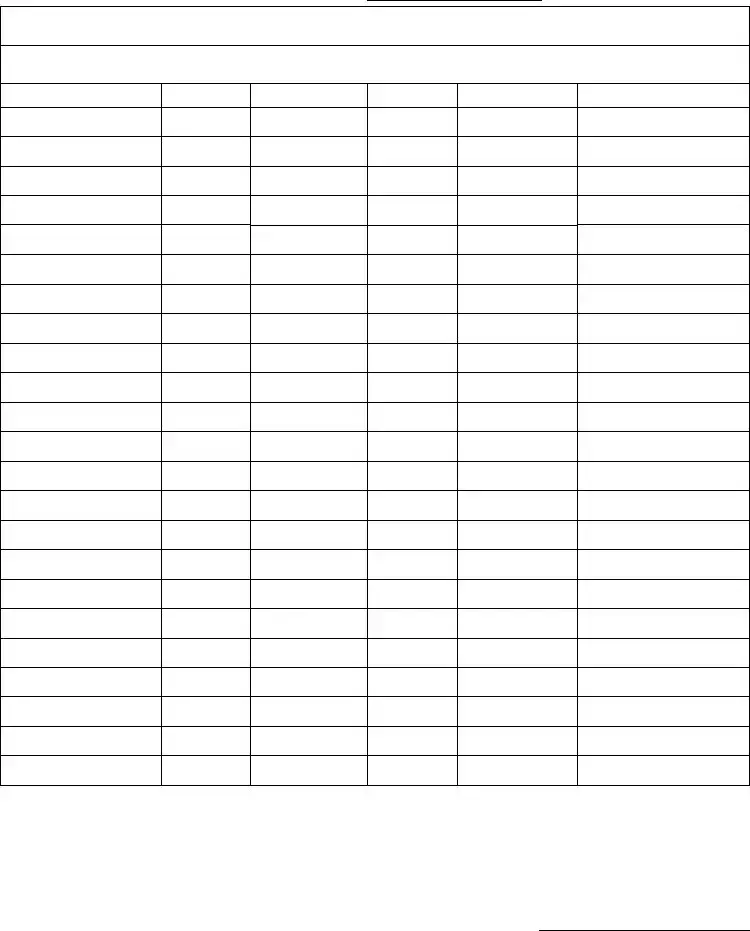
Texas Department of Aging |
Form 8584 |
and Disability Services |
June 2014 |
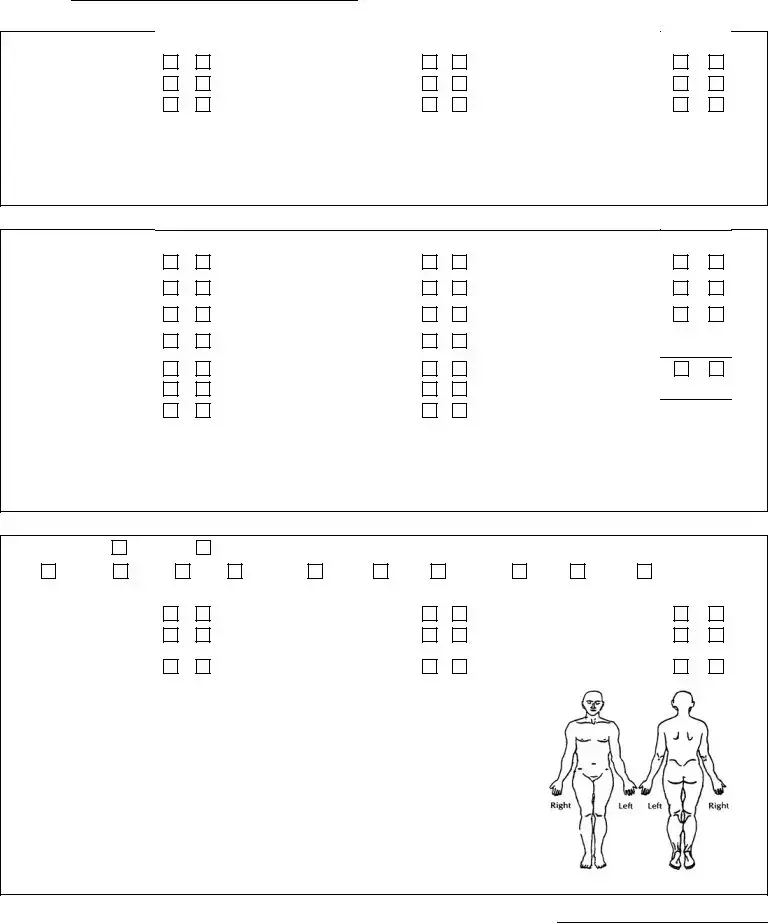
Comprehensive Nursing Assessment
To be performed by a Registered Nurse
Individual
Date of Birth
Today’s Date
I. Review
Review of Health Care Team
Health Care Practitioners |
Date Last Seen |
Comments |
Primary Care
Psychiatrist
Neurologist
Dentist
Optometrist
Natural Supports |
Relationship |
Telephone No. |
Client Responsible Adult (CRA)
Guardian
Health History
Axis I:
Axis II:
Axis III:
Axis IV:
History of Major Medical/Surgical Occurrences:
RN
Form 8584
Page 2 /
Individual |
|
Date |
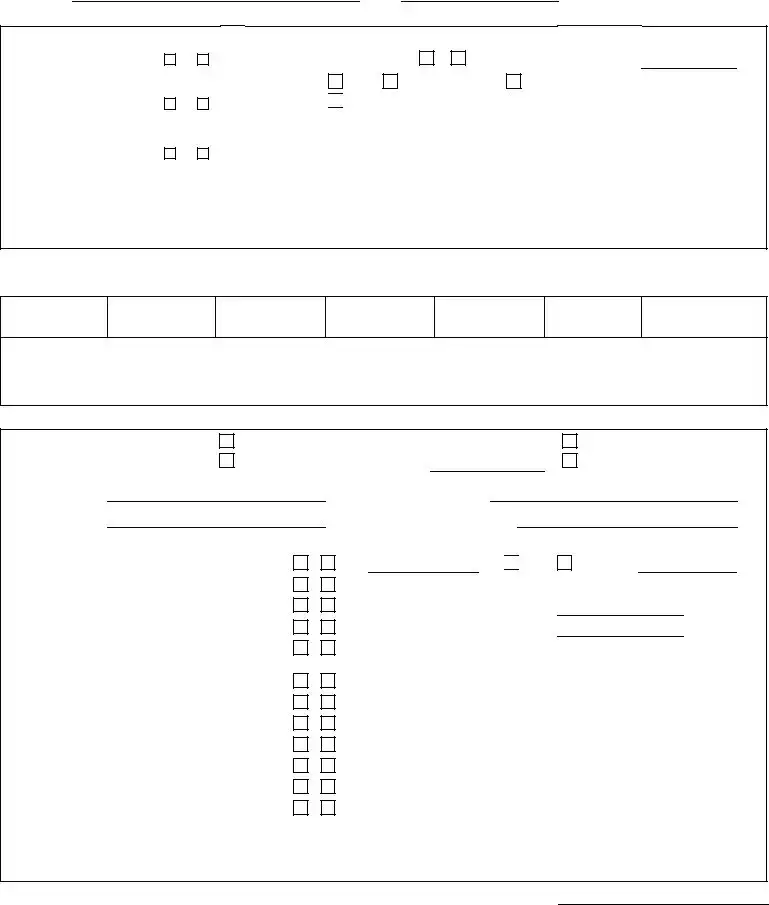
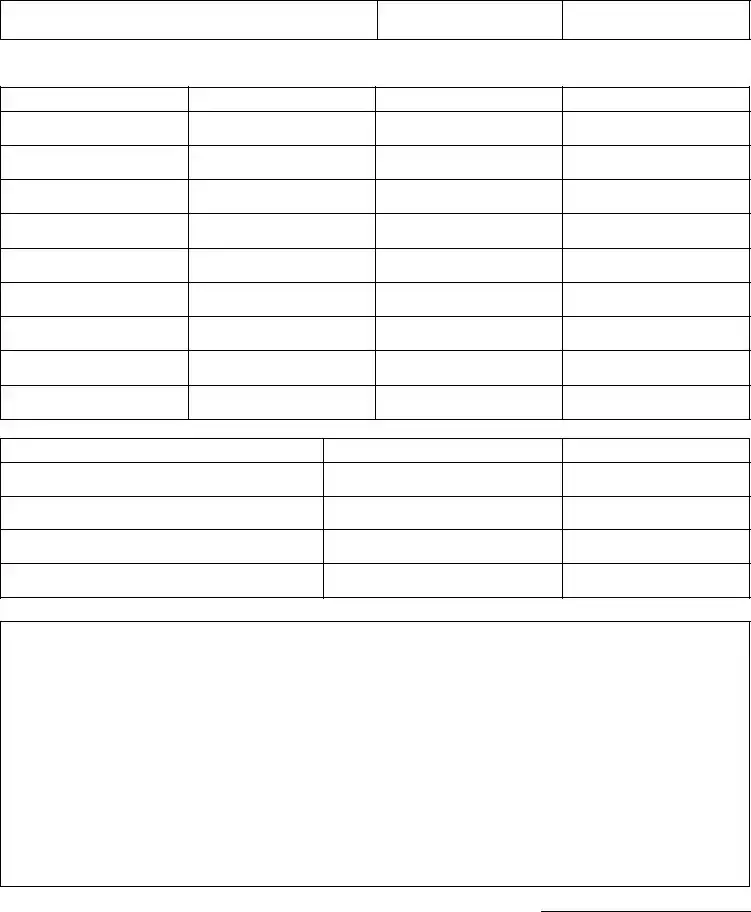
Review of Current Medications
Include OTCs, vitamins and herbs
Allergies:
Medication
Dose
Freq.
Route
Purpose/Rationale
Side Effects/Labs
RN
Form 8584
Page 3 /
Individual |
|
Date |
|
|
|
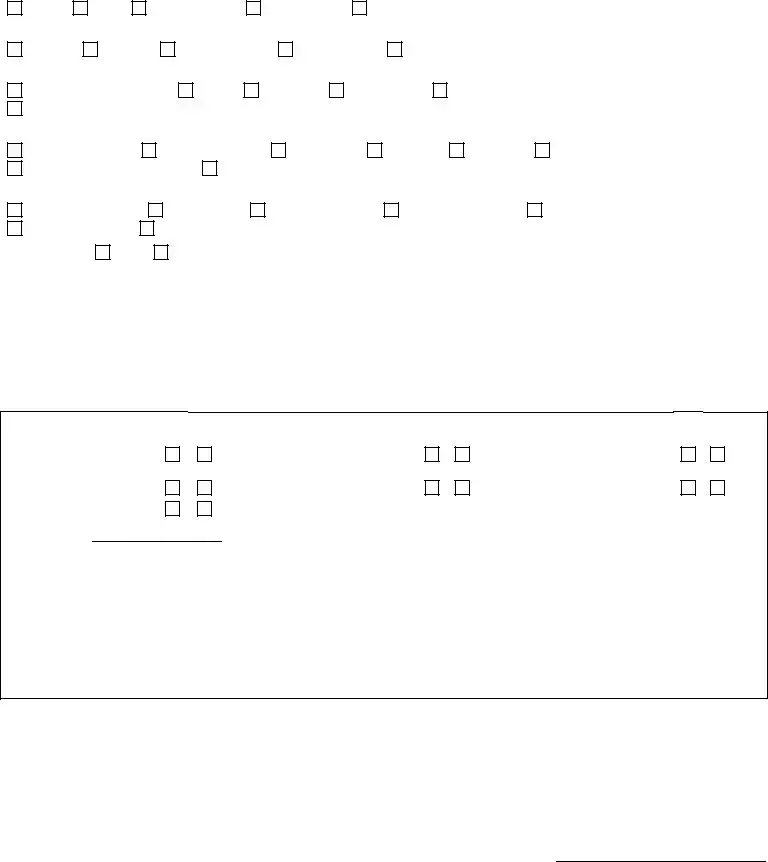
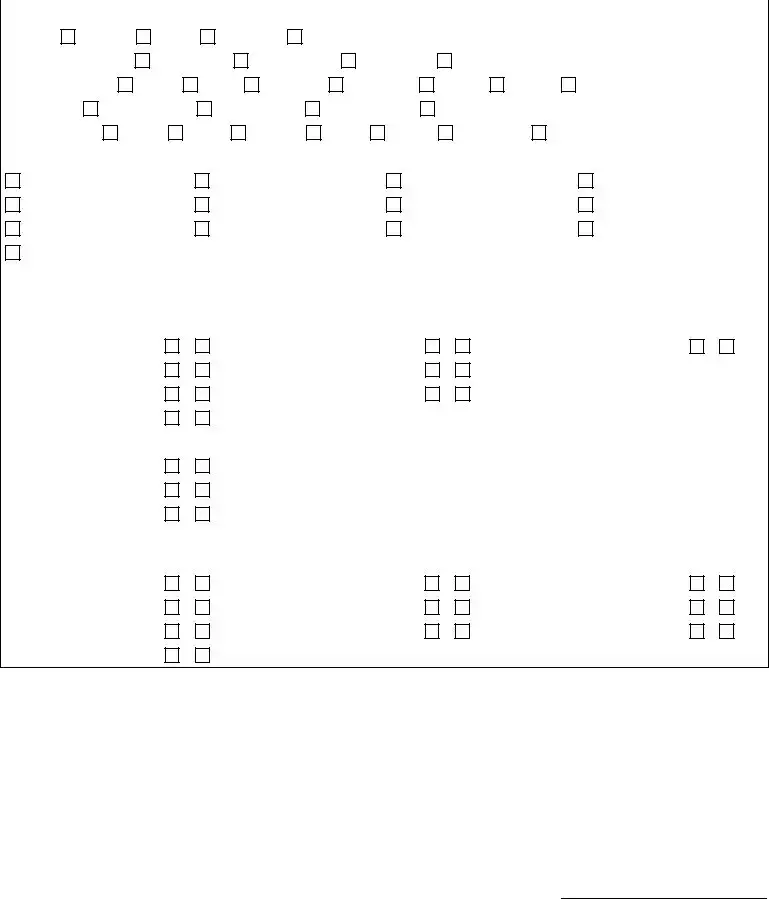
II. Current Status
Current medical and psychiatric history
Briefly describe recent changes in health or behavioral status, hospitalizations, falls, seizure activity, restraints, etc., within the past year.
What is of primary concern/greatest expressed needs of the individual, legally authorized representative (LAR) or client’s responsible adult (CRA) from their own perspective?
Vital Signs
Blood pressure |
Pulse |
Respirations |
|
Rate |
Rhythm |
Rate |
Rhythm |
||
|
|
|
|
|
|
|
Temperature |
Pain level |
|
Blood sugar |
Weight |
|
Height |
|
|
|
|
|
|
|
Comments
RN
Form 8584
Page 4 /
Individual |
|
Date |
|
|
|
Labs
Briefly review ordered labs, dates and abnormal values within the past year.
Fall Risk Assessment
Has a fall risk assessment been completed?
No
Yes (attached). Fall risk due to:
Neurological
Musculoskeletal
Unknown
Comments
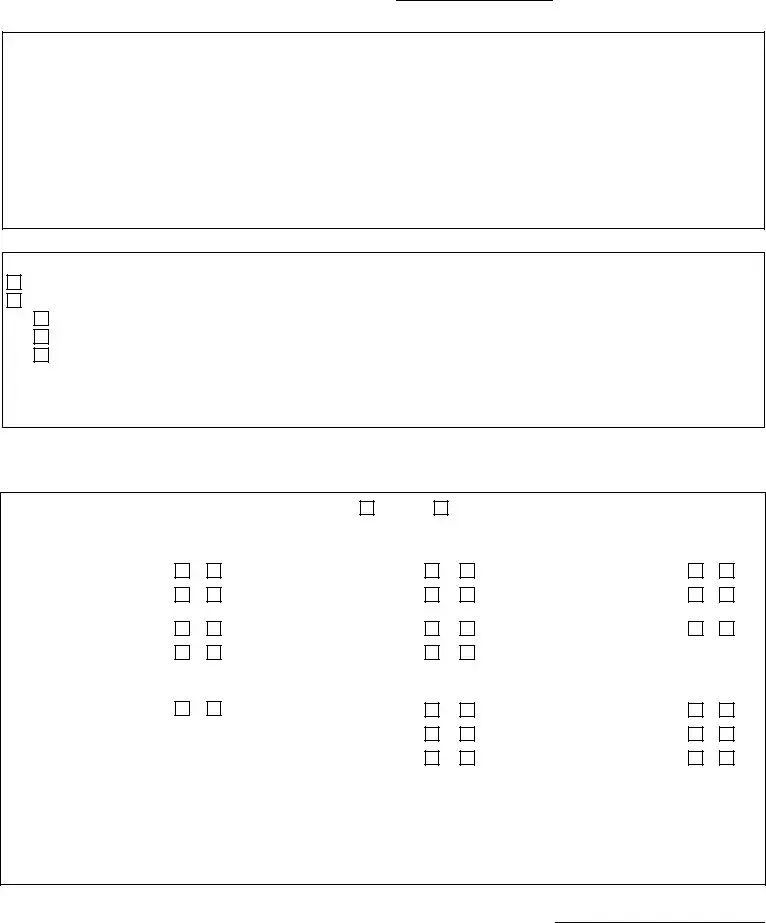
III. Review of Systems
Neurological
Abnormal Involuntary Movement Scale (AIMS) Assessment: |
Attached |
|
Deferred |
|
|
|||
|
Y |
N |
|
Y |
N |
Y |
N |
|
|
|
|
Pupils equal and reactive to |
|
|
|
|
|
Headaches |
light and accommodation |
|
|
Tremors |
|
|||
Dizziness |
Tremors |
|
|
Heat/cold reflex |
|
|||
Impaired balance/ |
|
Numbness/tingling/ |
|
|
|
|
|
|
coordination |
|
Paresthesia |
|
|
Extrapyramidal symptoms |
|
||
Medication side effects |
|
Paralysis |
|
|
|
|
||
|
Y |
N |
|
Y |
N |
Y |
N |
|
Seizures |
Petit Mal |
|
|
Clonic (repetitive jerking) |
|
|||
|
|
|
|
|
|
|||
Frequency |
|
|
Absence |
|
|
Tonic (muscle rigidity) |
|
|
Duration |
|
|
Myoclonic (sporadic jerking) ... |
|
|
Atonic (loss of muscle tone).... |
|
|
Comments |
|
|
|
|
|
|
|
|
RN
Form 8584
Page 5 /
Individual |
|
|
|
|
|
|
Date |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
||
Eye, Ear, Nose and Throat |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Eyes/Vision |
|
|
|
|
|
|
|
|
|
|
|
|
Clear |
Red |
Right impaired |
Left impaired |
Adaptive aid |
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Ears/Hearing |
|
|
|
|
|
|
|
|
|
|
|
|
Normal |
Ringing |
Right impaired |
Left impaired |
|
Adaptive aid |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Nose/Smell |
|
|
|
|
|
|
|
|
|
|
|
|
Within normal limits Smell: |
intact |
not intact |
Nose bleeds |
Frequent sinus congestion |
||||||||
Frequent sinus infection |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Oral |
|
|
|
|
|
|
|
|
|
|
|
|
Within normal limits |
Difficulty chewing |
Mouth pain |
Halitosis |
Dentures |
Edentulous |
|||||||
Involuntary tongue movement |
Dry mouth from medications |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Throat |
|
|
|
|
|
|
|
|
|
|
|
|
Within normal limits |
Sore throats |
Difficulty speaking |
|
Difficulty swallowing |
Tonsil enlargement |
|||||||
History of choking |
Thyroid enlargement |
|
|
|
|
|
|
|
||||
Swallow Study: |
Yes |
No |
Date: |
|
Results: |
|
|
|
||||
Comments |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
Cardiovascular
Y N
Edema.................................
Chest pain ...........................
High/Low blood pressure.....
Normal range
Comments
Y N
Cool/Numb extremities...........
Activities of daily living (ADL)
limitations...............................
Y N
Capillary refill less than or
equal to two seconds...............
Compression stockings ...........
RN
Form 8584
Page 6 /
Individual |
|
|
|
|
|
|
Date |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
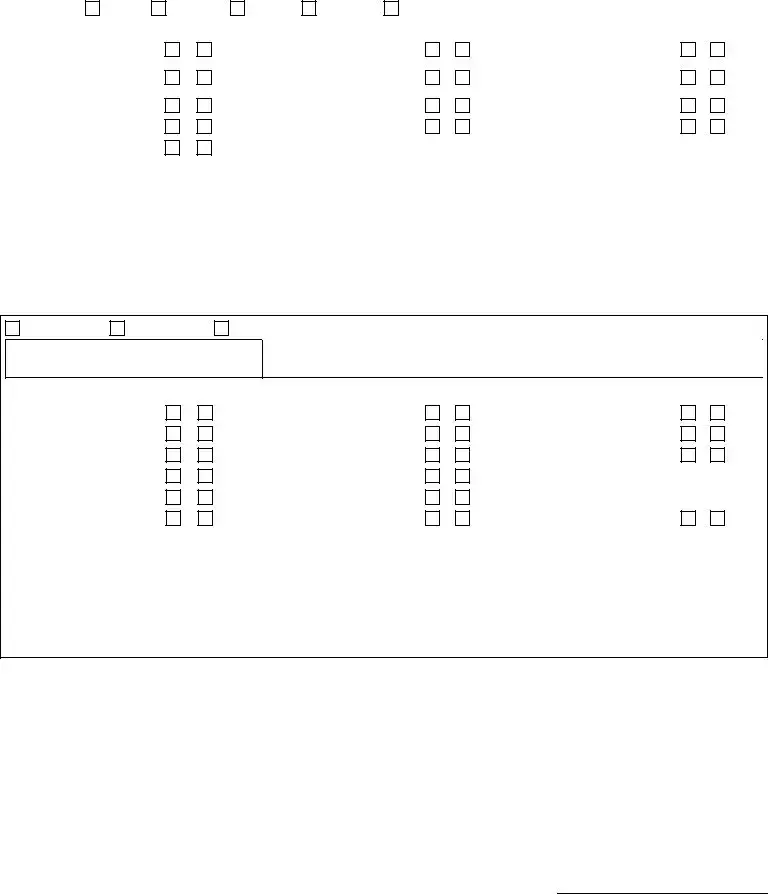
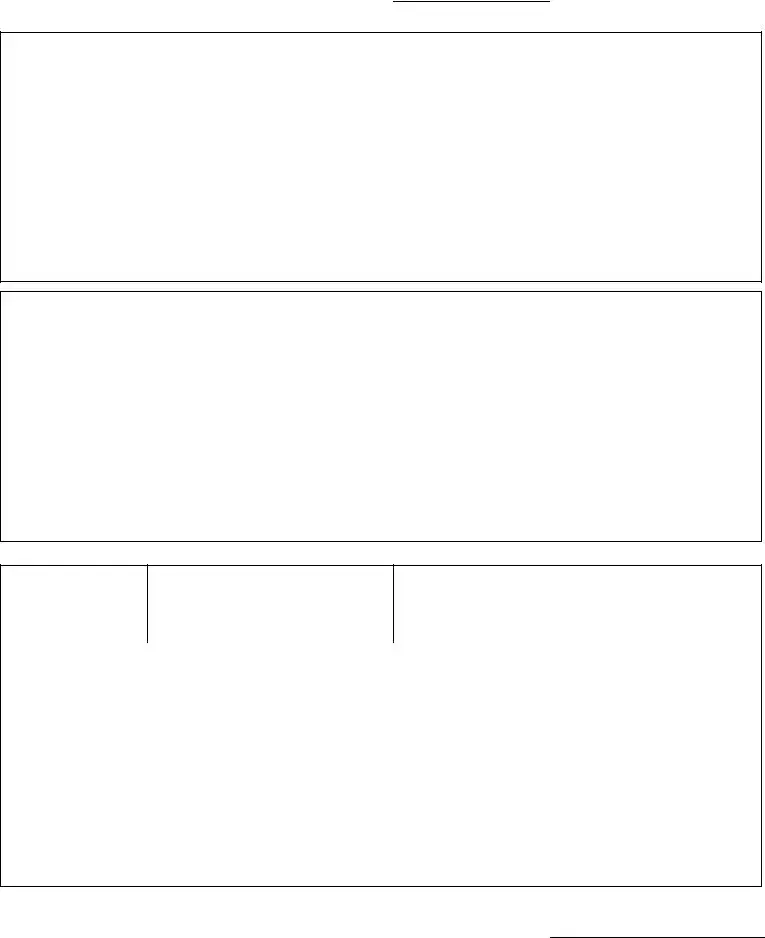
Respiratory |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Breathing: |
Slow |
Normal |
Rapid |
Shallow |
|
Painful |
|
|
|
|
|||
|
|
|
Y |
N |
|
|
|
|
Y |
N |
|
Y |
N |
Short of breath |
.................... |
|
|
Feeding tube |
........................... |
|
|
|
Tracheostomy |
|
|||
|
|
|
|
|
|
|
|
|
|
|
Continuous positive airway |
|
|
Wheezing |
|
|
Positioning orders |
|
|
pressure (CPAP) |
|
||||||
Fatigue |
|
|
Aspiration history |
|
|
Inhalation agent |
|
||||||
Cough |
|
|
Pneumonia history |
|
|
Oxygen @ |
|
||||||
Productive |
|
|
|
|
|
|
|
|
|
|
|
||
Comments |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Gastrointestinal
Gastrostomy
Bowel sounds
Jejunostomy
No tube
Last bowel movement |
Bowel habits (frequency and description) |
|
|
Y NY NY N
Continent.............................
Frequent nausea .................
Frequent vomiting ...............
Indigestion...........................
Heartburn ............................
Appetite loss........................
Comments
Reflux......................................
Straining pain..........................
Diarrhea..................................
Odd stools...............................
Hemorrhoids ...........................
Independent toileting...............
History of risk constipation .......
History of risk impaction ...........
Bowel program .........................
Medications influencing bowels (laxatives,
RN
Form 8584
Page 7 /
Individual
Musculoskeletal
Pain.....................................
Weakness ...........................
Stiffness ..............................
Comments
|
|
Date |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Y |
N |
|
Y |
N |
|
|
Y |
N |
|
Prosthesis |
|
|
Impaired range of motion |
||||
|
Deformity |
|
|
Impaired gait |
||||
|
Contractures |
|
|
Adaptive equipment |
||||
Genitourinary
Y N
Incontinent..........................
Stress.......................
Urge .........................
Bladder program ................
Frequent urination ..............
Cloudy/dark urine ...............
Bloody urine .......................
Comments
Y N
Flank pain ...............................
History of urinary tract
infections ................................
Noctouria ................................
Discharge ...............................
Itching .....................................
Hemodialysis ..........................
Peritoneal dialysis...................
Y N
Sexually active.....................
Prostate issues ....................
Menstrual cycle regular........
Date of last menstrual period:
Menopausal:
If yes, date of onset:
Integumentary
Skin Assessment: |
Attached |
|
Deferred |
|
|
|
|
|
|
|
|
Skin: |
Normal |
Moist |
Dry |
Cyanotic |
Warm |
Pale |
Jaundice |
Cold |
Dusky |
Flushed |
|
|
|
Y |
N |
|
|
Y |
N |
|
|
Y |
N |
Open wound |
|
Rash |
|
|
Blemished |
............................ |
|
||||
Bruising |
.............................. |
|
Diaphoretic |
|
|
Poor skin turgor |
|
||||
Breakdown related to |
|
|
|
|
|
|
|
|
|
|
|
adaptive aids/prosthesis |
|
Risk for breakdown |
|
History of breakdown |
|
||||||
Comments
RN
Form 8584
Page 8 /
Individual
Endocrine
Y N
Thyroid dysfunction ............
Atypical antiphychotics or other medications affecting blood sugar.........................
hyperglycemic episodes .....
Comments
Date
|
|
Y |
N |
|
Diabetes |
|
|
If yes, type |
|
Management: |
Diet |
Oral medications |
Insulin |
|

 Other injectable medication to manage diabetes Desired blood sugar range:
Other injectable medication to manage diabetes Desired blood sugar range:
IV. Additional Health Status Information Immunizations: Date last received
DPT
TOPV
HIB
MMR
TD
TDS
Flu Shot
Comments
Nutritional Assessment
How receive nutrition:
Therapeutic diet
Food texture
Orally
Via gastrotomy tube if residual
Liquid consistency
Reason/date/ordered by:
Via jejunostomy tube Other
YN
Recent weight change ...............................................
Recent changes in appetite/medication.....................
Satisfied with current weight......................................
Food use as a coping mechanism.............................
Assistive devices with eating .....................................
Use of medications that can cause difficulty
swallowing (e.g., Abilify, other psychoactives)...........
Knowledge of 4 basic food groups.............................
Access to healthy/appropriate diet.............................
Dietary deficiencies ...................................................
Adequate fluid intake.................................................
Nutritional supplements .............................................
Interactions with medications and food......................
Comments
lbs. 
 gain
gain
Desired weight range
Number of meals/snacks per day
loss over
RN
Form 8584
Page 9 /
Individual |
|
Date |
|
|
|
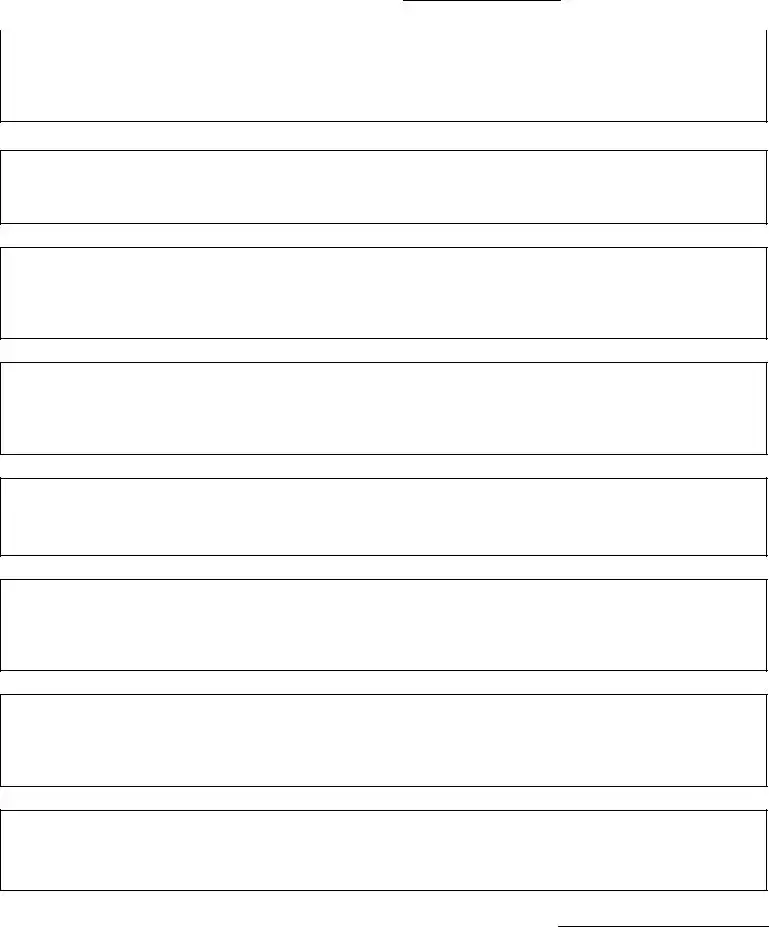
Sleep Patterns
Average number of hours per night; difficulty falling asleep; number of times awake at night; number of naps during a day
Activity Level/Exercise
Substance Use/Abuse
Caffeine, tobacco, alcohol, recreational drugs, history of
Home Life
Satisfaction/Desires
Work/School/Day Activity
Satisfaction/Desires
Social Life
Satisfaction/Desires
Spiritual Life
Satisfaction/Desires
Coping Skills
RN
Form 8584
Page 10 /
Individual |
|
|
|
|
|
|
|
Date |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mental Status |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Appearance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Posture: |
Normal |
Rigid |
Slouched |
Other: |
|
|
|
|
|
|
||||
Grooming and Dress: |
Appropriate |
Inappropriate |
|
Disheveled |
Neat |
|
|
|
||||||
Facial Expression: |
Calm |
Alert |
Stressed |
Perplexed |
Tense |
Dazed |
|
Other: |
||||||
Eye contact: |
|
Eyes not open |
Good contact |
|
Avoids contact |
Stares |
|
|
|
|||||
Speech Quality: |
Clear |
Slow |
Slurred |
|
Loud |
Rapid |
Incoherent |
Mute |
||||||
Mood |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cooperative
Excited
Irritable
Other/Describe
Uncooperative
Agitated
Scared
Depressed
Anxious
Hostile
Euphoric
Suspicious
Angry
Cognition
Y N
Cognitive impairment
Mild.....................................
Moderate ............................
Severe ................................
Profound.............................
Y N
Oriented
Person....................................
Place ......................................
Time .......................................
Y N
Attention span
Easily distracted ......................
Memory
Remote...............................
Recent ................................
Immediate recall .................
Emotions
Y N
Euphoric .............................
Happy .................................
Apathetic ............................
Sadness .............................
Y N
Depressed..............................
Anxious ..................................
Irritable ...................................
Y N
Hostile feelings .......................
Emotional lability ....................
Inappropriate affect.................
RN
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of Form | The 8584 form is a Comprehensive Nursing Assessment used to evaluate an individual's health status. |
| Authority | This form is governed by Texas Administrative Code, Title 40, Part 1, Chapter 19. |
| Completion Requirement | A Registered Nurse must perform the assessment to ensure accuracy and compliance. |
| Key Components | The assessment includes sections on health history, current medications, vital signs, and a review of systems. |
| Update Frequency | The form should be updated annually or whenever there are significant changes in health status. |
Guidelines on Utilizing 8584
Filling out the 8584 form may seem daunting, but with a clear approach, you can complete it efficiently. This form requires detailed information about the individual’s health care needs and history. The information gathered will help create a comprehensive assessment to provide the best care possible.
- Gather Information: Collect all necessary personal and health-related documents. This includes medical history, medications, and any recent health reports.
- Complete Individual Information: At the top of the form, write the individual's name and date of birth. Don't forget to enter today’s date.
- Review Health Care Team: List all health care practitioners involved in the individual’s care. Note the last visit date and any comments. Be thorough.
- Identify Natural Supports: Provide information about any family members or friends who support the individual. Share their relationship to the individual and contact details.
- Record Health History: Fill out the sections related to health history, including axes I through IV. Include major medical or surgical occurrences.
- List Current Medications: Document all current medications, including over-the-counter drugs and supplements. Include doses, frequency, route, purpose, and any side effects.
- Detail Current Status: Write a brief narrative about the individual's current medical and psychiatric status. Address any changes in health, recent issues, or expressed needs.
- Vital Signs: Record the vital signs, including blood pressure, pulse, respiration, temperature, pain level, blood sugar, weight, and height.
- Summarize Lab Results: Create a brief overview of any labs ordered in the past year, noting dates and any abnormal values.
- Complete Fall Risk Assessment: Indicate if a fall risk assessment has been completed, and note contributing factors such as neurological or musculoskeletal issues.
- Review Systems: Go through the system review sections and mark any relevant findings for neurological, cardiovascular, and sensory evaluations.
- Provide Comments: Throughout the form, use the comments sections to add any other relevant details that could be important for care considerations.
Once you've filled out the form, review all information for accuracy and completeness. Ensuring each field is addressed will help in the evaluation process. With everything in order, you can submit the form and move forward with the assessment process.
What You Should Know About This Form
What is Form 8584?
Form 8584 is a Comprehensive Nursing Assessment used by the Texas Department of Aging and Disability Services. It is designed to assess the health and functional status of individuals in need of care. This assessment is performed by a registered nurse and covers a wide range of health-related information.
Who completes Form 8584?
A registered nurse completes Form 8584. This professional is tasked with conducting a thorough review of the individual's health history, current medications, and other relevant factors impacting the person's care and well-being.
What information is required on Form 8584?
Form 8584 requires various types of information, including the individual’s medical history, recent changes in health status, allergies, current medications, and vital signs. It also assesses specific systems, such as neurological, cardiovascular, and sensory functions. Additionally, comments from the individual or their responsible adult may be included to highlight specific concerns.
Is a fall risk assessment included in Form 8584?
Yes, Form 8584 includes a fall risk assessment. The registered nurse will determine whether an assessment has been completed and will note any fall risks identified, such as neurological or musculoskeletal factors. This is crucial for ensuring the safety of the individual.
What happens if a medication is identified with side effects?
If any current medications are noted to have potential side effects, these are documented on Form 8584. It is important for the nurse to communicate these findings to relevant health care providers to address any concerns and adjust medications as necessary.
Can supplementary information be attached to Form 8584?
Yes, supplementary information such as lab results or additional assessments can be attached to Form 8584. This provides a more comprehensive view of the individual’s health status and is encouraged for ensuring thorough evaluations.
How often should Form 8584 be completed?
Form 8584 should be completed as needed, particularly when there are significant changes in the individual’s health condition or upon admission into a care facility. Regular updates may be required to ensure accurate and current health assessments.
What role does the Client Responsible Adult (CRA) play in the assessment?
The Client Responsible Adult (CRA) or legally authorized representative plays a crucial role in the assessment process. They provide valuable insights regarding the individual’s specific needs and concerns, ensuring that their perspective is incorporated into the overall evaluation.
Where can I access Form 8584?
Form 8584 can typically be accessed through the Texas Department of Aging and Disability Services website or obtained from health care providers involved in the care process. Ensure that you are using the most recent version to comply with current regulations and standards.
Common mistakes
Filling out Form 8584 correctly is crucial for a comprehensive nursing assessment. However, many people make common mistakes that can lead to incomplete or inaccurate information. One frequent error is not providing enough detail in the health history section. This includes failing to document important past medical or surgical occurrences. Such omissions can prevent health care providers from gaining a full understanding of a patient’s background and needs.
Another mistake often made is neglecting to list all current medications, including over-the-counter drugs, vitamins, and herbal supplements. Missing this information can lead to dangerous drug interactions or misunderstandings about a patient’s treatment plan. It is essential to review and update medication lists thoroughly before submitting the form.
People also sometimes fail to report changes in the individual’s current medical or psychiatric status. The section addressing recent changes, hospitalizations, or any concerning behaviors should be completed with care. This information is vital for health care professionals to provide appropriate support and adjustments to care based on the individual's most recent conditions.
Completing the vital signs section incorrectly is another common issue. It’s important to ensure accuracy in recording blood pressure, pulse, respirations, and temperature. Any discrepancies can mislead caregivers about the patient’s current condition. Moreover, neglecting to comment on pain levels, blood sugar, weight, and height can leave significant gaps in information.
The fall risk assessment section is often overlooked or filled out inadequately. It is necessary to either attach a completed fall risk assessment or provide thorough details explaining the patient’s risks. This assessment can result in critical interventions that might prevent falls and enhance safety.
Lastly, failing to provide comments or additional notes in various sections can be detrimental. Always include relevant observations, especially in sections reviewing systems and current medication side effects. These notes can guide healthcare teams in making informed decisions about care. Taking the time to ensure each part of Form 8584 is complete and accurate benefits both the individual and their care team.
Documents used along the form
The Texas Department of Aging Form 8584 is primarily used for comprehensive nursing assessments. While this form serves a specific purpose, several other documents may be required to support its findings or to provide additional context. Here is a list of related forms and documents that are often used alongside Form 8584.
- Consent for Treatment Form: This document grants permission for healthcare providers to administer treatment or perform procedures on a patient. It ensures that clients or their guardians understand the risks and benefits of treatments offered.
- Medical History Form: This form captures a patient’s past medical and surgical history. It provides a comprehensive overview of previous conditions, treatments, and outcomes that can influence current care.
- Medications Administration Record (MAR): The MAR is used to document all medications administered to a patient. This record includes details such as dose, frequency, and administration route, ensuring medication management is tracked effectively.
- Fall Risk Assessment Form: This document evaluates a patient’s risk of falling based on various factors including medical history and functional abilities. It is often used in conjunction with the Form 8584 to assess safety in care settings.
- Nursing Care Plan: A nursing care plan outlines specific care strategies based on assessment findings. It details nursing diagnoses, goals, and interventions tailored to the individual’s needs as identified in the 8584 form.
- Incident Report Form: This form is completed following any incident that affects a patient’s health or safety. It documents details such as nature of the incident and responses, and is vital for quality control and improvement.
- Client Rights and Responsibilities Form: This document outlines the rights of patients and their responsibilities while receiving care. It helps ensure that clients understand their entitlements and obligations in a healthcare setting.
- Health Insurance Portability and Accountability Act (HIPAA) Authorization Form: This form is necessary for sharing a patient’s protected health information (PHI) with others, typically required for treatment or billing purposes.
- Advanced Directive Form: This document provides guidance on a patient's preferences for medical treatment in case they become unable to communicate their wishes. It can include living wills and powers of attorney.
- Discharge Summary Form: This form summarizes a patient’s health status upon discharge. It includes treatment received, follow-up plans, and any ongoing needs, ensuring continuity of care post-discharge.
These documents are essential in providing a comprehensive view of a patient’s health, ensuring that care is tailored to individual needs while also adhering to legal and procedural standards. Each form plays a specific role in the broader context of healthcare documentation.
Similar forms
- Form 485: This is a similar document used for home health care services. It encompasses health assessments and care plans for individuals, much like the comprehensive evaluations in Form 8584.
- Form 5500: This form is utilized for employee benefit plans. It helps in reporting health and welfare benefits, establishing compliance with regulations, akin to the assessment of medical needs in Form 8584.
- Form CMS-1500: Primarily used for insurance claims, this form collects similar health information and services rendered by healthcare providers, aligning with the medical history collection in Form 8584.
- Form 1040: While typically associated with taxes, certain sections require disclosures about health expenses. This reflects the financial aspect of healthcare that impacts the assessments in Form 8584.
- Form I-485: This application for a green card collects personal health and background information, similarly examining individual circumstances as seen in Form 8584.
- Form 2781: Used for Medicaid eligibility determination, it gathers health and financial information, paralleling the detailed health reviews in Form 8584.
- Form 1493: Similar to Form 8584, this document is used for disability claims and includes assessments of medical conditions and support needs.
- Form MDS (Minimum Data Set): This assessment tool is used in nursing homes to evaluate residents' medical, physical, and mental conditions, sharing a focus on comprehensive evaluations like Form 8584.
Dos and Don'ts
When filling out the 8584 form, it's essential to follow some basic guidelines to ensure accuracy and completeness. Here are four things you should and shouldn't do.
- Do provide complete and accurate personal information, including the date of birth and today's date.
- Don't leave any sections blank unless instructed. Fill in all relevant details to avoid delays.
- Do list all current medications, including over-the-counter drugs, vitamins, and herbal supplements.
- Don't assume the reviewer knows the individual's medical or psychiatric history. Provide thorough explanations for any changes or concerns.
Misconceptions
Misconceptions about the Texas Form 8584 can often lead to confusion and frustration regarding its purpose and use. Here's a list of common myths and explanations to clarify them:
- Form 8584 is only for elderly patients. This form is designed for individuals of various ages who require a comprehensive nursing assessment, not solely for older adults.
- You only need to fill out Form 8584 if there are major health issues. Even if the patient appears healthy, this form helps establish a baseline for future assessments and identifies potential risks.
- All healthcare providers are required to use Form 8584. While it is a standard form in many facilities, not every provider may use it. Some may employ different assessment tools based on their protocols.
- The assessment must be completed by a doctor. Form 8584 specifically states that it should be performed by a registered nurse, ensuring nurses play a key role in patient assessments.
- Once submitted, the form cannot be updated. Updates and revisions are allowed; it's important to keep the information current as the patient’s health status changes.
- Filling out the form is optional. For many healthcare facilities, a comprehensive nursing assessment and the subsequent documentation are mandatory processes for patient care.
- Form 8584 is complicated and time-consuming. While thorough, the form is structured to facilitate clear communication among care teams, ultimately benefiting patient care.
- The form only gathers medical information. It also includes assessments of social factors and patient concerns, providing a holistic view of the individual’s needs.
Understanding these misconceptions helps clarify the importance of the Form 8584 in delivering quality healthcare. It serves as a vital tool for capturing a complete picture of an individual's health status and supporting their healthcare journey.
Key takeaways
Filling out and utilizing the 8584 form properly is essential for ensuring comprehensive nursing assessments. Here are some key takeaways to consider:
- Preparation is crucial. Gather all necessary medical history, including information about medications, allergies, and previous medical encounters before starting the form.
- Details matter. Provide thorough descriptions of the individual's health status, changes in behavior, and any recent hospitalizations or falls to paint a complete picture for healthcare providers.
- Team collaboration is important. Consultation with the healthcare team, including primary care and specialists, is encouraged to ensure that all viewpoints are represented and any concerns are addressed.
- Ongoing monitoring is necessary. Regularly review and update the individual’s information, including vital signs and lab results, to reflect any changes in their condition.
- Fall risk assessments should be prioritized. Completing a fall risk assessment is vital, as it helps identify potential hazards and informs strategies to prevent falls in high-risk individuals.
Browse Other Templates
Argosy University Online - It is essential to include the name of the college or university attended for accurate processing.
How to Pay a Cell Phone Ticket in California - To submit, save the form as an attachment.
How to Get Pa License Plate - Detailed instructions guide the user on how to fill out different sections.