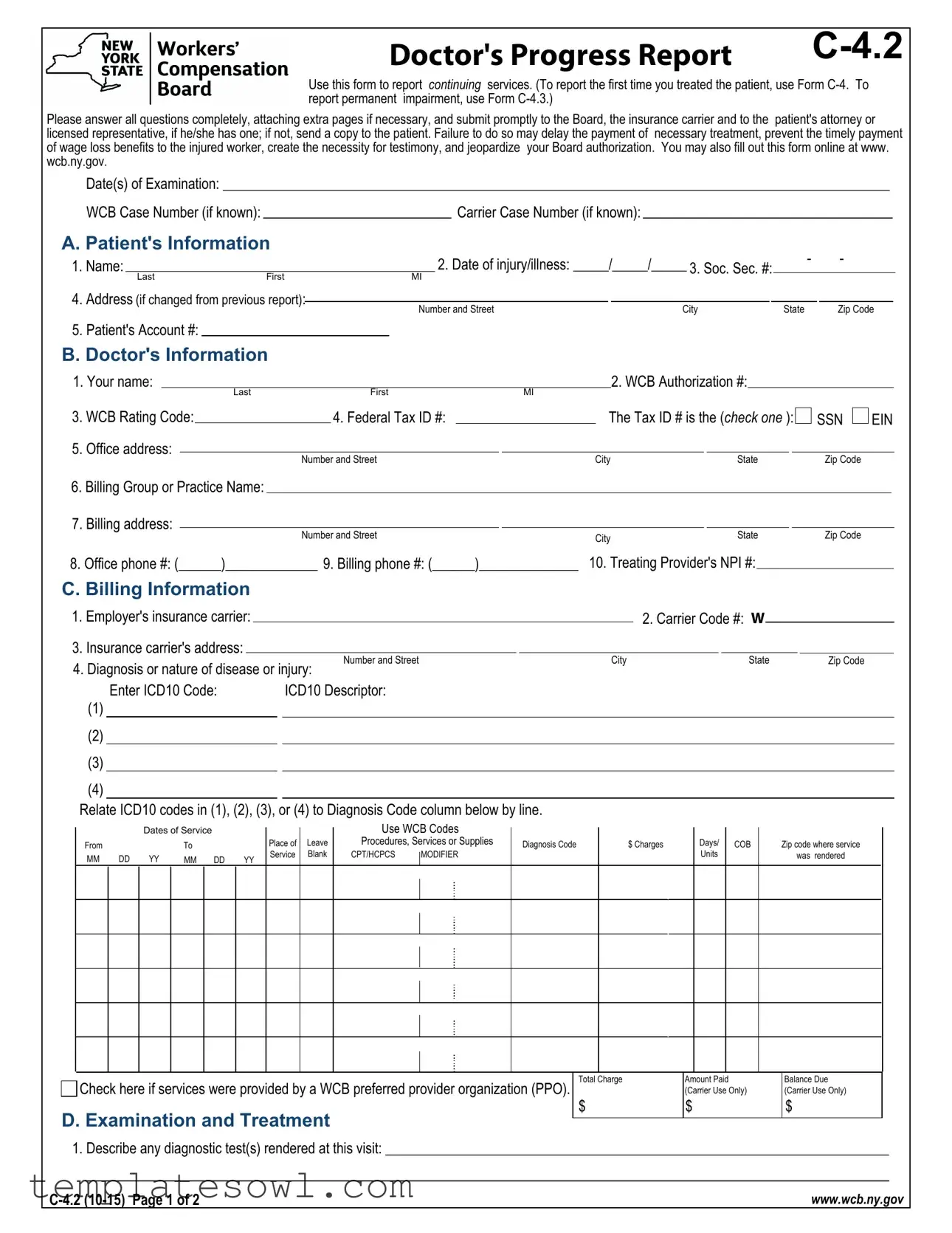
Fill Out Your C4 2 Form
The C4 2 form, officially termed the Doctor's Progress Report C-4.2, serves a critical role in the workers’ compensation system. It is specifically designed for healthcare providers to document and report ongoing treatment and medical evaluations for patients with work-related injuries or illnesses. This form must be filled out following the initial report, known as Form C-4, and is essential for maintaining consistent communication between doctors, the Workers' Compensation Board, insurance carriers, and any legal representatives involved. Each field on the form requires comprehensive answers, ensuring that treatment updates, diagnostic tests, and any changes in a patient’s condition are clearly noted. Submitting this form promptly is crucial; delays can result in payment issues for medical services, hinder wage-loss benefits for injured workers, and potentially jeopardize the healthcare provider's authorization status. Notably, if the injured party is represented by an attorney, an exact copy must be forwarded to them as well. For your convenience, the form can also be completed online, making the process more efficient and accessible.
C4 2 Example
Doctor's Progress Report |
Use this form to report continuing services. (To report the first time you treated the patient, use Form
Please answer all questions completely, attaching extra pages if necessary, and submit promptly to the Board, the insurance carrier and to the patient's attorney or licensed representative, if he/she has one; if not, send a copy to the patient. Failure to do so may delay the payment of necessary treatment, prevent the timely payment of wage loss benefits to the injured worker, create the necessity for testimony, and jeopardize your Board authorization. You may also fill out this form online at www. wcb.ny.gov.
Date(s) of Examination: ______________________________________________________________________________________________
WCB Case Number (if known):Carrier Case Number (if known):
A. Patient's Information
1. Name: |
|
|
|
2. Date of injury/illness: _____/_____/_____ 3. Soc. Sec. #: |
- |
|
- |
|
||||
|
|
|
|
|
|
|
||||||
|
Last |
First |
MI |
|
|
|
|
|
|
|
|
|
4. Address (if changed from previous report): |
|
|
|
|
|
|
|
|
|
|
||
Number and Street |
|
City |
State |
Zip Code |
||||||||
|
|
|
|
|||||||||
5.Patient's Account #:
B.Doctor's Information
1.Your name:
3.WCB Rating Code:
5.Office address:
Last |
|
First |
MI |
2. WCB Authorization #: |
|||||
|
|
|
|
|
|||||
|
|
4. Federal Tax ID #: |
|
|
The Tax ID # is the (check one ): |
||||
|
|
|
|
|
|
|
|
|
|
|
Number and Street |
City |
|
|
State |
||||
SSN  EIN
EIN
Zip Code
6.Billing Group or Practice Name:
7.Billing address:
Number and Street
8. Office phone #: (______)_____________ 9. Billing phone #: (______)______________
City |
State |
Zip Code |
|
|
10. Treating Provider's NPI #:
C. Billing Information
1. Employer's insurance carrier: |
|
|
|
|
|
|
2. Carrier Code #: W |
|
|
|||||
|
|
|
|
|
|
|
|
|||||||
3. Insurance carrier's address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number and Street |
|
City |
|
|
State |
Zip Code |
||||
4. Diagnosis or nature of disease or injury: |
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
||||||
|
Enter ICD10 Code: |
|
ICD10 Descriptor: |
|
|
|
|
|
|
|
|
|||
(1) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(2) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(3) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(4)
Relate ICD10 codes in (1), (2), (3), or (4) to Diagnosis Code column below by line.
|
|
Dates of Service |
|
|
From |
|
|
To |
|
MM |
DD |
YY |
MM DD |
YY |
Place of Service
Leave Blank
Use WCB Codes
Procedures, Services or Supplies
CPT/HCPCS MODIFIER
Diagnosis Code
$ Charges
Days/
Units
COB
Zip code where service
was rendered
Check here if services were provided by a WCB preferred provider organization (PPO).
D. Examination and Treatment
Total Charge
$
Amount Paid (Carrier Use Only)
$
Balance Due (Carrier Use Only)
$
1. Describe any diagnostic test(s) rendered at this visit: _______________________________________________________________________
www.wcb.ny.gov |
|||
|
|
|
|
Patient's Name: |
|
|
|
Date of injury/onset of illness:______/______/______ |
|
Last |
First |
MI |
|
2.List any changes revealed by your most recent examination in the following: area of injury, type/nature of injury, patient's subjective complaints
or your objective findings: _____________________________________________________________________________________________
3.List additional body parts affected by this injury, if any: ______________________________________________________________________
4.Based on your most recent examination, list changes to the original treatment plan, prescription medications or assistive devices, if any:
5. Based on this examination, does the patient need diagnostic tests or referrals? |
Yes |
No |
If yes, check all that apply: |
|||||
Tests: |
|
Referrals: |
|
|
|
|||
CT Scan |
EMG/NCS |
Chiropractor |
|
|
Internist/Family Physician |
|||
MRI (specify): |
|
|
Occupational Therapist |
|
||||
Labs (specify): |
|
|
Physical Therapist |
|
|
|||
|
Specialist in: |
|
|
|
||||
|
|
|
|
|
|
|
|
|
Other (specify): |
|
Other (specify): |
|
|
||||
Important: Form
6. Describe treatment rendered today:
7. When is patient's next
Within a week
____ months
as needed
E. Doctor's Opinion (based on this examination)
1. In your opinion, was the incident that the patient described the competent medical cause of this injury/illness? 2. Are the patient's complaints consistent with his/her history of the injury/illness? 



Yes
No
3.Is the patient's history of the injury/illness consistent with your objective findings?
4.What is the percentage

 N/A (no findings at this time)
N/A (no findings at this time)
5.Describe findings and relevant diagnostic test results:_______________________________________________________________________
_________________________________________________________________________________________________________________
F.Return to Work
1. Is patient working now? |
Yes |
No |
If yes, are there work restrictions? |
Yes |
No If yes, describe the work restrictions: |
|
||||
|
|
|
|
|
|
|
|
|||
|
How long will the work restrictions apply? |
15+ days |
Unknown at this time |
|
||||||
2. Can patient return to work? (check only one) |
|
|
|
|
|
|||||
|
a. |
The patient cannot return to work because (explain): |
|
|
|
|
|
|||
b. The patient can return to work without limitations on: _______/_______/_______
The patient can return to work without limitations on: _______/_______/_______
c. The patient can return to work with the following limitations (check all that apply) on: _______/_______/_______
The patient can return to work with the following limitations (check all that apply) on: _______/_______/_______
Bending/twisting |
|
Lifting |
|
|
|
Sitting |
|
|
||
Climbing stairs/ladders |
|
Operating heavy equipment |
|
Standing |
|
|
||||
Environmental conditions |
|
Operation of motor vehicles |
|
Use of public transportation |
|
|||||
Kneeling |
|
Personal protective equipment |
|
Use of upper extremities |
|
|
||||
Other (explain): |
|
|
|
|
|
|
|
|
|
|
Describe/quantify the limitations: |
|
|
|
|
|
|
|
|
|
|
How long will these limitations apply? |
15+ days |
Unknown at this time |
N/A |
|
||||||
3. With whom will you discuss the patient's returning to work and/or limitations? |
with patient |
with patient's employer |
N/A |
|
||||||
4. Would the patient benefit from vocational rehabilitation? |
Yes |
No |
|
|
|
|
|
|||
This form is signed under penalty of perjury. |
|
|
|
|
|
|
|
|
||
Board Authorized Health Care Provider - Check one: |
|
|
|
|
|
|
|
|||
I provided the services listed above. |
|
|
||
I actively supervised the |
|
|||
|
Provider's name___________________________________________________ Specialty__________________________________ |
|||
Board Authorized Health Care Provider signature: |
|
|
||
|
|
|
/ |
/ |
Name |
|
Signature |
Specialty |
Date |
www.wcb.ny.gov |
|||
|
|
|
|
MEDICAL REPORTING
IMPORTANT - TO THE ATTENDING DOCTOR
1.This form is to be used to file reports in workers' compensation, volunteer firefighters' or volunteer ambulance workers' benefit cases as follows:
PROGRESS REPORTS - Following the filing of Form
When reporting on MMI and/or Permanent Impairment, use Form
All reports are to be filed with the Workers' Compensation Board, the workers' compensation insurance carrier,
Ophthalmologists use Form
2.Please ask your patient for his/her WCB Case Number and the Insurance Carrier's Case Number, if they are known to him/her, and show these numbers on your reports. In addition, ask your patient if he/she has retained a representative. If so, ask for the name and address of the representative. You are required to send copies of all reports to the patient's representative, if any.
3.This form must be signed by the attending doctor and must contain her/his authorization certificate number, code letters and NPI number. If the patient is hospitalized, it may be signed by a licensed doctor to whom the treatment of the case has been assigned as a member of the attending staff of the hospital.
4.AUTHORIZATION FOR SPECIAL SERVICES - Form
AUTHORIZATION FOR SPECIAL SERVICES IS NOT REQUIRED IN AN EMERGENCY
5.LIMITATION OF PODIATRY TREATMENT - Podiatry treatment is limited as defined in Section 7001 of the Education Law and Section
6.LIMITATION OF CHIROPRACTIC TREATMENT - Chiropractic treatment is limited as defined in Section 6551 of the Education Law and the Chair's Rules Relative to Chiropractic Practice Under Section
A CHIROPRACTOR OR PODIATRIST FILING THIS REPORT CERTIFIES THAT THE INJURY DESCRIBED CONSISTS SOLELY OF A CONDITION(S) WHICH MAY LAWFULLY BE TREATED AS
DEFINED IN THE EDUCATION LAW AND, WHERE IT DOES NOT, HAS ADVISED THE INJURED PERSON TO CONSULT A PHYSICIAN OF HIS/HER CHOICE.
7.HIPAA NOTICE - In order to adjudicate a workers' compensation claim,
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR
BILLING INFORMATION
Complete all billing information contained on this form. Use continuation Form
IMPORTANT TO THE PATIENT
YOUR DOCTORS' BILLS (AND BILLS FOR HOSPITALS AND OTHER SERVICES OF A MEDICAL NATURE) WILL BE PAID BY YOUR EMPLOYER, THE LIABLE POLITICAL SUBDIVISION OR ITS INSURANCE COMPANY OR THE UNAFFILIATED VOLUNTEER AMBULANCE SERVICE IF YOUR CLAIM IS ALLOWED. DO NOT PAY THESE BILLS YOURSELF, UNLESS YOUR CASE IS DISALLOWED OR CLOSED FOR FAILURE TO PROSECUTE.
IF YOU HAVE ANY QUESTIONS CONCERNING THIS NOTICE OR YOUR CASE, OR WITH RESPECT TO YOUR RIGHTS UNDER THE WORKERS' COMPENSATION LAW, OR THE VOLUNTEER FIREFIGHTERS' OR VOLUNTEER AMBULANCE WORKERS' LAWS, YOU SHOULD CONSULT THE NEAREST OFFICE OF THE BOARD FOR ADVICE. ALWAYS USE THE CASE NUMBERS SHOWN ON THE OTHER SIDE OFTHIS NOTICE, OR ON OTHER PAPERS RECEIVED BY YOU, IF YOU FIND IT NECESSARY TO COMMUNICATE WITH THE BOARD OR THE CARRIER. ALSO, MENTION YOUR SOCIAL SECURITY NUMBER IF YOU WRITE OR CALL THE BOARD.
LAS FACTURAS POR SERVICIOS MEDICOS INCLUYENDO HOSPITALES Y TODO SERVICIO DE NATURALEZA MEDICA SERA PAGADO POR EL PATRONO O POR LA ENTIDAD RESPONSABLE O SU COMPANIA DE SEGUROS SEGUN SEA EL CASO; SI SU RECLAMACION ES APROBADA. NO PAGUE ESTAS FACTURAS A MENOS QUE SU CASO SEA DESESTIMADO EN SU FONDO O ARCHIVADO POR NO REALIZAR LOS TRAMITES CORRESPONDIENTES.
SI USTED TIENE ALGUNA PREGUNTA, EN RELACION A ESTA NOTIFICACION O A SU CASO O EN RELACION A SUS DERECHOS BAJO LA LEY DE COMPENSACION OBRERA O LA LEY DE BOMBEROS VOLUNTARIOS O LA LEY DE SERVICIOS DE AMBULANCIAS VOLUNTARIOS DEBE COMUNICARSE CON LA OFICINA MAS CERCANA DE LA JUNTA PARA ORIENTACION. SIEMPRE USE EL NUMERO DEL CASO QUE APARECE EN LA PARTE DEL FRENTE DE ESTA NOTIFICACION, O EN OTROS DOCUMENTOS RECIBIDOS POR USTED. SI LE ES NECESARIO COMUNICARSE CON LA JUNTA O CON EL "CARRIER."
TAMBIEN MENCIONE EN SU COMUNICACION ORAL O ESCRITA SU NUMERO DE SEGURO SOCIAL.
WORKERS' COMPENSATION BOARD
Reports should be filed by sending directly to the WCB at the address below with a copy sent to the insurance carrier:
NYS Workers' Compensation Board
Centralized mailing
PO Box 5205
Binghamton, NY
Customer Service
Statewide Fax Line:
THE WORKERS' COMPENSATION BOARD EMPLOYS AND SERVES PEOPLE WITH DISABILITIES WITHOUT DISCRIMINATION
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The C4 2 Form, also known as the Doctor's Progress Report, is used to report ongoing treatment and services related to workers' compensation cases. |
| Initial Reporting | For the first treatment report, healthcare providers must use Form C-4 instead of the C4 2 Form. |
| Permanent Impairment Report | To report permanent impairment, Form C-4.3 should be utilized. |
| Filing Requirements | Reports must be submitted to the Workers' Compensation Board, the patient's insurance carrier, and the patient's attorney if they have one. Failure to do so may delay necessary payments. |
| Timelines | The form should be submitted promptly and no later than 15 days after the initial report following continued treatment. |
| Patient Information | Providers must include comprehensive patient information, such as name, date of injury, and social security number, to ensure accurate processing. |
| Doctor's Insights | Among various sections, healthcare providers are tasked with providing opinions about the relationship between the incident and the patient's injury. |
| Return to Work Assessment | The form includes questions about the patient's ability to return to work and any needed work restrictions. |
| Online Submission | Providers can fill out and submit the form online through the New York Workers' Compensation Board's website. |
| Governing Laws | New York Workers' Compensation Law governs the use and filing of the C4 2 Form, as well as related forms. |
Guidelines on Utilizing C4 2
Completing the C4 2 form is essential for healthcare providers reporting ongoing treatment. The process requires careful attention to detail. Each section must be filled out accurately to avoid delays in processing. Following the steps outlined below will help ensure that the form is completed correctly.
- Date(s) of Examination: Enter the date(s) when the examination took place.
- WCB Case Number: If known, provide the Workers' Compensation Board case number.
- Patient's Information: Complete the patient's full name, date of injury or illness, Social Security number, address, and account number.
- Doctor's Information: Fill in your name, WCB authorization number, federal tax ID number, billing group name, office address, contact numbers, and NPI number.
- Billing Information: Indicate the employer's insurance carrier, carrier code, insurance carrier’s address, diagnosis or nature of disease or injury, and relevant ICD10 codes and descriptors.
- Dates of Service: Record the service dates, place of service, procedures or services performed, applicable WCB codes, charges, and units.
- Examination and Treatment: Describe any diagnostic tests performed, changes in injury status, affected body parts, revisions to the treatment plan, and any diagnostic tests or referrals needed.
- Doctor's Opinion: Provide your opinion on the incident's causation of the injury, consistency of complaints, history matching findings, percentage of temporary impairment, and relevant findings from tests.
- Return to Work: Answer if the patient is currently working, detail any work restrictions and their duration, and indicate whether the patient can return to work with or without limitations.
- Signature: Ensure to sign the form, providing your name, specialty, and the date.
Once the form is completed, it must be submitted to the appropriate parties including the Workers' Compensation Board, the insurance carrier, and the patient or their representative if applicable. Timely submission is crucial to avoid hindering the patient's treatment and consultation processes.
What You Should Know About This Form
What is the purpose of the C4 2 form?
The C4 2 form, also known as the Doctor's Progress Report, is used to report ongoing treatment for patients involved in workers' compensation cases. This form is particularly important for tracking a patient's progress and outlining any changes in their treatment plan or condition. It is vital to complete this form accurately and submit it promptly to avoid delays in treatment and benefits.
Who should fill out the C4 2 form?
The C4 2 form must be completed by the attending physician or licensed medical provider overseeing the patient's treatment. This includes detailing the patient's condition, treatment provided, and future care plans. The form needs to be signed by the doctor, ensuring that it is valid and documents the necessary information regarding the patient's progress.
When should the C4 2 form be submitted?
The C4 2 form should be submitted within 15 days following the initial report using Form C-4. It is essential to continue submitting follow-up reports as the patient receives further treatment, but no more than every 90 days should pass between reports. Timeliness is critical for the processing of claims and the provision of benefits.
What information must be included on the C4 2 form?
The C4 2 form requires comprehensive information, including the patient's and physician's contact details, the WCB case number, details of examinations, treatments provided, and any diagnostic tests performed. Additionally, changes to the treatment plan, findings from examinations, and the physician's opinion about the patient's work capabilities are also needed. Providing complete and accurate information is crucial.
What happens if the C4 2 form is not submitted correctly?
Failure to submit the C4 2 form accurately or on time can result in several complications. It may delay payments for necessary treatments and disrupt wage loss benefits for the injured worker. In some cases, it could result in the need for legal testimony and even jeopardize the physician's authorization to provide treatment under workers' compensation law.
How does a patient or doctor determine any changes in the treatment plan?
Changes in the treatment plan can emerge based on the physician's latest examination findings, the patient's reports of symptoms, and any diagnostic tests conducted during the recent visit. The doctor will thoroughly assess these elements and determine if adjustments are needed before documenting them on the C4 2 form.
Can the C4 2 form be filled out online?
Yes, the C4 2 form can be completed online, which can streamline the process. Healthcare providers can visit the New York State Workers' Compensation Board website at www.wcb.ny.gov to access the form and submit it electronically, making it more convenient and efficient.
What should a patient do if they do not have a representative?
If a patient does not have a legal representative, the physician must send a copy of the C4 2 form directly to the patient. This ensures that the patient remains informed about their treatment progress and any pertinent information related to their workers' compensation claim.
What forms should be used in conjunction with the C4 2 form?
When dealing with initial reports, the physician should use Form C-4. If addressing permanent impairment, Form C-4.3 is appropriate. For special medical services that exceed $1,000 or need pre-authorization, Form C-4 AUTH should be submitted when required.
Why is accurate diagnosis coding important on the C4 2 form?
Accurate diagnosis coding is critical for ensuring that the patient's treatment is appropriately covered under their workers' compensation claim. It helps in proper categorization, streamlining the billing process, and ensuring compliance with medical guidelines. Mistakes in coding can lead to denial of claims and complications in receiving necessary care.
Common mistakes
Filling out the C4 2 form can be a complex task, and errors can lead to significant delays in treatment and benefits for injured workers. One common mistake occurs during the completion of the patient's information section. Often, individuals fail to provide complete or accurate details, such as the patient’s name or social security number. This omission can complicate the identification process for the Workers' Compensation Board and the insurance carrier, potentially delaying critical services.
Another frequent error involves the WCB and carrier case numbers. Many people neglect to ensure that these numbers are correctly recorded. When the case numbers are missing or incorrect, it can lead to confusion and may require multiple follow-ups to get the necessary paperwork sorted out. This delay further complicates the patient's treatment and recovery timeline.
In the doctor’s information section, mistakes can also occur. Providers might misenter their federal tax ID numbers or fail to specify their WCB authorization number. These details are vital for reimbursement processes. If the insurance carrier cannot verify a provider's credentials, claims may be rejected, and payment delays will ensue.
Another area prone to error is the billing information section. It is crucial to detail the diagnosis accurately. Incorrect ICD10 codes can lead to denied claims. If a provider overlooks specifying the nature of the disease or injury or enters a diagnosis code that does not correspond to the reported symptoms, it can result in complications and delays in obtaining payments for services rendered.
Patients and providers alike often misjudge the examination and treatment details. When describing any diagnostic tests rendered, some may overlook providing complete information. A vague description leaves questions unanswered, which can delay authorization for further treatment. Similarly, failing to note any changes in the patient's condition since the last visit or neglecting to document additional affected body parts can lead to a lack of clarity around the patient's ongoing needs.
In the return to work section, individuals may fail to clearly indicate the patient’s work status and any restrictions that may apply. Inadequately outlining these limitations poses a risk; it might send conflicting signals to employers or fail to protect the patient from undertaking inappropriate work tasks during recovery. Accurate and clear communication of such limitations is vital for compliance and for the patient’s welfare.
Finally, taking too long to submit the completed C4 2 form can result in unnecessary complications. The form must be submitted promptly to prevent delays in treatment and ensure that the injured worker can access wage loss benefits without interruption. Anything less than prompt submission can affect the entire workers’ compensation claim process, leading to frustration and stress for all parties involved.
Documents used along the form
The C4 2 form, also known as the Doctor's Progress Report, serves a critical role in the reporting and management of workers’ compensation claims. Several other forms accompany this document in the workers’ compensation process. Each form serves a specific purpose, ensuring that proper information is collected, reviewed, and followed up on as needed. Below is a list of additional forms often utilized in conjunction with the C4 2 form.
- C-4 Form: This is the Doctor's Initial Report. It is the first report made by a doctor after treating a patient for a work-related injury or illness. This form establishes the initial details of the patient's condition, diagnosis, and treatment plan.
- C-4.3 Form: Known as the Doctor’s Permanent Impairment Report, this form is used when the patient is evaluated for any lasting impairment due to their injury. It assesses the extent of long-term effects and helps determine ongoing benefits.
- C-4 AUTH Form: This Authorization for Special Services form is required to request any medical services that exceed a cost of $1,000. It also covers any services that require prior approval according to specific medical guidelines.
- C-4.1 Form: This is a Continuation Report for billing purposes. It is often used when the original form does not have enough space to accommodate additional billing information. This helps ensure that all charges are accurately recorded for the insurance carrier.
- OT/PT-4 Form: Occupational and physical therapists use this form to file their reports when they are providing treatment. The report details the nature of the therapy and its progress over time.
- C-5 Form: Ophthalmologists use this form to report on treatment related to eye injuries incurred while working. This document captures specific details relevant to eye care and treatment progress.
- PS-4 Form: This form is utilized by psychologists to document their treatment and evaluations of patients who have experienced mental health issues due to work-related incidents. It includes important details about assessments and therapeutic interventions.
Utilizing these forms in conjunction with the C4 2 form helps ensure a comprehensive approach to managing workers’ compensation claims. Accurate and timely reporting not only facilitates the claims process but also supports the injured worker's recovery and access to necessary benefits.
Similar forms
Form C-4: The initial report filed by a doctor after a patient's first treatment. Like the C4 2 form, it collects essential patient data and details the nature of the injury or illness.
Form C-4.3: This form is used to report permanent impairment. Similar to the C4 2, it presents information about the patient's condition after a thorough examination, ensuring that detailed medical information flows seamlessly for insurance evaluation.
Form C-5: An ophthalmologist’s report used to document conditions related to vision. It follows a similar structure as the C4 2 form but is specific to eye-related injuries, requiring detailed examinations and treatment plans.
Form OT/PT-4: Designed for occupational and physical therapists, this form captures treatment reports and progress like the C4 2. Both forms aim to keep insurance carriers informed on patient progress and necessary changes in treatment.
Form PS-4: This form is utilized by psychologists to report on mental health treatment. Its purpose aligns with the C4 2 as it chronicles the patient's mental state and necessary therapeutic measures.
Form C-4 AUTH: This form requests special medical services costing over $1000. While it serves a different purpose, it complements the C4 2 by ensuring that necessary and expensive treatments receive appropriate approval.
Form C-4.1: A continuation form used for billing when additional space is needed. Like the C4 2, it serves to ensure that all billing information is clearly documented and submitted correctly for timely processing.
Form C-11: This is an application for the reimbursement of medical expenses related to a worker's compensation claim. It parallels the C4 2 in documenting treatment costs and ensuring proper submission to the relevant compensation board.
Form WCB-703: This form is for reporting and documenting injuries sustained by volunteer firefighters. Similarly structured to the C4 2, it emphasizes rapid reporting to facilitate the claims process.
Form WCB-8: Used for employer reporting to document accidents or workplace injuries. Like the C4 2, it serves to keep all parties informed and strengthens the claims process through clear communication.
Dos and Don'ts
When completing the C4 2 form, it's essential to ensure accuracy and thoroughness. To help you navigate the process, here are seven important points to keep in mind:
- DO fill out the form completely, answering all questions to avoid delays in processing.
- DON'T submit the form late; ensure it is sent promptly to the appropriate parties.
- DO attach any additional pages if you run out of space for detailed answers.
- DON'T forget to provide the WCB Case Number and the Carrier Case Number, if known.
- DO include your signature and necessary authorization codes before submission.
- DON'T overlook the billing information; complete all sections to facilitate timely payment.
- DO inform the patient about who will receive copies of the report, especially if they have legal representation.
Following these guidelines can help ensure the process goes smoothly for all parties involved. Proper completion of the C4 2 form is crucial in facilitating the patient's continuous treatment and securing appropriate benefits.
Misconceptions
Misconception 1: The C4 2 form is only for initial injuries.
This form is designed for ongoing treatment reporting. It is used after the initial report filed with Form C-4 and for any subsequent progress in treatment.
Misconception 2: All information on the form is optional.
Many fields must be completed. Providing complete information is crucial to ensure timely payment for treatment and benefits.
Misconception 3: Only doctors can fill out the C4 2 form.
While physicians generally complete this form, any authorized healthcare provider can do so as long as they meet the required qualifications.
Misconception 4: The C4 2 form does not require submission to multiple parties.
This form must be submitted to the Workers' Compensation Board, the insurance carrier, and the patient's attorney or licensed representative if one exists. Failing to do so can delay benefits.
Misconception 5: Patients do not need a copy of the C4 2 form.
Patients are entitled to receive a copy, especially if they do not have legal representation. This increases their awareness of their treatment progress and rights.
Misconception 6: The C4 2 form can be submitted at any time.
It should be filed within 15 days after the initial report and periodically thereafter, not exceeding 90 days between reports for continuous treatment.
Misconception 7: The C4 2 form covers any type of medical service.
This form specifically pertains to workers' compensation claims. For services over $1,000 or that require pre-authorization, a different form, C4 AUTH, must be used.
Misconception 8: Completing the C4 2 form guarantees payment for treatment.
Submission of the form does not guarantee payment. The insurance carrier reviews the documentation and may issue objections or requests for additional information.
Misconception 9: A single signature is acceptable on the C4 2 form.
The form requires signature from the attending doctor, ensuring that the healthcare provider authorizes the reported services and findings.
Key takeaways
Here are some key points to remember when filling out and using the C4 2 form:
- Complete the Form: Make sure to answer all questions completely. You can include additional pages if needed.
- Timely Submission: Submit the form promptly to the relevant parties, including the Board, insurance carrier, and the patient's attorney or representative.
- Use the Correct Form: Remember to use Form C-4 for the initial treatment report and Form C-4.3 for permanent impairment reports.
- Field Details Matter: Fill in all required fields, especially patient and doctor information, diagnosis codes, and billing details.
- Follow-Up Visits: Indicate when the next follow-up appointment is scheduled. This helps track the patient’s progress.
- Keep Copied Records: Always keep a copy of the submitted form for your records and future reference.
Using this form accurately is crucial for ensuring proper treatment payment and benefits for the injured worker.
Browse Other Templates
Anthem Vision Claim Form - Use the claims form to request reimbursement for various types of vision services.
When Do You Need Probate - The document ensures that only interested parties can participate in the probate process, maintaining fairness in representation.
How to Register With Blackfoot Indian Tribe - The address change form must be filled out in print.