Fill Out Your Cdc 7336 Form
The CDC 7336 form plays a crucial role in ensuring the health and safety of employees within the California Department of Corrections and Rehabilitation (CDCR). This confidential document is designed specifically for the Tuberculin Skin Test (TST) and evaluation, which is mandated for employees to screen for tuberculosis (TB) infection. The TST must be administered by a licensed healthcare provider who has the authority to conduct medical examinations. It allows for the systematic collection of medical information concerning each employee's TB status and previous test history. The form prompts the employee to provide personal details, including name, gender, birth date, and whether they are a new hire. Moreover, it includes sections that healthcare providers must complete to document the administration of the TST or any TB blood tests. Section 4 calls for a thorough evaluation for signs and symptoms of TB, and if necessary, a chest X-ray. This information is vital for protecting not only the individual employee but also their coworkers and the broader community from potential TB exposure. Proper completion and submission of the CDC 7336 form ensures compliance with the guidelines set forth by public health authorities, ultimately contributing to the management and prevention of tuberculosis in a workplace setting.
Cdc 7336 Example
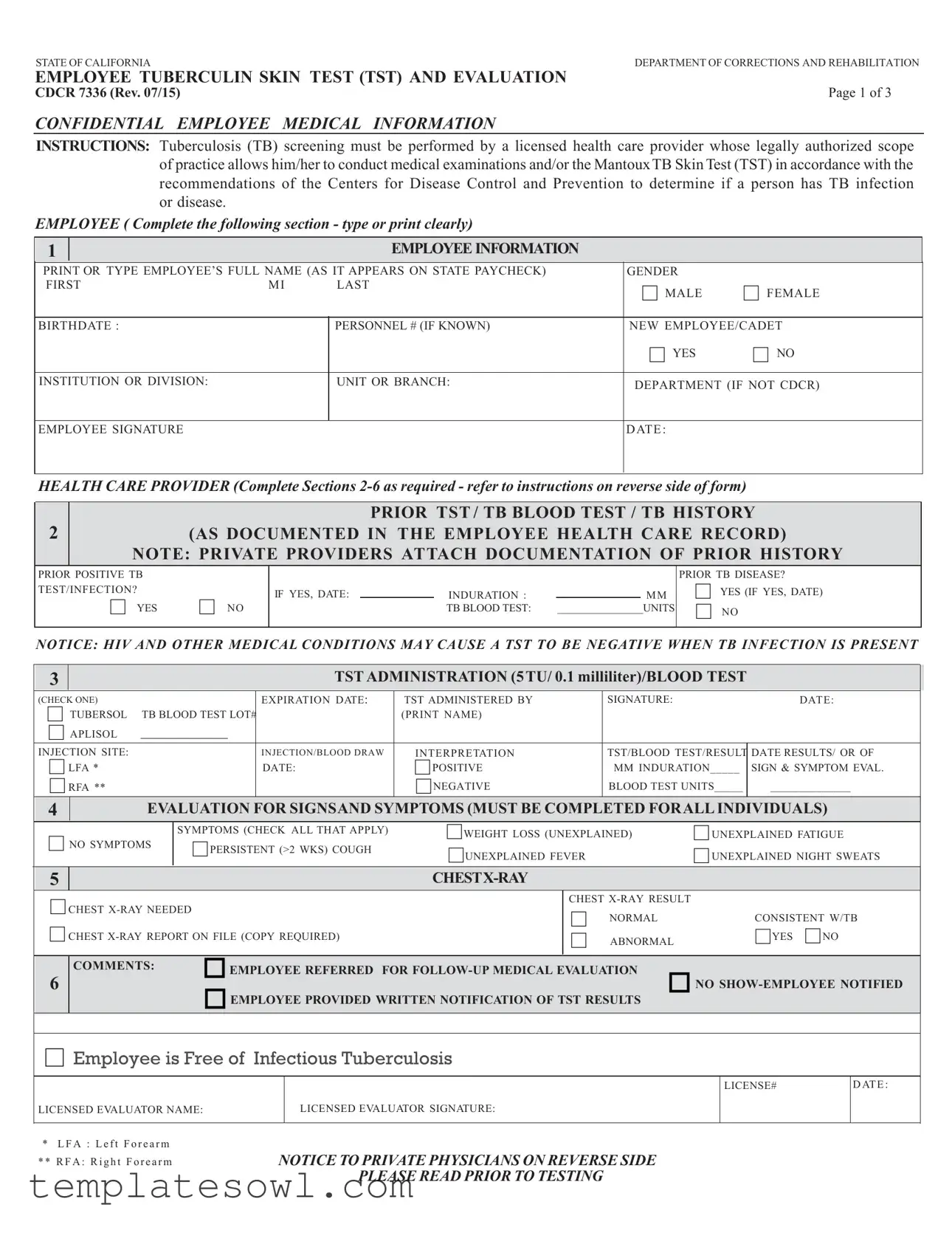
STATE OF CALIFORNIA |
DEPARTMENT OF CORRECTIONS AND REHABILITATION |
EMPLOYEE TUBERCULIN SKIN TEST (TST) AND EVALUATION |
|
CDCR 7336 (Rev. 07/15) |
Page 1 of 3 |
CONFIDENTIAL EMPLOYEE MEDICAL INFORMATION
INSTRUCTIONS: Tuberculosis (TB) screening must be performed by a licensed health care provider whose legally authorized scope of practice allows him/her to conduct medical examinations and/or the MantouxTB Skin Test (TST) in accordance with the recommendations of the Centers for Disease Control and Prevention to determine if a person has TB infection or disease.
EMPLOYEE ( Complete the following section - type or print clearly)
1
EMPLOYEE INFORMATION
PRINT OR TYPE EMPLOYEE’S FULL NAME (AS IT APPEARS ON STATE PAYCHECK) |
GENDER |
|
||
FIRST |
MI |
LAST |
MALE |
FEMALE |
|
|
|
||
|
|
|
|
|
BIRTHDATE : |
|
PERSONNEL # (IF KNOWN) |
NEW EMPLOYEE/CADET |
|
|
|
|
YES |
NO |
|
|
|
|
|
INSTITUTION OR DIVISION: |
|
UNIT OR BRANCH: |
DEPARTMENT (IF NOT CDCR) |
|
EMPLOYEE SIGNATURE
DATE :
HEALTH CARE PROVIDER (Complete Sections
2 |
|
|
|
PRIOR TST / TB BLOOD TEST / TB HISTORY |
||||
|
(AS DOCUMENTED IN THE EMPLOYEE HEALTH CARE RECORD) |
|||||||
|
NOTE: PRIVATE PROVIDERS ATTACH DOCUMENTATION OF PRIOR HISTORY |
|||||||
PRIOR POSITIVE TB |
|
|
|
|
|
|
PRIOR TB DISEASE? |
|
TEST/INFECTION? |
|
IF YES, DATE: |
|
INDURATION : |
|
MM |
YES (IF YES, DATE) |
|
|
YES |
NO |
|
|
TB BLOOD TEST: |
________________UNITS |
NO |
|
NOTICE: HIV AND OTHER MEDICAL CONDITIONS MAY CAUSE A TST TO BE NEGATIVE WHEN TB INFECTION IS PRESENT
3
TST ADMINISTRATION (5TU/ 0.1 milliliter)/BLOOD TEST
(CHECK ONE) |
EXPIRATION DATE: |
TST ADMINISTERED BY |
SIGNATURE: |
DATE: |
||
TUBERSOL TB BLOOD TEST LOT# |
|
(PRINT NAME) |
|
|
||
APLISOL |
|
|
|
|
|
|
|
|
|
|
|
||
INJECTION SITE: |
INJECTION/BLOOD DRAW |
INTERPRETATION |
TST/BLOOD TEST/RESULT |
DATE RESULTS/ OR OF |
||
LFA * |
DATE: |
POSITIVE |
MM INDURATION_____ |
SIGN & SYMPTOM EVAL. |
||
RFA ** |
|
NEGATIVE |
BLOOD TEST UNITS_____ |
______________ |
||
4EVALUATION FOR SIGNSAND SYMPTOMS (MUST BE COMPLETED FORALL INDIVIDUALS)
|
|
|
|
|
|
SYMPTOMS (CHECK ALL THAT APPLY) |
|
|
|
NO SYMPTOMS |
PERSISTENT (>2 WKS) COUGH |
WEIGHT LOSS (UNEXPLAINED) |
|
UNEXPLAINED FATIGUE |
UNEXPLAINED FEVER |
UNEXPLAINED NIGHT SWEATS |
|||
5
|
CHEST |
|
CHEST |
|
|||
|
|
|
NORMAL |
|
CONSISTENT W/TB |
||
|
CHEST |
|
|||||
|
ABNORMAL |
YES NO |
|||||
|
6 |
COMMENTS: |
EMPLOYEE REFERRED FOR |
NO |
|||
|
|
EMPLOYEE PROVIDED WRITTEN NOTIFICATION OF TST RESULTS |
|||||
|
|
|
|||||
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
Employee is Free of Infectious Tuberculosis |
|
|
|
|
||
LICENSED EVALUATOR NAME:
LICENSED EVALUATOR SIGNATURE:
LICENSE#
D ATE :
*LFA : Left Forearm ** RFA: Right Forearm
NOTICE TO PRIVATE PHYSICIANS ON REVERSE SIDE PLEASE READ PRIOR TO TESTING

STATE OF CALIFORNIADEPARTMENT OF CORRECTIONS AND REHABILITATION
EMPLOYEE TUBERCULIN SKIN TEST (TST) AND EVALUATION
CDCR 7336 (Rev. 07/15)
NOTICE TO PRIVATE PHYSICIANS
CONFIDENTIAL EMPLOYMENT MEDICAL INFORMATION
THE CALIFORNIA PENAL CODE, SECTION 6006 et seq., REQUIRES ALL CALIFORNIA DEPARTMENT OF CORRECTIONS AND REHABILITATION (CDCR) employees and certain other individuals to have an initial, annual, and as medically necessary Mantoux Tuberculin Skin Test (TST) or evaluation. The testing must occur as instructed below. The employee must provide the results of the TST and/or evaluation on the REQUIRED form: the Employee Annual Tuberculin Skin Test (TST) and Evaluation, CDCR 7336.
DEFINITIONS:
INDURATION: Swelling or raised skin. Note: the presence of erythema is NOT indicative of a TST reaction; only the induration is measured.
MANTOUX TST: Intradermal injection of 0.1 milliliters (ml) of Purified Protein Derivative, 5 Tuberculin Units (TU).
PRIOR TST: A Mantoux TST in which clearly documented and dated results are available in millimeters (mm).
NEGATIVE TST RESULT: Induration of less than (<) 10 mm if new, or < 5 mm, if contact or known immunocompromised.
POSITIVE TST RESULT: Induration equal to or greater than (>) 10 mm, OR > 5 mm if contact or known immunocompromised.
INSTRUCTIONS: EMPLOYEE
1.Complete all of the items in SECTION 1 - All Boxes Must Be Completely Filled In.
•Be sure the information you provide is accurate and complete.
•The health care provider(s) (HCP) administering and evaluating the TST, including the exam for TB signs and
symptoms, must sign and date the appropriate blocks.
•Advise the HCP to follow the steps below when completing SECTION 2 through SECTION 6.
•If a chest
•Submit the completed form (Employee Tuberculin Skin Test (TST) and Evaluation, CDCR 7336), in a sealed envelope, as instructed by your supervisor/TB coordinator.
INSTRUCTIONS: HEALTH CARE PROVIDER - All Boxes Must Be Completely Filled In.
SECTION 2: If prior test TST results are available, the employee or HCP must provide written documentation including the patient’s name, date test was administered, and reaction in mm or IU. Document this in SECTION 2. If documented results are:
•NEGATIVE and more than 30 days old, proceed to Section 3.
•NEGATIVE and less than 30 days old, proceed to Section 4.
•POSITIVE on any date: proceed to Section 4. Must also complete Section 5.
If there are no appropriately documented prior TST or TB blood test results, go to the instructions for Section #3.
SECTION 3: Administer a new TST or TB blood test, and document results in SECTION 3. NOTE: The HCP administering the TST (SECTION 3), and the HCP evaluating the TST (SECTION 6), must sign in the appropriate blocks. If the TST or TB blood test results are:
•NEGATIVE, complete Section 4. Evaluator must sign and date under Section 6.
•POSITIVE, proceed to Section 4. Must also complete Section 5. Evaluator must sign and date under Section 6.
If an individual claims to have a prior positive TB testST, but cannot provide appropriate documentation, a TST or TB blood test must still be administered.
This is not medically contraindicated. However, if there are still questions, although this is not a CDCR procedure, it has been found useful to administer a diluted TST: dilute 0.2 cc of the standard 5 TU/0.1cc solution with 0.8 cc of sterile saline, then use
0.1of this solution to administer a TST. If the results are positive, no further testing is necessary, proceed as directed below for positive TST’s. If the results are negative, proceed with a standard TST.
If the administered or documented TST or TB blood testshows a NEGATIVE result, the employee probably does not have TB infection. Factors affecting the immune system, pregnancy, or recent TB infection may cause a false negative TST or TB blood test reaction, even when TB disease exists, but
CDCR HCPs CANNOT ASK CDCR EMPLOYEES ABOUT NON TB HEALTH HISTORY, INCLUDING
IMMUNOSUPPRESSIVE CONDITIONS
If the TB test TST indicates a POSITIVE reaction, further medical evaluation and a CXR are needed to rule out active TB disease.
STATE OF CALIFORNIADEPARTMENT OF CORRECTIONS AND REHABILITATION
EMPLOYEE TUBERCULIN SKIN TEST (TST) AND EVALUATION
CDCR 7336 (Rev. 07/15)
•Complete SECTIONS 4, 5 AND 6. The HCP evaluating for TB signs and symptoms, must sign and date the form in the space provided at the bottom of the form (SECTION 6).
•Give a copy of the CXR report, if a CXR is taken, to the employee for the CDCR records.
The space identified as “DATE TST READ OR OF SIGNS & SYMPTOMS EXAM” refers to date that the employee’s TB status is determined.
•After evaluation and/or treatment the CDCR 7336 is completed.
•Give the completed CDCR 7336 and the CXR report to the employee.
SECTION 4: Complete evaluation for all employees, regardless of TB testTST result, for TB signs and symptoms; 3 or more positives warrant special concern.
SECTION 5: To be completed for individuals with a documented prior or newly significant TST or TB blood test. Attach copy of CXR report.
SECTION 6: Comments as necessary. Evaluator (Physician and Surgeon or a licensed designee) must sign and date the form.
The Centers for Disease Control and Prevention and the California Tuberculosis Controllers Association recommend the
following:
1.Tine test is NOT an acceptable skin test to determine exposure to the TB bacillus.
2.CXR is an unacceptable screening method for detecting TB infection.
3.The only acceptable screening method(s) for detecting TB infection are TB screening tests that are licensed by the Federal Food and Drug Administration (FDA) and recommended by the Centers for Disease Control (CDC).
4.The process for administering, evaluation, and documenting the Mantoux TST are:
a)Must be given intradermally.
b)0.1 ml (s) of 5 TU Purified Protein Derivative must be used.
c)The test must be interpreted by a qualified HCP.
d)Results must be documented/reported in mm(s) of induration.
DISTRIBUTION: WHITE- HCSD PUBLIC HEALTH SECTION, YELLOW- EMPLOYEE MEDICAL FILE, PINK- EMPLOYEE
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The CDCR 7336 form is used for tuberculosis (TB) screening of employees and cadets within the California Department of Corrections and Rehabilitation (CDCR). |
| Legal Requirement | California Penal Code, Section 6006 et seq., mandates that all CDCR employees undergo initial, annual, and medically necessary TB tests. |
| Administration | The form must be completed by a licensed healthcare provider who is authorized to conduct medical examinations and administer the Mantoux Tuberculin Skin Test (TST). |
| Confidentiality | The form contains confidential medical information about the employee, which must be handled in accordance with privacy laws and regulations. |
| Testing Recommendations | The form follows recommendations set by the Centers for Disease Control and Prevention (CDC) for TB testing and evaluation procedures. |
Guidelines on Utilizing Cdc 7336
Filling out the CDC 7336 form is an important step in your health evaluation process. It requires personal information and assessment by a licensed healthcare provider. After completing this form, it will be reviewed to determine if further action is needed regarding tuberculosis evaluation and management.
- Begin by completing the EMPLOYEE INFORMATION section at the top of the form. Ensure you include your full name as it appears on your state paycheck, gender, birthdate, and personnel number if known.
- Indicate whether you are a new employee or cadet by checking the appropriate box.
- Specify your institution or division along with your unit or branch.
- Sign and date the form in the designated area under your name.
- In the PRIOR TST / TB BLOOD TEST / TB HISTORY section, provide any available documentation regarding prior TB test history. If you have a prior positive result, indicate the date and measure of induration.
- Select the appropriate options in the TST ADMINISTRATION section. Specify whether you received TUBERSOL or APLISOL and complete relevant details, including the injection site.
- Check the appropriate box under EVALUATION FOR SIGNS AND SYMPTOMS to indicate if you are experiencing any symptoms. Mark all that apply.
- If a chest x-ray is necessary, indicate yes and provide the results in SECTION 5. Attach a copy of the chest x-ray report if applicable.
- Fill in any additional comments as needed in the comments section.
- Finally, ensure that the licensed evaluator signs their name, licenses number, and the date in Section 6 of the form.
After submitting the filled-out form, it will be processed, and you will be provided with the results and any necessary follow-up instructions. Ensure that you keep a copy of the form for your records, as it may be needed for future evaluations or documentation.
What You Should Know About This Form
What is the CDCR 7336 form used for?
The CDCR 7336 form serves as a Tuberculin Skin Test (TST) and evaluation record specifically for employees in the California Department of Corrections and Rehabilitation (CDCR). It documents critical medical information regarding tuberculosis (TB) screening, ensuring employees are evaluated and monitored in compliance with public health recommendations. This form helps to identify whether individuals have TB infections or diseases by following the guidelines established by the Centers for Disease Control and Prevention (CDC).
Who is required to complete the CDCR 7336 form?
All CDCR employees, as well as certain other individuals working within the department, are required to complete the CDCR 7336 form. This includes new employees and those undergoing annual evaluations or other medically necessary screenings as mandated by California law (Penal Code Section 6006 et seq.). The form must be filled out by the employee in conjunction with their licensed healthcare provider.
How do employees fill out the form?
Employees must complete Section 1 of the CDCR 7336 form by clearly providing their full name (as shown on their paycheck), gender, birthdate, and any applicable personnel number. It’s crucial that all boxes are filled accurately and completely. The employee must also sign and date the form, ensuring that the healthcare provider responsible for administering the test completes the necessary sections as well.
What happens if an employee has a prior positive TB test?
If an employee has a history of a positive TB test, this should be documented in Section 2 of the form. The healthcare provider will then proceed with necessary evaluations, including a chest X-ray, to rule out active TB disease. Even if the employee cannot provide documentation for the prior positive result, a new TST or TB blood test must be administered to assess the current TB status.
What are the possible results from the TST?
The results from the Tuberculin Skin Test can be categorized as either negative or positive. A negative result indicates an induration of less than 10 mm (or less than 5 mm for immunocompromised individuals), suggesting no TB infection. Conversely, a positive result is characterized by an induration of 10 mm or more (or more than 5 mm for those at higher risk), which necessitates further medical evaluation including potential chest X-rays.
What should employees do if they are experiencing symptoms of TB?
Employees who notice symptoms such as persistent cough, unexplained weight loss, fatigue, fever, or night sweats must report these to their healthcare provider. Section 4 of the CDCR 7336 form is mandatory to document any signs and symptoms, including questions regarding the above indicators. This step is essential in evaluating potential TB infections and ensuring timely follow-up care.
What is the role of the healthcare provider in this process?
The healthcare provider plays a vital role by administering the TST or TB blood test and interpreting the results. They must complete Sections 2 through 6 of the CDCR 7336 form, providing necessary documentation regarding any prior tests, administering the new tests, and evaluating symptoms. The provider is also responsible for signing the form to validate the results and the follow-up actions needed based on the findings.
Is a chest X-ray necessary for all TB tests?
A chest X-ray is not required for every employee taking the TST but is necessary for those who test positive or have a documented prior positive test result. The results of the chest X-ray must be attached to the CDCR 7336 form, providing additional information about the employee’s TB status and ensuring comprehensive evaluation and follow-up if any abnormalities are found.
How is the completed CDCR 7336 form handled after submission?
Once the CDCR 7336 form is completed, it should be placed in a sealed envelope as instructed by the employee’s supervisor or TB coordinator. The form is confidential and includes medical information pertinent to the employee. Proper distribution includes a copy for the employee, a copy for the employee medical file, and submission to the designated health care authority within the department.
Common mistakes
Filling out the CDC 7336 form can be straightforward, but errors can lead to issues with TB screening compliance. One common mistake is failing to provide complete and accurate personal information. It’s essential that the employee's full name is entered exactly as it appears on their state paycheck. If even one letter or number is incorrect, it can cause confusion and delays in processing.
Another frequent error occurs in Section 2, where prior TB test results should be documented. Employees may forget to attach prior test results. Missing documentation can lead to unnecessary tests or complications in the screening process. Always ensure that any previous results are documented correctly and attached as required.
Employees sometimes overlook the importance of signatures. Both the licensed health care provider who administers the test and the one who evaluates the results must sign the appropriate sections of the form. Without these signatures, the form may not be considered valid, and this can result in having to redo tests.
Moreover, some people neglect to check for symptoms. Section 4 requires an evaluation of existing symptoms. If symptoms such as persistent cough or unexplained weight loss are present, they must be checked. Ignoring this part may overlook important health conditions requiring follow-up.
Finally, many individuals forget to include a copy of the chest x-ray report, if applicable. If an employee has positive TB results, they must have a chest x-ray performed, and the report should accompany the CDC 7336 form. Failing to do so may lead to a lack of clarity regarding the TB status and hinder necessary follow-up medical evaluations.
Documents used along the form
The CDC 7336 form is part of the tuberculosis screening process for employees in California's correctional system. Along with this form, several other documents may be required or helpful in ensuring proper documentation and compliance. Here’s a list of some of those forms and documents:
- Employee Health Care Record: This record contains all the health-related documentation for an employee, including past TB tests and other medical history that may impact the screening process.
- Chest X-Ray Report: If a chest x-ray is needed, this report must be attached to the CDC 7336 form. It helps assess whether there are abnormalities that could indicate active TB.
- Prior TB Test Documentation: Any previous TB test results should be included, especially if they show positive reactions. This helps health care providers understand the employee's TB history.
- Tuberculosis Risk Assessment Form: This document evaluates an individual's risk factors related to TB exposure and infection, aiding in deciding the necessity for additional testing.
- Employee Notification of Results: After evaluations are completed, a written notification should be provided to the employee detailing their TB test results.
- Follow-Up Evaluation Records: If additional evaluations are required, records of these follow-ups must be kept to document ongoing assessments and any necessary treatments.
- Informed Consent for Testing: A signed consent form from the employee confirming their understanding and approval of the TB test being administered is important for legal and ethical compliance.
These accompanying documents work together to ensure that TB screenings are conducted thoroughly and correctly. It is vital to keep accurate records for the health and safety of all employees and the populations they may serve.
Similar forms
The CDC 7336 form is related to various other documents used for health screenings and evaluations, particularly concerning tuberculosis. Below is a list of similar documents, along with descriptions highlighting how each serves a comparable purpose:
- CDC 8281: Employee Tuberculosis Risk Assessment - This document is used to assess an employee's risk of tuberculosis exposure. It collects relevant history and environmental factors influencing TB risk, paralleling the aim of the CDC 7336 in evaluating individual TB status.
- CDC 7266: Tuberculosis Screening Questionnaire - This questionnaire gathers symptom-related information from employees, similar to the symptom evaluation section on the CDC 7336 form. It helps determine if further testing is warranted based on reported symptoms.
- CDC 3300: Tuberculosis Exposure Notification Form - Used when an individual has been exposed to TB, this form reminds employees of the importance of screening, just as the CDC 7336 does in organizing follow-up testing.
- Form H22: Tuberculosis Test Results - This document provides formal results of TB tests, thus helping track employee health status. It shares the purpose of the CDC 7336 by documenting individual test outcomes and necessary follow-up actions.
- CDC 6941: Follow-Up Evaluation Report for TB Testing - This report is focused on follow-up assessments for employees who tested positive for TB. It ensures continuity in care, aligning with the follow-up evaluation steps included in the CDC 7336.
- State Health Department TB Screening Template - Many states use templates for TB screening that fulfill similar functions to the CDC 7336. They guide the screening process and documentation, ensuring thorough evaluations of tuberculosis status.
Each of these documents aims to ensure personnel safety regarding tuberculosis, streamlining the process of screening, documenting, and following up on TB-related health concerns.
Dos and Don'ts
When filling out the CDC 7336 form for the Employee Tuberculin Skin Test (TST) and evaluation, it is essential to follow certain guidelines to ensure accuracy and compliance. Below is a list of dos and don'ts that can assist in this process.
- Do complete all items in Section 1 completely, ensuring no field is left blank.
- Do provide accurate and complete information, as this affects your health record.
- Do ensure the health care provider signs and dates the appropriate sections of the form.
- Do submit the completed form in a sealed envelope to maintain confidentiality.
- Don't write any information in areas that are not designated for employee input.
- Don't forget to attach documentation for any prior TB test results or chest x-ray reports when applicable.
- Don't assume your test results from a previous provider are acceptable without proper documentation.
- Don't leave any symptoms unchecked in Section 4; all must be acknowledged.
Misconceptions
Many people have misconceptions about the CDC 7336 form, which is used for Tuberculosis (TB) screening for employees of the California Department of Corrections and Rehabilitation. Let's clarify some of these misunderstandings.
- Misconception 1: The CDC 7336 form is only for new employees.
- Misconception 2: A positive TB test automatically means an employee has active TB.
- Misconception 3: Only the initial test needs to be documented.
- Misconception 4: The CDC 7336 form can be filled out by anyone.
This is not true. The form is required for all employees, including current staff who need annual screenings or evaluations as medically necessary. It's important that all employees maintain up-to-date health records.
In reality, a positive test result indicates exposure to the TB bacteria, but not necessarily that the individual has active TB disease. Further medical evaluation is needed to determine the true status.
This is a common error. A complete history including prior tests, results, and any relevant medical evaluations must be documented in the form. This ensures a comprehensive understanding of the employee’s TB status over time.
It can only be completed by a licensed healthcare provider. This is crucial since only qualified professionals can appropriately assess TB risk and interpret test results.
Key takeaways
Using the CDC 7336 form requires attention to detail and adherence to specific instructions. Below are key takeaways regarding its use:
- Complete Employee Information: Ensure all sections are accurately filled in, including the employee's full name, gender, birthdate, and personnel number.
- Prior History Documentation: If there is prior TB testing, include documented results in Section 2.
- TST Administration: The health care provider must administer the TST or TB blood test as per the defined protocol and record the results.
- Induration Measurements: Only the induration (swelling) is significant for TB test results, not the presence of redness or erythema.
- Chest X-ray Requirement: If the test results are positive, a chest x-ray is necessary to rule out active TB disease.
- Follow-up Evaluation: Evaluation for signs and symptoms of TB is required for all individuals, regardless of test results.
- Submission Procedure: The completed form must be submitted in a sealed envelope, as instructed by the supervisor.
- Interpreter Requirement: A qualified health care provider must interpret the TST results, and their signature is required.
- Confidentiality Maintenance: This form contains confidential employee medical information and must be handled accordingly.
Browse Other Templates
California Repo Affidavit - All signatures on the affidavit must be authentic to validate the document.
Ku Official Transcript - Transcripts requested before Fall 1983 may require additional processing time.