Fill Out Your Certificate Necessity Form
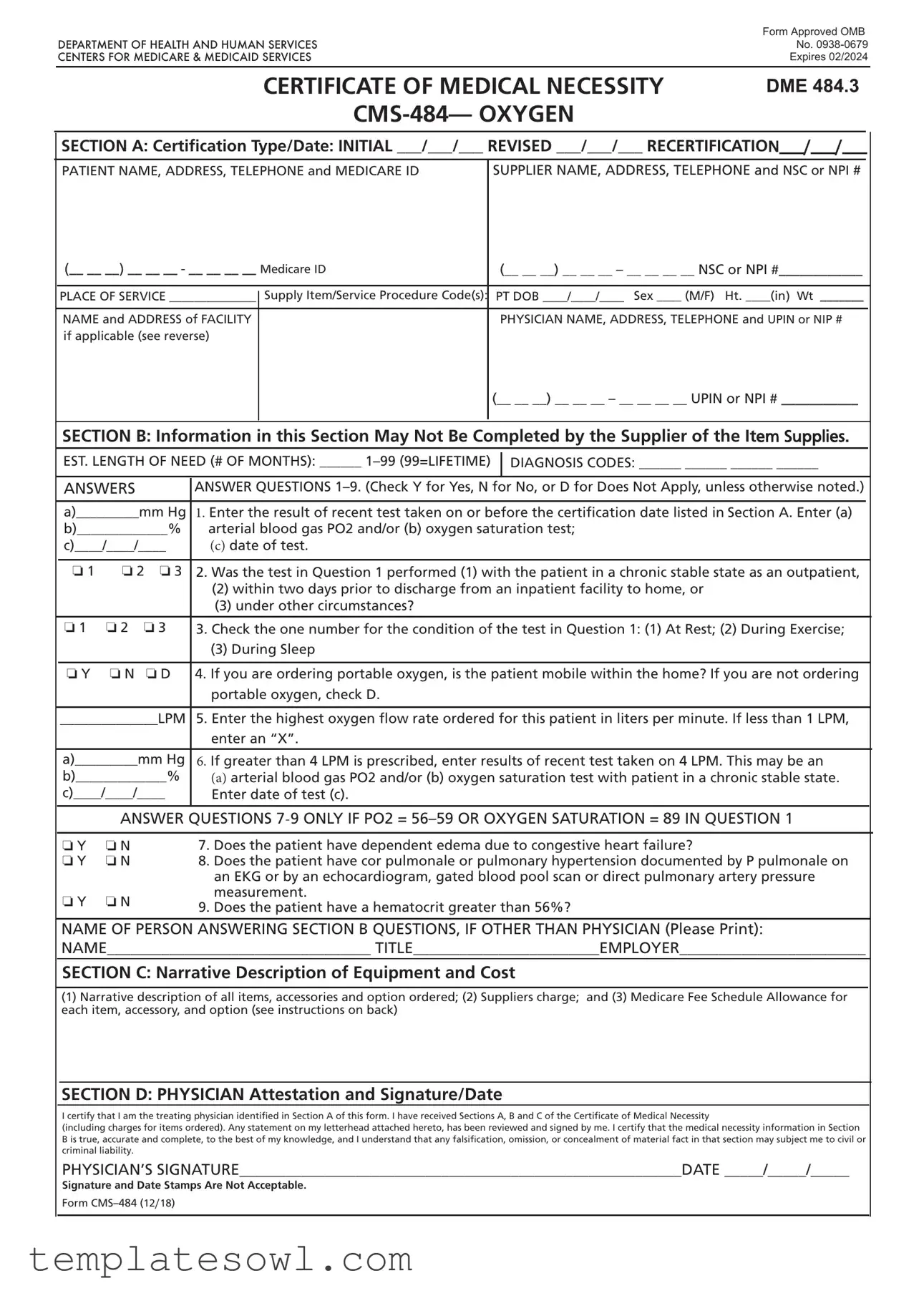
The Certificate of Medical Necessity (CMN), specifically Form CMS-484, is a critical document utilized within the Medicare system for oxygen-related durable medical equipment (DME). This form is intended to substantiate the medical necessity for oxygen therapy by collecting detailed patient and supplier information. It includes sections that require patient demographics, medical diagnosis codes, and estimates of how long the patient will need the equipment. It also features questions that help healthcare providers clarify the patient’s condition and the urgency of the need for oxygen support. The form demands physician certification, confirming that the ordered items are indeed necessary based on thorough medical assessments and tests. Completing the CMN correctly is essential not only to ensure patients receive the needed supplies but also to facilitate the reimbursement process from Medicare. The precise information required, including the patient's test results and the physician's signature, underscores the importance of accuracy in supporting patient care and compliance with Medicare's guidelines.
Certificate Necessity Example
|
Form Approved OMB |
DEPARTMENT OF HEALTH AND HUMAN SERVICES |
No. |
CENTERS FOR MEDICARE & MEDICAID SERVICES |
Expires 02/2024 |
CERTIFICATE OF MEDICAL NECESSITY
DME 484.3
SECTION A: Certifcation Type/Date: INITIAL ___/___/___ REVISED ___/___/___ RECERTIFICATION___/___/___
PATIENT NAME, ADDRESS, TELEPHONE and MEDICARE ID |
SUPPLIER NAME, ADDRESS, TELEPHONE and NSC or NPI # |
|
(__ __ __) __ __ __ - __ __ __ __ Medicare ID |
(__ __ __) __ __ __ – __ __ __ __ NSC or NPI #____________ |
|
||
|
|
|
|
|
|
|
PLACE OF SERVICE ______________ |
|
Supply Item/Service Procedure Code(s): |
PT DOB ____/____/____ Sex ____ (M/F) Ht. ____(in) Wt _______ |
|
|
|
||||
|
|
|
|
|
|
|
NAME and ADDRESS of FACILITY |
|
|
PHYSICIAN NAME, ADDRESS, TELEPHONE and UPIN or NIP # |
|
|
if applicable (see reverse) |
|
|
|
|
|
|
|
|
(__ __ __) __ __ __ – __ __ __ __ UPIN or NPI # ___________ |
|
|
|
|
|
|
|
SECTION B: Information in this Section May Not Be Completed by the Supplier of the Item Supplies.
EST. LENGTH OF NEED (# OF MONTHS): ______
DIAGNOSIS CODES: ______ ______ ______ ______
|
ANSWERS |
|
ANSWER QUESTIONS |
|
|
|
a)_________mm Hg |
1. Enter the result of recent test taken on or before the certifcation date listed in Section A. Enter (a) |
|||
|
b)_____________% |
arterial blood gas PO2 and/or (b) oxygen saturation test; |
|||
|
c)____/____/____ |
(c) date of test. |
|||
|
|
|
|
|
|
|
o 1 |
o 2 o 3 |
2. Was the test in Question 1 performed (1) with the patient in a chronic stable state as an outpatient, |
||
|
|
|
|
(2) within two days prior to discharge from an inpatient facility to home, or |
|
|
|
|
|
(3) under other circumstances? |
|
|
|
|
|
|
|
|
o 1 |
o 2 |
o 3 |
3. Check the one number for the condition of the test in Question 1: (1) At Rest; (2) During Exercise; |
|
|
|
|
|
(3) During Sleep |
|
|
|
|
|
|
|
|
o Y |
o N |
o D |
4. If you are ordering portable oxygen, is the patient mobile within the home? If you are not ordering |
|
|
|
|
|
portable oxygen, check D. |
|
|
|
|
|
||
|
______________LPM |
5. Enter the highest oxygen fow rate ordered for this patient in liters per minute. If less than 1 LPM, |
|||
|
|
|
|
enter an “X”. |
|
|
|
|
|
||
|
a)_________mm Hg |
6. If greater than 4 LPM is prescribed, enter results of recent test taken on 4 LPM. This may be an |
|||
|
b)_____________% |
(a) arterial blood gas PO2 and/or (b) oxygen saturation test with patient in a chronic stable state. |
|||
|
c)____/____/____ |
Enter date of test (c). |
|||
|
|
|
|
|
|
ANSWER QUESTIONS
o Y |
o N |
o Y |
o N |
o Y |
o N |
7.Does the patient have dependent edema due to congestive heart failure?
8.Does the patient have cor pulmonale or pulmonary hypertension documented by P pulmonale on an EKG or by an echocardiogram, gated blood pool scan or direct pulmonary artery pressure measurement.
9.Does the patient have a hematocrit greater than 56%?
NAME OF PERSON ANSWERING SECTION B QUESTIONS, IF OTHER THAN PHYSICIAN (Please Print):
NAME__________________________________ TITLE________________________EMPLOYER________________________
SECTION C: Narrative Description of Equipment and Cost
(1)Narrative description of all items, accessories and option ordered; (2) Suppliers charge; and (3) Medicare Fee Schedule Allowance for each item, accessory, and option (see instructions on back)
SECTION D: PHYSICIAN Attestation and Signature/Date
I certify that I am the treating physician identifed in Section A of this form. I have received Sections A, B and C of the Certifcate of Medical Necessity
(including charges for items ordered). Any statement on my letterhead attached hereto, has been reviewed and signed by me. I certify that the medical necessity information in Section B is true, accurate and complete, to the best of my knowledge, and I understand that any falsifcation, omission, or concealment of material fact in that section may subject me to civil or criminal liability.
PHYSICIAN’S SIGNATURE_________________________________________________________DATE _____/_____/_____
Signature and Date Stamps Are Not Acceptable.
Form

INSTRuCTIONS FOR COMPLETING THE CERTIFICATE OF MEDICAL NECESSITY
FOR OXYGEN
SECTION A:
CERTIFICATION DATE:
(May be completed by the supplier)
If this is an initial certification for this patient, indicate this by placing date (MM/DD/YY) needed initially in the space TYPE/ marked “INITIAL.” If this is a revised certification (to be completed when the physician changes the order, based on the patient’s changing clinical needs), indicate the initial date needed in the space marked “INITIAL,” and indicate the recertification date in the space marked “REVISED.” If this is a recertification, indicate the initial date needed in the space marked “INITIAL,” and indicate the recertification date in the space marked “RECERTIFICATION.” Whether submitting a REVISED or a RECERTIFIED CMN, be sure to always furnish the INITIAL date as well as the REVISED or RECERTIFICATION date.
PATIENT |
Indicate the patient’s name, permanent legal address, telephone number and his/her Medicare ID as it appears on his/her |
|
INFORMATION: |
Medicare card and on the claim form. |
|
|
||
SUPPLIER |
Indicate the name of your company (supplier name), address and telephone number along with the Medicare Supplier Number |
|
assigned to you by the National Supplier Clearinghouse (NSC) or applicable National Provider Identifier (NPI). If using the NPI |
||
INFORMATION: |
||
Number, indicate this by using the qualifier XX followed by the |
||
|
||
|
e.g. NSC number, use the qualifier 1C followed by the |
PLACE OF SERVICE:
FACILITY NAME:
SUPPLY ITEM/SERVICE PROCEDURE CODE(S):
PATIENT DOB, HEIGHT, WEIGHT AND SEX:
PHYSICIAN NAME, ADDRESS:
PHYSICIAN INFORMATION:
PHYSICIAN’S
TELEPHONE NO:
SECTION B:
EST. LENGTH OF NEED:
DIAGNOSIS CODES:
QUESTION SECTION:
NAME OF PERSON ANSWERING SECTION B QUESTIONS:
SECTION C:
NARRATIVE DESCRIPTION OF EQUIPMENT & COST:
SECTION D: PHYSICIAN
ATTESTATION:
PHYSICIAN SIGNATURE AND DATE:
Indicate the place in which the item is being used, i.e., patient’s home is 12, skilled nursing facility (SNF) is 31, End Stage Renal Disease (ESRD) facility is 65, etc.
If the place of service is a facility, indicate the name and complete address of the facility.
List all procedure codes for items ordered. Procedure codes that do not require certification should not be listed on the CMN.
Indicate patient’s date of birth (MM/DD/YY) and sex (male or female); height in inches and weight in pounds, if requested.
Indicate the PHYSICIAN’S name and complete mailing address.
Accurately indicate the treating physician’s Unique Physician Identification Number (UPIN) or applicable National Provider Identifier (NPI). If using the NPI Number, indicate this by using the qualifier XX followed by the
Indicate the telephone number where the physician can be contacted (preferably where records would be accessible pertaining to this patient) if more information is needed.
(May not be completed by the supplier. While this section may be completed by a
Indicate the estimated length of need (the length of time the physician expects the patient to require use of the ordered item) by filling in the appropriate number of months. If the patient will require the item for the duration of his/her life, then enter “99”.
In the first space, list the diagnosis code that represents the primary reason for ordering this item. List any additional diagnosis codes that would further describe the medical need for the item (up to 4 codes).
This section is used to gather clinical information to help Medicare determine the medical necessity for the item(s) being ordered. Answer each question which applies to the items ordered, checking “Y” for yes, “N” for no, or “D” for does not apply.
If a clinical professional other than the treating physician (e.g., home health nurse, physical therapist, dietician) or a physician employee answers the questions of Section B, he/she must print his/her name, give his/her professional title and the name of his/ her employer where indicated. If the physician is answering the questions, this space may be left blank.
(To be completed by the supplier)
Supplier gives (1) a narrative description of the item(s) ordered, as well as all options, accessories, supplies and drugs;
(2)the supplier’s charge for each item(s), options, accessories, supplies and drugs; and (3) the Medicare fee schedule allowance for each item(s), options, accessories, supplies and drugs, if applicable.
(To be completed by the physician)
The physician’s signature certifies (1) the CMN which he/she is reviewing includes Sections A, B, C and D; (2) the answers in Section B are correct; and (3) the
After completion and/or review by the physician of Sections A, B and C, the physician’s must sign and date the CMN in Section D, verifying the Attestation appearing in this Section. The physician’s signature also certifies the items ordered are medically necessary for this patient.
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is
DO NOT SuBMIT CLAIMS TO THIS ADDRESS. Please see http://www.medicare.gov/ for information on claim filing.
Form
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Certificate of Medical Necessity (CMN) form, specifically CMS-484, is used to justify the medical necessity for oxygen therapy and related supplies for Medicare beneficiaries. |
| Components | This form includes several sections: patient information, certification details, medical evaluation, and physician attestation. |
| Expiration Date | The current version of the CMS-484 form expires in February 2024, requiring updates after this date to ensure compliance. |
| Length of Need | Suppliers must indicate the estimated length of need for the medical equipment, which can range from 1 month to a lifetime (99 months). |
| Physician Signature | A physician's signature is mandatory for the completion of this form, certifying the accuracy and necessity of the information provided. |
| State Requirements | The governing laws for CMNs can vary by state, and practitioners should be aware of specific regulations and requirements for their state, such as health service regulations in California or Florida. |
| Submission Instructions | Completed forms should not be sent to the address listed for feedback. Instead, they should be submitted through the established Medicare claims process. |
Guidelines on Utilizing Certificate Necessity
Completing the Certificate of Medical Necessity (CMN) form is essential for ensuring that patients receive the necessary equipment and treatment. Follow the instructions below carefully to fill out the form accurately. Mistakes can delay the approval process, so attention to detail is crucial.
- Indicate the type and date of certification in Section A. Choose from Initial, Revised, or Recertification, and provide the corresponding date.
- Enter the patient’s full name, address, telephone number, and Medicare ID as it appears on the Medicare card.
- Provide the supplier’s name, address, telephone number, and either the National Supplier Clearinghouse (NSC) number or National Provider Identifier (NPI) number.
- Fill in the place of service and supply item/service procedure code(s).
- Record the patient’s date of birth, height, weight, and sex.
- List the physician’s name, address, telephone number, and their UPIN or NPI number.
- In Section B, enter the estimated length of need in months, choosing from 1-99, with 99 indicating lifetime use.
- Fill in the diagnosis codes relevant to the patient’s condition (up to four codes).
- Answer questions 1 to 9 with “Y” for Yes, “N” for No, or “D” for Does Not Apply, as appropriate.
- Include the name of the person answering Section B if it is not the physician, along with their title and employer.
- In Section C, provide a narrative description of the items ordered, including the supplier’s charge and Medicare fee schedule allowance.
- In Section D, the physician must sign and date the form, certifying the information provided is true and complete.
After completing the form, ensure all sections are reviewed for accuracy. The physician's signature is critical to validate the medical necessity of the items ordered, which is necessary for proper claims processing. Be diligent, as timely submissions can influence patient care outcomes significantly.
What You Should Know About This Form
What is a Certificate of Medical Necessity (CMN) and why is it required?
A Certificate of Medical Necessity (CMN) is a form used primarily in the context of Medicare to demonstrate that specific medical equipment or services are required for a patient's treatment. It provides crucial documentation that the prescribed items, such as oxygen therapy, are medically necessary based on the patient’s conditions. This form helps ensure that both healthcare providers and suppliers meet Medicare’s requirements for reimbursement.
Who completes the Certificate of Medical Necessity?
The CMN must be completed by an authorized healthcare provider, typically the treating physician. The physician needs to provide their information, sign the form, and confirm that the medical necessity information is accurate. Certain sections, particularly related to the patient's diagnosis and medical details, may be filled out by non-physician clinicians, but they must be reviewed and verified by the physician before submission.
What information is included in the CMN?
The CMN contains several sections that collect critical information. This includes patient details such as name, address, and Medicare ID; supplier details; certification type and date; a section for medical information related to the patient's condition; and a narrative description of the equipment or supplies needed along with associated costs. Proper completion requires attention to detail to ensure that all necessary data is accurately reported for Medicare to process claims.
When should a new CMN be submitted?
New CMNs should be submitted in several scenarios: when starting a new treatment requiring equipment (initial certification), when there are significant changes to an existing order (revised certification), or when the physician reassesses the patient and determines ongoing eligibility for continued equipment use (recertification). It is important to update the CMN as patient's needs or conditions change to ensure proper coverage under Medicare.
Common mistakes
When filling out the Certificate of Medical Necessity (CMN), many individuals encounter various pitfalls that can delay or jeopardize the approval process. Here are nine common mistakes that can occur during this important task.
Firstly, one prevalent error is neglecting to fill in the Certification Type and Date. It is essential to indicate whether the form is for an initial certification, a revised one, or a recertification. Omitting this crucial information can lead to confusion about the patient’s current status and requirements.
Secondly, incorrect or incomplete patient information can create significant issues. Ensure that the patient's name, address, telephone number, and Medicare ID are entered accurately. Any discrepancies might result in the denial of the claim or additional unnecessary complications.
Another common mistake is failing to provide the facility name and place of service. It is vital to indicate where the equipment will be used, such as the patient's home or another medical facility. This information helps contextualize the necessity of the oxygen equipment.
Moreover, some individuals may overlook the length of need. Accurately estimating how long the patient will require the oxygen equipment is critical. Entering the correct number of months helps in determining the medical necessity and appropriateness of the item.
Section B of the form, which contains clinical information, is often mishandled. Respondents might skip questions or provide unclear answers. It is important to answer each question thoroughly, choosing 'Y' for yes, 'N' for no, or 'D' for does not apply, to ensure a complete profile of the patient’s condition.
In addition, misunderstanding or misrepresenting the results of recently conducted tests can lead to faulty conclusions regarding medical necessity. The test results must be accurately documented, including the date and specific metrics, to support the need for oxygen therapy.
Furthermore, forgetting to include the name and credentials of the individual answering Section B questions can lead to delays. If a professional other than the physician completes this section, their qualifications must be clearly identified to uphold the integrity of the information provided.
Finally, signatures should not be overlooked. Only the physician is authorized to sign Section D, and the use of date stamps is not acceptable. A valid signature confirms the physician's attestation regarding the medical necessity of the items ordered.
In summary, avoiding these nine errors can lead to smoother processing of the Certificate of Medical Necessity. Patients deserve prompt and efficient care, so taking the time to carefully complete this form is a small yet crucial step in that direction.
Documents used along the form
The Certificate of Medical Necessity form is a critical document in the healthcare process, especially for obtaining necessary medical equipment. While the CMN form is vital on its own, there are other documents and forms often used alongside it to support the approval and fulfillment of medical needs. Below is a brief overview of six essential forms that can work in tandem with the Certificate of Medical Necessity.
- Prescription Order Form: This document is a directive from a healthcare provider, detailing specific medications or treatments a patient should receive. It often accompanies the CMN to ensure that prescribed items are both requested and justified medically.
- Patient Intake Form: Collected from the patient at the start of care, this form gathers crucial information, including medical history, insurance details, and contact information. It helps healthcare providers develop a comprehensive care plan and is often referenced during the CMN process.
- Prior Authorization Request: Insurance companies often require this form to assess the medical necessity of treatments or equipment before coverage is granted. Completing this form accurately can streamline the approval process for items listed in the CMN.
- Detailed Medical History Form: This extensive document outlines a patient's medical background, past treatments, and relevant health conditions. It provides context for the medical necessity outlined in the CMN and supports the need for specific equipment or services.
- Clinical Evaluation Form: Used by medical professionals to document physical examinations and assessments related to the patient's condition, this form complements the CMN by providing objective evidence of medical necessity.
- Equipment Specification Sheet: This document lists the specifications and features of the medical equipment requested. It serves to further clarify the specific needs outlined in the CMN and ensures that the equipment provided aligns with the patient's medical requirements.
Incorporating these additional documents can enhance the clarity and effectiveness of the Certificate of Medical Necessity process. Together, they create a robust framework that helps healthcare providers, patients, and insurance companies navigate the complexities of medical equipment approvals with confidence.
Similar forms
Prior Authorization Request (PAR): Similar to the Certificate Necessity form, the PAR is required to confirm that a service or item is medically necessary before treatment or delivery takes place.
Durable Medical Equipment (DME) Modifiers: DME modifiers provide additional information regarding the patient's needs or the specific type of equipment required, paralleling the detailed information found in the Certificate Necessity form.
Medical Necessity Checklist: This document lists criteria that must be met for a treatment or service to be considered necessary, mirroring the questions in Section B of the Certificate Necessity form.
Letter of Medical Necessity (LMN): An LMN is an official communication from a healthcare provider confirming the need for a specific treatment or service, reflecting the attestation aspect of the Certificate Necessity form.
CMS 1490S - Medicare Secondary Payer Questionnaire: This form collects information regarding other insurance coverage and is similar in that it validates eligibility and necessity of services rendered.
Patient Referral Form: This document facilitates coordination of care between providers and includes information on patient needs, akin to the details required in the Certificate Necessity form.
Claim Form (CMS 1500): The claim form documents services rendered and payment requested, paralleling the necessary documentation processes found in the Certificate Necessity form.
Diagnostic Test Orders: Ordering diagnostic tests requires specific input on patient conditions and necessity, similar in nature to the information captured in the Certificate Necessity form.
Home Health Certification Evidence: This document certifies the need for home health services, aligning closely with the goals of establishing medical necessity found in the Certificate Necessity form.
Clinical Documentation Requirements (CDR): CDR guidelines specify what information must be included to support medical necessity for billing, mirroring aspects of the Certificate Necessity form.
Dos and Don'ts
When filling out the Certificate of Medical Necessity form, it is essential to follow certain guidelines to ensure that your submission is accurate and complete. Here is a list of what to do and what to avoid:
- DO: Clearly indicate the type of certification by selecting "INITIAL," "REVISED," or "RECERTIFICATION." Include the corresponding dates.
- DO: Provide the patient's name, address, telephone number, and Medicare ID exactly as they appear on the Medicare card.
- DO: Make sure to complete Section B with accurate information about the patient's condition and medical needs.
- DO: Review the form carefully for accuracy before submission to avoid delays.
- DO: Have the attending physician sign and date the document in Section D to certify the medical necessity.
- DON'T: Skip any required sections. Each part of the form plays a crucial role in conveying information.
- DON'T: Use stamps for signatures. The physician's handwritten signature is mandatory for the certification to be valid.
- DON'T: Include irrelevant procedure codes that do not require certification. Only list those pertinent to the medical necessity claim.
Keeping these points in mind will help ensure that the Certificate of Medical Necessity is filled out correctly and processed in a timely manner.
Misconceptions
Misconceptions about the Certificate of Medical Necessity (CMN) can lead to confusion regarding its use and requirements. Below are seven common misconceptions, clarified to help ensure accurate understanding.
- The CMN is only required for certain patients. In reality, the CMN is necessary whenever a physician prescribes durable medical equipment (DME) for Medicare beneficiaries; it isn't limited to specific conditions.
- Only physicians can complete the form. While the treating physician must sign the CMN, healthcare professionals such as nurse practitioners or physician assistants can assist in providing information—as long as the physician reviews and signs the final document.
- The CMN must be completed in its entirety by the supplier. This is a misconception. Sections A, C, and D can involve contributions from both the supplier and the physician, but Section B must be answered by the physician or a qualified professional under their supervision.
- The date of the test is not critical. Contrary to this belief, providing the date of the relevant medical tests is essential. Tests should be conducted within a specific timeframe relative to the certification date to ensure their applicability.
- Suppliers can just fill out everything on the form. This is not correct. Suppliers cannot complete Section B, which requires clinical information. That section must be filled out by a qualified healthcare provider.
- All answers in Section B must be “Yes.” It is inaccurate to assume that all responses should affirm medical necessity. Each answer should reflect the patient's specific situation, allowing for "No" or "Does Not Apply" responses.
- A CMN is sufficient for all claims without further documentation. This is misleading. While necessary, the CMN may require supporting documentation, such as detailed patient records, to substantiate the claims for DME reimbursement adequately.
Understanding these misconceptions can significantly reduce administrative errors and improve the quality of patient care delivered through Medicare services.
Key takeaways
Here are some key takeaways about filling out and using the Certificate Necessity form:
- Certification Type: Clearly indicate whether it's an initial, revised, or recertification in Section A. This ensures proper processing of the request.
- Patient Information: Accurate patient details including name, address, and Medicare ID are essential. Any errors can lead to delays in service.
- Supplier Information: Include the supplier’s name, address, and NSC or NPI number. This identifies who is providing the items or services.
- Length of Need: Specify the estimated duration for which the patient will need the service or item. This helps Medicare evaluate the medical necessity.
- Relevant Tests: Ensure that the results of recent tests are documented in Section B. These results should be from tests taken close to the certification date.
- Answers to Questions: Complete all applicable questions (1-9) in Section B with accurate indications. This information is critical for supporting the medical necessity of the request.
- Physician Signature: The physician must sign and date the form in Section D. This confirms that the information provided is complete and accurate.
Browse Other Templates
Change Llc Name Missouri - This form is essential when adding officers to your business account.
Fan Chart - Each section of the form represents a different branch of your ancestry.
Merrill Lynch 401k Withdrawal Form - Trustees must provide accurate and honest information to mitigate future disputes.