Fill Out Your Dab 101 Form
The DAB 101 form serves a crucial purpose within the Medicare system, allowing individuals to formally challenge decisions made by Administrative Law Judges (ALJs) regarding their Medicare claims. This form, officially titled "Request for Review of Administrative Law Judge Medicare Decision/Dismissal," requires specific information to initiate the appeal process. Appellants must provide details such as their name, the relevant ALJ appeal number, and the health insurance claim number associated with the disputed claims. Furthermore, the form outlines necessary fields for identifying providers, practitioners, or suppliers involved in the issue at hand. It also highlights essential choices regarding the type of Medicare claim—be it Part A, B, C, or D—and whether the request involves services not yet furnished. Another critical aspect of the DAB 101 is the opportunity to request expedited review if the situation threatens the beneficiary's health or well-being. Completing the form correctly is vital, as it sets the foundation for a timely and effective appeal process. Additionally, the form also requires a declaration of disagreement with the ALJ's decision and invites attachable evidence supporting the appellant's claims. Those intending to submit this form should be aware of the strict 60-day deadline for submission, alongside the importance of notifying other involved parties. Thus, understanding the DAB 101 form is essential for any beneficiary or provider navigating the complexities of Medicare appeals.
Dab 101 Example
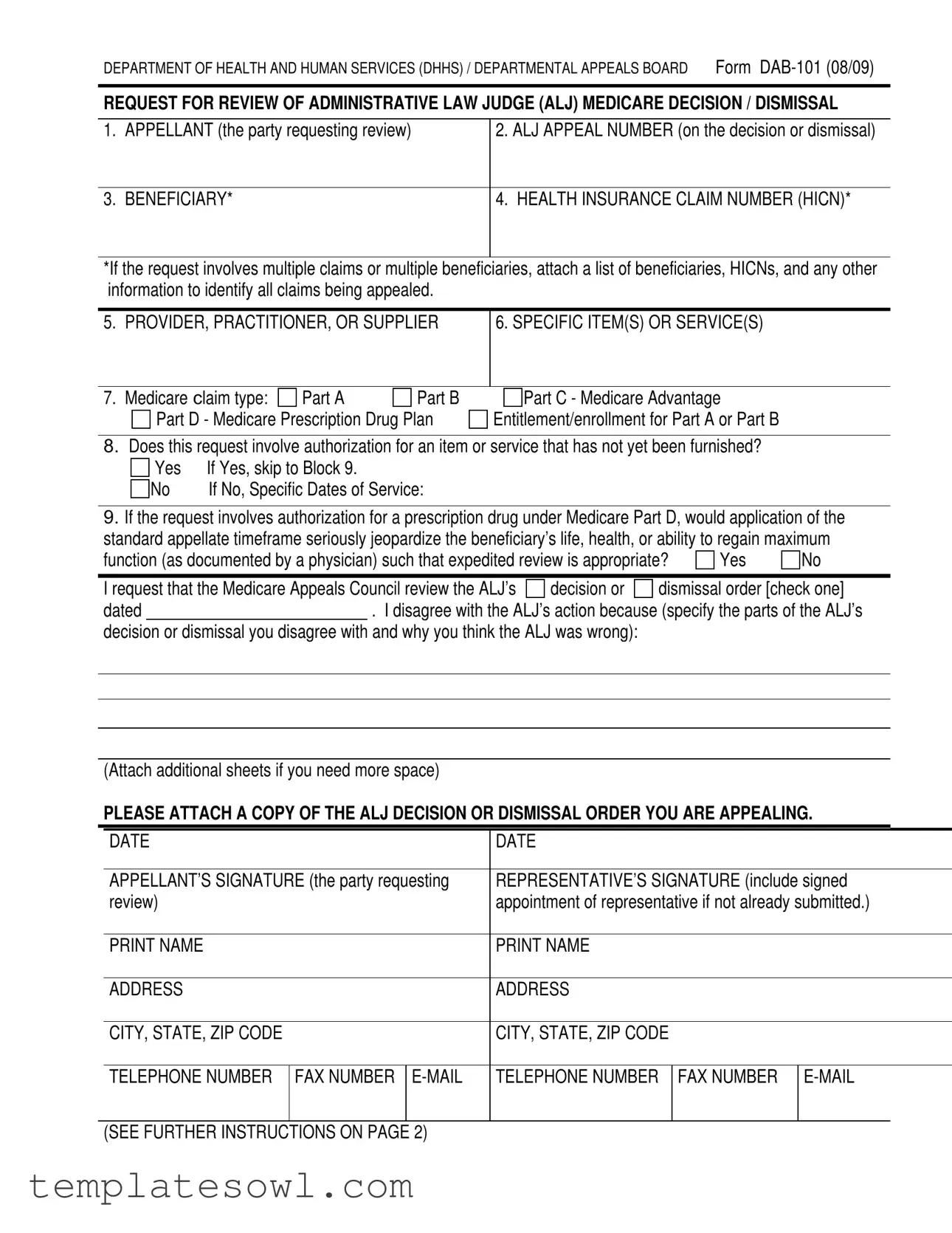
DEPARTMENT OF HEALTH AND HUMAN SERVICES (DHHS) / DEPARTMENTAL APPEALS BOARD Form
REQUEST FOR REVIEW OF ADMINISTRATIVE LAW JUDGE (ALJ) MEDICARE DECISION / DISMISSAL
1. APPELLANT (the party requesting review)
2. ALJ APPEAL NUMBER (on the decision or dismissal)
3. BENEFICIARY*
4. HEALTH INSURANCE CLAIM NUMBER (HICN)*
*If the request involves multiple claims or multiple beneficiaries, attach a list of beneficiaries, HICNs, and any other information to identify all claims being appealed.
5. PROVIDER, PRACTITIONER, OR SUPPLIER
6. SPECIFIC ITEM(S) OR SERVICE(S)
7. Medicare Claim type: |
Part A |
Part B |
Part D - Medicare Prescription Drug Plan

 Part C - Medicare Advantage Entitlement/enrollment for Part A or Part B
Part C - Medicare Advantage Entitlement/enrollment for Part A or Part B
8.Does this request involve authorization for an item or service that has not yet been furnished?
Yes |
If Yes, skip to Block 9. |
No |
If No, Specific Dates of Service: |
9.If the request involves authorization for a prescription drug under Medicare Part D, would application of the standard appellate timeframe seriously jeopardize the beneficiary’s life, health, or ability to regain maximum
function (as documented by a physician) such that expedited review is appropriate? |
Yes |
No |
||||
|
|
|
||||
I request that the Medicare Appeals Council review the ALJ’s |
decision or |
dismissal order [check one] |
||||
dated |
|
. I disagree with the ALJ’s action because (specify the parts of the ALJ’s |
||||
decision or dismissal you disagree with and why you think the ALJ was wrong):
(Attach additional sheets if you need more space)
PLEASE ATTACH A COPY OF THE ALJ DECISION OR DISMISSAL ORDER YOU ARE APPEALING.
|
DATE |
DATE |
|||||
|
|
|
|
|
|
|
|
|
APPELLANT’S SIGNATURE (the party requesting |
REPRESENTATIVE’S SIGNATURE (include signed |
|||||
|
review) |
appointment of representative if not already submitted.) |
|||||
|
|
|
|
|
|
|
|
|
PRINT NAME |
PRINT NAME |
|||||
|
|
|
|
|
|
|
|
|
ADDRESS |
ADDRESS |
|||||
|
|
|
|
|
|
|
|
|
CITY, STATE, ZIP CODE |
CITY, STATE, ZIP CODE |
|||||
|
|
|
|
|
|
|
|
|
TELEPHONE NUMBER |
FAX NUMBER |
TELEPHONE NUMBER |
FAX NUMBER |
|||
|
|
|
|
|
|
|
|
|
(SEE FURTHER INSTRUCTIONS ON PAGE 2) |
|
|
|
|
||
Form
If you have additional evidence, submit it with this request for review. If you need more time, you must request an extension of time in writing now, explaining why you are unable to submit the evidence or legal argument now.
If you are a provider, supplier, or a beneficiary represented by a provider or supplier, and your case was reconsidered by a Qualified Independent Contractor (QIC), the Medicare Appeals Council will not consider new evidence related to issues the QIC has already considered unless you show that you have a
good reason for submitting it for the first time to the Medicare Appeals Council.
IMPORTANT: Include the HICN and ALJ Appeal Number on any letter or other material you submit.
This request must be received within 60 calendar days after you receive the ALJ’s decision or dismissal, unless we extend the time limit for good cause. We assume you received the decision or dismissal 5 calendar days after it was issued, unless you show you received it later. If this request will not be received within
65 calendar days from the date on the decision or dismissal order, please explain why on a separate sheet.
You must file your request for review in writing with the Medicare Appeals Council at:
Department of Health and Human Services
Departmental Appeals Board
Medicare Appeals Council, MS 6127
Cohen Building Room
330 Independence Ave., S.W.
Washington, D.C. 20201
You may send the request for review by U.S. Mail, a common carrier such as FedEx, or by fax to (202)
If you have any questions about your request for review or wish to request expedited review of a claim involving authorization of your prescription drug under Medicare Part D, you may call the Medicare Appeals Council’s staff in the Medicare Operations Division of the Departmental Appeals Board at (202)
PRIVACY ACT STATEMENT
The collection of information on this form is authorized by the Social Security Act (section 205(a) of title II, section 702 of title VII, section 1155 of Title XI, and sections 1852(g)(5), 1869(b)(1), 1871, 1872, and 1876(c)(5)(B) of title XVIII, as appropriate). The information provided will be used to further document your claim. Information requested on this form is voluntary, but failure to provide all or any part of the requested information may affect the determination of your claim. Information you furnish on this form may be disclosed by the Department of Health and Human Services or the Social Security Administration to another person or governmental agency only with respect to programs under the Social Security Act and to comply with Federal laws requiring the disclosure of information or the exchange of information between the Department of Health and Human Services, the Social Security Administration, or other agencies.
Form Characteristics
| Fact Name | Detail |
|---|---|
| Form Purpose | The DAB-101 form is used to request a review of an administrative law judge (ALJ) decision or dismissal regarding Medicare claims. |
| Submission Deadline | Requests must be submitted within 60 calendar days after receiving the ALJ's decision, with a presumption of receipt five days after issuance. |
| Additional Evidence | If you have more evidence, include it with the submission. New evidence will not be accepted unless a valid reason is provided. |
| Governing Laws | Applies to provisions under the Social Security Act including sections 205(a), 702, 1155, and various sections of title XVIII. |
| Communication Method | Requests can be sent via U.S. Mail, common carrier, or by fax. If faxed, do not mail a copy. |
| Beneficiary Involvement | If the request involves multiple beneficiaries, attach a list identifying them and their corresponding Health Insurance Claim Numbers (HICNs). |
Guidelines on Utilizing Dab 101
Completing the DAB 101 form involves several key steps. This form is used to request a review of a decision made by an Administrative Law Judge regarding Medicare. Make sure to gather all necessary information before starting to fill it out. Follow the instructions carefully to ensure your submission is complete and accurate.
- Begin with the APPELLANT section. Enter the name of the person or entity requesting the review.
- Next, fill in the ALJ APPEAL NUMBER, which can be found on the decision or dismissal you are appealing.
- Provide the BENEFICIARY name, which refers to the person covered under Medicare.
- Enter the HEALTH INSURANCE CLAIM NUMBER (HICN) for the beneficiary. If you have multiple claims or beneficiaries, attach a list with all relevant details.
- In the PROVIDER, PRACTITIONER, OR SUPPLIER section, include the name of the provider associated with the case.
- List the SPECIFIC ITEM(S) OR SERVICE(S) involved in your appeal.
- Select the Medicare Claim type: Part A, Part B, Part C, or Part D.
- Indicate if this request involves authorization for an item or service that has not yet been furnished. If Yes, skip to the next step. If No, provide the Specific Dates of Service.
- If your request involves a Medicare Part D prescription drug, check whether application of the standard appellate timeframe could jeopardize the beneficiary’s health. Answer Yes or No.
- Write the date of the ALJ decision or dismissal that you are appealing.
- Clearly state your reasons for disagreement with the ALJ’s action. Specify the parts of the decision you think were incorrect. You may attach additional sheets if necessary.
- Attach a copy of the ALJ decision or dismissal order you are appealing.
- Sign and date the form in the specified sections for APPELLANT’S SIGNATURE and, if applicable, REPRESENTATIVE’S SIGNATURE.
- Provide printed names, addresses, and contact information for both the appellant and the representative, if applicable.
- Submit your request for review within 60 days of receiving the ALJ decision. Include the HICN and ALJ Appeal Number on any additional materials.
After filling out the form, send it to the Medicare Appeals Council. You may use U.S. Mail, a common carrier, or fax the request. Ensure that a copy is sent to all other parties involved. If you need assistance, contact the Medicare Appeals Council for guidance.
What You Should Know About This Form
What is the purpose of the Dab 101 form?
The Dab 101 form is used to request a review of an Administrative Law Judge (ALJ) decision or dismissal regarding Medicare claims. Individuals or organizations dissatisfied with an ALJ’s ruling can use this form to formally appeal the decision to the Medicare Appeals Council.
Who can submit the Dab 101 form?
The form can be submitted by appellants, which includes beneficiaries, providers, practitioners, or suppliers. If a beneficiary is represented, the representative must also sign the form. It is important that all parties involved in the claim are correctly identified on the form.
What information must be included on the Dab 101 form?
Required information includes the appellant's details, ALJ appeal number, beneficiary's name, Health Insurance Claim Number (HICN), specific services or items involved, and the type of Medicare claim (Part A, B, C, or D). If the request involves multiple claims or beneficiaries, provide a detailed attachment.
What is the deadline for submitting the Dab 101 form?
The request must be submitted within 60 calendar days of receiving the ALJ’s decision. It is assumed that individuals received the decision five calendar days after it was issued unless a later date can be demonstrated. The form must reach the Medicare Appeals Council within this timeframe to be considered.
Can new evidence be included with the Dab 101 form?
New evidence can be submitted with the form; however, if the case has already been reconsidered by a Qualified Independent Contractor (QIC), the Medicare Appeals Council may not accept this evidence unless there is a valid reason for introducing it at that stage.
What should I do if I need more time to file my appeal?
If more time is needed to submit evidence or legal arguments, a written extension request must be made. You should explain the reasons for needing additional time and submit it alongside your Dab 101 form.
How can I submit the Dab 101 form?
The Dab 101 form can be submitted by U.S. Mail, a common carrier like FedEx, or via fax. If faxing, do not send a mailed copy. Ensure that a copy of the appeal is sent to all involved parties, including beneficiaries.
Where should I send the Dab 101 form?
The form should be sent to the Medicare Appeals Council at the following address: Department of Health and Human Services, Departmental Appeals Board, Medicare Appeals Council, MS 6127 Cohen Building Room G-644, 330 Independence Ave., S.W., Washington, D.C. 20201. For fax submissions, use (202) 565-0227.
Common mistakes
Filling out the DAB-101 form can be tricky, and people often make mistakes along the way. One common error is not providing the correct ALJ Appeal Number. This number is crucial in identifying the appeal you are filing. Without it, your request could be delayed or dismissed altogether. Always double-check that you’ve entered the correct number to avoid any issues.
Another frequent mistake is failing to include the necessary supporting documents. It's important to attach a copy of the ALJ decision or dismissal order you are appealing. Some people think that sending the completed form alone is sufficient. However, without this crucial documentation, your appeal may not be processed. Be sure to include all required documents when submitting your request.
Many individuals also overlook the deadline for submitting their request. The form must be received within 60 calendar days after the ALJ's decision. Some people mistakenly believe they have more time, resulting in missed deadlines. Mark your calendar as a reminder to ensure you submit your appeal on time.
Lastly, improper completion of contact information can create obstacles. Many forget to fill in all fields like telephone number or email. Providing accurate contact details is essential for communication regarding your appeal. If there are questions or further information needed, the Medicare Appeals Council must be able to reach you easily.
Documents used along the form
When filing a request for review using the DAB 101 form, it’s often necessary to attach or complete additional documents. Each of these forms plays a unique role in the appeals process and helps to ensure that all relevant information is considered. Here’s a brief overview of other documents frequently used alongside the DAB 101 form:
- ALJ Decision or Dismissal Order: This document provides the details of the decision made by the Administrative Law Judge. A copy must be attached to the DAB 101 form to provide context for the appeal.
- Request for Extension of Time: If more time is needed to gather evidence or legal arguments, this written request should explain the reasons for the delay and the additional time required.
- Additional Evidence Submission: Any supplementary documentation that supports the appeal can be included. This may consist of medical records, treatment plans, or other relevant information.
- Appointment of Representative Form: If an individual is being represented by another person (like an attorney), this form should verify the appointment of the representative, ensuring they have the authority to act on the appellant’s behalf.
- Cover Letter: A cover letter can accompany the appeal to summarize the requested actions and clarify the enclosed materials. If multiple beneficiaries are involved, a cover letter listing all parties can be beneficial.
- Medicare Claim Documents: This includes any prior claims or notices related to the case that may help establish the background of the appeals. These can provide crucial information for review.
- Appeal Checklist: A self-created checklist of required documents and actions can help ensure that all necessary steps are completed before submission. This is not an official document but serves as a helpful guide.
- Proof of Mailing: Keeping a record of how and when the appeal was sent, including any tracking information, can protect against issues of timeliness or submission verification.
Having these documents prepared and organized alongside the DAB 101 form can significantly streamline the appeals process. Clear and complete submissions lead to better understanding and processing, ultimately supporting the goal of receiving a fair review of the case.
Similar forms
- Medicare Appeal Form (CMS-20033): Similar to DAB 101, this form is used to appeal decisions made by Medicare Administrative Contractors (MACs) regarding denied claims. Both forms require information about the appellant and the specific claim in question.
- Request for Reconsideration (CMS Form 20034): This is the next step after the initial denial, similar to the DAB 101 in that it specifically addresses the need for an urgent review of a previously denied claim. Both forms demand detailed information relevant to the decision being contested.
- ALJ Hearing Request Form: Like the DAB 101, it initiates a request for a hearing before an Administrative Law Judge. Both demand identification of the appellant and essential details surrounding the case.
- Medicaid Fair Hearing Request Form: This document is used for appeals in the Medicaid system, similar to DAB 101, which allows beneficiaries to contest decisions impacting their benefits. Each form requires the submission of supporting documents.
- Medicare Part D Coverage Determination Request Form: This form is used when beneficiaries want to appeal a decision regarding prescription drug coverage. It parallels the DAB 101's focus on specific services and requested actions.
- CMS Form 10147 - Medicare Advantage Enrollment Form: Similar in structure, this form is used for decisions related to Medicare Advantage plans. Both forms involve the benefits and services received and require detailed beneficiary information.
- Advanced Beneficiary Notice of Noncoverage (ABN): Though slightly different in purpose, the ABN informs patients about non-covered services. It is similar to the DAB 101 in that both forms focus on the necessity of documenting the patient’s understanding and consent related to Medicare benefits.
Dos and Don'ts
- Do double-check the accuracy of all personal information, such as your name and address, before submission.
- Do attach a copy of the ALJ decision or dismissal order you are appealing.
- Do ensure that the request is filed within 60 calendar days of receiving the ALJ’s decision.
- Do include any additional evidence relevant to your appeal.
- Do send copies of your appeal to all parties involved, including all beneficiaries.
- Don't leave any required fields blank; incomplete forms may delay your appeal.
- Don't forget to reference both the HICN and the ALJ Appeal Number on any correspondence.
- Don't submit new evidence if the issue has already been reviewed by a Qualified Independent Contractor without a valid reason.
- Don't use fax and mail simultaneously; choose one method for submission.
- Don't miss the opportunity to explain any delays in filing your request after the 60-day period if applicable.
Misconceptions
Misconceptions about the Dab 101 form can lead to confusion and potential issues in the appeals process. Here are five common misconceptions, along with clarifications:
-
Anyone can submit the Dab 101 form at any time.
This is incorrect. You must submit the request within 60 calendar days of receiving the ALJ’s decision or dismissal. If you cannot meet this deadline, you need to explain why in writing.
-
You do not need to provide a copy of the ALJ decision.
This misconception can lead to delays. It’s essential to attach a copy of the ALJ decision or dismissal order you are appealing, as this ensures your request is properly processed.
-
Submitting additional evidence after the initial filing is always allowed.
This is not true. If your case was reconsidered by a Qualified Independent Contractor (QIC), the Medicare Appeals Council generally will not accept new evidence unless you provide a good reason for offering it for the first time.
-
There’s no need to notify other parties about the appeal.
This belief can complicate the process. You must send a copy of your appeal to other involved parties and confirm that all beneficiaries are informed.
-
The Dab 101 form can be filed through any method, without restrictions.
This is misleading. Although you can send the form by U.S. Mail, FedEx, or fax, you must follow specific guidelines, such as not mailing a copy if you have already sent a fax.
Understanding these key points about the Dab 101 form can help ensure a smoother appeals process and enhance your chances of a favorable review.
Key takeaways
Understanding the DAB 101 form is essential for navigating the Medicare appeals process. Here are key takeaways to help you fill it out effectively:
- Identify yourself clearly. Start by providing your information as the Appellant. Include your name and contact details prominently.
- Document necessary details. Ensure you fill in the ALJ Appeal Number and Health Insurance Claim Number (HICN). This information is crucial for tracking your appeal.
- List all relevant beneficiaries. If your appeal involves multiple claims or beneficiaries, attach a comprehensive list to avoid confusion.
- Specify the type of claim. Indicate which Medicare claim type applies—whether it's Part A, Part B, Part C, or Part D. This specification helps direct your request appropriately.
- Adhere to deadlines. Submit your request within 60 calendar days of receiving the ALJ’s decision. If you need more time, request an extension promptly and explain your circumstances.
- Ensure completeness. Attach any additional evidence relevant to your case, and do not forget to include the ALJ’s decision with your appeal.
Taking the time to fill out the DAB 101 form correctly can make a significant difference in the outcome of your appeal. Ensure clarity, stay organized, and keep track of all deadlines to enhance your chances of a favorable review.
Browse Other Templates
Css Profile Income Limits - Students should mark their noncustodial parent’s contact details as completely as possible.
Emergency Medication Self-Administration Request,Student Medication Authorization Form,Chesapeake Emergency Inhaler Form,Medication Self-Administer Permission Slip,Self-Administered Medication Notification,Asthma Medication Self-Administration Consen - The form includes a legal clause referring to the Code of Virginia Section 22.1-274.2.
Patient Demographic Form PDF - Please specify the best time to call you for any follow-up or questions.