Fill Out Your Health Claim Form
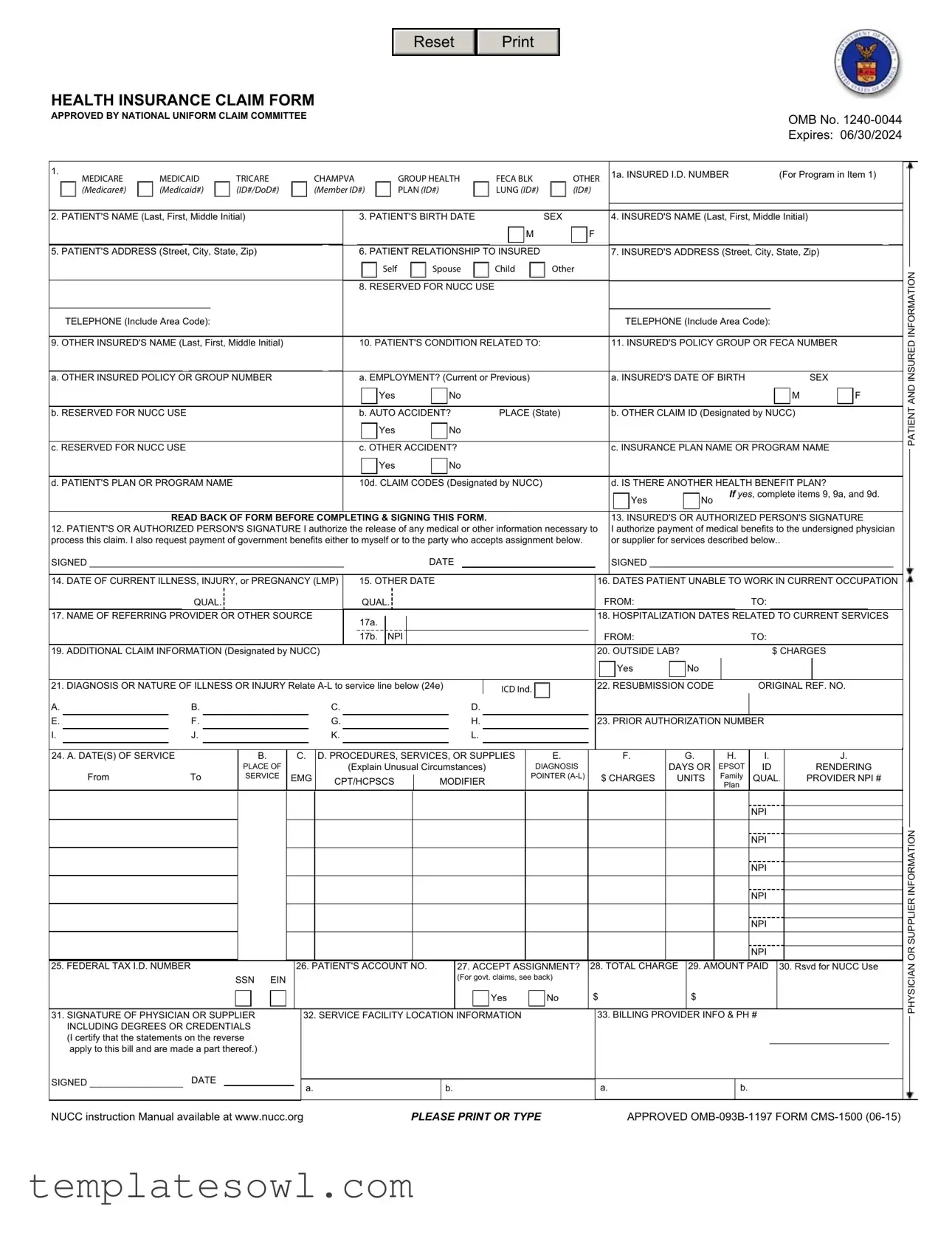
The Health Claim form is a critical document for individuals navigating the complexities of medical insurance claims. This form plays a vital role in gathering essential information about both the patient and the insured. Key sections include the patient’s identification details, relationship to the insured, and information regarding any other insurance plans that may cover the medical services. The form requires specifics related to the patient's condition, including diagnosis codes and dates of service, ensuring that providers and insurers are on the same page. Additionally, signatures from both the patient and the authorized representative are necessary; these endorsements facilitate the release of medical information and authorize payment directly to healthcare providers. Detailed instructions for completing each section help users avoid common pitfalls, while the form also outlines how various types of insurance—such as Medicare, Medicaid, and private health plans—affect the process. Overall, understanding the Health Claim form is essential for ensuring that medical expenses are reimbursed efficiently and accurately.
Health Claim Example
Reset
HEALTH INSURANCE CLAIM FORM
APPROVED BY NATIONAL UNIFORM CLAIM COMMITTEE
OMB No.
Expires: 06/30/2024
1. |
MEDICARE |
MEDICAID |
TRICARE |
CHAMPVA |
GROUP HEALTH |
FECA BLK |
OTHER |
1a. INSURED I.D. NUMBER |
(For Program in Item 1) |
|
|||||||||
|
|
|
|||||||
|
(Medicare#) |
(Medicaid#) |
(ID#/DoD#) |
(Member ID#) |
PLAN (ID#) |
LUNG (ID#) |
(ID#) |
|
|
|
2. PATIENT'S NAME (Last, First, Middle Initial) |
|
|
|
|
|
|
|
|
3. PATIENT'S BIRTH DATE |
|
|
|
|
|
|
SEX |
|
|
|
|
|
4. INSURED'S NAME (Last, First, Middle Initial) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
M |
|
|
|
|
F |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INSURED |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
5. PATIENT'S ADDRESS (Street, |
|
City, State, Zip) |
|
|
|
|
|
|
|
|
6. PATIENT RELATIONSHIP TO |
|
|
|
|
|
7. INSURED'S ADDRESS (Street, City, State, Zip) |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Self |
|
|
|
|
|
Spouse |
|
|
Child |
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
8. RESERVED FOR NUCC USE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
TELEPHONE (Include Area Code): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TELEPHONE (Include Area Code): |
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
9. OTHER INSURED'S NAME (Last, First, Middle Initial) |
|
|
|
|
|
|
|
|
10. PATIENT'S CONDITION RELATED TO: |
|
|
|
|
|
11. INSURED'S POLICY GROUP OR FECA NUMBER |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a. EMPLOYMENT? (Current or Previous) |
|
|
|
|
|
|
|
|
a. INSURED'S DATE OF BIRTH |
|
|
|
|
|
|
|
|
|
|
SEX |
||||||||||||||||||||||||||||||||||||||||
|
a. OTHER INSURED POLICY OR GROUP NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
M |
|
|
|
F |
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b. AUTO ACCIDENT? |
PLACE (State) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
by NUCC) |
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
b. RESERVED FOR NUCC USE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b. OTHER CLAIM ID (Designated |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
c. RESERVED FOR NUCC USE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c. OTHER ACCIDENT? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c. INSURANCE PLAN NAME OR PROGRAM NAME |
|||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
d. PATIENT'S PLAN OR PROGRAM NAME |
|
|
|
|
|
|
|
|
|
|
|
10d. CLAIM CODES (Designated by NUCC) |
|
|
|
|
|
d. IS THERE ANOTHER HEALTH BENEFIT PLAN? |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
No |
|
If yes, complete items 9, 9a, and 9d. |
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
READ BACK OF FORM BEFORE COMPLETING & SIGNING THIS FORM. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
13. INSURED'S OR AUTHORIZED PERSON'S SIGNATURE |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
12. PATIENT'S OR AUTHORIZED PERSON'S SIGNATURE I authorize the release of any medical or other information necessary to I authorize payment of medical benefits to the undersigned physician |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
process this claim. I also request payment of government benefits either to myself or to the party who accepts assignment below. |
|
|
|
|
|
or supplier for services described below.. |
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
SIGNED _________________________________________________ |
|
|
|
|
|
|
|
|
|
|
DATE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SIGNED _______________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
14. DATE OF CURRENT ILLNESS, INJURY, or PREGNANCY (LMP) |
|
15. OTHER DATE |
|
|
|
|
|
|
|
|
|
|
|
16. DATES PATIENT UNABLE TO WORK IN CURRENT OCCUPATION |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FROM: |
|
|
|
|
|
|
|
|
TO: |
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
17. NAME OF REFERRING PROVIDER OR OTHER SOURCE |
|
|
17a. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18. HOSPITALIZATION DATES |
RELATED |
|
TO CURRENT SERVICES |
|||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
19. ADDITIONAL CLAIM INFORMATION (Designated by NUCC) |
|
|
17b. |
NPI |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FROM: |
|
|
|
|
|
|
|
|
TO: |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20. OUTSIDE LAB? |
|
|
|
|
|
|
|
|
|
|
$ CHARGES |
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
21. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate |
|
|
|
|
|
|
|
|
|
22. RESUBMISSION CODE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
ICD Ind. |
|
|
|
|
|
|
|
|
|
|
ORIGINAL REF. NO. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
A. |
|
|
B. |
|
|
|
|
|
|
|
|
|
|
C. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
D. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
E. |
|
|
F. |
|
|
|
|
|
|
|
|
|
|
|
G. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
H. |
|
|
|
|
|
|
|
|
|
|
|
|
23. PRIOR AUTHORIZATION NUMBER |
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
I. |
|
|
J. |
|
|
|
|
|
|
|
|
|
|
|
K. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
L. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
G. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
J. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
24. A. DATE(S) OF SERVICE |
|
|
|
|
|
B. |
|
C. |
D. PROCEDURES, SERVICES, OR SUPPLIES |
|
|
|
E. |
|
|
|
|
|
|
F. |
|
|
H. |
|
I. |
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
PLACE OF |
|
|
|
|
|
|
|
(Explain Unusual Circumstances) |
|
|
|
|
|
|
DIAGNOSIS |
|
|
|
|
|
|
|
|
|
DAYS OR |
EPSOT |
|
ID |
|
|
|
RENDERING |
||||||||||||||||||||||||||||||||||||||
|
|
From |
To |
SERVICE |
EMG |
|
CPT/HCPSCS |
|
|
|
MODIFIER |
|
|
|
|
|
POINTER |
|
|
|
$ CHARGES |
UNITS |
Family |
QUAL. |
|
|
PROVIDER NPI # |
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Plan |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI |
|
|
|
|
|
|
|
|
|
|
||||||
|
25. FEDERAL TAX I.D. NUMBER |
|
|
|
|
26. |
PATIENT'S ACCOUNT |
NO. |
|
|
|
|
|
27. ACCEPT |
ASSIGNMENT? |
|
28. TOTAL CHARGE |
29. AMOUNT PAID |
30. Rsvd for NUCC Use |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
SSN EIN |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(For govt. claims, see back) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
$ |
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
31. SIGNATURE OF PHYSICIAN OR SUPPLIER |
|
|
32. SERVICE FACILITY LOCATION |
|
INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
33. BILLING PROVIDER INFO & PH # |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
INCLUDING DEGREES OR CREDENTIALS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
(I certify that the statements on the reverse |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
apply to this bill and are made a part thereof.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
SIGNED __________________ |
DATE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a. |
|
|
|
|
|
b. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
a. |
|
|
|
|
|
|
|
|
|
|
|
|
|
b. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PATIENT AND INSURED INFORMATION
 PHYSICIAN OR SUPPLIER INFORMATION
PHYSICIAN OR SUPPLIER INFORMATION
NUCC instruction Manual available at www.nucc.org |
PLEASE PRINT OR TYPE |
APPROVED |
Instructions for Completing
GENERAL
FEES: The Department of Labor's Office of Workers' Compensation Programs (OWCP) is responsible for payment of all reasonable charges stemming from covered medical services provided to claimants eligible under FECA and EEOICPA. OWCP uses a relative value scale fee schedule and other tests to determine reasonableness. Schedule limitations are applied through an automated billing system that is based on the identification of procedures as defined in the AMA's Current Procedural Terminology (CPT); correct CPT code and modifier(s) is required. Incorrect coding will result in inappropriate payment. For specific information about schedule limits, call the Dept. of Labor's Federal Employees' Compensation office or Energy Employees Occupational Illness Compensation office that services your area.
REPORTS: A medical report that indicates the dates of treatment, diagnosis(es), findings, and type of treatment offered is required for services provided by a physician (as defined above). For FECA claimants, the initial medical report should explain the relationship of the injury or illness to the employment. Test results and
GENERAL
SIGNATURE OF PHYSICIAN OR SUPPLIER: Your signature in Item 31 indicates your agreement to accept the charge determination of OWCP on covered services as payment in full, and indicates your agreement not to seek reimbursement from the patient of any amounts not paid by OWCP for covered services as the result of the application of its fee schedule or related tests for reasonableness (appeals are allowed). Your signature in Item 31 also indicates that the services shown on this form were medically indicated and necessary for the health of the patient and were personally furnished by you or were furnished incident to your professional services by your employee under your immediate personal supervision, except as otherwise expressly permitted by FECA, Black Lung or EEOICPA regulations. For services to be considered as "incident" to a physician's professional service, 1) they must be rendered under the physician's immediate personal supervision by his/her employee, 2) they must be an integral, although incidental, part of a covered physician's service, 3) they must be of kinds commonly furnished in physician's offices, and 4) the services of
NOTICE TO PATIENT ABOUT THE COLLECTION AND USE OF FECA, BLACK LUNG AND EEOICPA INFORMATION
(PRIVACY ACT STATEMENT)
We are authorized by OWCP to ask you for information needed in the administration of the FECA, Black Lung and EEOICPA programs. Authority to collect information is in 5 USC 8101 et seq.; 30 USC 901 et seq.; 38 USC 613; E.O. 9397; and 42 USC 7384d, 20 CFR 30.11 and E.O. 13179. The information we obtain to complete claims under these programs is used to identify you and to determine your eligibility. It is also used to decide if the services and supplies you received are covered by these programs and to insure that proper payment is made. Your response regarding the medical service(s) received or the amount charged is required to receive payment for the claim. See 20 CFR §§ 10.801, 30.701, 725.406, 725.701, and 725.704. Failure to supply the claim number or CPT codes will delay payment or may result in rejection of the claim because of incomplete information. The information may also be given to other providers of services, carriers, intermediaries, medical review boards, health plans, and other organizations or Federal agencies, for the effective administration of Federal provisions that require other third party payers to pay primary to Federal programs, and as otherwise necessary to administer these programs. For example, it may be necessary to disclose information about the benefits you have used to a hospital or doctor. Additional disclosures are made through routine uses for information contained in systems of records. See Department of Labor systems
You should be aware that P.L.
FORM SUBMISSION
DEEOIC: Send all forms for DEEOIC to Energy Employees Occupational Illness Compensation Programs, PO Box 8304, London, KY
DCMWC: Send all forms for DCMWC to Federal Black Lung program, PO Box 8302, London, KY
INSTRUCTIONS FOR COMPLETING THE FORM: A brief description of each data element and its applicability to requirements under FECA, BLBA and EEOICPA are listed below. For further information contact OWCP.
Item 1. Leave blank.
Item 1a. Enter the patient's claim number.
Item 2. Enter the patient's last name, first name, middle initial.
Item 3. Enter the patient's date of birth (MM/DD/YY) and check appropriate box for patient's sex.
Item 4. For FECA: leave blank. For BLBA and EEOICPA: complete only if patient is deceased and this medical cost was paid by a survivor or estate. Enter the name of the party to whom medical payment is due.
Item 5. Enter the patient's address (street address, city, state, ZIP code; telephone number is optional). Item 6. Leave blank.
Item 7. For FECA: leave blank. For BLBA and EEOICPA: complete if Item 4 was completed. Enter the address of the party to be paid. Item 8. Leave blank.
Item 9. Leave blank.
Item 10. Leave blank.
Item 11. For FECA: enter patient's claim number. OMISSION WILL RESULT IN DELAYED BILL PROCESSING. For BLBA and EEOICPA: leave blank.
OMB No. |
|
Expires: 06/30/2024 |
|
Item 11a. |
Leave blank. |
|
Item 11b. |
Leave blank. |
|
Item 11c. |
Leave blank. |
|
Item 11d. |
Leave blank. |
|
Item 12. |
The signature of the patient or authorized representative authorizes release of the medical information necessary to process the claim, and |
|
|
requests payment. Signature is required; mark (X) must be |
|
Item 13. |
Signature indicates authorization for payment of benefits directly to the provider. Acceptance of this assignment is considered to be a |
|
|
contractual arrangement. The "authorizing person" may be the beneficiary (patient) eligible under the program billed, a person with a power of |
|
|
attorney, or a statement that the beneficiary's signature is on file with the billing provider. |
|
Item 14. |
Leave blank. |
|
Item 15. |
Leave blank. |
|
Item 16. |
Leave blank. |
|
Item 17. |
Leave blank. |
|
Item 18. |
Leave blank. |
|
Item 19. |
Leave blank. |
|
Item 20. |
Leave blank. |
|
Item 21. |
Enter the diagnosis(es) of the condition(s) being treated using current ICD codes. Enter codes in priority order (primary, secondary condition). |
|
|
Coding structure must follow the International Classification of Disease, 10th Edition, Clinical Modification or the latest revision published. A |
|
|
brief narrative may also be entered but not substituted for the ICD code. |
|
Item 22. |
Leave blank. |
|
Item 23. |
Leave blank. |
|
Item 24. |
Column A: enter month, day and year (MM/DD/YY) for each service/consultation provided. If the "from" and "to" dates represent a series of |
|
|
identical services, enter the number of services provided in Column G. |
|
|
Column B: enter the correct CMS/OWCP standard "place of service" (POS) code (see below). |
|
|
Column C: not required. |
|
|
Column D: enter the proper |
|
|
Column E: enter the diagnostic reference letter (A, B, C, etc. in Item 21) to relate the date of service and the procedure(s) performed to |
the |
|
appropriate ICD code, or enter the appropriate ICD code. |
|
|
Column F: enter the total charge(s) for each listed service(s). |
|
|
Column G: enter the number of services/units provided for period listed in Column A. Anesthesiologists enter time in total minutes, not |
units. |
|
Column H: Leave blank. |
|
|
Column I: Leave blank. |
|
|
Column J: Enter NPI. For FECA: required. OMISSION WILL RESULT IN DELAYED BILL PROCESSING. |
|
Item 25: |
Enter the Federal tax I.D. |
|
Item 26: |
Provider may enter a patient account number that will appear on the remittance voucher. |
|
Item 27: |
Leave blank. |
|
Item 28: |
Enter the total charge for the listed services in Column F. |
|
Item 29: |
If any payment has been made, enter that amount here. |
|
Item 30: |
Enter the balance now due. |
|
Item 31: |
For BLBA and EEOICPA: sign and date the form. For FECA: signature stamp or "signature on file" is acceptable. |
|
Item 32: |
Enter complete name of hospital, facility or physician's office were services were rendered. Item 32a. Enter NPI. Item 32b. Enter taxonomy |
|
|
number. |
|
Item 33: |
Enter (1) the name and address to which payment is to be made, and (2) your DOL provider number after "PIN #" if you are an individual |
|
|
provider, or after "GRP #" if you are a group provider. FAILURE TO ENTER THIS NUMBER WILL DELAY PAYMENT OR CAUSE A |
|
|
REJECTION OF THE BILL FOR INCOMPLETE/INACCURATE INFORMATION. |
|
Item 33a. |
Enter NPI. |
|
Item 33b. |
Enter taxonomy number. |
|
Place of Service (POS) Codes for Item 24B |
|
|
|
|
2 |
Telehealth |
34 |
Hospice |
|
3 |
School |
41 |
Ambulance - Land |
|
4 |
Homeless Shelter |
42 |
Ambulance - Air or Water |
|
5 |
Indian Health Service |
49 |
Independent Clinic |
|
6 |
Indian Health Service |
50 |
Federally Qualified Health Center |
|
7 |
Tribal 638 |
51 |
Inpatient Psychiatric Facility |
|
8 |
Tribal 638 |
52 |
Psychiatric Facility Partial Hospitalization |
|
9 |
Prison |
53 |
Community Mental Health Center (CMHC) |
|
11 |
Office |
54 |
Intermediate |
Care Facility/Mentally Retarded |
12 |
Patient Home |
55 |
Residential Substance Abuse Treatment Facility |
|
13 |
Assisted Living |
56 |
Psychiatric Residential Treatment Center |
|
14 |
Group Home |
57 |
||
15 |
Mobile Unit |
60 |
Mass Immunization Center |
|
17 |
Walk in Retail Health Clinic |
61 |
Comprehensive Inpatient Rehabilitation Facility |
|
18 |
Place of Employment/Worksite |
62 |
Comprehensive Outpatient Rehabilitation Facility |
|
19 |
Off Campus Outpatient Hospital |
65 |
End Stage Renal Disease Treatment Facility |
|
20 |
Urgent Care |
71 |
State or Local Public Health Clinic |
|
21 |
Inpatient Hospital |
72 |
Rural Health |
Clinic |
22 |
Outpatient Hospital |
81 |
Independent |
Laboratory |
23 |
Emergency Room - Hospital |
99 |
Other Place of Service |
|
24Ambulatory Surgical Center
25Birthing Center
26Military Treatment Facility
31Skilled Nursing Facility
32Nursing Facility
33Custodial Care Facility
OMB No. |
|
Expires: 06/30/2024 |
|
Public Burden Statement
According to the Paperwork Reduction Act of 1995, an agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is
THESE OFFICES.
NOTICE
If you have a substantially limiting physical or mental impairment, Federal disability nondiscrimination law gives you the right to receive help from OWCP in the form of communication assistance, accommodation and modification to aid you in the claims process. For example, we will provide you with copies of documents in alternate formats, communication services such as sign language interpretation, or other kinds of adjustments or changes to account for the limitations of your disability. Please contact our office or your claims examiner to ask about this assistance.
OMB No. |
|
Expires: 06/30/2024 |
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of the Form | The Health Claim Form facilitates the processing of medical claims for various insurance programs, including Medicare, Medicaid, and federal compensation acts. |
| Programs Covered | The form is used for claims under Medicare, Medicaid, TRICARE, CHAMPVA, FECA, and Black Lung benefits. |
| Identification Numbers | Insured's identification numbers are required for verification of eligibility under the respective programs. |
| Authorized Signatures | The form requires signatures from both the patient and the insured, certifying the accuracy of provided information and authorizing payment. |
| Date Requirements | Claim submitters must provide dates of service, related illnesses, and any dates the patient was unable to work. |
| Diagnosis Codes | Claimants need to include ICD codes to describe the patient’s condition, ordered by priority. |
| Fee Structure | The Department of Labor uses a fee schedule to determine the reasonableness of charges for covered medical services. |
| Medical Reports | Reports detailing the treatment dates, diagnoses, and nature of medical services must accompany the claim for processing. |
| Privacy Act Compliance | The collection and use of information adhere to the Privacy Act, ensuring confidentiality in the claims process. |
| State-Specific Regulations | State laws govern insurance policies and the handling of health claims, which may vary significantly from one state to another. |
Guidelines on Utilizing Health Claim
Completing the Health Claim form can feel overwhelming, but breaking it down into simple steps makes the process manageable. By following these instructions, you’ll provide all necessary information accurately. Let's get started.
- Leave the first box (1) blank.
- In box 1a, enter the patient's claim number.
- Write the patient's full name (last name, first name, middle initial) in box 2.
- In box 3, enter the patient's date of birth using the format MM/DD/YY and mark the appropriate box for the patient's sex (M or F).
- For box 4, if applicable, provide the name of the party to whom medical payment is due.
- Fill in the patient's address in box 5 (street, city, state, ZIP code); phone number is optional.
- Leave box 6 blank.
- If needed, complete box 7 for patients covered under BLBA and EEOICPA by entering the address of the party to be paid.
- Leave box 8 blank.
- In box 9, leave it blank.
- For box 10, leave it blank.
- Complete box 11 with the patient's claim number for FECA; leave it blank for other programs.
- Leave boxes 11a, 11b, 11c, and 11d blank.
- In box 12, have the patient or authorized representative sign to permit release of medical information and request payment.
- For box 13, provide the signature for authorization of benefit payment directly to the healthcare provider.
- Leave boxes 14 through 19 blank.
- In box 21, enter the diagnosis codes as per the ICD guideline, detailing the conditions treated, with primary and secondary conditions prioritized.
- Leave boxes 22 and 23 blank.
- In box 24, fill in dates of service (Column A), Place of service (Column B), and CPT code (Column D), relating them to the diagnosis codes (Column E).
- Enter the total charge for services in Column F and the number of services or units in Column G.
- Leave columns H and I blank.
- In Column J, enter your NPI; this is required for FECA.
- Enter your Federal tax I.D. in box 25.
- Optionally, include a patient account number in box 26.
- Leave box 27 blank.
- Provide the total charge for all services in box 28.
- Include any payments made in box 29.
- Calculate the balance due and record it in box 30.
- Sign and date the form in box 31.
- In box 32, enter the name of the hospital or facility where services were provided.
- Complete box 33, including the name and address for payment and provider number if applicable.
- Finally, ensure you're familiar with all codes and that the form is submitted according to the guidelines for your program.
Once the form is filled out, double-check all entries for accuracy. This attention to detail ensures a smoother processing experience for your health claim. If you encounter any issues, remember that help is available.
What You Should Know About This Form
What is the purpose of the Health Claim form?
The Health Claim form is used to request reimbursement for medical services provided to patients under various health insurance programs, including Medicare, Medicaid, and other federal programs. It allows healthcare providers to document services rendered and claim payment for those services from the appropriate insurance provider.
Who needs to fill out the Health Claim form?
The form must be filled out by healthcare providers delivering medical services to patients. Additionally, patients may need to provide information, such as their personal details and coverage information. If a patient has an authorized representative, that individual can also sign the form on behalf of the patient.
What information is required on the Health Claim form?
Key information needed includes the patient's name, date of birth, and address. Providers also need to include details about the medical services rendered, including dates of service, procedure codes, and the total charges. Insurance information, including claimant ID numbers and diagnosis codes, is also critical for processing the claim accurately.
What should I do if I make a mistake while filling out the form?
If an error occurs, it is best to start a new form rather than attempting to cross things out. This ensures clarity and avoids confusion for the claims processor. Always double-check to verify that all information is accurate before submission to prevent delays in processing.
How do I submit the Health Claim form?
Submission methods depend on the specific program. Generally, claims can be mailed to designated PO boxes based on the type of claim. For instance, FECA claims should be sent to the Office of Workers' Compensation Programs, while those under the Black Lung program have a different address. Be sure to check the instructions applicable to the specific claim you are filing.
How long does it take to process a claim once the form is submitted?
Processing times can vary significantly based on the type of claim and the specific insurance program. Typically, it may take several weeks for a claim to be reviewed and processed. Factors like the volume of claims, accuracy of submitted forms, and whether additional information is needed can all influence timing.
What happens if my claim is denied?
If a claim is denied, the insurance provider will generally send a notification explaining the reason for the denial. Patients and providers can appeal the decision by following the instructions provided with the denial notice. It is important to provide any additional documentation or clarification that may support the claim during the appeals process.
Can I check the status of my claim?
Yes, patients and providers can usually check the status of their claims by contacting the insurance provider directly. The provider may offer online tools for tracking claims or set up a customer service line specifically for inquiries. Keeping a record of the claim submission date and reference numbers can help facilitate this process.
What should I do if I need assistance with the Health Claim form?
Assistance is available through different channels. You can consult your healthcare provider's billing department, access resources from the insurance company, or review online guidelines provided by federal programs. Don’t hesitate to ask for help if you encounter difficulties in filling out the form correctly or understanding the requirements.
Common mistakes
Filling out a Health Claim form can feel daunting, but avoiding common pitfalls can streamline the process and ensure you receive your benefits promptly. One frequent mistake is failing to provide accurate and complete patient information. Every field asking for personal details, like the patient's name, birth date, and insurance identification number, must be filled out correctly. Omissions or errors in these details can lead to processing delays or even rejection of the claim.
Another common error involves the diagnosis codes. It's crucial to enter the correct medical diagnosis using the latest ICD codes. Participants often neglect to order the codes according to their importance, leading to improper claim assessments. If medical services relate to multiple conditions, ensure that the primary diagnosis is listed first, with secondary conditions following in order of treatment relevance.
Many also misunderstand the requirements for signatures on the form. The patient's or authorized representative's signature is essential; failure to secure a signature could result in the denial of payment. Be particularly cautious about when and where to sign. A witnessed mark or missing details related to the witness’ relationship to the patient can further complicate matters.
In addition, items left blank often create confusion and delays. Items such as the dates of service and the procedure codes need to be populated accurately. Leaving these fields empty can cause immediate rejection or delay in processing. Ensure that the dates reflect the accurate timeframe of the services provided.
A significant issue arises when the provider's NPI number is omitted. This number is essential for processing the claim. Claims lacking this critical information may face rejection or major delays. Always double-check that the NPI is written correctly in the appropriate field.
Moreover, many individuals overlook the importance of total charges and amounts paid. This information must be filled in correctly to prevent discrepancies or payment issues later on. If these figures are miscalculated or missing, it can stall the payment process entirely.
Finally, the relationship between the patient and the insured is often not specified correctly. It's vital to clearly identify whether the patient is the self, spouse, or child of the insured. Errors here can lead to complications in validating the claim, possibly affecting the eligibility for reimbursement.
By steering clear of these common mistakes when completing the Health Claim form, you'll increase your chances of a smooth and timely claims process. Taking extra care with these details pays dividends in the long run—don’t let a simple oversight compromise your benefits.
Documents used along the form
The Health Claim Form is just one part of the documentation required for submitting health insurance claims. Several other forms and documents may be necessary to ensure proper processing and approval of claims. Below is a list of these commonly used documents, each described briefly to provide context for their use. Gathering these documents ahead of time can streamline the claims process and help facilitate timely payments.
- Medical Report: This document outlines the patient's diagnosis, treatment, and any test results. It is essential for detailing the medical necessity of services rendered.
- Authorization Form: This form grants permission for the release of medical information. It is signed by the patient or an authorized representative before the claim is submitted.
- Itemized Bill: An itemized statement from the healthcare provider that details the services rendered, including dates, charges, and descriptions. This is often required to accompany the claim form for accurate billing.
- Referral Letter: If applicable, this letter from a primary care provider refers the patient to a specialist. It supports the necessity of the specialized treatment and may be required for claim approval.
- Coordination of Benefits Form: This form is necessary when a patient has multiple insurance plans. It helps coordinate payments between the insurers to avoid overpayment and communicate the sequence of coverage.
- Proof of Eligibility: Documentation, such as an insurance card or capitation agreement, that confirms the patient's active enrollment in the health plan at the time of service.
- Claim Summary: A summary of any previous claims submitted by the patient. This document is useful to show patterns or issues with past submissions that may affect the current claim.
Including the appropriate supplementary documents can help avoid delays or denials in processing health insurance claims. Proper preparation and attention to detail in gathering these forms will promote a smoother experience for both the patient and the healthcare provider.
Similar forms
The Health Insurance Claim Form shares similarities with several other important documents used in the healthcare and insurance sectors. Here is a detailed comparison:
- Medicare Claim Form (CMS-1500): Like the Health Claim form, the Medicare Claim Form is utilized for billing services provided to patients under Medicare. Both forms require similar patient and provider information, diagnosis codes, and procedure descriptions.
- Medicaid Claim Form: This form serves a similar purpose for Medicaid recipients. It gathers similar information necessary for the processing of claims, including patient demographics, services rendered, and provider details.
- Workers' Compensation Claim Form: Used for work-related injuries, this form captures information akin to the Health Claim form. Both documents include sections for patient information, the nature of the injury, and the services provided.
- Insurance Reimbursement Request Form: This generic form is used for submitting expenses incurred for medical services to various insurance companies. It seeks similar information about the treatment provided, along with supporting details like payment amounts.
- Accident Claim Form: When injuries occur due to accidents, this form is utilized to summarize the incident and related medical expenses. It parallels the Health Claim form in that both require detailed accounts of the patient’s medical condition and treatments received.
- Dental Claim Form: This form is specifically for dental services but integrates many of the same concepts found in the Health Claim form, including patient and provider identification, diagnosis codes, and descriptions of services rendered.
- Chiropractic Claim Form: Tailored for chiropractic services, it shares the format and general content requirements of the Health Claim form. Both require documentation of services, diagnosis codes, and practitioner information.
- Pharmacy Claim Form: Used to bill for prescription medications, this form, like the Health Claim form, includes patient identification and medication details but focuses on pharmaceuticals rather than broader medical services.
In conclusion, while each of these forms has its specifics tailored to different types of care and coverage, they all serve a common purpose: facilitating clear communication of medical services and claims processing between patients, providers, and insurance entities.
Dos and Don'ts
When filling out the Health Claim form, it is important to follow specific guidelines to ensure a smooth submission. Below is a list of things to do and avoid in this process.
- Ensure Clarity: Fill out the form clearly, using legible handwriting or typing to avoid misunderstandings.
- Include All Required Information: Provide all necessary details, such as patient and insured information, diagnosis codes, and service dates, to prevent processing delays.
- Sign the Form: Both the patient and the authorized person must sign the relevant sections to authorize the necessary actions.
- Double-check for Accuracy: Review all entries for any errors or omissions before submission.
- Keep a Copy: Retain a copy of the completed form and any attached documents for your records.
- Do Not Leave Items Blank: Leaving required fields empty may result in a rejection or delay of your claim.
- Avoid Incorrect Codes: Using outdated or incorrect diagnosis or procedure codes can lead to payment issues.
- Neglecting to Attach Supporting Documents: Failing to include necessary medical reports or bills can hinder the claim's processing.
- Rushing the Submission: Take time to carefully complete the form rather than hurrying, which can lead to mistakes.
- Submitting Multiple Claims Duplicately: Avoid sending the same claim multiple times, as this can create confusion and delays.
Misconceptions
Below are some common misconceptions about the Health Claim form that can impact the claims process:
- The Health Claim form is the same across all insurance providers. In reality, each insurance program often has its own specific requirements and formats, which can vary significantly from one to another.
- Any errors on the form will simply delay processing. Depending on the nature of the error, it could lead to outright denial of the claim, making it crucial to ensure all information is accurate and complete before submission.
- Only medical professionals need to enter information on the form. Claimants themselves, or their authorized representatives, play a critical role in providing necessary details, particularly in sections related to patient information and authorization.
- Submitting the form once is sufficient. Some claims may require follow-up submissions, additional documentation, or clarification. Hence, monitoring the process and being prepared for further requests is important.
- Diagnosis codes are optional. This is a critical misconception. Accurate diagnosis codes must be provided to ensure that the services billed correspond correctly to the treatment provided, and they are essential for claim processing.
- The signature on the form only indicates basic agreement. In actuality, the signature signifies an understanding of the financial arrangement and acceptance of the terms of service. It is a legally binding acknowledgment.
- Claims can be submitted without documentation of medical necessity. Detailed medical reports and documentation to support the services provided are often required. Lack of this information can lead to delays or denials.
Key takeaways
- Know the Purpose: The Health Claim form is primarily used to process medical claims under various programs, including Medicare, Medicaid, and private health insurance.
- Correct Identification: Ensure that the patient’s name, birth date, and ID numbers are entered accurately to avoid processing delays.
- Signatures Matter: Both the patient and the healthcare provider must sign the form to authorize the release of medical information and payment responsibilities.
- Required Information: Fill out all relevant sections, particularly those related to diagnosis codes and dates of service, as incomplete information can lead to claim rejection.
- Coding: Use the most current ICD codes for diagnosis. Accurate coding is crucial, as incorrect codes can result in underpayment or denial of the claim.
- Itemized Charges: Ensure to list each service provided, associated charges, and relevant CPT codes for proper billing to the insurance provider.
- Submission Protocol: Claims should be sent to the appropriate address based on the specific program under which the service was rendered.
- Reviewing Guidelines: Patients and providers should familiarize themselves with the guidelines on the back of the claim form to ensure compliance with all requirements.
- Privacy Considerations: Understand the Privacy Act statement that informs users how the information collected will be utilized in the administration of the claim.
- Follow-Up: If a claim is delayed or denied, prompt follow-up with both the provider and the insurance company can help clarify any issues.
Browse Other Templates
Tdiu Va - Employers should specify the beginning and ending dates of the veteran’s employment in Section II.
Sba Debt Schedule - The current balance should reflect any payments made up to the date.