Fill Out Your Mds Form
The Minimum Data Set (MDS) form is a critical tool used in the United States to assess the health and functional status of residents in nursing homes and similar facilities. Crucial for ensuring compliance with federal regulations, this structured assessment helps establish a comprehensive profile of each resident, which is essential for creating tailored care plans. The MDS form includes sections that gather identification information, such as residency and medical details, demographics like race and language, and conditions that might affect care, including mental health evaluations. It also captures various assessments, including those required for Medicare and Medicaid, ensuring that providers have an accurate understanding of the resident’s needs. By meticulously documenting factors such as hearing, speech, vision, and other critical health indicators, the MDS is not just a formality; it is a fundamental part of how facilities provide individualized care. This comprehensive data not only assists in regulatory compliance but also enhances quality of care, ensuring each resident has access to the appropriate resources and support. Understanding the nuances of the MDS form is vital for administrators, healthcare providers, and family members advocating for optimal care for their loved ones.
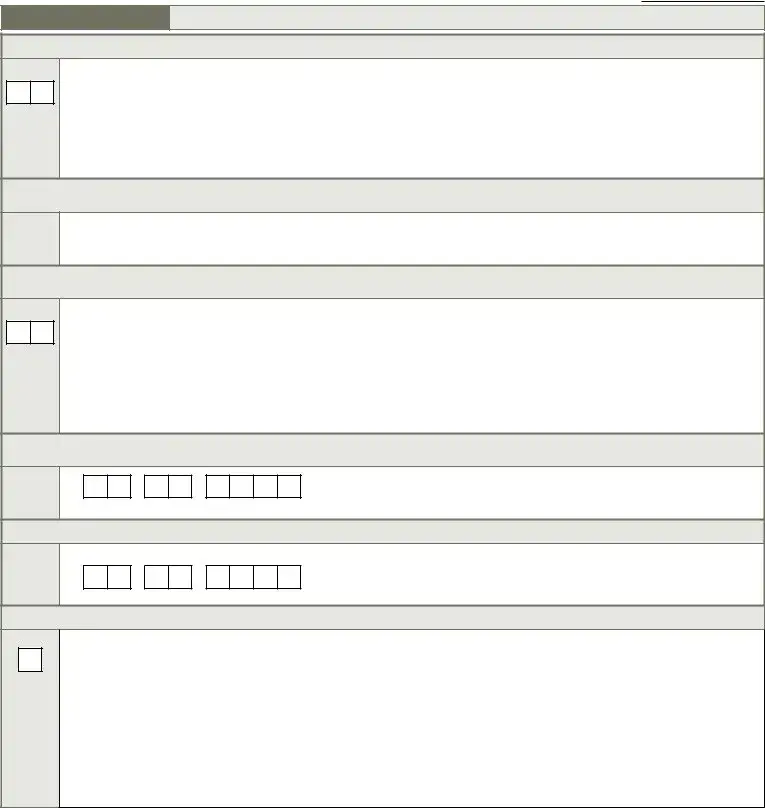
Mds Example
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
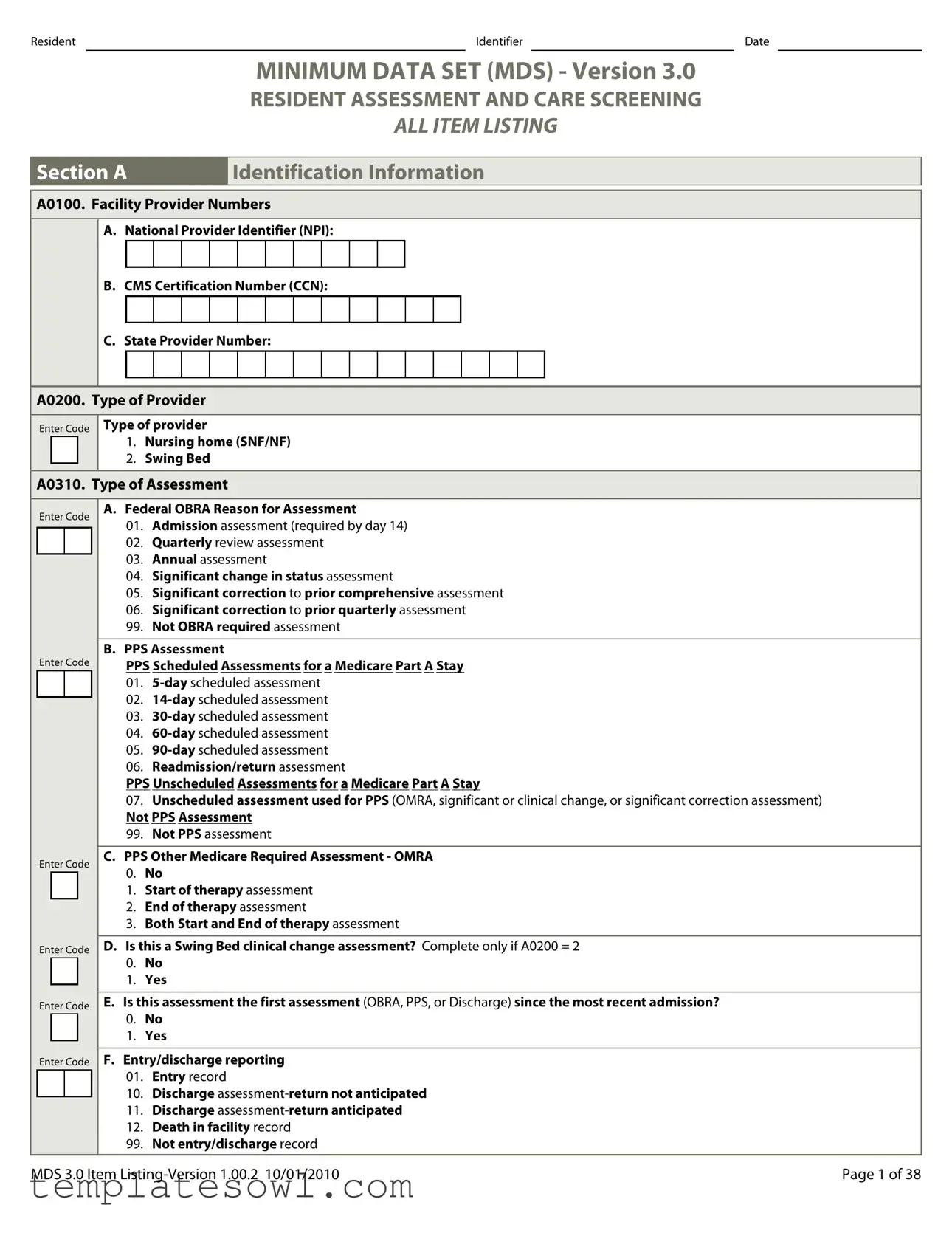
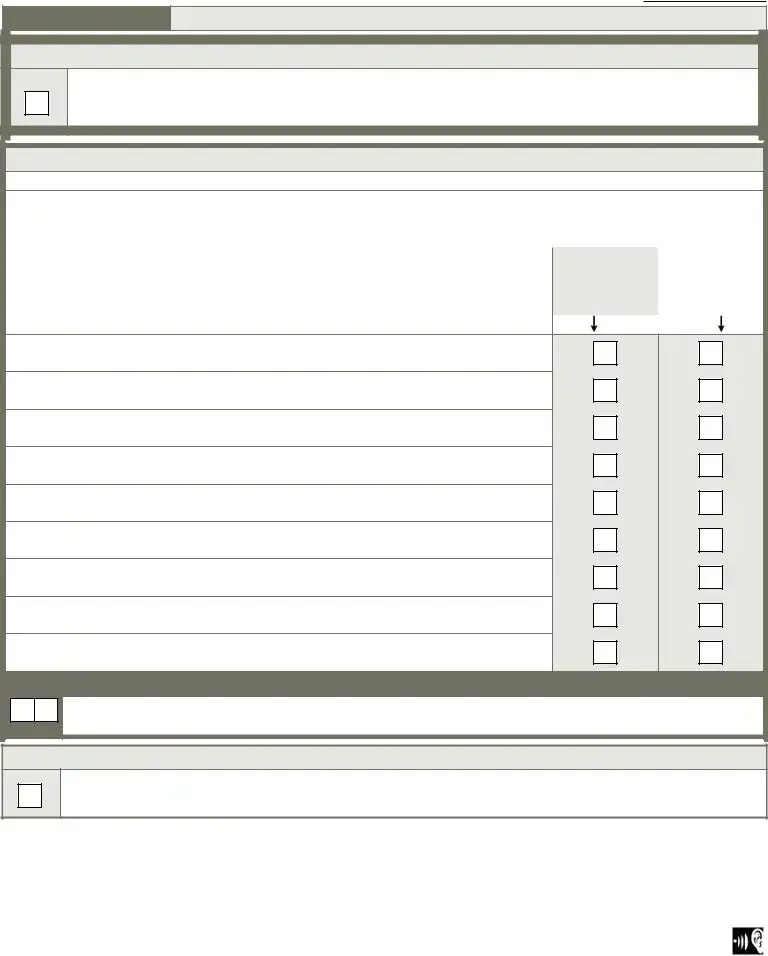
MINIMUM DATA SET (MDS) - Version 3.0
RESIDENT ASSESSMENT AND CARE SCREENING
ALL ITEM LISTING
Section A. |
Identification Information. |
A0100. Facility Provider Numbers.
A.National Provider Identifier (NPI):
B.CMS Certification Number (CCN):
C.State Provider Number:
A0200. Type of Provider.
Enter Code
Type of provider.
1.Nursing home (SNF/NF).
2.Swing Bed.
A0310. Type of Assessment.
Enter Code
Enter Code
Enter Code
Enter Code
Enter Code
Enter Code
A.Federal OBRA Reason for Assessment.
01.Admission assessment (required by day 14).
02.Quarterly review assessment.
03.Annual assessment.
04.Significant change in status assessment.
05.Significant correction to prior comprehensive assessment.
06.Significant correction to prior quarterly assessment.
99.Not OBRA required assessment.
B.PPS Assessment.
PPS Scheduled Assessments for a Medicare Part A Stay.
01.
02.
03.
04.
05.
06.Readmission/return assessment.
PPS Unscheduled Assessments for a Medicare Part A Stay.
07.Unscheduled assessment used for PPS (OMRA, significant or clinical change, or significant correction assessment).
Not PPS Assessment.
99.Not PPS assessment.
C.PPS Other Medicare Required Assessment - OMRA.
0.No...
1.Start of therapy assessment.
2.End of therapy assessment.
3.Both Start and End of therapy assessment.
D.Is this a Swing Bed clinical change assessment? Complete only if A0200 = 2.
0.No...
1.Yes.
E.Is this assessment the first assessment (OBRA, PPS, or Discharge) since the most recent admission?
0.No...
1.Yes.
F.Entry/discharge reporting
01.Entry record.
10.Discharge
11.Discharge
12.Death in facility record.
99.Not entry/discharge record.
MDS 3.0 Item |
Page 1 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
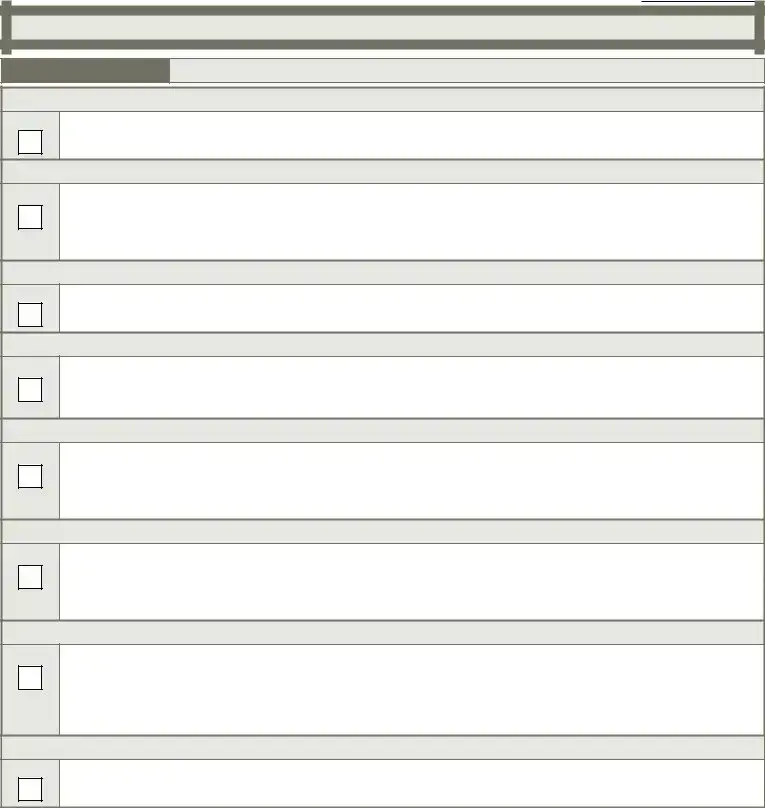
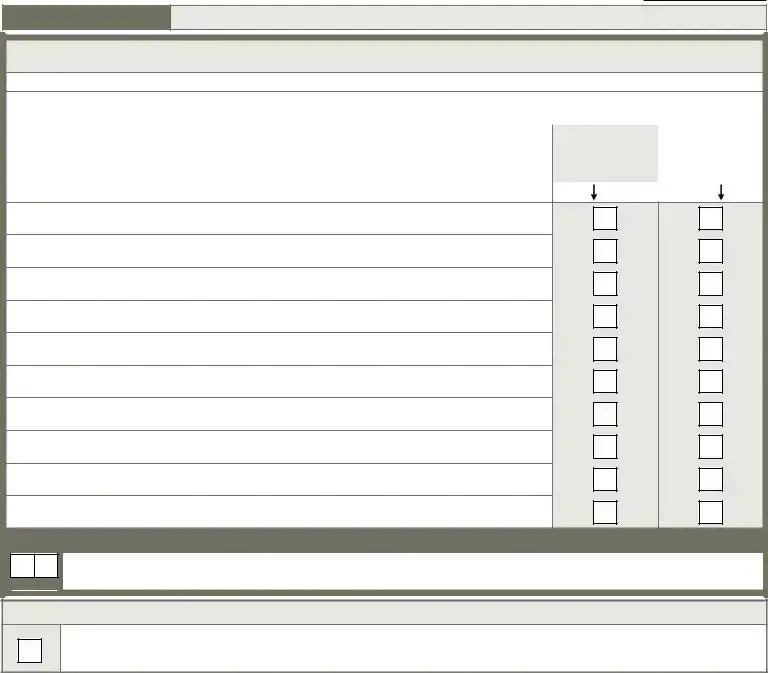
Section A.
Identification Information.
A0410. Submission Requirement.
Enter Code |
1. |
Neither federal nor state required submission. |
||
|
|
|
2. |
State but not federal required submission (FOR NURSING HOMES ONLY). |
|
|
|
3. |
Federal required submission. |
|
|
|
|
|
A0500. Legal Name of Resident.
|
A. |
First name: |
|
|
|
|
|
|
B. |
Middle initial: |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C. |
Last name: |
|
|
|
|
|
|
D. |
Suffix: |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A0600. Social Security and Medicare Numbers.
|
|
|
A. Social Security Number: |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B. Medicare number (or comparable railroad insurance number): |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A0700. Medicaid Number - Enter "+" if pending, "N" if not a Medicaid recipient. |
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A0800. Gender. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Enter Code |
1. |
Male. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
2. |
Female. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A0900. Birth Date. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
Day |
|
|
|
|
Year |
|||||||||||||||
A1000. Race/Ethnicity. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Check all that apply. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
A. American Indian or Alaska Native. |
||||||||||||||||||||||
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B. Asian. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C. Black or African American. |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
D. Hispanic or Latino. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
E. Native Hawaiian or Other Pacific Islander. |
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
F. White. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
A1100. Language. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Enter Code |
A. Does the resident need or want an interpreter to communicate with a doctor or health care staff? |
||||||||||||||||||||||||
0. |
No... |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
1. Yes Specify in A1100B, Preferred language. |
|||||||||||||||||||||
|
|
|
|
9. Unable to determine. |
|||||||||||||||||||||
|
|
|
|
||||||||||||||||||||||
|
|
|
B. Preferred language: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MDS 3.0 Item |
Page 2 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
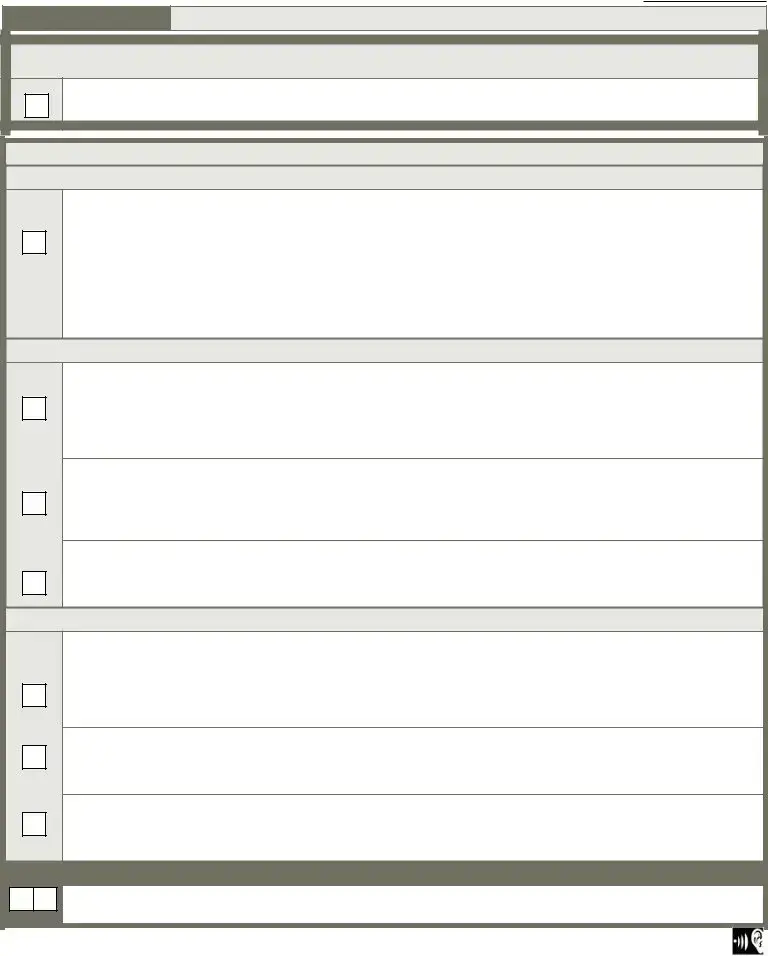
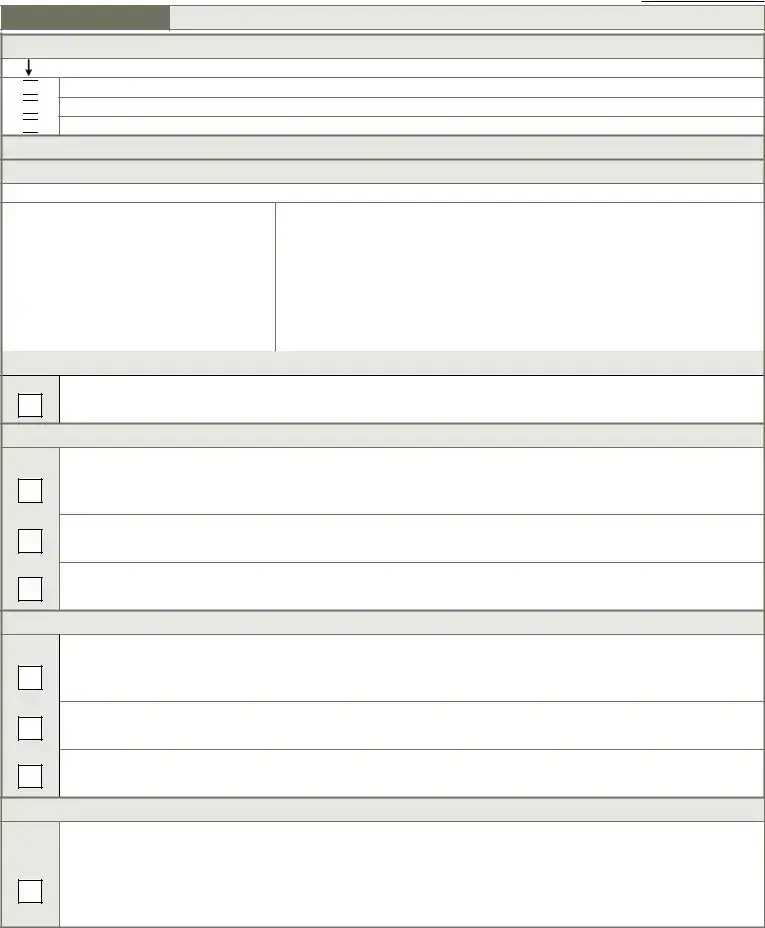
Section A.
Identification Information.
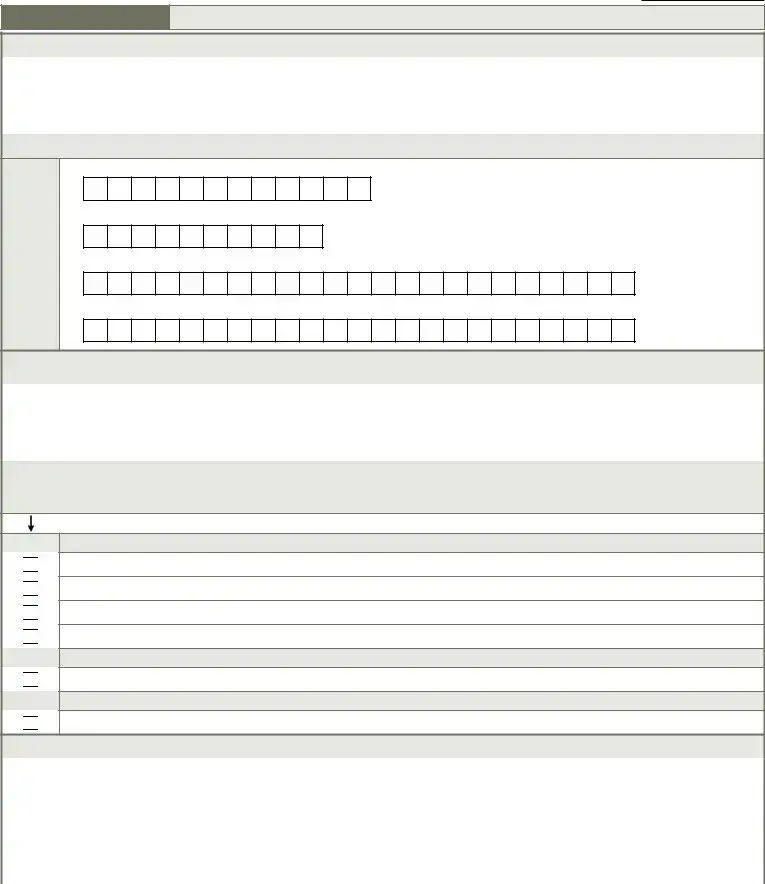
A1200. Marital Status.
Enter Code |
1. |
Never married. |
|||
2. |
Married. |
||||
|
|
|
|||
|
|
|
3. |
Widowed. |
|
|
|
|
4. |
Separated. |
|
|
|
|
5. |
Divorced. |
|
|
|
|
|
|
|
A1300. Optional Resident Items.
A. Medical record number:
B. Room number:
C. Name by which resident prefers to be addressed:
D. Lifetime occupation(s) - put "/" between two occupations:
A1500. Preadmission Screening and Resident Review (PASRR).
Complete only if A0310A = 01
Enter Code |
Has the resident been evaluated by Level II PASRR and determined to have a serious mental illness and/or mental retardation or a |
|||
|
|
|
related condition? |
|
|
|
|
0. |
No... |
|
|
|
1. |
Yes. |
|
|
|
9. |
Not a Medicaid certified unit. |
|
|
|
|
|
A1550. Conditions Related to MR/DD Status.
If the resident is 22 years of age or older, complete only if A0310A = 01.
If the resident is 21 years of age or younger, complete only if A0310A = 01, 03, 04, or 05.
Check all conditions that are related to MR/DD status that were manifested before age 22, and are likely to continue indefinitely.
MR/DD With Organic Condition.
 A. Down syndrome.
A. Down syndrome.
 B. Autism.
B. Autism.
 C. Epilepsy.
C. Epilepsy.
 D. Other organic condition related to MR/DD.
D. Other organic condition related to MR/DD.
MR/DD Without Organic Condition.
 E. MR/DD with no organic condition.
E. MR/DD with no organic condition.
No MR/DD.
 Z. None of the above.
Z. None of the above.
A1600. |
Entry Date (date of this admission/reentry into the facility). |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
Day |
|
|
Year |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A1700. |
Type of Entry. |
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Enter Code |
|
1. |
Admission. |
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
2. |
Reentry. |
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MDS 3.0 Item |
Page 3 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
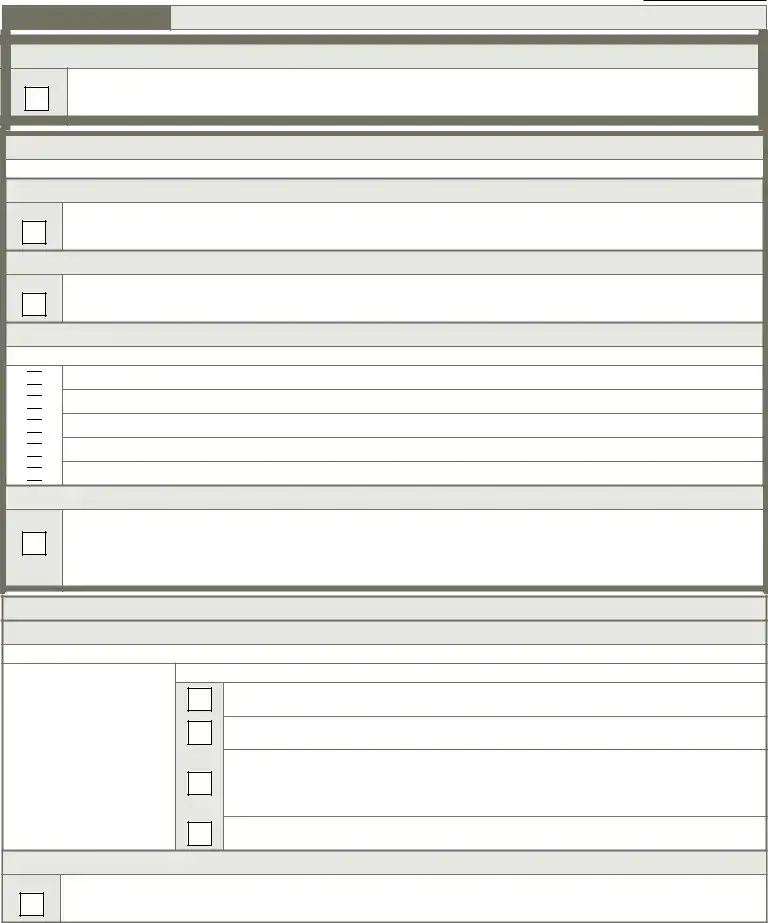
Section A.
Identification Information.
A1800. Entered From.
Enter Code
01.Community (private home/apt., board/care, assisted living, group home).
02.Another nursing home or swing bed.
03.Acute hospital.
04.Psychiatric hospital.
05.Inpatient rehabilitation facility.
06.MR/DD facility.
07.Hospice.
99.Other.
A2000. Discharge Date.
Complete only if A0310F = 10, 11, or 12
|
|
|
_ |
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
|
Day |
|
|
Year |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
A2100. Discharge Status.
Complete only if A0310F = 10, 11, or 12
Enter Code
01.Community (private home/apt., board/care, assisted living, group home).
02.Another nursing home or swing bed.
03.Acute hospital.
04.Psychiatric hospital.
05.Inpatient rehabilitation facility.
06.MR/DD facility.
07.Hospice.
08.Deceased.
99.Other.
A2200. Previous Assessment Reference Date for Significant Correction. Complete only if A0310A = 05 or 06.
_
_
Month |
Day |
Y ear |
A2300. Assessment Reference Date.
Observation end date:
_
Month Day
_
Year
A2400. Medicare Stay.
Enter Code
A.Has the resident had a
0.No  Skip to B0100, Comatose.
Skip to B0100, Comatose.
1.Yes  Continue to A2400B, Start date of most recent Medicare stay.
Continue to A2400B, Start date of most recent Medicare stay.
B. Start date of most recent Medicare stay:
|
|
_ |
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
|
Day |
|
|
Year |
||||
C. End date of most recent Medicare stay - Enter dashes if stay is ongoing:
|
|
_ |
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Month |
|
Day |
|
|
Year |
||||
MDS 3.0 Item |
Page 4 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Look back period for all items is 7 days unless another time frame is indicated.
Section B.
Hearing, Speech, and Vision.
B0100. Comatose.
Enter Code
Persistent vegetative state/no discernible consciousness.
0.No  Continue to B0200, Hearing.
Continue to B0200, Hearing.
1.Yes  Skip to G0110, Activities of Daily Living (ADL) Assistance.
Skip to G0110, Activities of Daily Living (ADL) Assistance.
B0200. Hearing.
Enter Code
Ability to hear (with hearing aid or hearing appliances if normally used).
0.Adequate - no difficulty in normal conversation, social interaction, listening to TV.
1.Minimal difficulty - difficulty in some environments (e.g., when person speaks softly or setting is noisy).
2.Moderate difficulty - speaker has to increase volume and speak distinctly.
3.Highly impaired - absence of useful hearing.
B0300. Hearing Aid.
Enter Code
Hearing aid or other hearing appliance used in completing B0200, Hearing.
0.No...
1.Yes.
B0600. Speech Clarity.
Enter Code
Select best description of speech pattern.
0.Clear speech - distinct intelligible words.
1.Unclear speech - slurred or mumbled words.
2.No speech - absence of spoken words.
B0700. Makes Self Understood.
Enter Code
Ability to express ideas and wants, consider both verbal and
0.Understood.
1.Usually understood - difficulty communicating some words or finishing thoughts but is able if prompted or given time.
2.Sometimes understood - ability is limited to making concrete requests.
3.Rarely/never understood.
B0800. Ability To Understand Others.
Enter Code
Understanding verbal content, however able (with hearing aid or device if used).
0.Understands - clear comprehension.
1.Usually understands - misses some part/intent of message but comprehends most conversation.
2.Sometimes understands - responds adequately to simple, direct communication only.
3.Rarely/never understands.
B1000. Vision.
Enter Code
Ability to see in adequate light (with glasses or other visual appliances).
0.Adequate - sees fine detail, including regular print in newspapers/books.
1.Impaired - sees large print, but not regular print in newspapers/books.
2.Moderately impaired - limited vision; not able to see newspaper headlines but can identify objects.
3.Highly impaired - object identification in question, but eyes appear to follow objects.
4.Severely impaired - no vision or sees only light, colors or shapes; eyes do not appear to follow objects.
B1200. Corrective Lenses.
Enter Code
Corrective lenses (contacts, glasses, or magnifying glass) used in completing B1000, Vision.
0.No...
1.Yes.
MDS 3.0 Item |
Page 5 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Section C.
Cognitive Patterns.
C0100. Should Brief Interview for Mental Status
Enter Code
0.No (resident is rarely/never understood)  Skip to and complete
Skip to and complete
1.Yes  Continue to C0200, Repetition of Three Words.
Continue to C0200, Repetition of Three Words.
Brief Interview for Mental Status (BIMS).
C0200. Repetition of Three Words.
Enter Code
Ask resident: “I am going to say three words for you to remember. Please repeat the words after I have said all three.
The words are: sock, blue, and bed. Now tell me the three words.”
Number of words repeated after first attempt.
0.None.
1.One.
2.Two.
3.Three.
After the resident's first attempt, repeat the words using cues ("sock, something to wear; blue, a color; bed, a piece of furniture"). You may repeat the words up to two more times.
C0300. Temporal Orientation (orientation to year, month, and day).
Enter Code
Enter Code
Enter Code
Ask resident: "Please tell me what year it is right now."
A.Able to report correct year.
0.Missed by > 5 years or no answer.
1.Missed by
2.Missed by 1 year.
3.Correct.
Ask resident: "What month are we in right now?"
B.Able to report correct month.
0.Missed by > 1 month or no answer.
1.Missed by 6 days to 1 month.
2.Accurate within 5 days.
Ask resident: "What day of the week is today?"
C.Able to report correct day of the week.
0.Incorrect or no answer.
1.Correct.
C0400. Recall.
Enter Code
Enter Code
Enter Code
Ask resident: "Let's go back to an earlier question. What were those three words that I asked you to repeat?" If unable to remember a word, give cue (something to wear; a color; a piece of furniture) for that word.
A.Able to recall "sock".
0.No - could not recall.
1.Yes, after cueing ("something to wear").
2.Yes, no cue required.
B.Able to recall "blue".
0.No - could not recall.
1.Yes, after cueing ("a color").
2.Yes, no cue required.
C.Able to recall "bed".
0.No - could not recall.
1.Yes, after cueing ("a piece of furniture").
2.Yes, no cue required.
C0500. Summary Score.
Enter Score
Add scores for questions
Enter 99 if the resident was unable to complete the interview.
MDS 3.0 Item |
Page 6 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Section C.
Cognitive Patterns.
C0600. Should the Staff Assessment for Mental Status (C0700 - C1000) be Conducted?
Enter Code
0.No (resident was able to complete interview )  Skip to C1300, Signs and Symptoms of Delirium.
Skip to C1300, Signs and Symptoms of Delirium.
1.Yes (resident was unable to complete interview)  Continue to C0700,
Continue to C0700,
Staff Assessment for Mental Status.
Do not conduct if Brief Interview for Mental Status
C0700.
Enter Code
Seems or appears to recall after 5 minutes.
0.Memory OK.
1.Memory problem.
C0800.
Enter Code
Seems or appears to recall long past.
0.Memory OK.
1.Memory problem.
C0900. Memory/Recall Ability.
 Check all that the resident was normally able to recall.
Check all that the resident was normally able to recall.
 A. Current season.
A. Current season.
 B. Location of own room.
B. Location of own room.
 C. Staff names and faces.
C. Staff names and faces.
 D. That he or she is in a nursing home.
D. That he or she is in a nursing home.
 Z. None of the above were recalled.
Z. None of the above were recalled.
C1000. Cognitive Skills for Daily Decision Making.
Enter Code
Made decisions regarding tasks of daily life.
0.Independent - decisions consistent/reasonable.
1.Modified independence - some difficulty in new situations only.
2.Moderately impaired - decisions poor; cues/supervision required.
3.Severely impaired - never/rarely made decisions.
Delirium.
C1300. Signs and Symptoms of Delirium (from CAM©).
Code after completing Brief Interview for Mental Status or Staff Assessment, and reviewing medical record.
Coding:
0.Behavior not present .
1.Behavior continuously present, does not fluctuate.
2.Behavior present, fluctuates (comes and goes, changes in severity).
 Enter Codes in Boxes.
Enter Codes in Boxes.
A.Inattention - Did the resident have difficulty focusing attention (easily distracted, out of touch or difficulty following what was said)?
B.Disorganized thinking - Was the resident's thinking disorganized or incoherent (rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject)?
C.Altered level of consciousness - Did the resident have altered level of consciousness (e.g., vigilant - startled easily to any sound or touch; lethargic - repeatedly dozed off when being asked questions, but responded to voice or touch; stuporous - very difficult to arouse and keep aroused for the interview; comatose - could not be aroused)?
D.Psychomotor retardation- Did the resident have an unusually decreased level of activity such as sluggishness, staring into space, staying in one position, moving very slowly?
C1600. Acute Onset Mental Status Change.
Enter Code
Is there evidence of an acute change in mental status from the resident's baseline?
0.No...
1.Yes.
Copyright © 1990 Annals of Internal Medicine. All rights reserved. Adapted with permission. |
|
MDS 3.0 Item |
Page 7 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Section D.
Mood.
D0100. Should Resident Mood Interview be Conducted? - Attempt to conduct interview with all residents.
Enter Code
0.No (resident is rarely/never understood)  Skip to and complete
Skip to and complete
1.Yes  Continue to D0200, Resident Mood Interview
Continue to D0200, Resident Mood Interview
D0200. Resident Mood Interview
Say to resident: "Over the last 2 weeks, have you been bothered by any of the following problems?"
If symptom is present, enter 1 (yes) in column 1, Symptom Presence.
If yes in column 1, then ask the resident: "About how often have you been bothered by this?"
Read and show the resident a card with the symptom frequency choices. Indicate response in column 2, Symptom Frequency.
1. Symptom Presence. |
2. Symptom Frequency. |
1. |
2. |
|
||
0. |
No (enter 0 in column 2). |
0. |
Never or 1 day. |
|
||
Symptom |
Symptom |
|
||||
1. |
Yes (enter |
1. |
|
|||
Presence. |
Frequency. |
|
||||
9. |
No response (leave column 2 |
2. |
|
|||
|
blank). |
3. |
Enter Scores in Boxes |
|
||
|
|
|
|
|
|
|
A. Little interest or pleasure in doing things.
B. Feeling down, depressed, or hopeless.
C. Trouble falling or staying asleep, or sleeping too much.
D. Feeling tired or having little energy.
E. Poor appetite or overeating.
F.Feeling bad about yourself - or that you are a failure or have let yourself or your family down.
G. Trouble concentrating on things, such as reading the newspaper or watching television.
H.Moving or speaking so slowly that other people could have noticed. Or the opposite - being so fidgety or restless that you have been moving around a lot more than usual.
I. Thoughts that you would be better off dead, or of hurting yourself in some way.
D0300. Total Severity Score.
Enter Score |
Add scores for all frequency responses in Column 2, Symptom Frequency. Total score must be between 00 and 27. Enter 99 if unable to complete interview (i.e., Symptom Frequency is blank for 3 or more items).
D0350. Safety Notification - Complete only if D0200I1 = 1 indicating possibility of resident self harm.
Enter Code
Was responsible staff or provider informed that there is a potential for resident self harm?
0.No...
1.Yes.
Copyright © Pfizer Inc. All rights reserved. Reproduced with permission. |
|
MDS 3.0 Item |
Page 8 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Section D.
Mood.
D0500. Staff Assessment of Resident Mood
Do not conduct if Resident Mood Interview
Over the last 2 weeks, did the resident have any of the following problems or behaviors?
If symptom is present, enter 1 (yes) in column 1, Symptom Presence.
Then move to column 2, Symptom Frequency, and indicate symptom frequency.
1. Symptom Presence. |
2. Symptom Frequency. |
1. |
2. |
|
||
0. |
No (enter 0 in column 2). |
0. |
Never or 1 day. |
|
||
Symptom |
Symptom |
|
||||
1. |
Yes (enter |
1. |
|
|||
Presence. |
Frequency. |
|
||||
|
|
2. |
|
|||
|
|
|
|
|
||
|
|
3. |
Enter Scores in Boxes |
|
||
|
|
|
|
|
|
|
A. Little interest or pleasure in doing things.
B. Feeling or appearing down, depressed, or hopeless.
C. Trouble falling or staying asleep, or sleeping too much.
D. Feeling tired or having little energy.
E. Poor appetite or overeating.
F. Indicating that s/he feels bad about self, is a failure, or has let self or family down.
G. Trouble concentrating on things, such as reading the newspaper or watching television.
H.Moving or speaking so slowly that other people have noticed. Or the opposite - being so fidgety or restless that s/he has been moving around a lot more than usual.
I. States that life isn't worth living, wishes for death, or attempts to harm self.
J. Being
D0600. Total Severity Score.
Enter Score |
Add scores for all frequency responses in Column 2, Symptom Frequency. Total score must be between 00 and 30.
D0650. Safety Notification - Complete only if D0500I1 = 1 indicating possibility of resident self harm.
Enter Code
Was responsible staff or provider informed that there is a potential for resident self harm?
0.No...
1.Yes.
* Copyright © Pfizer Inc. All rights reserved. |
|
MDS 3.0 Item |
Page 9 of 38 |
Resident |
|
Identifier |
|
Date |
|
|
|
|
|
Section E.
Behavior.
E0100. Psychosis.
Check all that apply
 A. Hallucinations (perceptual experiences in the absence of real external sensory stimuli).
A. Hallucinations (perceptual experiences in the absence of real external sensory stimuli).
 B. Delusions (misconceptions or beliefs that are firmly held, contrary to reality).
B. Delusions (misconceptions or beliefs that are firmly held, contrary to reality).
 Z. None of the above.
Z. None of the above.
Behavioral Symptoms.
E0200. Behavioral Symptom - Presence & Frequency.
Note presence of symptoms and their frequency.
 Enter Codes in Boxes.
Enter Codes in Boxes.
Coding: |
|
|
|
|
A. |
Physical behavioral symptoms directed toward others (e.g., hitting, |
|
|
|
|
|||||
|
|
|
|
kicking, pushing, scratching, grabbing, abusing others sexually). |
|||
0. |
Behavior not exhibited. |
|
|
|
|
||
|
|
|
|
|
|||
1. |
Behavior of this type occurred 1 to 3 days. |
|
|
|
B. |
Verbal behavioral symptoms directed toward others (e.g., threatening |
|
|
|
|
|
others, screaming at others, cursing at others). |
|||
2. |
Behavior of this type occurred 4 to 6 days, |
|
|
|
|
||
|
|
|
|
|
|||
|
but less than daily. |
|
|
|
C. |
Other behavioral symptoms not directed toward others (e.g., physical |
|
|
|
|
|
||||
3. |
Behavior of this type occurred daily. |
|
|
|
|
symptoms such as hitting or scratching self, pacing, rummaging, public |
|
|
|
|
|
|
|
|
sexual acts, disrobing in public, throwing or smearing food or bodily wastes, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
or verbal/vocal symptoms like screaming, disruptive sounds). |
|
|
|
|
|
|
|
|
E0300. Overall Presence of Behavioral Symptoms.
Enter Code
Were any behavioral symptoms in questions E0200 coded 1, 2, or 3?
0.No  Skip to E0800, Rejection of Care.
Skip to E0800, Rejection of Care.
1.Yes  Considering all of E0200, Behavioral Symptoms, answer E0500 and E0600 below.
Considering all of E0200, Behavioral Symptoms, answer E0500 and E0600 below.
E0500. Impact on Resident.
Enter Code
Enter Code
Enter Code
Did any of the identified symptom(s):
A.Put the resident at significant risk for physical illness or injury?
0.No...
1.Yes.
B.Significantly interfere with the resident's care?
0.No...
1.Yes.
C.Significantly interfere with the resident's participation in activities or social interactions?
0.No...
1.Yes.
E0600. Impact on Others.
Enter Code
Enter Code
Enter Code
Did any of the identified symptom(s):
A.Put others at significant risk for physical injury?
0.No...
1.Yes.
B.Significantly intrude on the privacy or activity of others?
0.No...
1.Yes.
C.Significantly disrupt care or living environment?
0.No...
1.Yes.
E0800. Rejection of Care - Presence & Frequency.
Enter Code
Did the resident reject evaluation or care (e.g., bloodwork, taking medications, ADL assistance) that is necessary to achieve the resident's goals for health and
0.Behavior not exhibited.
1.Behavior of this type occurred 1 to 3 days.
2.Behavior of this type occurred 4 to 6 days, but less than daily.
3.Behavior of this type occurred daily.
MDS 3.0 Item |
Page 10 of 38 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Version | The MDS form is currently in Version 3.0, which was implemented as of October 1, 2010. |
| Purpose | The MDS is used for resident assessment and care planning in skilled nursing facilities. |
| Submission Requirements | Submission may be required by both federal and state laws, particularly for nursing homes. |
| Assessment Types | Assessment is categorized into various types, including admission, annual, and significant change assessments. |
| Resident Identification | Specific resident identifiers are mandatory, including Social Security and Medicare numbers. |
| Data Collection Period | The look-back period for data collection on most items is seven days, unless otherwise specified. |
| Governing Laws | The MDS is governed by federal regulations under the Omnibus Budget Reconciliation Act (OBRA) and relevant state laws. |
| Language Needs | Facilities must identify residents who require interpreter services to ensure effective communication. |
| Comorbidity Screening | The MDS includes questions about coexisting conditions, particularly for mental health concerns. |
Guidelines on Utilizing Mds
Filling out the MDS form can seem daunting, but taking it step by step can simplify the process. After completing the MDS form, various care decisions and assessments are made regarding the resident’s health and needs. Here’s how to get started.
- Begin with Identification Information: Fill in the Resident Identifier and the Date at the top of the form.
- Enter Facility Provider Numbers: Input the National Provider Identifier (NPI), CMS Certification Number (CCN), and State Provider Number.
- Type of Provider: Select the appropriate type of provider by entering the corresponding code.
- Type of Assessment: Choose the type of assessment being conducted by entering the proper codes.
- Submission Requirement: Indicate the submission requirement by selecting the appropriate code.
- Provide Resident's Legal Name: Enter the first name, middle initial, last name, and any suffix.
- Social Security and Medicare Numbers: Fill in the necessary Social Security Number and Medicare number.
- Medicaid Number: Indicate whether the resident has a Medicaid number, using "+" for pending or "N" if not a recipient.
- Gender: Choose the gender of the resident by entering the appropriate code.
- Birth Date: Enter the resident's birth date in the designated format (Month, Day, Year).
- Race/Ethnicity: Check all applicable race/ethnicity categories.
- Language Needs: Indicate whether an interpreter is needed and provide the preferred language, if applicable.
- Marital Status: Fill in the marital status by entering the corresponding code.
- Optional Resident Items: Provide optional information such as medical record number, room number, and preferred name.
- Preadmission Screening: Complete the required section if applicable.
- Entry Information: Fill in the entry date, type of entry, and the place the resident came from.
- Discharge Information: If applicable, fill in the discharge date and status.
- Assessment Reference Dates: Complete any required dates related to prior assessments.
- Medicare Stay: Indicate whether the resident has had any Medicare-covered stay and provide the relevant dates.
- Hearing, Speech, and Vision: Complete the assessment items related to hearing, speech, and vision abilities.
What You Should Know About This Form
What is the MDS form?
The Minimum Data Set (MDS) form is a standardized assessment tool used in nursing homes and other long-term care facilities. It collects important information about each resident's clinical status, functional capabilities, and care needs. This data helps care staff develop individualized care plans and monitor resident health over time.
Who needs to fill out the MDS form?
The MDS form is typically completed by a licensed nurse or qualified healthcare professional involved in the resident's care. This assessment is mandatory for every resident upon admission to a nursing home and is also required regularly thereafter, including quarterly and annually.
What kind of information does the MDS form collect?
The MDS form gathers a variety of information. This includes resident identification details, medical history, health conditions, cognitive function, and ability to perform daily activities. It also captures information about hearing, vision, and communication skills. These data points help ensure that residents receive appropriate care tailored to their specific needs.
How often is the MDS form updated?
The MDS form must be updated every 12 months during an annual assessment. Additionally, it should be revised if there is a significant change in the resident's condition or circumstances. Regular quarterly assessments are also required to track any ongoing changes in the resident's health status.
Why is the MDS form important?
The MDS form plays a critical role in ensuring quality care for residents in long-term care facilities. By systematically collecting and analyzing patient data, healthcare providers can enhance care plans, comply with regulatory requirements, and pursue reimbursement for services provided under Medicare and Medicaid programs.
What happens if the MDS form is not completed correctly?
Inaccurate or incomplete MDS forms can lead to issues such as improper care plans, denial of Medicare or Medicaid reimbursement, and potential penalties for the facility. Therefore, it’s crucial for healthcare professionals to be thorough and precise when completing the form to avoid these complications and ensure residents receive the best possible care.
Common mistakes
Filling out the MDS form correctly is crucial for accurately assessing residents in nursing facilities. However, mistakes often occur that can lead to significant repercussions. One common error is incomplete resident identification information. Failing to provide the full legal name of the resident, including middle initial and suffix, can lead to confusion and misidentification.
An additional mistake involves the submission requirements. Incorrectly marking the submission requirement can result in delays in required reports. It's essential to double-check whether the assessment is federally required or only required by the state. Documentation of provider numbers can also be a stumbling block. Omitting the National Provider Identifier (NPI) or filling in outdated information can complicate the submission process.
Another frequent issue is inaccurately coding the type of provider. There are specific codes for nursing homes and swing beds, and using the wrong code may impact compliance and reimbursement processes. Similarly, errors in selecting the appropriate type of assessment can lead to serious issues. For example, marking a quarterly review when an annual assessment is required could violate regulations.
When entering a resident's birth date, incorrect formatting is a common mistake. The date should be entered in MM/DD/YYYY format. Failing to adhere to this standard can lead to confusion and errors in the system. Additionally, the section on race/ethnicity often contains errors, as it's important to check all that apply and ensure that all options are considered carefully.
Missing or inaccurately completed medical record numbers can lead to confusion and chaos within medical and legal records. Each number serves as a unique identifier crucial for policymakers, family members, and health care providers. Similarly, incorrect entries in the therapy assessment section may result in inadequate care plans, as accurate therapy-related assessments provide necessary insights for treatment.
Other pitfalls include misrepresenting marital status or failing to provide the Medicaid number correctly. Options here must align with the resident's current status. Failure to do so may prevent appropriate coverage for care. Finally, language needs and preferences can be overlooked, which could complicate communication between residents and healthcare staff.
These common mistakes can complicate the care process. Attending to every detail when completing the MDS form ensures that residents receive the most appropriate and timely care possible.
Documents used along the form
The Minimum Data Set (MDS) form is a critical document used in healthcare settings to assess resident health, demographic information, and care needs in facilities such as nursing homes. Along with the MDS form, several other documents may be commonly used to support the assessment process and care planning. Here is a list of relevant forms and documents.
- Care Plan: This document outlines the specific care and services that the resident will receive. It is based on the assessment results and focuses on individualized goals and interventions.
- Resident Assessment Protocols (RAPs): These are supplementary tools that provide guidance on further assessments needed for specific health issues identified during the MDS assessment.
- Patient History Forms: These forms collect background information on the resident, including past medical history, medications, and any allergies, ensuring that caregivers have a comprehensive understanding of the resident's needs.
- Physician Orders: This document details specific treatments and medications prescribed by the resident's physician, based on assessment findings and the care plan.
- Functional Assessment Tools: These tools evaluate the resident's ability to perform daily activities. Information gathered helps in tailoring care to enhance the resident's independence and quality of life.
- Incident Reports: These reports record any unexpected events, accidents, or safety issues involving residents. They are vital for quality assurance and evaluating the effectiveness of safety protocols.
- Discharge Summary: This document outlines the resident's status upon discharge, including any follow-up care needed and instructions for ongoing treatment outside the facility.
Each of these documents plays a significant role in the overall care of residents in healthcare facilities. Accurate completion and maintenance of these records ensure that residents receive high-quality and personalized care.
Similar forms
- Patient Assessment Instrument (PAI): Similar to the MDS form, the PAI collects comprehensive data about a patient's health and wellness needs in a clinical setting. Both documents aim to ensure proper care planning and quality assessments specific to patient needs.
- Resident Assessment Protocol (RAP): The RAP works closely with the MDS by providing a structured approach to assess specific issues identified during the MDS evaluation. It helps in creating targeted care plans to address particular health concerns.
- Care Plan: After completing the MDS assessment, a care plan is developed, which outlines the specific services and interventions needed for a resident's care. Both documents work together to promote effective care delivery.
- Patient Care Summary (PCS): The PCS provides a concise overview of key information from various assessments, including the MDS. This summary is valuable for caregivers and healthcare providers for quick reference and decision-making regarding the resident’s care.
- Minimum Data Set for Home Health Care (MDS-HHC): This version of the MDS is tailored for home health care settings, sharing many similarities with the MDS used in long-term care facilities. Both facilitate ongoing monitoring of patient conditions and the effectiveness of care plans.
- Quality Assessment and Performance Improvement (QAPI) Plan: The QAPI utilizes data from the MDS to evaluate a facility's performance in delivering quality care. The insights drawn help organizations enhance services and comply with regulations, similar to how the MDS informs care delivery.
Dos and Don'ts
When filling out the MDS form, consider the following do's and don'ts:
- Do: Double-check all resident identifiers to ensure accuracy.
- Do: Provide complete and clear information for each section.
- Do: Use the most recent assessment data available.
- Do: Confirm that all necessary signatures are in place before submission.
- Don't: Leave any required fields blank.
- Don't: Use abbreviations that may cause confusion.
- Don't: Submit the form without accurate dates for entries and assessments.
- Don't: Rely on memory; always refer to documentation for precise details.
Misconceptions
- Misconception 1: The MDS form is solely for nursing homes.
- Misconception 2: The MDS form is only necessary at admission.
- Misconception 3: Completing the MDS form is a quick task.
- Misconception 4: The MDS is irrelevant for reimbursement.
While the MDS (Minimum Data Set) is widely associated with nursing home assessments, it can also apply to swing beds and other healthcare facilities. It serves as a comprehensive tool for evaluating resident care across various settings.
Many believe that the MDS is required only during the initial admission of a resident. In reality, periodic assessments, including quarterly and annual reviews, are mandated to ensure that resident needs are consistently addressed and care plans are updated accordingly.
Some think that filling out the MDS form can be done swiftly. However, the detailed nature of the form demands careful consideration and data collection, often requiring inputs from various healthcare professionals to ensure accuracy and compliance.
This misunderstanding overlooks the critical role of the MDS in the reimbursement process. Accurate completion of the form is essential, as it directly influences funding and resource allocation for the care of residents, especially in a Medicare Part A stay.
Key takeaways
The MDS form is crucial for resident assessment, driving care planning and reimbursement.
Each section must be completed with accuracy, including identifying the resident's legal name, Social Security number, and Medicare details.
Regular updates are essential. Be aware of timing requirements for different assessments, such as admission and quarterly reviews.
Clarify the resident's communication needs early on, including preferred language and any need for interpreters.
Incomplete sections can delay processing and affect quality of care, so thoroughness is key.
Browse Other Templates
T-22b Form - Section A outlines necessary vehicle details that need to be thoroughly recorded.
Background Investigation Questionnaire,National Security Evaluation Form,Federal Security Clearance Application,Security Clearance Questionnaire,Classified Access Application,Government Background Disclosure Form,Security Eligibility Questionnaire,Pe - Certain sections concern financial responsibilities and legal matters needing disclosure.
London Visa Process - Identify your main reason for visiting the UK in the form.