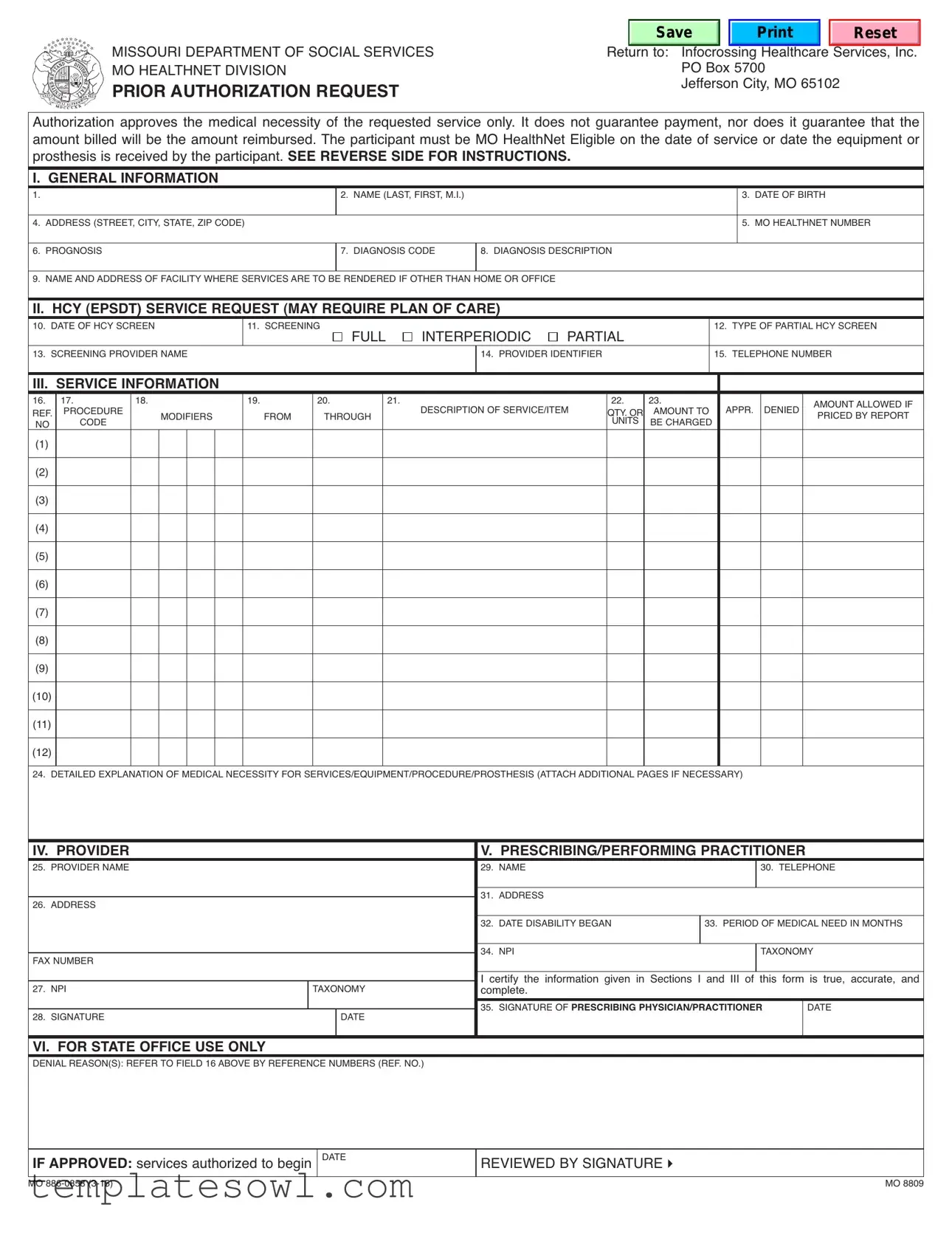
Fill Out Your Mo 886 0858 Form
The MO 886 0858 form serves as a crucial tool within the Missouri Department of Social Services for managing prior authorization requests related to healthcare services. This form helps ensure that medical services or equipment meet the necessary medical criteria before being rendered to a participant. However, it's important to understand that completion of this form does not guarantee payment or confirm that the billed amount will be reimbursed. The participant's eligibility under the MO HealthNet program is a critical factor, as services must be requested on or after the date of eligibility. The form requires comprehensive information, including the participant's name, date of birth, and health information such as diagnosis codes and prognosis. It also encompasses sections for providers seeking authorization, detailed explanations of the medical necessity of services or equipment, and information about the prescribing or performing practitioner. Additional instructions are provided on the form to help ensure accuracy in submission, and the review and approval process by state office personnel includes specific remarks about the outcome of the request.
Mo 886 0858 Example
|
|
missouri department of social services |
|
|
|
Save |
Reset |
|||||||||
|
|
|
|
return to: infocrossing healthcare services, inc. |
||||||||||||
|
|
mo healthnet division |
|
|
|
|
|
|
|
po box 5700 |
|
|||||
|
|
PRIOR AUTHORIzATION REQUEST |
|
|
|
|
Jefferson city, mo 65102 |
|||||||||
authorization approves the medical necessity of the requested service only. it does not guarantee payment, nor does it guarantee that the |
||||||||||||||||
amount billed will be the amount reimbursed. the participant must be mo healthnet eligible on the date of service or date the equipment or |
||||||||||||||||
prosthesis is received by the participant. SEE REVERSE SIDE FOR INSTRUCTIONS. |
|
|
|
|
||||||||||||
I. GENERAL INFORMATION |
|
|
|
2. name (last, first, m.i.) |
|
|
|
|
3. date of birth |
|||||||
1. |
|
|
|
|
|
|
|
|
|
|
|
|||||
4. address (street, city, state, zip code) |
|
|
|
|
|
|
|
|
|
|
5. mo healthnet number |
|||||
6. prognosis |
|
|
|
|
|
|
7. diagnosis code |
8. diagnosis description |
|
|
|
|||||
9. name and address of facility where services are to be rendered if other than home or office |
|
|
|
|
|
|||||||||||
II. HCY (EPSDT) SERVICE REQUEST (MAY REQUIRE PLAN OF CARE) |
partial |
|
|
|
||||||||||||
10. date of hcy screen |
|
11. screening |
full |
interperiodic |
|
12. type of partial hcy screen |
||||||||||
13. screening provider name |
|
|
|
|
|
|
14. provider identifier |
|
15. telephone number |
|||||||
III. SERVICE INFORMATION |
19. |
|
20. |
|
21. |
|
|
|
22. |
23. |
|
|
||||
16. |
17. |
|
18. |
|
|
|
description of service/item |
appr. denied |
amount allowed if |
|||||||
ref. |
procedure |
|
modifiers |
|
from |
through |
|
qty. or |
amount to |
|||||||
no |
code |
|
|
|
|
|
|
|
units |
be charged |
|
priced by report |
||||
(1) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(2) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(3) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(4) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(5) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(6) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(8) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(9) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(10) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(11) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(12) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
24. detailed explanation of medical necessity for services/equipment/procedure/prosthesis (attach additional pages if necessary) |
|
|||||||||||||||
IV. PROVIDER |
|
|
|
|
|
|
|
|
V. PRESCRIBING/PERFORMING PRACTITIONER |
|
||||||
25. provider name |
|
|
|
|
|
|
|
|
29. name |
|
|
|
30. telephone |
|||
26. address |
|
|
|
|
|
|
|
|
|
31. address |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
32. date disability began |
33. period of medical need in months |
||||||
|
|
|
|
|
|
|
|
|
|
|
||||||
fax number |
|
|
|
|
|
|
|
|
|
34. npi |
|
|
|
taxonomy |
||
|
|
|
|
|
|
|
|
|
i certify the information given in sections i and iii of this form is true, accurate, and |
|||||||
27. npi |
|
|
|
|
|
taxonomy |
|
|
||||||||
|
|
|
|
|
|
|
complete. |
|
PRESCRIBING PHYSICIAN/PRACTITIONER |
|
||||||
28. signature |
|
|
|
|
|
|
date |
|
|
35. signature of |
date |
|||||
VI. FOR STATE OFFICE USE ONLY |
|
|
|
|
|
|
|
|
|
|
||||||
denial reason(s): refer to field 16 above by reference numbers (ref. no.) |
|
|
|
|
|
|
||||||||||
IF APPROVED: services authorized to begin
mo
date
reviewed by signature4
mo 8809
INSTRUCTIONS FOR COMPLETION
I. GENERAL INFORMATION - To be completed by the provider requesting the prior authorization. 1. leave blank
2. participant’s name - enter the participant’s name as it appears on the mo healthnet id card. enter the participant’s current address.
3. date of birth - enter the participant’s date of birth.
4. address - enter the participant’s address, city, state, and zip.
5. mo healthnet number - enter the participant’s
6. prognosis - enter the participant’s prognosis.
7. diagnosis code - enter the diagnosis code(s).
8. diagnosis description - enter the diagnosis description. if there is more than one diagnosis, enter all descriptions appropriate to the services being requested.
9. name and address of the facility where services are to be rendered if service is to be provided other than home or office.
II. HCY SERVICE REQUEST (Plan of care may be required, see your provider manual) 10. date of hcy screen - enter the date the hcy screen was done.
11. screening - check whether the screening performed was full, interperiodic, or partial.
12. type of partial hcy screen - enter the type of partial hcy screen that was performed. (e.g., vision, hearing, etc.)
13. screening provider name - enter the provider’s name who performed the screening.
14. provider identifier - enter the provider’s npi number who performed the screening.
15. telephone number - enter the screening provider’s telephone number including the area code.
III. SERVICE INFORMATION
16. ref. no. - (reference number) a unique designator
17. procedure code - enter the procedure code(s) for the services being requested.
18. modifier - enter the appropriate modifier(s) for the services being requested.
19. from - enter the from date that services will begin if authorization is approved (mm/dd/yy format).
20. through - enter the through date the services will terminate if authorization is approved (mm/dd/yy format).
21. description of service/item - enter a specific description of the service/item being requested.
22. quantity or units - enter the quantity or units of service/item being requested.
23. amount to be charged - enter the amount to be charged for the service.
24. detailed explanation of medical necessity of the service, equipment/procedure/prosthesis, etc. attach additional page(s) as necessary.
Do not use another Prior Authorization Form.
IV. PROVIDER REQUESTING PRIOR AUTHORIzATION
25. provider name - enter the requested provider’s information. if a clinic or group practice, also complete section v.
26. address - enter the complete mailing address in this field.
27. npi - enter the provider’s npi and taxonomy code (if applicable).
28. signature/date - the provider of services should sign the request and indicate the date the form was completed. (check your provider manual to determine if this field is required.)
V. PRESCRIBING/PERFORMING PRACTITIONER
this section must be completed for services which require a prescription such as durable medical equipment, physical therapy, or for services which will be prescribed by a physician/practitioner that require prior authorization, or when the provider in section iv is a clinic or group practice. check your provider manual for additional instructions.
29. name - enter the name of the prescribing/performing practitioner.
30. telephone number - enter the prescribing/performing practitioner telephone number including area code.
31. address - enter the address, city, state, and zip code.
32. date disability began - enter the date the disability began. for example, if a disability originated at birth, enter date of birth.
33. period of medical need in months - enter the estimated number of months the participant will need the equipment/services.
34. npi - enter the provider’s npi and taxonomy code (if applicable).
35. signature of prescribing/performing practitioner - the prescribing physician/practitioner must sign and indicate the date signed in mm/dd/yy format. (Signature stamps are not acceptable)
VI. FOR STATE OFFICE USE ONLY
approval or denial for each line will be indicated in the box to the right of section iii. also in this box the consultant will indicate allowed amount if procedure requires manual pricing.
at the bottom, the consultant may explain denials or make notations referencing the specific procedure code and description by number (1 thru 12). the consultant will sign or initial the form.
mo |
mo 8809 |
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The Mo 886 0858 form is primarily used to request prior authorization for medical services or equipment through Missouri's MO HealthNet program. |
| Eligibility Requirement | Participants must be eligible for MO HealthNet on the date of service or when the equipment is received to successfully obtain authorization. |
| Authorization Clarification | Obtaining authorization through this form signifies approval of medical necessity but does not ensure payment or guarantee the reimbursement amount. |
| Data Submission | Providers must fill in specific participant and service information including name, address, diagnosis, and prognosis among others. |
| HCY Screening Details | The form includes a section for the Health Check (HCY) screening, which may require an accompanying plan of care from the provider. |
| Provider Information | Providers are required to enter their National Provider Identifier (NPI) and taxonomy code, along with contact information to ensure proper processing. |
| Governing Law | This form is governed by Missouri state law, specifically under the MO HealthNet regulations and guidelines related to medical service authorizations. |
Guidelines on Utilizing Mo 886 0858
After completing the Mo 886 0858 form, you will submit it to the Missouri Department of Social Services, specifically to the HealthNet division, for prior authorization of the requested medical services or equipment. It is essential that all sections are thoroughly filled out to avoid delays in processing. Be ready to provide additional documentation if needed to support your request.
- Leave the first field blank.
- In the second field, enter the participant's name exactly as it appears on their Mo HealthNet ID card.
- Provide the participant’s date of birth in the third field.
- Fill in the participant's complete address, including street, city, state, and zip code in the fourth field.
- Enter the participant’s 8-digit Mo HealthNet identification number in the fifth field.
- In the sixth field, provide the participant's prognosis.
- For the seventh field, enter the appropriate diagnosis code(s).
- In the eighth field, describe the diagnosis in detail; include all relevant descriptions for services being requested.
- If the service will be rendered somewhere other than home or office, specify the name and address of that facility in the ninth field.
- Complete the tenth field with the date the HCY screen was performed.
- In the eleventh field, select whether the screening was full, interperiodic, or partial.
- For the twelfth field, indicate the type of partial HCY screen that was carried out.
- Enter the name of the provider who conducted the screening in the thirteenth field.
- Input the provider’s unique identifier, the NPI number, in the fourteenth field.
- In the fifteenth field, provide the screening provider’s telephone number, including area code.
- In the sixteenth field, assign a unique reference number for the request.
- For the seventeenth field, input the procedure code(s) corresponding to the services being requested.
- In the eighteenth field, enter any applicable modifiers for the requested services.
- For the nineteenth field, fill in the starting date for the services to commence if authorized.
- In the twentieth field, indicate the termination date for the services, if authorized.
- Provide a detailed description of the requested service/item in the twenty-first field.
- In the twenty-second field, note the quantity or units of the service/item being requested.
- Enter the amount to be charged for the service in the twenty-third field.
- In the twenty-fourth field, give a detailed explanation of the medical necessity for the requested service/equipment, and attach additional pages as necessary.
- In the twenty-fifth field, enter the name of the provider requesting prior authorization.
- Fill in the complete mailing address of the provider in the twenty-sixth field.
- Provide the provider’s NPI and taxonomy (if applicable) in the twenty-seventh field.
- Have the provider of services sign and date the request in the twenty-eighth field.
- In the twenty-ninth field, enter the name of the prescribing or performing practitioner.
- Provide the practitioner’s telephone number in the thirtieth field.
- In the thirty-first field, note the provider's address, including city, state, and zip code.
- Fill in the date the participant's disability began in the thirty-second field.
- In the thirty-third field, indicate the estimated period of medical need in months.
- Provide the prescribing practitioner’s NPI and taxonomy (if applicable) in the thirty-fourth field.
- Finally, obtain the signature of the prescribing physician/practitioner and the date signed in the thirty-fifth field.
What You Should Know About This Form
What is the purpose of the Mo 886 0858 form?
The Mo 886 0858 form is designed for submitting prior authorization requests for medical services, equipment, or procedures under the Missouri health care program known as Mo HealthNet. This form is essential for healthcare providers to demonstrate the medical necessity of the requested services. However, it’s important to note that obtaining authorization does not guarantee payment or the amount to be reimbursed. Eligibility for Mo HealthNet must exist on the date of service or when the equipment is received.
What information do I need to provide when completing the form?
To properly complete the Mo 886 0858 form, you must provide comprehensive details about the participant. Key information includes the participant’s name, date of birth, and current address. You will also need to include their Mo HealthNet number, prognosis, diagnosis codes, and a detailed explanation of the medical necessity for the requested service. Additionally, you should indicate the provider's name, contact details, and any relevant screening information associated with the service.
How does the review process for the authorization request work?
Once the request is submitted using the Mo 886 0858 form, it enters the review process managed by Missouri's state office. A designated consultant evaluates the request based on the information provided. They will either approve or deny the authorization request. If denied, the form will indicate the reasons for the decision, referencing specific procedure codes. If approved, the authorization will specify the services that have been authorized to begin.
Are there specific qualifications for services requiring the form?
Yes, the Mo 886 0858 form is often required for services that necessitate a prescription, such as durable medical equipment and physical therapy. Understanding the specific qualifications for each service is crucial, as certain services might also require a plan of care. Providers should consult the Mo HealthNet provider manual for guidance on what qualifies as a service requiring prior authorization and any additional documentation that may be necessary.
What happens if the request is denied?
If a prior authorization request using the Mo 886 0858 form is denied, the provider will receive a detailed explanation of the denial reasons, referenced by specific codes. Understanding these reasons is key for providers looking to address any issues or make necessary adjustments to future requests. It may be beneficial for providers to re-evaluate the information provided in the form and ensure that all necessary documentation supporting medical necessity is complete and accurate for subsequent attempts.
Common mistakes
Filling out the Mo 886 0858 form correctly is vital for ensuring that medical services are authorized and covered. Many people make mistakes during this process, which can delay or derail needed care. Focus on the details—every section counts.
One common error is related to providing the participant's name. It may seem straightforward, but if the name listed does not match exactly with the name on the Mo HealthNet ID card, it can lead to immediate denials. Always double-check the spelling and arrangement of the name. The form must reflect the official documentation to avoid unnecessary complications.
Another mistake often encountered occurs in the diagnosis section. Individuals frequently miscode the illness or fail to provide a complete description. It is essential to ensure that both the diagnosis code and the diagnosis description are accurate and detailed. A vague or incorrect entry can halt the authorization process. Don’t leave any ambiguity; specificity is crucial.
In the service information section, people often overlook the amount to be charged. This section must be completed accurately, as any discrepancies can lead to denials. It’s important to be realistic about the costs associated with the service or item requested. Overestimating or underestimating can both create hurdles. Ensure that the amounts you provide align with what is reasonable and expected.
Lastly, many individuals forget to include the provider's signature and the date of completion. This oversight is more common than it should be and can lead to rejections. Every signature serves as confirmation of the information provided. Make sure that the person completing the form signs and dates it to validate the request. Attention to these details could make the difference between a swift approval and a frustrating delay.
Documents used along the form
The Missouri Department of Social Services provides various documents that are often used alongside the Mo 886 0858 form. Understanding these forms can help in efficiently navigating the prior authorization process for medical services. Below is a list of commonly associated documents, along with brief descriptions of each.
- Mo 8809 - Prior Authorization Quick Reference: This form serves as a quick guide for providers on the requirements and process for submitting prior authorization requests, detailing necessary documentation and procedures.
- Mo 886-0859 - Provider Enrollment Form: Providers must complete this form when seeking enrollment in the Missouri Medicaid system, enabling them to bill for services rendered to Medicaid participants.
- Mo 581-1133 - Health Insurance Portability and Accountability Act (HIPAA) Form: This form ensures compliance with HIPAA regulations, safeguarding patient privacy while allowing necessary information sharing between providers and insurers.
- Mo 886-0856 - Medical Necessity Documentation: This document is filed to explain the medical necessity of services requested and to justify the need for specific treatments or equipment being sought.
- Mo 630-1030 - EPSDT Referral Form: Used to refer children for special services under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, ensuring comprehensive care for eligible individuals.
- Mo 2300 - Request for Information: This is a standard request form that providers use to obtain necessary information from the Missouri Medicaid program regarding a participant’s eligibility and coverage details.
- Mo 885-0857 - Authorization Renewal Form: Providers use this form to request a renewal of previously approved services, documenting ongoing medical necessity and updates in patient information.
- Mo 969 - Chart Audit Request Form: This form is needed for providers to request an audit of medical records, ensuring compliance with regulatory standards and best practices within the Medicaid program.
- Mo 286 - Encounter Report Form: This report records the details of the patient encounter, documenting services delivered and providing data that supports claims for reimbursement.
- Mo 340 - Participant Authorization Form: This form is utilized by participants to authorize the release of their medical information to specific providers or organizations, facilitating communication and services.
Utilizing these forms alongside the Mo 886 0858 can streamline the process of seeking authorization for medical services. It's important to ensure that all required documentation is completed accurately to facilitate timely processing of requests and to maintain compliance with state regulations.
Similar forms
- Prior Authorization Form (PAF) - Similar to the Mo 886 0858 form, the Prior Authorization Form is used to obtain approval from insurance providers for certain medical services before they are rendered. Both require detailed patient information and a description of the services needed, emphasizing medical necessity.
- Request for Coverage (RFC) - The Request for Coverage documents are comparable in that they also seek pre-approval for specific healthcare services or devices. Like the Mo 886 0858, they often require diagnosis codes and provider information to substantiate the request.
- Diagnostic Evaluation Form - This type of form focuses on collecting necessary diagnostic information for patients, much like the Mo 886 0858. Both documents require details about the patient's condition, including prognosis and diagnosis description.
- Medical Necessity Attestation - Much like the Mo 886 0858, this document serves to confirm that the services requested are essential for the patient’s health. Both emphasize the importance of explaining why the requested service is required.
- Durable Medical Equipment (DME) Request Form - This form is specific for requesting medical equipment. Similar to the Mo 886 0858, it requires specifics about the equipment needed and the patient’s information, ensuring proper justification for the request.
- EHR Patient Information Registration - While broader in scope, this form collects essential data on a patient’s medical history and treatment needs. Like the Mo 886 0858, all necessary patient demographics and medical details contribute to ongoing care management.
- Behavioral Health Authorization Request - This document shares a purpose with the Mo 886 0858 by requiring healthcare providers to seek approval before commencing treatment. Both emphasize the necessity of thorough documentation regarding the patient’s mental health status.
- Home Health Services Request - This request form shares similarities with the Mo 886 0858 in that it aims to gain prior authorization for services to be provided in-home. Documentation of the patient’s needs and medical justification are crucial in both instances.
- Medication Prior Authorization Form - This is akin to the Mo 886 0858 since it seeks approval for specific medications before they can be filled. Both require detailed information on the patient's diagnosis and the medical justification for prescribed therapies.
Dos and Don'ts
Things to Do:
- Fill in the participant's name exactly as it appears on their MO HealthNet ID card.
- Provide a detailed explanation of medical necessity for the requested service.
- Enter accurate contact information for both the service provider and the prescribing practitioner.
- Sign the form and date it before submission to ensure its validity.
Things Not to Do:
- Do not leave any required fields blank; this may result in delays or denials.
- Avoid using signature stamps as they are not acceptable.
- Do not submit another Prior Authorization Form for the same request.
- Do not forget to specify the dates for the service period; incorrect dates can lead to approval issues.
Misconceptions
- Myth 1: Completing the Mo 886 0858 form guarantees service approval.
- Myth 2: The form can be filled out at any level of detail.
- Myth 3: It does not matter when the participant was eligible for Mo HealthNet.
- Myth 4: The form is only for medical services.
- Myth 5: Signature stamps are acceptable.
- Myth 6: All required fields must be filled out by the same person.
- Myth 7: Denial reasons are always provided clearly.
Many believe that submitting this form ensures approval for the requested services. In reality, the authorization only confirms medical necessity, not payment or reimbursement.
Some assume that any level of detail is acceptable. However, detailed explanations of medical necessity are crucial for the request to be considered properly.
Some people think the eligibility date is irrelevant. In fact, the participant must be eligible on the date of service or when the equipment is received for the request to be valid.
While many use this form for medical services, it also applies to medical equipment and prosthetics, which often require prior authorization.
A common misconception is that signature stamps can be used when signing the form. This is incorrect; the prescribing physician must provide a handwritten signature.
People often think that the same individual must complete all sections. However, the form can be completed by different parties—the provider and the practitioner can fill out their respective sections.
It is assumed that the denial reasons will be clearly communicated. In some cases, the reasons may not be explicitly listed, but they can be found by referencing specific procedure codes.
Key takeaways
Filling out the Mo 886 0858 form correctly is crucial for obtaining the necessary prior authorization for medical services. Here are some key takeaways to keep in mind:
- Eligibility Check: Ensure the participant is eligible for Mo HealthNet on the date of service or at the time the equipment or prosthesis is received.
- Detailed Information: Complete all relevant fields thoroughly, including the participant’s name, date of birth, and address as they appear on official documents.
- Medical Necessity: Provide a comprehensive explanation of the medical necessity for the requested services or equipment. Attach additional pages if needed.
- Screening Details: If applicable, include details about the HealthCheck (HCY) screening, such as the date and type of screening performed.
- Supported Documentation: Gather and attach any required supporting documents, like a plan of care, especially for requests involving durable medical equipment.
- Provider and Practitioner Information: Include accurate information for both the requesting provider and the prescribing or performing practitioner, including their contact details.
- Signature Requirement: The form must be signed by the prescribing physician or practitioner to validate the request, as signature stamps are not acceptable.
By following these guidelines, one can enhance the chances of getting the necessary authorization for medical services or equipment in a timely manner.
Browse Other Templates
Nis Forms - The address of the certifier should also be included on the form.
Eagle Project Requirements - An applicant may earn multiple palms throughout their scouting journey.