Fill Out Your Nursing Notes Form
When it comes to documenting patient care, the Nursing Notes form is an essential tool for healthcare professionals. This straightforward document captures important information related to medical treatments, medication administration, and patient observations. It assists nurses in maintaining a clear and organized record for each patient, ensuring continuity of care and communication among the medical team. Sections for patient identification, including name and medical facility, set the stage for accurate documentation. Furthermore, it incorporates fields for vital signs, medications administered, and even notes on patient reactions or conditions over time. This level of detail guarantees that all critical information is accessible, allowing nurses to make informed decisions about patient care. Importantly, the form is designed for ongoing use, meaning that updates and changes can be consistently recorded, reflecting the patient’s evolving health status. By understanding the structure and purpose of the Nursing Notes form, healthcare professionals can enhance their documentation practices, ultimately benefiting patient outcomes.
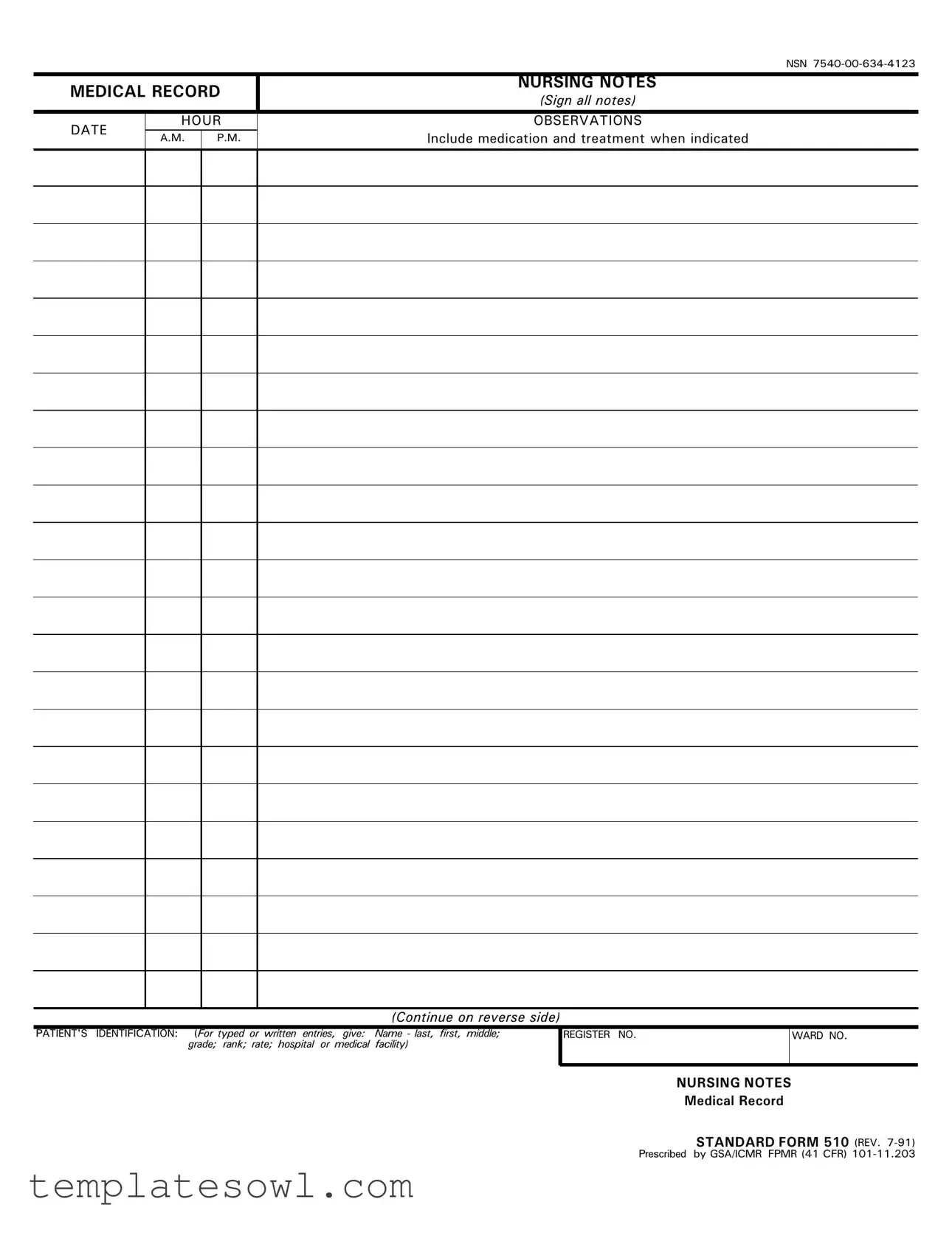
Nursing Notes Example

161
0(',&$/5(&25' |
1856,1*127(6 |
|||
6LJQDOOQRWHV |
||||
|
|
|
||
|
|
|
|
|
'$7( |
+285 |
2%6(59$7,216 |
||
|
|
,QFOXGHPHGLFDWLRQDQGWUHDWPHQWZKHQLQGLFDWHG |
||
$0 |
30 |
|||
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
&RQWLQXHRQUHYHUVHVLGH
3$7,(176 ,'(17,),&$7,21 )RU W\SHG RU ZULWWHQ HQWULHV JLYH 1DPH ODVW ILUVW PLGGOH JUDGH UDQN UDWH KRVSLWDO RU PHGLFDO IDFLOLW\
5(*,67(5 12 |
:$5' 12 |
|
|
1856,1*127(6
0HGLFDO5HFRUG
67$1'$5')2505(9
3UHVFULEHG E\*6$,&05 )305&)5
1856,1*127(6
6LJQDOOQRWHV
'$7(
+285
$0 |
30 |
|
|
2%6(59$7,216
,QFOXGHPHGLFDWLRQDQGWUHDWPHQWZKHQLQGLFDWHG
&RQWLQXHRQUHYHUVHVLGH
67$1'$5')2505(9 %$&.
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | The Nursing Notes form is used to document patient care, including medications and treatments administered during a patient's stay in a healthcare facility. |
| Components | This form includes sections for patient identification, medical record number, and various entries regarding patient care, such as medications and treatments. |
| Signature Requirement | A healthcare professional's signature is required to validate the report, ensuring accountability in patient care documentation. |
| Regulation | In many states, Nursing Notes must conform to the standards set by the Nurse Practice Act, which governs nursing practice and documentation. |
| Frequency of Use | This form is typically used regularly throughout a patient's hospitalization, with entries made at each shift or as care is provided. |
| Importance of Accuracy | Accurate and detailed notes are essential for continuity of care and can be crucial in legal situations regarding patient treatment. |
Guidelines on Utilizing Nursing Notes
Filling out the Nursing Notes form is an important task that helps ensure accurate medical records. This process is straightforward and can help improve the quality of care for patients. Below are the steps to guide you through completing the form effectively.
- Begin by gathering all necessary information including the patient's details and the date of the notes.
- In the first section, input the patient's name, last name, first name, middle initial, age, and grade level. Make sure this information is correct.
- Next, indicate the hospital or medical facility where the care is being provided.
- Proceed to fill in the relevant date and time when the notes are being recorded.
- In the section for medication and treatment, accurately document any medications administered and treatments provided, ensuring you include specific dosages and times.
- Next, describe the patient's condition and response to treatments. Use clear and concise language to provide an accurate overview.
- In the designated area for additional notes, include any observations or relevant information that could assist other healthcare providers in understanding the patient's care.
- Finally, review the entire form for accuracy and completeness before signing and dating the document at the bottom.
Once the form is filled out, it's important to file it properly and ensure the information is accessible to relevant healthcare professionals. This helps maintain continuity of care and supports effective communication. Be mindful of confidentiality as you proceed with handling the completed form.
What You Should Know About This Form
What is the purpose of the Nursing Notes form?
The Nursing Notes form serves as a vital tool for healthcare professionals to document patient care, treatments, and any significant observations. This documentation aids in creating a comprehensive medical record that can be referenced by other healthcare providers. Accurate notes ensure continuity in care, facilitate communication among medical staff, and provide legal protection by offering a clear account of the patient's treatment journey.
What information is typically included in the Nursing Notes?
The Nursing Notes usually include patient demographics, such as name, age, and medical record number, alongside detailed records of medications administered, treatment interventions provided, and the patient’s response to these actions. Additionally, any changes in the patient’s condition—be it physical, emotional, or cognitive—are documented. This comprehensive approach ensures that all relevant information is captured for quality care and safety.
How often should the Nursing Notes be updated?
Nursing Notes should be updated regularly, ideally after each patient interaction. This could be after a procedure, medication administration, or any notable change in the patient's condition. Continuous documentation allows for real-time updates that are crucial in providing immediate care and enables healthcare professionals to track the patient's progress accurately.
Who is authorized to fill out the Nursing Notes?
Authorized personnel typically include registered nurses, licensed practical nurses, and nurse practitioners. These individuals are trained to observe patient behaviors, assess conditions, and implement care plans. However, in some facilities, specific procedures may allow for trained support staff to contribute to the documentation under supervision, depending on the established protocols.
Can Nursing Notes be shared with other healthcare providers?
Yes, Nursing Notes can be shared with other healthcare providers involved in the patient’s care. However, sharing must comply with privacy laws, such as HIPAA, which protects patient information. When sharing, it is crucial to ensure that only relevant details are disclosed and that all parties understand and adhere to confidentiality requirements.
What are the consequences of not accurately using the Nursing Notes form?
Failing to accurately use the Nursing Notes form can lead to numerous issues. Poor documentation may result in inadequate patient care, miscommunication among healthcare providers, and increase the risk of legal liability. Inaccurate record-keeping can also contribute to potential safety hazards for patients and may impact treatment outcomes significantly, underscoring the importance of diligent and precise documentation.
Common mistakes
Filling out the Nursing Notes form accurately is crucial for patient care. However, many common mistakes can lead to important information being overlooked. Let’s discuss five of these mistakes in detail.
One significant error is incomplete information. Nurses often skip sections of the form due to time pressures or oversight. Leaving out crucial details, such as patient allergies or medications, can have serious repercussions on a patient’s treatment. It is vital to ensure that every section is filled out completely and accurately.
Another common mistake is the use of inconsistent terminology. Terminology in medical notes must be clear and standardized. Using vague or unconventional terms can lead to confusion among healthcare providers. Consistency in language is fundamental for effective communication within the healthcare team.
In addition, some individuals fail to document changes in patient status promptly and thoroughly. When a patient’s condition changes, timely updates are essential. Delayed or missing notes can hinder appropriate medical responses and affect patient outcomes dramatically.
Additionally, mistakes in timing can occur. Some nurses submit notes too late, while others may forget to log notes altogether. Timely documentation ensures accurate records that reflect real-time patient care. Neglecting this can result in gaps that may compromise treatment plans.
Lastly, many overlook the importance of reviewing notes before submission. Failing to proofread can lead to typographical errors that alter the meaning of documented information. Taking a moment to review notes can prevent misunderstandings and enhance the clarity of patient records.
Recognizing these mistakes and taking proactive steps to avoid them can greatly improve patient care and ensure that healthcare providers have the most accurate information available.
Documents used along the form
In the nursing practice, documentation is essential for effective patient care and communication among healthcare providers. Various forms and documents accompany nursing notes, contributing to a comprehensive understanding of a patient's condition and treatment plan. Below is a list of common forms and documents that are frequently used alongside the Nursing Notes form.
- Patient Assessment Form: This document captures initial evaluations made by nurses, outlining a patient's medical history, vital signs, and any immediate health concerns. It provides a baseline for future assessments and interventions.
- Medication Administration Record (MAR): The MAR tracks all medications given to a patient, including dosages and administration times. It is crucial for ensuring that medications are given accurately and for monitoring potential interactions.
- Care Plan: A care plan outlines the specific goals and interventions tailored to each patient’s needs. It serves as a guide for the nursing staff, ensuring that everyone is aware of the patient's treatment objectives and strategies.
- Incident Report: This document is used to describe any unusual or unexpected event occurring during patient care, such as falls or medication errors. Incident reports are critical for improving safety standards and understanding risks in clinical settings.
- Progress Notes: Progress notes are periodically updated by nursing staff to record changes in a patient's condition, responses to treatment, and any new assessments. This documentation helps maintain continuity of care among healthcare professionals.
- Discharge Summary: Upon a patient’s release from healthcare services, the discharge summary provides a concise record of the patient’s treatment during their stay, follow-up instructions, and recommendations for ongoing care.
- Consent Forms: These forms document that a patient has given their informed consent for treatments or procedures. They emphasize the importance of communication between the patient and the healthcare provider regarding risks and benefits.
These documents work in tandem with nursing notes to ensure that patient care is thorough, coordinated, and compliant with healthcare standards. Effective documentation not only enhances patient safety but also supports accountability and professionalism within the nursing profession.
Similar forms
Patient Assessment Form: This document includes detailed evaluations of a patient's health, similar to the Nursing Notes form. Both documents track observations and condition changes over time.
Medication Administration Record (MAR): The MAR lists all medications given to a patient. Like the Nursing Notes, it requires documentation of treatments and responses to medications.
Care Plan Documentation: This outlines the specific care a patient will receive. Both it and the Nursing Notes form involve a plan and its execution to meet the patient’s needs.
Vital Signs Chart: This chart records a patient's vital signs over time. Similar to Nursing Notes, both track important health indicators and changes.
Interdisciplinary Progress Notes: These notes are written by multiple healthcare team members. They share a common goal with Nursing Notes: to provide a comprehensive view of patient progress.
Discharge Summary: This document summarises a patient's stay and outlines aftercare. It shares the narrative style of the Nursing Notes, detailing the patient's journey.
Incident Report: This document records any unusual events affecting patient care. Like the Nursing Notes, it emphasizes communication about significant occurrences in patient management.
Referral Letter: A referral document introduces a patient to another healthcare provider. Both documents contain essential patient information and treatment history to ensure continuity of care.
Dos and Don'ts
Things You Should Do:
- Clearly document every relevant detail about the patient’s condition.
- Use professional language and avoid slang or informal terminology.
- Be timely in your entries; make sure to write notes as soon as possible after providing care.
- Ensure that all entries are signed and dated to maintain accountability and traceability.
Things You Shouldn't Do:
- Do not omit important information that could affect patient care.
- Avoid using vague terms; specific descriptions help convey accurate information.
- Never alter previous entries; make new notes if corrections are necessary.
- Do not share patient notes or sensitive information with unauthorized individuals.
Misconceptions
Here are 9 common misconceptions about the Nursing Notes form, along with explanations for each one:
- Nursing Notes are Optional. Many believe that completing Nursing Notes is not mandatory. In reality, these notes are crucial for ensuring patient care continuity and legal documentation.
- Only Nurses Can Fill Out Nursing Notes. While nurses primarily complete these notes, other healthcare team members can contribute information as necessary.
- Nursing Notes Do Not Need to Be Detailed. Some think brief notes are sufficient. However, detailed notes provide better context for patient care and can help avoid misunderstandings.
- Errors in Nursing Notes Can Be Ignored. It's a misconception that mistakes in the notes can simply be overlooked. Any errors must be corrected appropriately, as they can have serious implications for patient care and legal responsibility.
- Nursing Notes Are Only for Medical Professionals. Many believe that only medical staff should access these notes. However, they are essential for anyone involved in the patient's care to ensure comprehensive treatment.
- The Format of Nursing Notes Is Inflexible. Some think there is only one way to write Nursing Notes. In truth, while there may be guidelines, flexibility exists in documenting as long as the critical information is included.
- Nursing Notes Are Submitted After Discharge Only. A common belief is that these notes are only necessary at discharge. Regular completion throughout a patient’s stay is vital for ongoing care and assessment.
- You Can Use Abbreviations Freely. While abbreviations can save time, overusing them can lead to confusion. Clarity in communication is always the priority.
- Once Submitted, Nursing Notes Cannot Be Changed. There is a misconception that Nursing Notes are final once submitted. However, amendments can and should be made when necessary, with appropriate documentation of changes.
Key takeaways
When using the Nursing Notes form, it is essential to follow certain guidelines to ensure accuracy and compliance. Here are eight key takeaways:
- Always enter information in a clear and concise manner to prevent misunderstandings.
- The form requires both a signature and date; ensure these are completed for accountability.
- Include all relevant medications and treatments as indicated in the instructions.
- Use the designated sections for each type of entry, such as medical history and treatment responses.
- Maintain confidentiality by securing the form when not in use; patient information is sensitive.
- Regularly review the completed Nursing Notes to ensure compliance with facility policies.
- Seek clarification on any parts of the form that are unclear; accuracy is crucial for patient care.
- Keep a record of all submitted forms for your own reference and to track patient progress over time.
Browse Other Templates
Va Form 28-1900 - The involvement of authorized officials helps streamline the application process and enhances its efficiency.
Trupanion Claim Form Canada - Ensure all invoices include treatment descriptions and charge amounts.