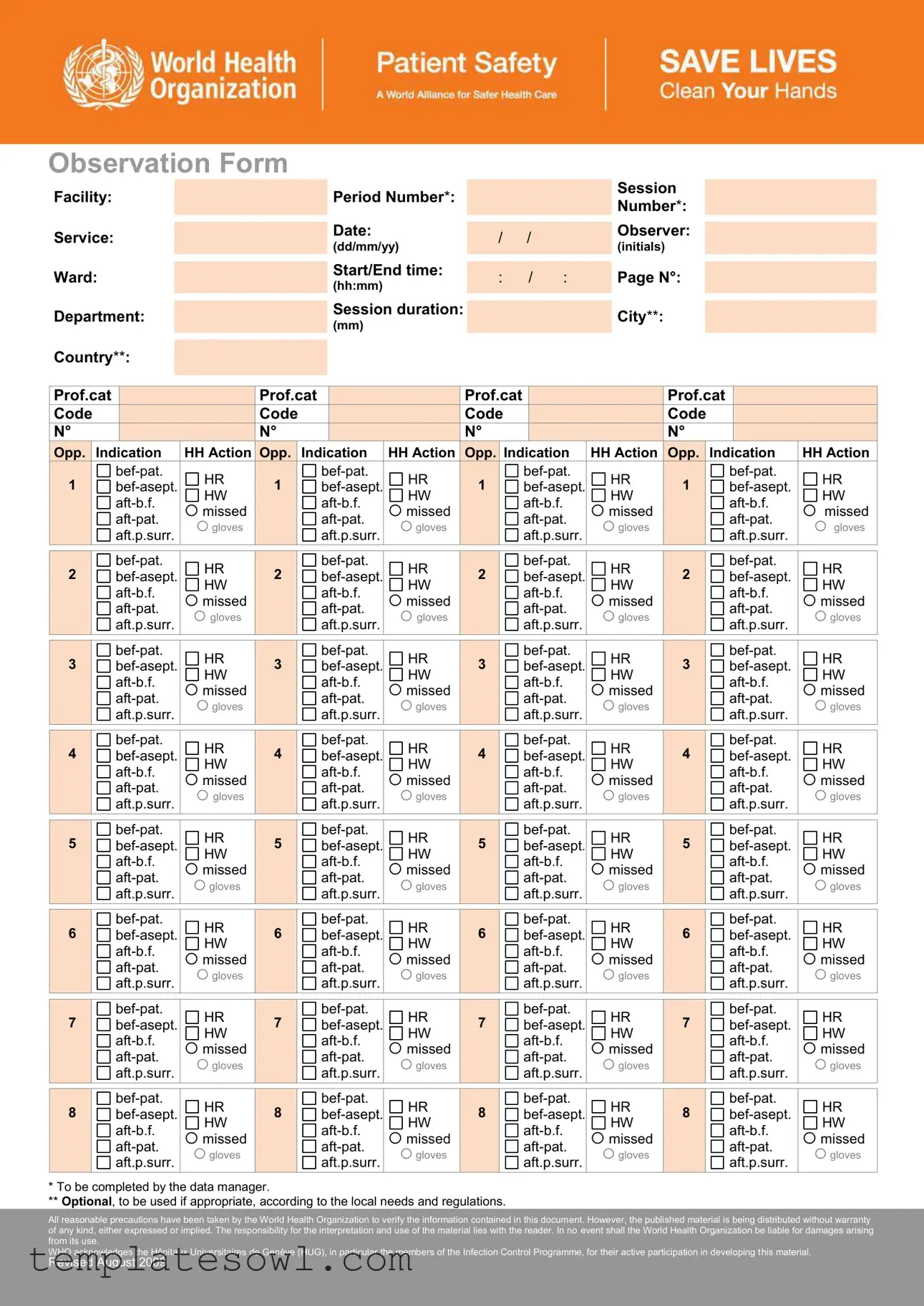
Fill Out Your Hand Hygiene Observation Form
The Hand Hygiene Observation Form is a vital tool in any health care setting, ensuring that proper hand hygiene protocols are observed. This form captures essential details about the observation process, including the facility, service, ward, department, and the date of observation. Key sections include the identification of the observer and the specifics of the observed health-care activity, such as the start and end times along with session duration. Each observation session is structured to last up to 30 minutes, focusing on how health-care workers perform hand hygiene at critical moments. The form details various opportunities for hand hygiene, categorized by indications like before patient contact or after exposure to bodily fluids. It also tracks the observed actions—whether handwashing or handrubbing was performed or missed. Potential errors and the context of glove use are noted, emphasizing the importance of accurate data collection. The results compiled in the form can contribute to an overall compliance calculation, reflecting the effectiveness of hand hygiene practices within the facility. This documentation is crucial for improving infection control measures and protecting patient safety.
Hand Hygiene Observation Example
Observation Form
Facility:
Service:
Ward:
Department:
Country**:
Period Number*: |
|
|
|
|
Session |
|
|
|
|
||
|
|
|
|
Number*: |
|
|
|
|
|
|
|
Date: |
|
|
|
|
Observer: |
|
|
|
|
||
|
/ |
/ |
|
||
(dd/mm/yy) |
|
|
(initials) |
||
|
|
|
|
||
Start/End time: |
|
|
|
|
Page N°: |
|
: |
/ |
: |
||
|
|||||
(hh:mm) |
|
||||
|
|
|
|
|
Session duration: |
|
City**: |
|
||
(mm) |
|
|
|
|
Prof.cat |
|
|
|
Prof.cat |
|
|
|
Prof.cat |
|
|
|
Prof.cat |
|
|
|
|||||
Code |
|
|
|
Code |
|
|
|
Code |
|
|
|
Code |
|
|
|
|||||
N° |
|
|
|
N° |
|
|
|
N° |
|
|
|
N° |
|
|
|
|||||
|
Opp. |
Indication |
HH Action |
Opp. |
Indication |
HH Action |
Opp. |
Indication |
HH Action |
Opp. |
Indication |
HH Action |
||||||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
1 |
|
1 |
|
1 |
|
1 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
2 |
|
2 |
|
2 |
|
2 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
3 |
|
3 |
|
3 |
|
3 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
4 |
|
4 |
|
4 |
|
4 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
5 |
|
5 |
|
5 |
|
5 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
6 |
|
6 |
|
6 |
|
6 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
7 |
|
7 |
|
7 |
|
7 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HR |
|
|
HR |
|
|
HR |
|
|
HR |
||||||||
|
8 |
|
8 |
|
8 |
|
8 |
|
||||||||||||
|
|
HW |
|
HW |
|
HW |
|
HW |
||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
missed |
|
|
missed |
|
|
missed |
|
|
missed |
||||||||
|
|
|
gloves |
|
|
gloves |
|
|
gloves |
|
|
gloves |
||||||||
|
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
|
|
aft.p.surr. |
||||||||
* To be completed by the data manager.
** Optional, to be used if appropriate, according to the local needs and regulations.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
Revised August 2009

General Recommendations
(refer to the Hand Hygiene Technical Reference Manual)
1.In the context of open and direct observations, the observer introduces him/herself to the
2.The
3.Detected and observed data should be recorded with a pencil in order to be immediately corrected if needed.
4.The top of the form (header) is completed before starting data collection (excepted end time and session duration).
5.The session should last no more than 20 minutes (± 10 minutes according to the observed activity); the end time and the session duration are to be completed at the end of the observation session.
6.The observer may observe up to three
7.Each column of the grid to record hand hygiene practices is intended to be dedicated to a specific professional category. Therefore numerous
8.As soon as you detect an indication for hand hygiene, count an opportunity in the appropriate column and cross the square corresponding to the indication(s) you detected. Then complete all the indications that apply and the related hand hygiene actions observed or missed.
9.Each opportunity refers to one line in each column; each line is independent from one column to another.
10.Cross items in squares (several may apply for one opportunity) or circles (only a single item may apply at one moment).
11.When several indications fall in one opportunity, each one must be recorded by crossing the squares.
12.Performed or missed actions must always be registered within the context of an opportunity.
13.Glove use may be recorded only when the hand hygiene action is missed while the
Short description of items
Facility: |
to complete according to the local nomenclature |
|
|
||
Service: |
to complete according to the local nomenclature |
|
|
||
Ward: |
to complete according to the local nomenclature |
|
|
||
Department: |
to complete according to the following standardized nomenclature: |
||||
|
medical, including dermatology, neurology, |
|
surgery, including neurosurgery, urology, EENT, |
||
|
haematology, oncology, etc. |
|
ophthalmology, etc. |
||
|
mixed (medical & surgical), including gynaecology |
|
obstetrics, including related surgery |
||
|
paediatrics, including related surgery |
|
intensive care & resuscitation |
||
|
emergency unit |
|
|
|
long term care & rehabilitation |
|
ambulatory care, including related surgery |
|
other (to specify) |
||
Period N°: |
1) |
||||
Date: |
day (dd) / month (mm) / year (yy) |
|
|
||
Start/end time: |
hour (hh) / minute (mm). |
|
|
||
Session duration: |
difference between start and end time, resulting in minutes of observation. |
||||
Session N°: |
attributed at the moment of data entry for analysis. |
|
|
||
Observer: |
observer’s initials (the observer is responsible for the data collection and for checking their accuracy |
||||
|
before submitting the form for analysis. |
|
|
||
Page N°: |
to write only when more than one form is used for one session. |
||||
Prof.cat: |
according to the following classification: |
|
|
||
|
1. nurse / midwife |
|
1.1 nurse, 1.2 midwife, 1.3 student. |
||
|
2. auxiliary |
|
|
|
|
|
3. medical doctor |
|
3.1 in internal medicine, 3.2 surgeon, 3.3 anaesthetist / resuscitator / emergency |
||
|
|
|
physician, 3.4 paediatrician, 3.5 gynaecologist, 3.6 consultant, 3.7 medical student. |
||
|
4. other health- |
|
4.1 therapist (physiotherapist, occupational therapist, audiologist, speech |
||
|
care worker |
|
therapist), 4.2 technician (radiologist, cardiology technician, operating room |
||
|
|
|
technician, laboratory technician, etc), 4.3 other (dietician, dentist, social worker |
||
|
|
|
and any other |
||
Number: |
number of observed |
||||
|
they enter the field of observation and you detect opportunities. |
||||
Opp(ortunity): |
defined by one indication at least |
|
|
||
Indication: |
reason(s) that motivate(s) hand hygiene action; all indications that apply at one moment must be recorded |
||||
|
bef.pat: before touching a patient |
|
aft.b.f: after body fluid exposure risk |
||
|
bef.asept: before clean/aseptic procedure |
|
aft.pat: after touching a patient |
||
|
|
|
|
|
aft.p.surr: after touching patient surroundings |
HH action: |
response to the hand hygiene indication(s); it can be either a positive action by performing handrub or |
||||
|
handwash, or a negative action by missing handrub or handwash |
||||
|
HR: hand hygiene action by handrubbing with an |
|
Missed: no hand hygiene action performed |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
HW: hand hygiene action by handwashing with soap and |
|
|
||
|
water |
|
|
|
|
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
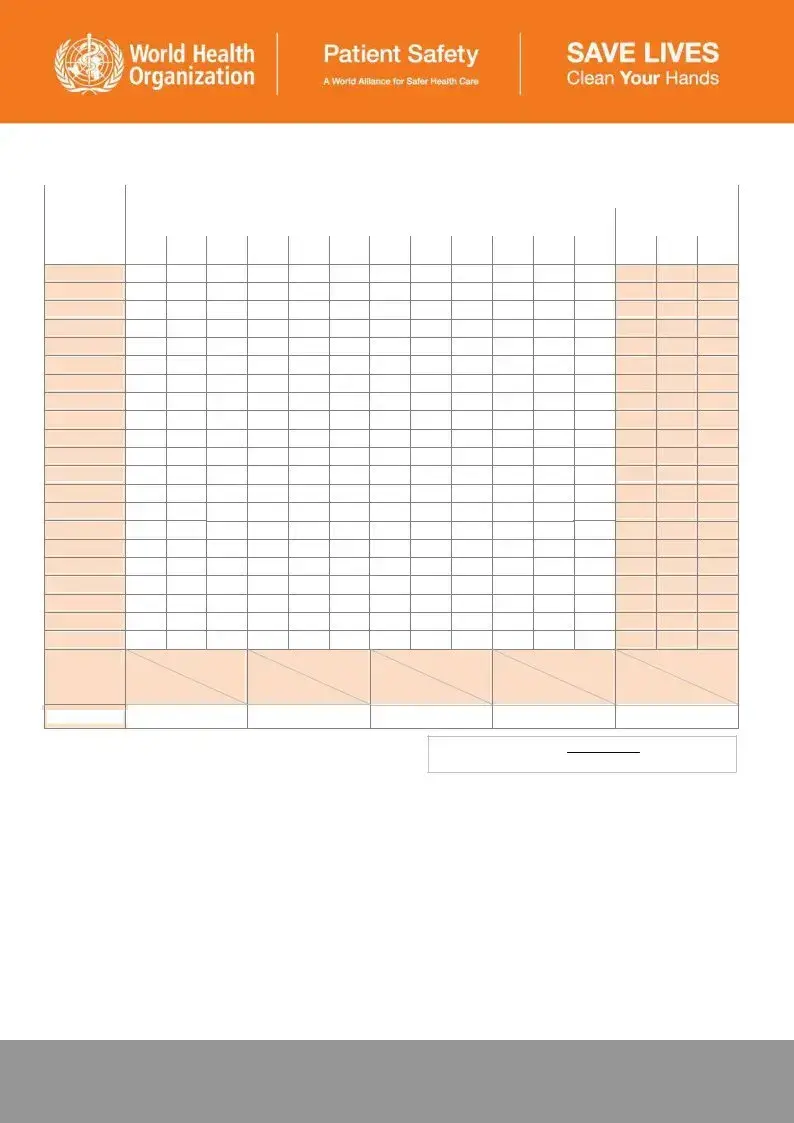
Observation Form – Basic Compliance Calculation
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Facility: |
|
|
|
|
|
Period: |
|
|
Setting: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prof.cat. |
|
|
Prof.cat. |
|
|
Prof.cat. |
|
|
Prof.cat. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total per session |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Session N° |
Opp |
HW |
HR |
Opp |
HW |
HR |
Opp |
HW |
HR |
Opp |
HW |
HR |
|
Opp |
HW |
HR |
|
|
|
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
(n) |
|
(n) |
(n) |
(n) |
1 |
|
|
|
|
|
|
2 |
|
|
|
|
|
|
3 |
|
|
|
|
|
|
4 |
|
|
|
|
|
|
5 |
|
|
|
|
|
|
6 |
|
|
|
|
|
|
7 |
|
|
|
|
|
|
8 |
|
|
|
|
|
|
9 |
|
|
|
|
|
|
10 |
|
|
|
|
|
|
11 |
|
|
|
|
|
|
12 |
|
|
|
|
|
|
13 |
|
|
|
|
|
|
14 |
|
|
|
|
|
|
15 |
|
|
|
|
|
|
16 |
|
|
|
|
|
|
17 |
|
|
|
|
|
|
18 |
|
|
|
|
|
|
19 |
|
|
|
|
|
|
20 |
|
|
|
|
|
|
Total |
|
|
|
|
|
|
Calculation |
Act (n) = |
Act (n) = |
Act (n) = |
Act (n) = |
|
Act (n) = |
|
Opp (n) = |
Opp (n) = |
Opp (n) = |
Opp (n) = |
Opp (n) = |
|
Compliance |
|
|
|
|
|
|
|
|
|
Compliance (%) = |
Actions |
x 100 |
|
|
|
|
|
Opportunities |
||
Instructions for use
1.Define the setting outlining the scope for analysis and report related data according to the chosen setting.
2.Check data in the observation form. Hand hygiene actions not related to an indication should not be taken into account and vice versa.
3.Report the session number and the related observation data in the same line. This attribution of session number validates the fact that data has been taken into count for compliance calculation.
4.Results per professional category and per session (vertical):
4.1Sum up recorded opportunities (opp) in the case report form per professional category: report the sum in the corresponding cell in the calculation form.
4.2Sum up the positive hand hygiene actions related to the total of opportunities above, making difference between handwash (HW) and handrub (HR): report the sum in the corresponding cell in the calculation form.
4.3Proceed in the same way for each session (data record form).
4.4Add up all sums per each professional category and put the calculation to calculate the compliance rate (given in percent)
5.The addition of results of each line permits to get the global compliance at the end of the last right column.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
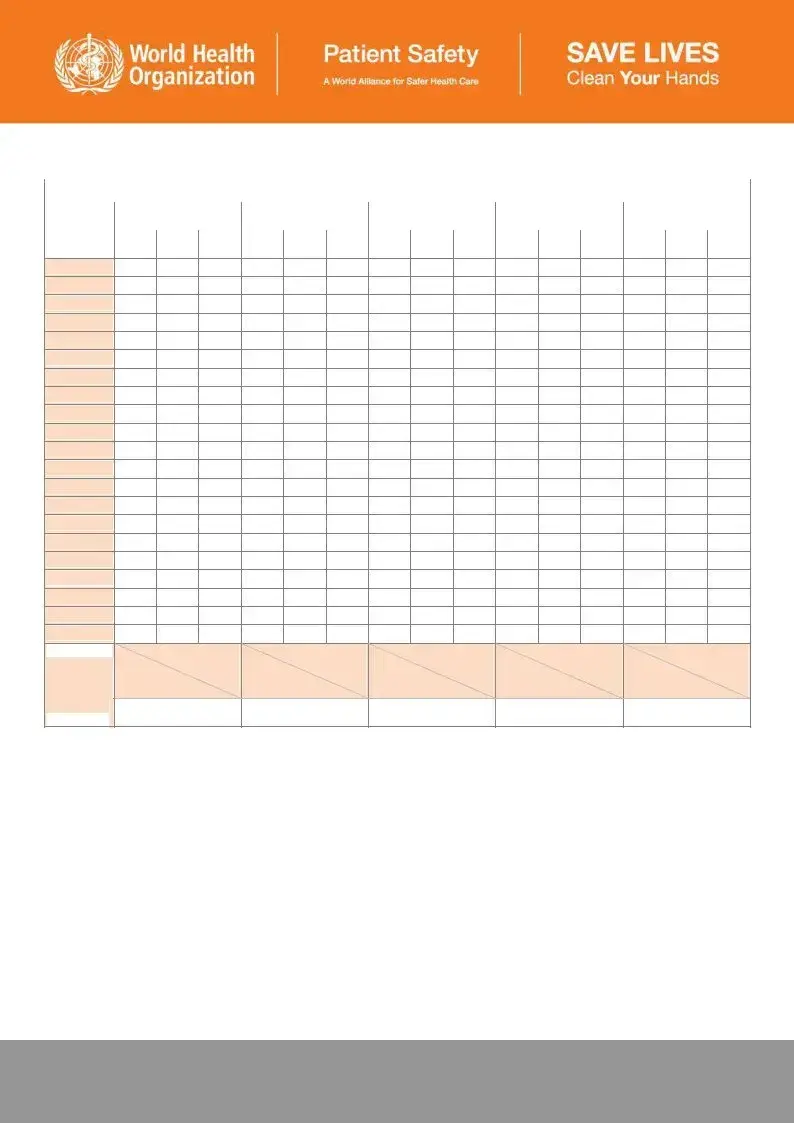
Observation Form – Optional Calculation Form
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Facility: |
|
|
|
|
|
|
|
Period: |
|
|
|
Setting: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Before touching a |
|
Before clean/ aseptic |
|
After body fluid |
|
|
After touching a |
|
|
After touching |
|
|||||||
|
|
|
|
|
|
|
|
||||||||||||
|
patient |
|
|
|
procedure |
|
|
exposure risk |
|
|
patient |
|
|
|
patient surroundings |
||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
Indic |
HW |
HR |
|
Indic |
HW |
HR |
|
Indic |
HW |
HR |
|
Indic |
HW |
HR |
|
Indic |
HW |
HR |
Session N° |
|
|
|
|
|||||||||||||||
|
(n) |
(n) |
(n) |
|
(n) |
(n) |
(n) |
|
(n) |
(n) |
(n) |
|
(n) |
(n) |
(n) |
|
(n) |
(n) |
(n) |
|
|
|
|
|
|||||||||||||||
1 |
|
|
|
|
|
2 |
|
|
|
|
|
3 |
|
|
|
|
|
4 |
|
|
|
|
|
5 |
|
|
|
|
|
6 |
|
|
|
|
|
7 |
|
|
|
|
|
8 |
|
|
|
|
|
9 |
|
|
|
|
|
10 |
|
|
|
|
|
11 |
|
|
|
|
|
12 |
|
|
|
|
|
13 |
|
|
|
|
|
14 |
|
|
|
|
|
15 |
|
|
|
|
|
16 |
|
|
|
|
|
17 |
|
|
|
|
|
18 |
|
|
|
|
|
19 |
|
|
|
|
|
20 |
|
|
|
|
|
Total |
|
|
|
|
|
Calculation |
Act (n) = |
Act (n) = |
Act (n) = |
Act (n) = |
Act (n) = |
|
Indic1 (n) = |
Indic2 (n) = |
Indic3 (n) = |
Indic4 (n) = |
Indic5 (n) = |
Ratio |
|
|
|
|
|
act / indic |
|
|
|
|
|
Instructions for use
1.Define the setting outlining the scope for analysis and report related data according to the chosen setting.
2.Check data in the observation form. Hand hygiene actions not related to an indication should not be taken into account and vice versa.
3.If several indications occur within the same opportunity, each one should be considered separately as well as the related action.
4.Report the session number and the related observation data in the same line. This attribution of session number validates the fact that data has been taken into count for compliance calculation.
5.Results per indication (indic) and per session (vertical):
4.1Sum up indications per indication in the observation form: report the sum in the corresponding cell in the calculation form.
4.2Sum up positive hand hygiene actions related to the total of indications above, making the difference between handwash (HW) and handrub (HR): report the sum in the corresponding cell in the calculation form.
4.3Proceed in the same way for each session (observation form).
4.4Add up all sums per each indication and put the calculation to calculate the ratio (given in percent)
Note: This calculation is not exactly a compliance result, as the denominator of the calculation is an indication instead of an opportunity. Action is artificially overestimated according to each indication. However, the result gives an overall idea of
of indication.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Hand Hygiene Observation form is designed to monitor hand hygiene practices among healthcare workers. |
| Data Collection | Observers collect data in real-time, noting opportunities and actions related to hand hygiene. |
| Professional Categories | The form distinguishes between different professional categories such as nurses, doctors, and technicians. |
| Documentation | Data must be recorded using a pencil to allow for immediate corrections if needed. |
| Session Duration | Each observation session should last no more than 20 minutes, plus or minus 10 minutes. |
| Indications | The form includes specific indications for when hand hygiene is required, such as before touching a patient. |
| Actions | Following an indication, the actions taken are recorded as either performed (handrub or handwash) or missed. |
| Reporting | Observations are reported according to local nomenclature and should be clear and concise. |
| Compliance Calculation | Compliance is calculated based on the ratio of actions performed to opportunities identified. |
| Legal Requirements | Use of the form may be subject to state-specific laws governing healthcare practices and infection control. |
Guidelines on Utilizing Hand Hygiene Observation
Before filling out the Hand Hygiene Observation form, ensure that you have the necessary details about the observation context at hand. Use the following steps to correctly complete each section of the form, ensuring accuracy in your observations and data entry.
- Begin by entering the Facility name according to the local nomenclature.
- Fill in the Service field similarly, following local standards.
- Provide the Ward name in accordance with local practices.
- Identify the Department by using the standardized nomenclature provided in the instructions.
- If needed, enter the Country and City. These fields are optional.
- Fill in the Period Number, selecting “pre-intervention” or “post-intervention” as appropriate.
- Record the Date using the format (dd/mm/yy).
- Input the Observer's initials to confirm accountability for the data collection.
- Document the Start time in the format (hh:mm).
- At the conclusion of the observation session, record the End time, also in the format (hh:mm).
- Calculate and enter the Session duration in minutes, based on start and end times.
- If you use more than one page, indicate the Page Number.
- In the grid, allocate appropriate spaces for professional categories observing health-care workers. Note: The indicated numbers correspond to specific roles outlined in the form.
- As you observe health-care practices, document each instance of hand hygiene opportunity. Assign it to the correct professional category column and mark the corresponding indication.
- Status of hand hygiene action (whether performed or missed) should be noted next to each indication by crossing the relevant squares.
- Use a pencil for recording to allow for immediate corrections if needed.
Following these steps will help ensure that the Hand Hygiene Observation form is filled out accurately and systematically. This will facilitate the collection of reliable data, critical for assessing hand hygiene practices in healthcare settings.
What You Should Know About This Form
What is the purpose of the Hand Hygiene Observation form?
The Hand Hygiene Observation form is designed to record and analyze the hand hygiene practices of healthcare workers. By documenting these practices, the form helps identify areas for improvement and promotes better hygiene within healthcare settings. This contributes to overall patient safety and infection control.
How is the form structured?
The form includes sections for essential information like the facility, service, department, date, and observer’s initials. It allows for tracking hand hygiene opportunities and actions taken, categorized by different professional roles. Observers note whether the hand hygiene actions were performed or missed for specific opportunities.
What are "opportunities" in the context of this form?
Opportunities refer to specific moments when hand hygiene should occur according to established guidelines. Examples include before touching a patient, before aseptic procedures, and after body fluid exposure. Each opportunity is logged to ensure comprehensive tracking of hand hygiene behavior.
How should I complete the form during observations?
As an observer, you should introduce yourself to both healthcare workers and patients. Start noting observations using a pencil for easy corrections. Tally the opportunities and corresponding actions, marking if each action was performed or missed. Each recorded action relates to a specific opportunity, and you might observe multiple healthcare workers simultaneously, depending on the conditions.
What should I do if I need to add or change information?
Changes can be made on the form while using a pencil, which makes corrections easy. Ensure you accurately reflect what was observed before submitting the data for analysis. It’s crucial to maintain precise records, as they will be vital for compliance calculations later on.
Can I observe more than one healthcare worker at a time?
Yes, you can observe up to three healthcare workers if the conditions allow. Each worker can have a dedicated column in the form. This flexibility helps ensure comprehensive data collection, but make sure that the density of hand hygiene opportunities is appropriate for multiple observations.
What happens if a healthcare worker misses a hand hygiene action while wearing gloves?
If a hand hygiene action is missed while the healthcare worker is wearing gloves, it should still be recorded. This serves to highlight the importance of hand hygiene even when gloves are used. Observations should always reflect the context of the opportunity to ensure accurate data for analysis.
What can I do with the data collected from the Hand Hygiene Observation form?
Once the observations are complete, the data can be used to calculate compliance rates and identify trends in hand hygiene practices. This information helps healthcare facilities implement strategies for improvement and ensure that hygiene standards are being met, leading to enhanced patient care and safety.
Common mistakes
When filling out the Hand Hygiene Observation form, several common mistakes can lead to inaccuracies in the data collected. One frequent error is incomplete header information. Observers often forget to provide essential details like the facility, service, or department. It's important to fill this information accurately to ensure that the data can be properly analyzed later.
Another mistake is failing to record the session duration correctly. Observers sometimes forget to calculate the difference between the start and end times, leading to gaps in the data. This oversight can affect the overall analysis of compliance rates.
Additionally, using the wrong professional category to label healthcare workers is a common error. Selecting the incorrect code for a healthcare worker can significantly misrepresent hand hygiene compliance. Each observation should align with the specific professional category to ensure that the data reflects accurate practices.
Many observers neglect to indicate missed opportunities for hand hygiene. Each time an opportunity arises, it must be documented. If missed actions are overlooked, the overall compliance rates may appear artificially high, which does not help in effective monitoring.
Crossing items incorrectly is yet another mistake. Observers might either not mark all applicable items or mistakenly mark too many choices for a single opportunity. Each observed action should align with the correct indication to maintain the integrity of the data.
Finally, another common issue is the use of pens instead of pencils. Recording observations with a permanent ink pen makes correcting mistakes difficult. Observers should use pencils so that any errors can be adjusted without leaving a trace.
Documents used along the form
In the context of maintaining effective hand hygiene practices, various forms and documents complement the Hand Hygiene Observation form. Each document serves a unique purpose, assisting healthcare facilities in tracking, analyzing, and improving hand hygiene compliance. Together, these resources provide vital data to enhance patient safety and care quality.
- Hand Hygiene Training Records: Documenting training sessions ensures that all healthcare workers understand proper hand hygiene techniques and protocols. It may include details like date, trainer, duration, and participant signatures.
- Infection Control Audits: Regular audits assess hand hygiene protocols and compliance within the facility. The findings from these audits help identify areas needing improvement and reinforce adherence to guidelines.
- Patient Satisfaction Surveys: These surveys collect feedback on patients' perceptions of care, including cleanliness and observed hand hygiene practices. Insights gained can drive changes to improve overall service quality.
- Incident Reports: Any infection-related incidents should be documented thoroughly. These reports help identify potential lapses in hand hygiene practices and allow for corrective measures to be implemented.
- Compliance Monitoring Logs: This document tracks adherence rates among healthcare workers over time. Logs may show patterns that require targeted training or reinforcement efforts.
- Action Plans for Improvement: Following assessments or observations, facilities should develop action plans outlining strategies to address non-compliance, including timelines and responsible parties.
- Hand Hygiene Promotional Material: Providing posters, pamphlets, or digital reminders promotes awareness and encourages healthcare workers and patients to maintain good hand hygiene.
- Local Policy Guidelines: Documenting institution-specific hand hygiene protocols aligns staff actions with established best practices, ensuring consistency in implementation across the facility.
- Equipment Maintenance Records: Keeping track of equipment used for hand hygiene (like dispensers and sinks) ensures that these resources are functional, thus preventing barriers to compliance.
In conclusion, using these various forms and documents alongside the Hand Hygiene Observation form creates a comprehensive approach to improving hand hygiene compliance. Each tool offers specific insights and data that can be leveraged to foster a culture of safety and accountability in healthcare settings.
Similar forms
- Patient Safety Incident Report: Like the Hand Hygiene Observation form, this document is used to track specific events, focusing on the safety of patients and adherence to protocols. It gathers detailed information to ensure improvements in practice and reduces future risks.
- Quality Improvement Checklist: Similar in purpose, this checklist helps healthcare facilities assess processes against established standards. Just as the Hand Hygiene Observation form monitors hand hygiene practices, this checklist identifies areas needing improvement in overall patient care.
- Infection Control Surveillance Form: This form tracks infection rates and adherence to infection control practices. Both documents rely on systematic observation and data collection, aiming to enhance patient and staff safety through better compliance.
- Staff Training Evaluation Form: Both documents focus on education and compliance, but the training evaluation form examines staff understanding and retention of practices. Effective training aims to reduce the need for many observations, similar to how hand hygiene education promotes proper behavior.
- Clinical Audit Form: This form evaluates the quality of care provided. Similar to the Hand Hygiene Observation form, it collects data through direct observations, helping identify trends and recommend changes to enhance care delivery.
- Patient Feedback Survey: Both tools are critical for assessing performance from a patient-centered perspective. While the Hand Hygiene Observation form assesses hygiene practices, the survey gathers patient insights, informing service improvement and ensuring quality care.
Dos and Don'ts
Dos:
- Introduce yourself to the health-care worker and the patient when appropriate.
- Explain the purpose of your observation clearly.
- Make sure to use a pencil for recording observations to allow for immediate corrections.
- Complete the header of the form before starting observations.
- Limit the observation session to a maximum of 20 minutes.
- Observe multiple health-care workers if possible, depending on the number of hand hygiene opportunities available.
- Record every detected hand hygiene opportunity accurately in the appropriate columns.
- Track missed hand hygiene actions in relation to the specific opportunities identified.
Don'ts:
- Do not use ink or permanent markers for recording observations.
- Avoid beginning the session without completing the header information first.
- Do not extend the observation time beyond 30 minutes under any circumstance.
- Refrain from merging data from different professional categories into a single column.
- Do not ignore any hand hygiene opportunity that arises; all should be counted.
- Do not record hand hygiene actions that occurred without a corresponding indication.
- Ensure not to report data without checking it for accuracy first.
- Do not record glove use unless the hand hygiene action was missed while wearing gloves.
Misconceptions
Misconception 1: The Hand Hygiene Observation form is only for auditing purposes.
This form is a tool for encouraging observed healthcare workers to improve their hand hygiene practices. While it can provide valuable data for auditing, its primary function is to enhance compliance through direct feedback.
Misconception 2: Observers are not required to introduce themselves.
Observers must introduce themselves to both the healthcare worker and the patient when appropriate. This approach fosters a collaborative environment and helps to alleviate any anxiety the healthcare worker may feel during the observation.
Misconception 3: The session duration can exceed 20 minutes.
The observation session is meant to last no more than 20 minutes. This time frame ensures that the data collected remains focused and manageable, allowing for more accurate results without overwhelming both the observer and the healthcare workers.
Misconception 4: Any mistakes made during the observation cannot be corrected.
Data should be recorded with a pencil, allowing immediate corrections if necessary. This flexibility encourages accuracy and reduces the fear of making mistakes while collecting important information.
Misconception 5: Only one healthcare worker can be observed at a time.
Observers may follow up to three healthcare workers simultaneously, provided that the density of hand hygiene opportunities allows for this. This practice enhances efficiency and maximizes the collected data during a single observation session.
Misconception 6: The data collected is automatically reliable.
While the form is designed for accurate data recording, the reliability of the information depends on the observer’s attentiveness and objectivity. The observer is responsible for the accuracy of data collection before submission for analysis.
Key takeaways
When using the Hand Hygiene Observation form, keep the following key points in mind:
- The observer should always introduce themselves to both the health-care worker and the patient, if relevant.
- It is essential to complete the header section of the form before data collection begins. This includes filling out the facility, service, ward, and date.
- Use a pencil for recording observations to allow for immediate corrections if necessary.
- Limit each observation session to about 20 minutes. Accurate start and end times should be recorded.
- Observations can include up to three health-care workers at once, depending on the number of hand hygiene opportunities available.
- Each column on the form corresponds to a specific health-care professional. Observers can either focus on a single worker in one column or multiple workers as long as they match the category.
- Count hand hygiene opportunities by marking the appropriate squares when indications for hand hygiene are observed.
- Register all corresponding hand hygiene actions, whether they were performed or missed, within the context of an opportunity.
- Use separate lines for each opportunity in different columns, allowing for detailed and organized data collection.
- Glove use may only be noted if a missed hand hygiene action occurs while the worker is wearing gloves.
Browse Other Templates
Cms-1490s Printable Form - The claimant’s signature signifies that the information provided is accurate to the best of their knowledge.
Register a Business in California - Barry County has specific provisions for conducting business that applicants must follow.