Fill Out Your Hdo Application Form
The HDO Application form is a critical document for organizations seeking participation in the Molina Healthcare network. This application is designed for initial credentialing or recredentialing and requires the submission of comprehensive information about the organization. It is essential to complete all sections of the form thoroughly; incomplete applications will be returned, causing delays in processing. The application requires pertinent organizational details, including legal names, facility licenses, and various identification numbers. Additionally, it mandates the inclusion of insurance coverage details, ensuring that liability insurance is in place. Organizations with multiple locations must follow specific guidelines regarding separate submissions or consolidated applications, depending on their accreditation status. Attachments, such as proof of CMS participation and the current liability insurance face sheet, are necessary to support the application. Ultimately, this form serves as the gateway for healthcare providers to establish their credentials with Molina Healthcare, underscoring the importance of accuracy and completeness throughout the application process.
Hdo Application Example

Molina Healthcare, Inc.
Health Delivery Organization (HDO) Application
INSTRUCTIONS:
Please submit this completed application and required attachments in order to apply for initial credentialing or recredentialing with Molina Healthcare. During initial credentialing, credentialing must be completed prior to completion of a contract for any organization/facility not currently contracted with Molina Healthcare. Approval of your credentialing does not constitute finalization/approval of your contract and network participation.
If your organization has more than one location:
•Complete a separate application for each of your locations if each location has had a separate state, CMS or accreditation survey.
•Complete one application which will cover all your locations if:
oYour organization has had one state, CMS and/or accreditation survey that covered all your locations on the same date(s), or
oYour organization is not accredited and not required to be surveyed by any state or federal organization as part of your licensure, registration and/or certification process.
•This application must be filled out completely with all sections answered:
oDo not use
oIf there is NOT a checkbox in the section header to indicate a why a section is not applicable, the section should be completed by all applicants.
•The information listed below should accompany the completed application:
Current organizational or facility licenses/certifications/registrations
A copy of the letter verifying approval of CMS participation (if applicable) Current liability insurance face sheet
W9 form(s) showing all federal Tax Identification Numbers (TINs) used by the organization/facility
(Only Page 1 of this form is needed:
•If your organization is not accredited by a body listed in Section 4 of this application and your organization is required to be certified by CMS or the State, we also request a copy of the most recent CMS or State
•Incomplete applications will be returned for completion prior to processing.
•Please return this application and all attachments to the location specified on your cover letter.
Revised: 12/05/2019 |
Page 1 of 5 |
Molina Healthcare, Inc.
Health Delivery Organization (HDO) Application
1. ORGANIZATION INFORMATION:
(Provide physical location information on the following page)
Legal Name of Organization
(Legal name listed with the IRS)
DBA Name of Organization (if applicable)
Historic Name(s) of Organization (if under same ownership)
Organization Medicare # (primary): |
|
|
Organization Medicaid # (primary): |
|
|||
|
|
|
|
|
|
|
|
Organization TIN (primary): |
|
|
|
Organization NPI (primary): |
|
||
|
|
|
|
|
|
|
|
Credentialing Contact |
|
|
|
Billing Address |
|
|
|
|
|
|
|
|
(if different than Credentialing) |
|
|
Street Address: |
|
|
|
|
Street Address: |
|
|
Address Line 2: |
|
|
|
|
Address Line 2: |
|
|
City: |
State: |
Zip: |
City: |
State: |
Zip: |
||
Contact |
|
|
|
Contact |
|
|
|
Name: |
|
|
|
Name: |
|
|
|
Email: |
|
|
|
Email: |
|
|
|
Phone: |
Fax: |
|
|
Phone: |
Fax: |
|
|
2. CURRENT INSURANCE COVERAGE:
(Please attach a copy of your current facility professional/general liability insurance
Please check here if your facility is not required to carry liability insurance.
|
|
Professional Liability Insurance Information (if available) |
|
|||
Current Carrier Name: |
|
|
|
Policy Number: |
|
|
Policy Start Date: |
|
Policy End Date: |
|
Policy Type |
|
|
|
|
(malpractice, general, etc.): |
|
|||
|
|
|
|
|
|
|
Coverage amount |
|
|
Coverage amount |
|
||
per occurrence: |
|
|
aggregate: |
|
||
|
General Liability Insurance Information |
(if no professional liability available) |
|
|||
Current Carrier Name: |
|
|
|
Policy Number: |
|
|
Policy Start Date: |
|
Policy End Date: |
|
Policy Type |
|
|
|
|
(malpractice, general, etc.): |
|
|||
|
|
|
|
|
|
|
Coverage amount per occurrence:
Coverage amount aggregate:
Revised: 12/05/2019 |
Page 2 of 5 |
Molina Healthcare, Inc.
Health Delivery Organization (HDO) Application
COMPLETE THE BELOW INFORMATION FOR EACH PRACTICE LOCATION
Only include information for locations that you wish to be listed with Molina Healthcare.
Complete a copy of sections
between locations
3. PHYSICAL LOCATION INFORMATION:
(Include any additional information relevant to this location on a separate sheet)
Location DBA
(if different than the Organization DBA)
Other DBAs Previously Used (if under same ownership)
Is this location Medicare Certified? |
|
|
Yes |
|
No |
Is this the primary address? |
|
|
Yes |
|
|
No |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
Physical Practice Location |
|
|
|
|
|
|
State provider # (if applicable, LTC, etc.): |
|
|
|
|
|
|||||||||||
Street Address: |
|
|
|
|
|
|
|
|
|
|
Is this location handicap accessible? |
|
|
Yes |
|
|
No |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Address Line 2: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
City: |
|
State: |
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Phone: |
|
Fax: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Please list any languages spoken by office personnel:
Practice Limitations (e.g., age, gender, etc.):
Location State License(s) and/or State Registration(s)
Please check here if this location is not required to be licensed, certified, or registered by a State agency.
Type of Credential |
State |
Number |
Expiration Date |
Most Recent Survey Date |
State License |
|
|
|
|
|
|
|
|
|
State Registration |
|
|
|
|
State Certification |
|
|
|
|
Other: |
|
|
|
|
Additional Location Credentials
Please check here if this location holds no additional licenses, certificates, registrations, etc.
Type of Credential |
State |
Number |
Expiration Date |
Additional Notes/Info |
DEA |
|
|
|
|
CLIA |
|
|
|
|
|
|
|
|
|
State CSR/CDS/DPS |
|
|
|
|
|
|
|
|
|
Other: |
|
|
|
|
|
|
|
|
|
Specialty & Federal Taxonomy Code
Specialty & Federal Taxonomy Code
Revised: 12/05/2019 |
Page 3 of 5 |
Molina Healthcare, Inc.
Health Delivery Organization (HDO) Application
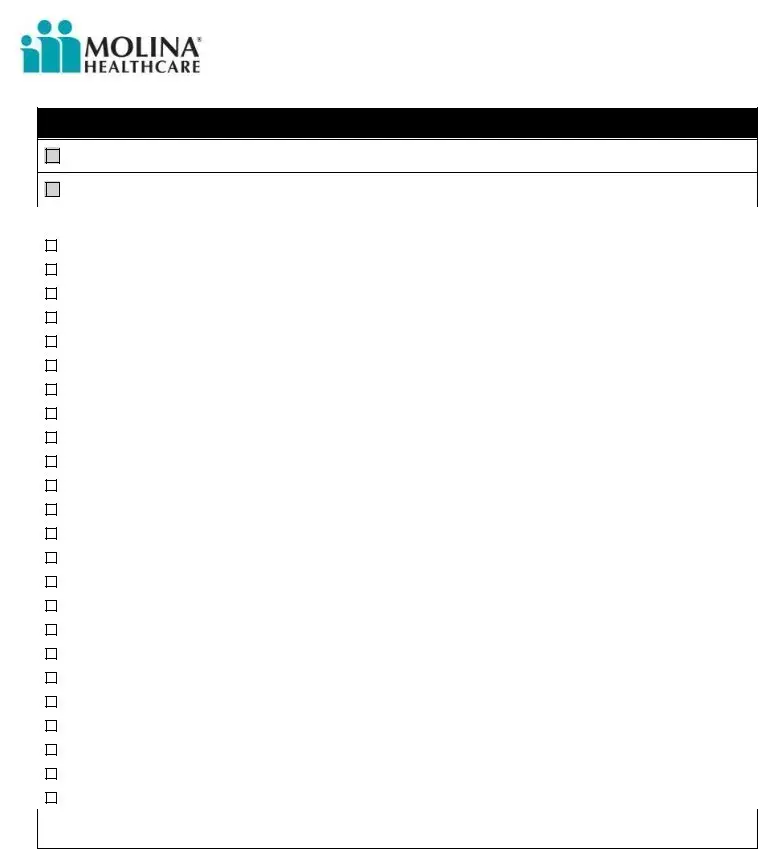
4. ACCREDITATION / CERTIFICATION (check all that apply):
Please check here if the State conducts routine surveys of your organization for license, registration, or clinical oversight.
Please check here if your organization is NOT accredited and NOT required to be surveyed by ANY organization.
|
|
|
Accreditation Organization |
Date of Last Survey |
|
|
|
|
|
|
|
(CMS) |
Medicare Certification (attach most recent survey and acceptance letter) |
|
|
|
|
||
|
|
|
|
|
|
|
(AAAHC) |
Accreditation Association for Ambulatory Health Care |
|
|
|
|
||
|
|
|
|
|
|
|
(ACHC) |
Accreditation Commission for Health Care |
|
|
|
|
||
|
|
|
|
|
|
|
(AAAASF) |
American Association for Accreditation of Ambulatory Surgery Facilities |
|
|
|
|
||
|
|
|
|
|
|
|
(ABCOP) |
American Board for Certification in Orthotics/Prosthetics |
|
|
|
|
||
|
|
|
|
|
|
|
(ACR) |
American College of Radiology |
|
|
|
|
||
|
|
|
|
|
|
|
(ASHI) |
American Society for Histocompatibility and Immunogenetics |
|
|
|
|
||
|
|
|
|
|
|
|
(BOC) |
Board of Certification / Accreditation, International (O&P or DMEPOS) |
|
|
|
|
||
|
|
|
|
|
|
|
(CAP) |
College of American Pathologists |
|
|
|
|
||
|
|
|
|
|
|
|
(CARF) |
Commission on Accreditation of Rehabilitation Facilities |
|
|
|
|
||
|
|
|
|
|
|
|
(COLA) |
Committee of Laboratory Accreditation |
|
|
|
|
||
|
|
|
|
|
|
|
(CHAP) |
Community Health Accreditation Program |
|
|
|
|
||
|
|
|
|
|
|
|
(CT) |
The Compliance Team |
|
|
|
|
||
|
|
|
|
|
|
|
(COA) |
Council on Accreditation |
|
|
|
|
||
|
|
|
|
|
|
|
(DNV) |
Det Norske Veritas |
|
|
|
|
||
|
|
|
|
|
|
|
(HFAP) |
Healthcare Facilities Accreditation Program - AOA |
|
|
|
|
||
|
|
|
|
|
|
|
(HQAA) |
Healthcare Quality Association on Accreditation |
|
|
|
|
||
|
|
|
|
|
|
|
(IAC) |
The Intersocietal Accreditation Commission |
|
|
|
|
||
|
|
|
|
|
|
|
(NABP) |
National Association of Boards of Pharmacy |
|
|
|
|
||
|
|
|
|
|
|
|
(NBAOS) |
National Board of Accreditation for Orthotics Suppliers |
|
|
|
|
||
|
|
|
|
|
|
|
(NCQA) |
National Commission for Quality Assurance |
|
|
|
|
||
|
|
|
|
|
|
|
(TJC) |
The Joint Commission |
|
|
|
|
||
|
|
|
|
|
|
|
(URAC) |
URAC, (aka, American Accreditation Healthcare Commission) |
|
|
|
|
||
|
|
|
|
|
|
|
(*CABC) |
*Commission for the Accreditation of Birth Centers |
|
|
|
|
||
|
|
|
|
|
*Molina only recognizes accreditation by CMS ‘Deemed’ bodies except for The CABC for ‘Birthing Centers’ and PPFA for ‘Planned Parenthood’ facilities.
Revised: 12/05/2019 |
Page 4 of 5 |

Molina Healthcare, Inc.
Health Delivery Organization (HDO) Application
ATTESTATION AND RELEASE OF INFORMATION
FORM Modifications Will Not Be Accepted
RELEASE OF INFORMATION:
As part of the application process and for the purpose of verifying any information provided on this application, I, the undersigned authorized agent of the applicant facility/organization, grant Molina Healthcare permission to contact any individual, institution, facility or agency identified on, or relative to, this application. Further, I hereby consent and authorize Molina Healthcare to request, receive and inspect any and all records pertinent to consideration of this application.
As a Molina Healthcare facility/organization applicant, I, the undersigned authorized agent, acknowledge that I am required to supply Molina Healthcare with any information and documentation necessary and relevant to the review of this application.
SITE REVIEW AUTHORIZATION:
I hereby grant permission for Molina Healthcare to conduct
ATTESTATION:
I certify the information on this entire application is complete, accurate, and current. I acknowledge that any misstatements in or omissions from this application constitute for denial or summary dismissal. A copy of this application has the same force and effect as the original. I have reviewed this information as of the most recent date listed below. I attest that the organization on this application maintains liability insurance as outlined by state requirements.
I acknowledge that decision of participation for the organization on this application will be delayed until all required information is received and/or verified. I acknowledge that acceptance of this application does not constitute approval or acceptance or participating status with Molina Healthcare and does not grant this facility any rights or privileges of participation until such time as a contract is consummated and written notice of participating status is issued to this facility by Molina Healthcare. All services rendered to Molina members must be individually authorized until a written notice of participation and conditions of participation is issued by Molina Healthcare.
This facility complies with all federal, state, and local handicapped access requirements as well as the standards required by the 1992 Federal Americans with Disabilities Act.
I certify that the appropriate state license or certification source is checked for all new employees or contracted service providers prior to the first provision of service. I certify that the appropriate state license or certification source is checked at least annually for existing and contracted service providers in order to ensure that every licensed individual providing services as a representative of the applicant holds a current license or certification to provide services. I certify that criminal background checks are conducted for all new employees or contracted service providers prior to the first provision of service. I certify the applicant does not employ or contract with any individual convicted of a felony for a
I certify that the
The individual executing this Attestation is duly authorized and has the proper authority and proper authorization to execute this Attestation and does so with the intent to fully bind Facility to the truthfulness of its answers.
Signature:
(Stamped signature is not acceptable)
Printed Name: |
|
Date: |
Revised: 12/05/2019 |
Page 5 of 5 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of Application | The HDO application facilitates the initial credentialing or recredentialing process with Molina Healthcare. |
| Submission Requirements | Applicants must submit the completed form along with required attachments for the processing to occur. |
| Separate Applications for Locations | Organizations with more than one location must submit separate applications if each location has undergone distinct surveys. |
| Complete Information | All sections of the application must be completed, and the use of white-out is prohibited. |
| Required Attachments | Along with the application, a copy of relevant licenses, CMS participation letters, and current insurance documents must be included. |
| Governing Laws | The application is subject to state and federal rules regarding health care credentialing and participation. |
| Incomplete Applications | Any application deemed incomplete will be returned for necessary information before processing begins. |
| Attestation Clause | The applicant must certify the accuracy of the information provided and consent to on-site reviews and verification procedures. |
Guidelines on Utilizing Hdo Application
Completing the HDO Application form is an essential step for organizations seeking initial credentialing or recredentialing with Molina Healthcare. The following steps will guide you through filling out the application accurately, ensuring that you have all the necessary information at hand.
- Gather Required Documents: Collect all necessary documents, including organizational licenses, CMS approval letters, and insurance information.
- Organization Information: Fill in the legal name, DBA name, historic names, and various numbers such as Medicare, Medicaid, TIN, and NPI.
- Credentialing Contact Details: Provide the contact name, email, phone, and fax for the individual handling credentialing.
- Insurance Coverage: Indicate whether your organization requires liability insurance. If applicable, enter insurance carrier names, policy numbers, and coverage amounts.
- Physical Location Information: Complete the sections for each practice location, specifying address, contact information, and whether the location is handicap accessible.
- Accreditation/Certification: Check all relevant accreditation options and provide the date of your last survey, if applicable.
- Attestation and Release of Information: Read and sign the attestation, consenting to allow Molina Healthcare to verify provided information and conduct site reviews.
- Review the Application: Ensure that all sections are completely filled out, and documents are attached. Do not use white-out on the application form.
- Submission: Submit the application and required documents to the address specified in your cover letter.
What You Should Know About This Form
1. What is the purpose of the HDO Application form?
The HDO Application form is utilized for the initial credentialing or recredentialing of health delivery organizations with Molina Healthcare. This process ensures that organizations meet required standards for participation in Molina's network. Successful completion of the application does not finalize contract approval but is a necessary step for organizations seeking to contract with Molina Healthcare.
2. What information must be included in the HDO Application?
The application must be filled out completely and include information such as the organization's legal name, Medicare and Medicaid numbers, Tax Identification Numbers (TINs), and National Provider Identifiers (NPIs). Incomplete applications will be returned for corrections before processing. Additionally, supporting documentation such as current licenses, proof of liability insurance, and the W9 form are required to accompany the application.
3. How should I submit the completed HDO Application?
The completed application, along with all required attachments, should be submitted to the address specified on your cover letter. Ensure that the application is complete and free of white-out or alterations, as these can cause delays or rejection.
4. What if my organization has multiple locations?
If your organization operates multiple locations, you may need to complete separate applications for each location, depending on your accreditation status and past surveys. For locations covered by a single survey, one application may be sufficient. Each location must provide relevant details as specified in the application form.
5. What happens if the application is incomplete?
Submitting an incomplete application will result in its return for completion prior to processing. It is crucial to ensure all sections are answered, even if the information is not applicable, to avoid delays in the credentialing process.
6. What accreditation documents are required with the HDO Application?
If your organization is accredited, you must provide documentation such as the most recent survey results and the letter verifying approval from CMS, if applicable. If not accredited and required to be certified by CMS or the State, you will need to submit the latest on-site survey results conducted by the appropriate agency.
7. What is the attestation section of the HDO Application?
The attestation section of the application requires the authorized agent to certify that the information provided is complete, accurate, and current. It also grants Molina permission to verify the information provided and conduct on-site reviews if necessary. Misstatements or omissions can lead to denial of the application, so accuracy is vital.
Common mistakes
Filling out the HDO Application form can be a straightforward process, but there are common mistakes that applicants often make. These mistakes can lead to delays or even rejection of the application. Understanding these pitfalls is essential for a successful submission.
One common error is failing to provide complete information. Every section of the application must be answered completely. Incomplete applications will be returned for further information, causing unnecessary delays. This includes not only the organization information but also current insurance coverage and physical location details.
Another mistake is the use of white-out or correction fluid on the application. This practice is prohibited, as it can obscure important information and may lead to the perception that the application is not being handled with care. It is essential to double-check entries and make corrections only by striking out the incorrect information and writing the correct information beside it.
Not understanding the requirements for multiple locations can also complicate the process. If an organization has more than one location, a separate application must be submitted for each if they have undergone different state or accreditation surveys. If unsure, it’s better to seek guidance on this matter before proceeding.
Inadequate documentation is another frequent misstep. All necessary attachments, such as licenses, certification approvals, and insurance coverage documents, must be included. Omitting these documents can lead to processing delays. If an organization isn't accredited, it's necessary to include recent survey results, as required.
Failing to provide the required contact details is also common and can hinder communication. Applicants often forget to fill out the contact name, email address, and phone numbers clearly. Ensuring this information is accurate and easily readable is vital for any follow-up communication.
Another mistake stems from misunderstanding accreditation requirements. Applicants sometimes check boxes incorrectly related to accreditation status or fail to check additional required boxes. It’s essential to thoroughly review the section on accreditation to ensure compliance and complete understanding.
Lastly, some applicants do not realize the importance of the attestation section. This section requires the authorized agent to certify that all information is accurate and complete. Neglecting to sign, date, or provide a printed name here can result in application delays. This signature signifies the commitment to uphold the information provided, which is integral to the approval process.
By being aware of these common mistakes and taking the necessary steps to avoid them, applicants can streamline the process of completing the HDO Application. Approaching the form with attention to detail can significantly enhance the chances of successful credentialing with Molina Healthcare.
Documents used along the form
The Health Delivery Organization (HDO) Application Form serves as a critical document in the credentialing process for healthcare organizations seeking to partner with Molina Healthcare. In order to complete this application effectively, several other documents are often required. Each of these documents plays a significant role in verifying the eligibility and operational status of the applying organization.
- Organizational Licenses/Certifications/Registrations: This document confirms that the healthcare organization holds the necessary state or federal licenses and certifications to operate legally. It ensures that the organization meets all relevant regulatory standards.
- Letter of CMS Participation Approval: If applicable, this letter serves as proof that the organization has received approval to participate in Medicare programs. It acts as a validation of the organization’s compliance with specific Medicare guidelines.
- Liability Insurance Face Sheet: This document details the organization's liability insurance coverage, including policy numbers and coverage amounts. It is essential for demonstrating the financial protection available in case of malpractice claims.
- W-9 Form: Organizations must provide a completed W-9 form to disclose their Tax Identification Numbers (TINs). This form is necessary for tax reporting purposes and ensures compliance with IRS regulations.
- CMS or State Survey Results: If the organization is not accredited, recent CMS or state survey results may be required. These results provide insight into the quality of care and operations of the organization, validating compliance with industry standards.
Submitting the proper accompanying documents with the HDO Application Form is crucial for a smooth credentialing process. Each document serves a purpose in establishing the qualifications and reliability of the healthcare organization, ultimately facilitating a successful partnership with Molina Healthcare.
Similar forms
-
Provider Credentialing Application: Like the HDO Application form, this document collects essential information for healthcare providers seeking to work with a specific health insurer. Both require detailed organizational information, including licensing, certifications, and insurance details.
-
Medicare Enrollment Application: This form is necessary for healthcare organizations or providers to enroll in the Medicare program. Similar to the HDO Application, it demands proof of current licensure and accreditation, ensuring that the applicants meet required standards.
-
State Licensing Application: Each state has its own licensing requirements for healthcare organizations. Much like the HDO Application, it mandates submission of detailed information regarding organizational structure, physical locations, and compliance with state regulations.
-
Facility Accreditation Application: When seeking accreditation from healthcare accreditation bodies, organizations must provide information about their policies, procedures, and standards. This process mirrors the HDO application in its depth of required documentation and commitment to quality care standards.
-
Insurance Provider Network Application: This application enables healthcare providers to become part of an insurance network, much like the HDO form. It entails documenting credentials, insurance coverages, and prior performance metrics.
-
National Practitioner Data Bank (NPDB) Report: This document collects data related to healthcare practitioners’ licenses, malpractice claims, and other professional behavior. It serves a similar purpose to the HDO application in assessing the validity and performance of healthcare organizations.
-
Credentialing Recredentialing Form: This form is completed at regular intervals for re-evaluation of healthcare providers. It resembles the HDO Application in its need for updated information regarding credentials, performance evaluations, and compliance with current regulations.
-
Corporate Insurance Information Form: This document outlines an organization’s liability coverage and risk management strategies. It parallels the HDO Application’s requirement for current insurance documentation, ensuring all entities have coverage in place.
-
Health Services Organization Application: This application is tailored for organizations providing a range of health services. Similar to the HDO Application, it requires comprehensive organizational details and a commitment to compliance with state and federal regulations.
-
Organizational Compliance Checklist: This checklist guides healthcare providers in ensuring adherence to legal and contractual obligations. It functions akin to the HDO Application by focusing on regulatory compliance and detailed documentation requirements.
Dos and Don'ts
10 Things to Do and Not to Do When Filling Out the HDO Application Form
- Do: Read all instructions carefully before starting the application.
- Do: Complete each section fully without leaving any blanks.
- Do: Submit all requested documents along with the application, such as licenses and insurance information.
- Do: Ensure the legal name of your organization matches the name registered with the IRS.
- Do: Use correct and updated contact information for your credentialing contact.
- Don't: Use white-out or any correction fluid on the application form.
- Don't: Forget to provide separate applications for multiple locations with differing information.
- Don't: Submit an incomplete application; it will be returned for correction.
- Don't: Assume your application is approved just because it has been submitted.
- Don't: Leave sections blank if there are no checkboxes indicating they are not applicable.
Misconceptions
- Misconception 1: The HDO Application can be submitted without all documentation.
- Misconception 2: Only accredited organizations need to complete the HDO Application.
- Misconception 3: You only need to submit one application for multiple locations.
- Misconception 4: White-out can be used on the application if needed.
- Misconception 5: The application is the only step in the credentialing process.
- Misconception 6: You can use any version of the W9 form for submission.
- Misconception 7: All applicants are automatically granted credentialing approval.
- Misconception 8: The application is optional for established facilities.
- Misconception 9: The application can be submitted via any method.
This is incorrect. A completed application must include all required documents. Incomplete applications will be returned, causing delays in processing.
This is not true. All organizations seeking initial credentialing or recredentialing with Molina Healthcare must submit this application, regardless of their accreditation status.
This depends on the situation. If each location has had separate surveys, a separate application is required for each. However, one application can be submitted if all locations have been surveyed on the same date or if they are not required to be surveyed.
Actually, using white-out on the application is not allowed. It is essential to fill out every section completely and clearly without alteration.
This is misleading. While the application is crucial, credentialing approval does not finalize network participation. A contract must also be completed for participation with Molina Healthcare.
This is incorrect; the application specifically requests Page 1 of a current W9 form showing all federal Tax Identification Numbers. It's important to use the correct version to avoid additional complications.
This is not the case. Credentialing approval is contingent upon meeting all requirements outlined in the application and additional evaluations by Molina Healthcare.
This is false. All facilities, including established ones, must submit the application for recredentialing or initial credentialing if seeking participation with Molina Healthcare.
It is important to follow specific submission guidelines. The application and all attachments should be sent to the location specified in the cover letter, as outlined in the instructions.
Key takeaways
- Complete Application: Fill out every section of the HDO Application form. Incomplete applications will be returned for completion.
- Separate Applications: If your organization has multiple locations with different surveys, use a separate application for each one.
- Attachments Required: Include necessary documents such as licenses, insurance information, and any CMS participation letters.
- Avoid White-Out: Do not use white-out on any part of the application; corrections should be made by crossing out and initialing.
- Contact Information: Provide accurate contact details for billing and credentialing purposes to ensure smooth communication.
- Insurance Details: Attach a copy of the current liability insurance face sheet and indicate if your facility is required to carry insurance.
- Survey and Accreditation: If the organization is not accredited, include the most recent CMS or State survey results if required.
- Signature Required: The application must be signed by an authorized agent, confirming accuracy and completeness of the provided information.
- Return Address: Send the completed application and attachments to the location specified in the cover letter, ensuring timely processing.
Browse Other Templates
Types of Advance Directives - This form can be revoked or changed at any time, as long as you communicate your wishes clearly.
Kinn's the Medical Assistant 14th Edition Study Guide Answer Key - Zachary Paul Staley's entries detail both charges for services and insurance reimbursements.
Surety Indemnity Agreement - The legal language supports a contract that is built on mutual trust and accountability.