Fill Out Your Health Practitioner Physical Assessment Form
The Health Practitioner Physical Assessment form serves as a vital instrument in evaluating the health status of residents within assisted living programs. Completed by qualified health professionals such as physicians, certified nurse practitioners, and registered nurses, this document includes key sections that cover various aspects of a resident's medical history and current health condition. Among its major components are inquiries about the resident’s recent medical and psychiatric history, including any hospitalizations or behavioral changes. The form also probes into allergies, communicable diseases, and substance abuse history, which are crucial for ensuring a safe living environment. Furthermore, it assesses risk factors for falls, skin conditions, sensory impairments, and nutritional status, all pivotal in tailoring appropriate care strategies. Cognition and behavioral status are also scrutinized, allowing healthcare providers to determine the individual’s ability to make health care decisions and to self-administer medications. The thoroughness of this assessment is underscored by Maryland’s regulations, which restrict admission for residents requiring extensive medical care, thus underscoring the need for comprehensive evaluations. Ultimately, the completion of this form plays a critical role in not only safeguarding the health of residents but also in guiding effective treatment plans that enhance their quality of life.
Health Practitioner Physical Assessment Example
1
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
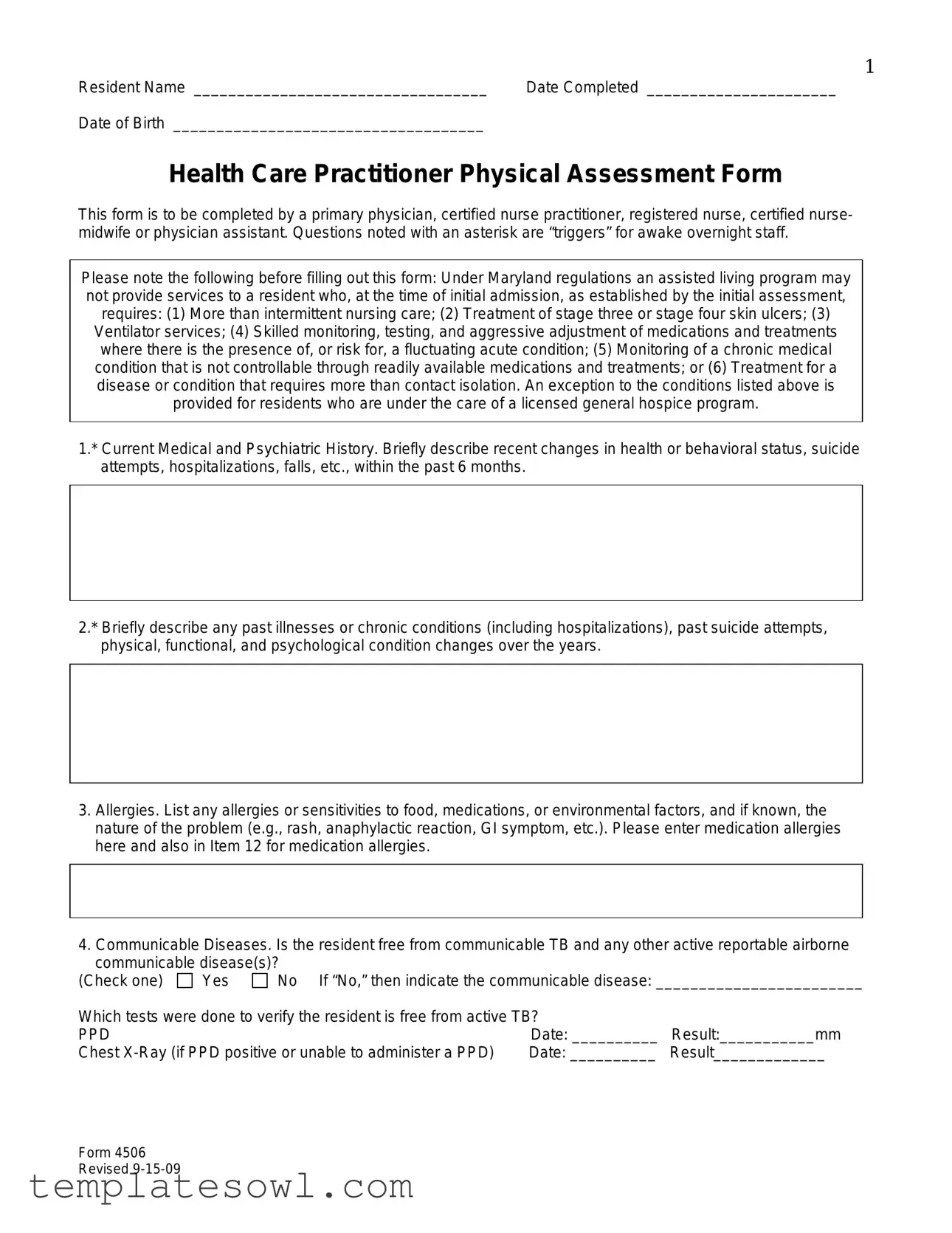
Health Care Practitioner Physical Assessment Form
This form is to be completed by a primary physician, certified nurse practitioner, registered nurse, certified nurse- midwife or physician assistant. Questions noted with an asterisk are “triggers” for awake overnight staff.
Please note the following before filling out this form: Under Maryland regulations an assisted living program may not provide services to a resident who, at the time of initial admission, as established by the initial assessment, requires: (1) More than intermittent nursing care; (2) Treatment of stage three or stage four skin ulcers; (3) Ventilator services; (4) Skilled monitoring, testing, and aggressive adjustment of medications and treatments where there is the presence of, or risk for, a fluctuating acute condition; (5) Monitoring of a chronic medical condition that is not controllable through readily available medications and treatments; or (6) Treatment for a disease or condition that requires more than contact isolation. An exception to the conditions listed above is provided for residents who are under the care of a licensed general hospice program.
1.* Current Medical and Psychiatric History. Briefly describe recent changes in health or behavioral status, suicide attempts, hospitalizations, falls, etc., within the past 6 months.
2.* Briefly describe any past illnesses or chronic conditions (including hospitalizations), past suicide attempts, physical, functional, and psychological condition changes over the years.
3.Allergies. List any allergies or sensitivities to food, medications, or environmental factors, and if known, the nature of the problem (e.g., rash, anaphylactic reaction, GI symptom, etc.). Please enter medication allergies here and also in Item 12 for medication allergies.
4.Communicable Diseases. Is the resident free from communicable TB and any other active reportable airborne communicable disease(s)?
(Check one) |
Yes |
No If “No,” then indicate the communicable disease: ________________________ |
||
Which tests were done to verify the resident is free from active TB? |
|
|||
PPD |
|
|
Date: __________ |
Result:___________mm |
Chest |
Date: __________ |
Result_____________ |
||
Form 4506 Revised
2
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
5.History. Does the resident have a history or current problem related to abuse of prescription,
(a)Substance: OTC,
1. |
Recent (within the last 6 months) |
Yes |
No |
2. |
History |
Yes |
No |
(b)Abuse or misuse of prescription medication or herbal supplements
1. |
Currently |
Yes |
No |
2. |
Recent (within the last 6 months) |
Yes |
No |
(c)History of
1. |
Currently |
Yes |
No |
2. |
Recent (within the last 6 months) |
Yes |
No |
(d)Describe misuse or abuse: _________________________________________________________
____________________________________________________________________________________
6.* Risk factors for falls and injury. Identify any conditions about this resident that increase his/her risk of falling or
injury (check all that apply): 
 orthostatic hypotension
orthostatic hypotension 
 osteoporosis
osteoporosis 
 gait problem
gait problem 
 impaired
impaired
balance  confusion
confusion  Parkinsonism
Parkinsonism  foot deformity
foot deformity  pain
pain  assistive devices
assistive devices  other (explain)
other (explain)
__________________________________________________________________________________________ |
|
||||||||||||||||
7.* Skin condition(s). Identify any history of or current ulcers, rashes, or skin tears with any standing treatment |
|
||||||||||||||||
orders. _________________________________________________________________________________ |
|
||||||||||||||||
__________________________________________________________________________________________ |
|
||||||||||||||||
8.* Sensory impairments affecting functioning. (Check all that apply.) |
|
|
|
|
|
|
|
||||||||||
(a) Hearing: |
Left ear: |
|
|
|
Adequate |
|
Poor |
Deaf |
|
Uses corrective aid |
|
|
|
||||
(b) Vision: |
Right ear: |
|
|
|
Adequate |
|
Poor |
Deaf |
|
Uses corrective aid |
|
|
|
||||
Adequate |
Poor |
|
Uses corrective lenses |
Blind (check all that apply) - |
R |
L |
|||||||||||
(c) Temperature Sensitivity: |
|
|
|
Normal |
Decreased sensation to: |
Heat |
Cold |
|
|
|
|||||||
9. Current Nutritional Status. |
Height |
|
|
inches |
|
|
Weight |
|
lbs. |
|
|
|
|
|
|||
(a) Any weight change (gain or loss) |
in the |
past 6 months? |
|
|
|
|
|
Yes |
No |
|
|
||||||
(b) How much weight change? |
|
|
lbs. in the past |
|
months (check one) |
Gain |
Loss |
|
|
||||||||
(c) Monitoring necessary? (Check one.) |
|
|
|
|
|
|
|
Yes |
No |
|
|
||||||
If items (a), (b), or (c) are checked, explain how and at what frequency monitoring is to occur: ___________ |
|
||||||||||||||||
__________________________________________________________________________________________ |
|
||||||||||||||||
(d) Is there evidence of malnutrition or risk for undernutrition? |
|
|
|
Yes |
No |
|
|
||||||||||
(e)* Is there evidence of dehydration or a risk for dehydration? |
|
|
|
Yes |
No |
|
|
||||||||||
(f) Monitoring of nutrition or hydration status necessary? |
|
|
|
|
|
Yes |
No |
|
|
||||||||
If items (d) or (e) are checked, explain how and at what frequency monitoring is to occur: _______________
__________________________________________________________________________________________
(g)Does the resident have medical or dental conditions affecting: (Check all that apply)
 Chewing
Chewing  Swallowing
Swallowing  Eating
Eating  Pocketing food
Pocketing food  Tube feeding
Tube feeding
(h)Note any special therapeutic diet (e.g., sodium restricted, renal, calorie, or no concentrated sweets restricted): _________________________________________________________________________________
__________________________________________________________________________________________
(i)Modified consistency (e.g., pureed, mechanical soft, or thickened liquids): _________________________
__________________________________________________________________________________________
(j) Is there a need for assistive devices with eating (If yes, check all that apply): |
Yes |
No |
||
Weighted spoon or built up fork |
Plate guard |
Special cup/glass |
|
|
(k) Monitoring necessary? (Check one.) |
|
|
Yes |
No |
If items (g), (h), or (i) are checked, please explain how and at what frequency monitoring is to occur:
__________________________________________________________________________________________
Form 4506 Revised
3
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
10.* Cognitive/Behavioral Status.
(a)* Is there evidence of dementia? (Check one.)
(b) Has the resident undergone an evaluation for dementia? (c)* Diagnosis (cause(s) of dementia): 

(d)
Yes |
No |
Yes |
No |

 Other
Other
10(e)* Instructions for the following items: For each item, circle the appropriate level of frequency or intensity, depending on the item. Use the “Comments” column to provide any relevant details.
Item 10(e) |
A |
B* |
C* |
|
D* |
Comments |
|
|
|
Cognition |
|
|
|
I. Disorientation |
Never |
Occasional |
Regular |
|
Continuous |
|
II. Impaired recall |
Never |
Occasional |
Regular |
|
Continuous |
|
(recent/distant events) |
|
|
||||
|
|
|
|
|
|
|
III. Impaired judgment |
Never |
Occasional |
Regular |
|
Continuous |
|
IV. Hallucinations |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
V. Delusions |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
Communication |
|
|
|
VI. Receptive/expressive |
Never |
Occasional |
Regular |
|
Continuous |
|
aphasia |
|
|
||||
|
|
|
|
|
|
|
|
|
Mood |
and Emotions |
|
|
|
VII. Anxiety |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
VIII. Depression |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
Behaviors |
|
|
|
IX. Unsafe behaviors |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
X. Dangerous to self or |
Never |
Occasional |
Regular |
|
Continuous |
|
others |
|
|
||||
|
|
|
|
|
|
|
XI. Agitation (Describe |
|
|
|
|
|
|
behaviors in comments |
Never |
Occasional |
Regular |
|
Continuous |
|
section) |
|
|
|
|
|
|
10(f) Health care
(a) Probably can make higher level decisions (such as whether to undergo or withdraw
(b) Probably can make limited decisions that require simple understanding.
(c) Probably can express agreement with decisions proposed by someone else.
(d) Cannot effectively participate in any kind of health care
11.* Ability to
(a) Independently without assistance
(b) Can do so with physical assistance, reminders, or supervision only
(c) Need to have medications administered by someone else
___________________________________ |
________________ |
Print Name |
Date |
______________________________________ |
|
Signature of Health Care Practitioner |
|
Form 4506 Revised
4
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
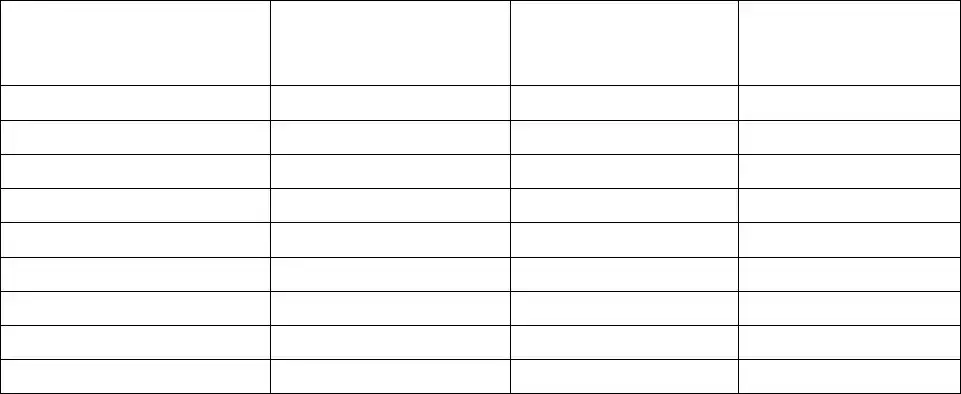
PRESCRIBER’S MEDICATION AND TREATMENT ORDERS AND OTHER INFORMATION
Allergies (list all): ___________________________________________________________________________________________________________________
Note: Does resident require medications crushed or in liquid form? Indicate in 12(a) with medication order. If medication is not to be crushed please indicate.
12(a) Medication(s). Including PRN, OTC, herbal, & dietary supplements.
Include dosage route (p.o., etc.), frequency, duration (if limited).
12(b) All related diagnoses, problems, conditions.
Please include all diagnoses that are currently being treated by this medication.
12(c) Treatments (include frequency & any instructions about when to notify the physician).
Please link diagnosis, condition or problem as noted in prior sections.
12(d) Related testing or monitoring.
Include frequency & any instructions to notify physician.
Prescriber’s Signature ________________________________________________________ |
Date |
______________________________ |
Office Address ______________________________________________________________ |
Phone |
______________________________ |
Form 4506 Revised
5
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
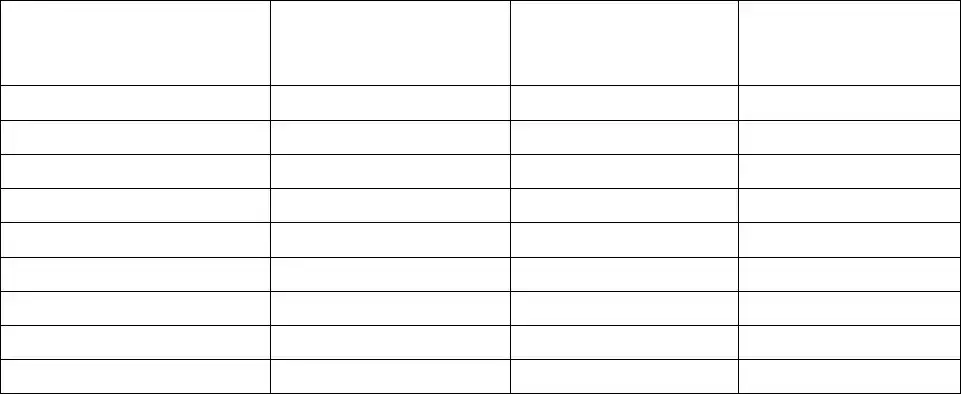
PRESCRIBER’S MEDICATION AND TREATMENT ORDERS AND OTHER INFORMATION
Allergies (list all): ___________________________________________________________________________________________________________________
Note: Does resident require medications crushed or in liquid form? Indicate in 12(a) with medication order. If medication is not to be crushed please indicate.
12(a) Medication(s). Including PRN, OTC, herbal, & dietary supplements.
Include dosage route (p.o., etc.), frequency, duration (if limited).
12(b) All related diagnoses, problems, conditions.
Please include all diagnoses that are currently being treated by this medication.
12(c) Treatments (include frequency & any instructions about when to notify the physician).
Please link diagnosis, condition or problem as noted in prior sections.
12(d) Related testing or monitoring.
Include frequency & any instructions to notify physician.
Prescriber’s Signature ________________________________________________________ |
Date |
______________________________ |
Office Address ______________________________________________________________ |
Phone |
______________________________ |
Form 4506 Revised
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Health Practitioner Physical Assessment form is designed to assess the health and well-being of residents in assisted living programs. It serves to ensure that basic healthcare needs are met before admission. |
| Governing Regulation | In Maryland, the regulations governing the use of this form state that assisted living programs cannot admit residents who require more than intermittent nursing care or who present with specific medical needs listed in the form. |
| Completing Authority | The form must be completed by authorized healthcare professionals, such as primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, or physician assistants. |
| Trigger Questions | Questions marked with an asterisk (*) are considered "triggers" for overnight staff to monitor residents more closely based on their health or behavioral responses. |
| Allergy Information | The form includes a section for listing any allergies, including medications and environmental factors. This helps ensure the safety and appropriate care of residents. |
| Substance Abuse History | It assesses whether the resident has a history or current issue with the abuse of drugs or alcohol, including prescription medication misuse, to inform care strategies. |
| Cognitive Assessment | The form examines cognitive and behavioral status, seeking evidence of conditions such as dementia, which can impact decision-making and care needs. |
| Monitoring Requirements | Specific items on the form require the healthcare practitioner to indicate if monitoring is necessary for nutritional or hydration status, as well as other health indicators. |
Guidelines on Utilizing Health Practitioner Physical Assessment
Completing the Health Practitioner Physical Assessment form is important for ensuring the health and safety of the resident. This form gathers essential information regarding their medical history, current health status, and potential needs. By following these steps carefully, you can provide the necessary details for a comprehensive assessment.
- Begin by filling in the resident's name, date completed, and date of birth at the top of the form.
- For Current Medical and Psychiatric History, briefly note any recent changes in health or behavioral status such as hospitalizations or falls over the past six months.
- In the section called Past Illnesses and Conditions, describe any historical medical issues, including previous hospitalizations or chronic conditions.
- List any allergies or sensitivities, specifically to food, medications, or environmental factors, along with the nature of the reaction.
- Indicate whether the resident is free from communicable diseases by checking 'Yes' or 'No' and providing details regarding testing for TB.
- Assess the history of substance abuse by answering the provided questions regarding prescription medication, over-the-counter drugs, and alcohol use.
- Identify any risk factors for falls or injury by checking all applicable conditions that apply to the resident.
- Note any skin conditions and detail any current ulcers, rashes, or skin issues that require treatment.
- Provide details on the resident's nutritional status, including height, weight, and any recent weight changes.
- Check for any cognitive or behavioral issues, including dementia symptoms, and provide details related to cognitive assessments.
- Rate the resident’s ability to self-administer medications based on their physical and cognitive capabilities.
- Fill out the prescriber's medication and treatment orders, listing all allergies, medications including dosages, and any related diagnoses or conditions.
- Provide the prescriber’s details, including their signature, date, office address, and phone number.
What You Should Know About This Form
What is the purpose of the Health Practitioner Physical Assessment form?
The Health Practitioner Physical Assessment form is designed for healthcare providers to document a resident’s medical and psychiatric history, current health status, and any specific needs. It helps ensure that residents receive the appropriate care and supports the overall assessment process in assisted living programs.
Who is authorized to complete this form?
This form should be completed by qualified healthcare professionals such as a primary physician, certified nurse practitioner, registered nurse, certified nurse-midwife, or physician assistant. Their expertise ensures accurate assessments and compliance with healthcare regulations.
What information is required regarding allergies?
Allergies or sensitivities to foods, medications, and environmental factors must be listed. It's important to specify the type of reaction experienced, such as a rash or gastrointestinal symptoms. Additionally, medication allergies should be mentioned both in this section and another designated area later in the form.
What is the significance of "triggers" marked with an asterisk?
Questions marked with an asterisk indicate critical information that the overnight staff must be aware of immediately. This includes changes in health status or risk factors. Addressing these triggers is essential for resident safety and health management.
How do I document recent changes in health or behavioral status?
In the section regarding current medical and psychiatric history, briefly describe any significant changes within the last six months. This could include hospitalizations, suicide attempts, or falls. Providing clear, concise information helps healthcare providers make informed decisions about the resident’s care.
What should be included in the nutritional status section?
The nutritional status section requires details such as height, weight, and any recent weight changes. It also includes questions about malnutrition, hydration risks, and any specific dietary needs or assistive devices required during meals. The answers will guide monitoring and care plans.
How does the form address cognitive and behavioral issues?
Sections assess cognitive status, including disorientation, impaired recall, and any signs of anxiety or depression. Providers can detail the resident's ability to make healthcare decisions. This information is crucial for tailoring care strategies that meet the resident’s cognitive abilities.
What steps should be taken if a resident has a history of substance abuse?
The form contains a section to record any history of substance abuse regarding prescription, non-prescription, or illegal drugs. Marking “yes” for current or recent issues allows healthcare staff to implement necessary interventions and provides vital information for ongoing health management.
Common mistakes
Filling out the Health Practitioner Physical Assessment form requires careful attention to detail. One common mistake is leaving fields blank that should be filled in, such as the resident’s name and date of birth. This essential information is vital for proper identification and tracking of medical history.
Another frequent error involves the omission of significant medical and psychiatric history. Residents may neglect to mention recent changes in health or any hospitalizations. These details are crucial for providing accurate care. If past illnesses or psychiatric conditions are not well documented, the assessment may not reflect the resident's true health status.
Some practitioners mistakenly do not specify the allergies a resident might have. Listing food, medication, or environmental allergies is critical. Additionally, indicating the severity of the reactions can protect residents from potential harm. Failing to do this disregards an important aspect of the resident's safety.
When checking for communicable diseases, another error can occur if the practitioner does not confirm previous tests for Tuberculosis (TB). Omitting to document the results of tests conducted can lead to severe public health risks. Clear verification is necessary to ensure the resident can safely be in an assisted living environment.
Risks associated with falls and injuries need careful examination. Often, critical information about fall risk factors is overlooked. Checking all relevant boxes ensures that caregivers are aware of risk factors, such as impaired balance or confusion. Failing to identify these risks can have serious consequences for the resident's safety.
Another mistake is providing incomplete information regarding the resident's dietary needs. It is essential to record any special diets and conditions affecting eating, such as chewing or swallowing difficulties. Incomplete details might lead to malnutrition or other health complications.
During the cognitive and behavioral assessment, practitioners sometimes forget to document evidence of dementia properly. This includes checking if the resident has undergone any evaluations. Without this information, care plans may not be adequately tailored to meet the individual’s needs.
Additionally, practitioners may inaccurately assess a resident’s ability to self-administer medications. Misjudging this capacity can lead to residents being unsafe with their medications. This assessment should be clear and reflective of the resident’s actual abilities.
Lastly, consistency is key in filling out the forms. Practitioners may use abbreviations or different terms for the same conditions throughout the form, leading to confusion about a resident’s health. It’s crucial to maintain uniformity in language and terminology to help avoid miscommunication among health care staff.
Documents used along the form
The Health Practitioner Physical Assessment form is a critical document used in the assessment and documentation of a resident's health status within various care settings. Alongside this form, several other documents may be necessary to ensure comprehensive care and accurate record-keeping. Here’s a list of some commonly used forms and documents associated with this assessment process.
- Medication Administration Record (MAR): This document tracks all medications administered to a resident, including dosage, frequency, and the person who administered the medication. It ensures accountability and aids in preventing medication errors.
- Care Plan: Developed after initial assessments, this outlines personalized care strategies based on the resident's needs. It targets specific health outcomes and can be updated regularly to reflect changes in the resident's condition.
- Progress Notes: These notes are made by healthcare providers documenting the resident's ongoing condition, treatment responses, and any significant changes. They provide a complete picture of the resident's health and care over time.
- Incident Report: This form is used to document any unusual events, such as falls or injuries. It helps analyze incidents to improve safety protocols and prevent future occurrences.
- Nutrition Assessment Form: This document evaluates the resident's dietary needs and current nutritional status. It is crucial for identifying any risks of malnutrition and planning the appropriate dietary interventions.
- Fall Risk Assessment: This assessment identifies residents who may be at increased risk of falling based on various criteria such as mobility, medications, and health conditions. It informs care strategies to minimize these risks.
- Palliative Care Assessment: If a resident is receiving palliative care, this assessment focuses on their quality of life, addressing physical, emotional, and spiritual needs to enhance overall well-being.
- Advance Care Directive: This document outlines a resident's preferences for medical treatment and care in the event that they are unable to communicate their wishes. It ensures that healthcare decisions align with the resident's values and desires.
Understanding these forms and their purposes is essential for healthcare providers in ensuring high-quality care. Together, they create a framework for managing resident health effectively and compliantly, enhancing the overall safety and well-being of individuals in care facilities.
Similar forms
- Comprehensive Assessment Form: Similar to the Health Practitioner Physical Assessment form, a Comprehensive Assessment Form gathers detailed information about a person's health history, physical condition, and any ongoing medical issues. Both forms aim to provide a complete overview of the individual's health status to aid in treatment planning.
- Patient Intake Form: The Patient Intake Form collects essential personal and medical history at the start of care. Like the Health Practitioner Physical Assessment form, it addresses previous health issues and current conditions to establish a baseline for care.
- Medication Reconciliation Form: This form tracks all medications a patient is taking, similar to how the Health Practitioner Physical Assessment form documents medications and treatment orders. Both are crucial for ensuring safe medication management and avoiding interactions.
- Nutritional Assessment Form: A Nutritional Assessment Form helps evaluate a patient’s dietary needs and restrictions. Similar to the nutrition section of the Physical Assessment form, it assesses dietary intake and any weight changes or nutritional deficiencies.
- Fall Risk Assessment Form: This form identifies individuals at risk of falling. It parallels the Health Practitioner Physical Assessment form's section on risk factors for falls and injury, both aiming to minimize risks in a care setting.
- Psychosocial Assessment Form: A Psychosocial Assessment Form evaluates a person's mental health and social circumstances. Like the Health Practitioner Physical Assessment form, it addresses psychological conditions and provides insights necessary for comprehensive care.
- Advance Directive Form: This document outlines a patient's preferences for medical care. It aligns with the Health Practitioner Physical Assessment form by ensuring that health care providers are aware of the individual’s wishes, particularly regarding life-sustaining treatment.
Dos and Don'ts
When filling out the Health Practitioner Physical Assessment form, attention to detail is essential. Here are eight important do's and don'ts to keep in mind:
- Do read the instructions carefully to understand each section.
- Do provide accurate and complete information regarding the resident's medical history.
- Do list all known allergies and sensitivities clearly.
- Do ensure that all required tests, like PPD for TB, are documented correctly.
- Don't skip any sections marked with an asterisk, as these may require special attention.
- Don't use abbreviations or unclear terms that could lead to misunderstandings.
- Don't leave any questions unanswered if the information is available.
- Don't forget to double-check for any errors before submission.
Misconceptions
Misunderstandings about the Health Practitioner Physical Assessment form can lead to errors in patient care. Below are nine common misconceptions:
- Only doctors can complete this form. In reality, certified nurse practitioners, registered nurses, nurse midwives, and physician assistants are all qualified to fill out the assessment.
- The form is only for initial admissions. This is incorrect. The form is also useful for ongoing assessments to monitor changes in a resident’s health status.
- All questions on the form must be answered. While thorough information is beneficial, some questions are optional. Focus on relevant information pertaining to the resident's condition.
- All triggers marked with an asterisk are mandatory for admission. These triggers indicate areas of concern but do not solely determine admission eligibility. Providers should evaluate each case individually.
- Negative answers to communicable disease questions mean the resident is healthy. A negative response does not guarantee overall health. It is essential to consider the full medical history and current status.
- The form is identical in every state. This is not true. Each state may have different regulations and requirements for physical assessments in assisted living or care facilities.
- The nutritional status section only pertains to weight changes. While weight is a significant factor, the section also addresses hydration, food consistency, and nutritional needs which are crucial for overall health.
- If a resident requires monitoring, it indicates poor health. This is misleading. Continuous monitoring can be part of a proactive approach to managing chronic conditions effectively.
- Assisted living facilities have no restrictions based on this form. In fact, Maryland regulations specify what care services may be provided based on an initial assessment, ensuring proper resident placement.
Addressing these misconceptions is vital for accurate assessments and appropriate care in assisted living settings.
Key takeaways
Filling out the Health Practitioner Physical Assessment form accurately is crucial for the proper care of residents. Here are key takeaways to keep in mind:
- Importance of Accuracy: Ensure that all information provided is complete and accurate. Any omissions can affect the quality of care.
- Regulatory Compliance: Understand the regulations that govern assisted living services in Maryland, highlighting the need for proper assessments related to nursing care and medical conditions.
- Trigger Questions: Pay close attention to questions marked with an asterisk. These items are critical for alerting staff to potential risks or necessary interventions.
- Medical History: Thoroughly document the resident's current and past medical history, including any psychiatric issues and hospitalizations. Such details inform appropriate care strategies.
- Allergens and Sensitivities: List out any allergies or sensitivities, as failing to do so could lead to severe reactions during care.
- Monitoring Requirements: Identify any necessary ongoing monitoring related to nutrition, hydration, or cognitive status. Specify frequency and methods for these observations.
Browse Other Templates
Fbar Limit - Any item marked with an asterisk is considered critical and must be filled out.
Negative Drug Test Results Form - Identifies the reason for the drug test.