Fill Out Your Healthnet Prior Authorization Form
Navigating the healthcare system can often feel overwhelming, especially when it comes to securing necessary medications for patients. One crucial step in this process is the completion of the Healthnet Prior Authorization form. This form plays an essential role in managing the coverage for specific blood clotting disorder medications, including FEIBA VH, FEIBA NF, NovoSeven, and NovoSeven RT. When the prescribing physician submits the request, prompt attention to detail becomes vital, as any blank or illegible sections may push back the approval timeline. Key components of the form include essential patient information, such as names and contact details, alongside specific questions that clarify the treatment's circumstances. For example, the form inquires whether the request is for initial therapy or ongoing treatment, while also prompting the physician to specify the patient's diagnosis. Strong supporting documentation can significantly impact the approval process, and this form allows for the inclusion of any pertinent medical history or clinical information. Understanding the nuances of the Healthnet Prior Authorization form can streamline the authorization process, ensuring patients receive their necessary treatments swiftly.
Healthnet Prior Authorization Example
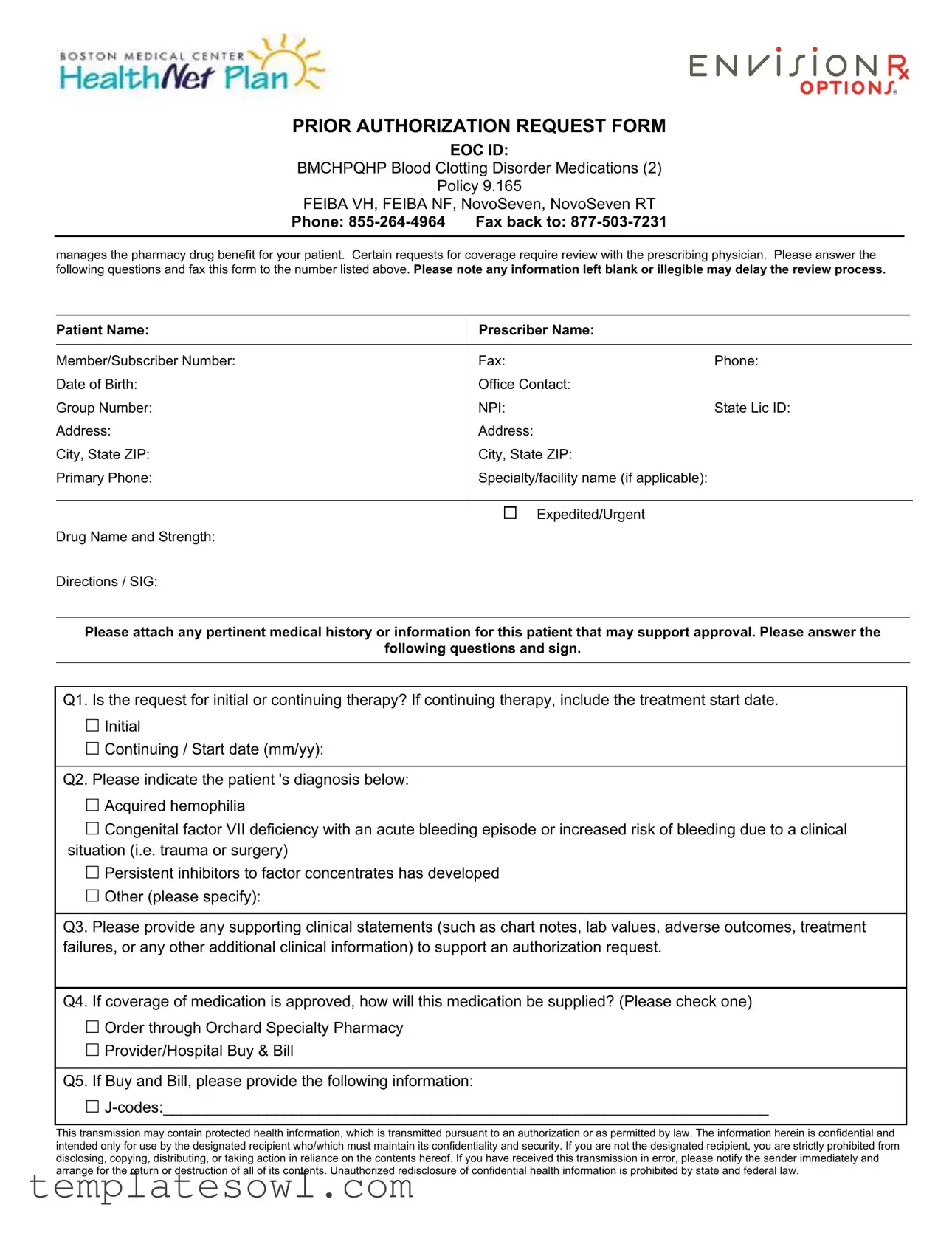
PRIOR AUTHORIZATION REQUEST FORM
EOC ID:
BMCHPQHP Blood Clotting Disorder Medications (2)
Policy 9.165
FEIBA VH, FEIBA NF, NovoSeven, NovoSeven RT
Phone:
manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. Please note any information left blank or illegible may delay the review process.
Patient Name: |
Prescriber Name: |
|
|
|
|
|
|
Member/Subscriber Number: |
Fax: |
Phone: |
|
Date of Birth: |
Office Contact: |
|
|
Group Number: |
NPI: |
State Lic ID: |
|
Address: |
Address: |
|
|
City, State ZIP: |
City, State ZIP: |
|
|
Primary Phone: |
Specialty/facility name (if applicable): |
|
|
|
|
|
|
|
Expedited/Urgent |
|
|
Drug Name and Strength: |
|
|
|
Directions / SIG: |
|
|
|
Please attach any pertinent medical history or information for this patient that may support approval. Please answer the
following questions and sign.
Q1. Is the request for initial or continuing therapy? If continuing therapy, include the treatment start date.
Initial
Continuing / Start date (mm/yy):
Q2. Please indicate the patient 's diagnosis below:
Acquired hemophilia
Congenital factor VII deficiency with an acute bleeding episode or increased risk of bleeding due to a clinical situation (i.e. trauma or surgery)
Persistent inhibitors to factor concentrates has developed
Other (please specify):
Q3. Please provide any supporting clinical statements (such as chart notes, lab values, adverse outcomes, treatment failures, or any other additional clinical information) to support an authorization request.
Q4. If coverage of medication is approved, how will this medication be supplied? (Please check one)
Order through Orchard Specialty Pharmacy
Provider/Hospital Buy & Bill
Q5. If Buy and Bill, please provide the following information:
This transmission may contain protected health information, which is transmitted pursuant to an authorization or as permitted by law. The information herein is confidential and intended only for use by the designated recipient who/which must maintain its confidentiality and security. If you are not the designated recipient, you are strictly prohibited from disclosing, copying, distributing, or taking action in reliance on the contents hereof. If you have received this transmission in error, please notify the sender immediately and arrange for the return or destruction of all of its contents. Unauthorized redisclosure of confidential health information is prohibited by state and federal law.
PRIOR AUTHORIZATION REQUEST FORM
EOC ID:
BMCHPQHP Blood Clotting Disorder Medications (2)
Policy 9.165
FEIBA VH, FEIBA NF, NovoSeven, NovoSeven RT
Phone:
manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. Please note any information left blank or illegible may delay the review process.
Patient Name:
Prescriber Name:
Procedure code(s) for administration of medication:____________________________________
Number of Units and Visits:_______________________________________________________
Date of planned administration:____________________________________________________
___________________________________________________________ |
_________________________________________ |
Prescriber Signature |
Date |
This telecopy transmission contains confidential information belonging to the sender that is legally privileged. This information is intended only for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other party. If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution or action taken in reference to the contents of this document is strictly prohibited. If you have received this telecopy in error, please notify the sender immediately to arrange for the return of this document.
This transmission may contain protected health information, which is transmitted pursuant to an authorization or as permitted by law. The information herein is confidential and intended only for use by the designated recipient who/which must maintain its confidentiality and security. If you are not the designated recipient, you are strictly prohibited from disclosing, copying, distributing, or taking action in reliance on the contents hereof. If you have received this transmission in error, please notify the sender immediately and arrange for the return or destruction of all of its contents. Unauthorized redisclosure of confidential health information is prohibited by state and federal law.
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Title | The form is titled "Prior Authorization Request Form" specifically for blood clotting disorder medications. |
| Contact Information | Submit the completed form via fax to 877-503-7231 or contact them by phone at 855-264-4964. |
| Patient Information Required | Vital patient details include the patient's name, date of birth, and address are mandatory. |
| Diagnosis Selection | The form requires the provider to indicate the patient’s specific diagnosis related to hemophilia or other bleeding disorders. |
| Supporting Documentation | Providers must attach relevant medical history or clinical statements that support the authorization request. |
| Medication Supply Method | The request asks providers to specify whether medication will be ordered through a specialty pharmacy or billed directly by the provider. |
| Confidentiality Notice | The form includes a warning regarding the confidentiality of protected health information and outlines the responsibilities of the recipient. |
Guidelines on Utilizing Healthnet Prior Authorization
Carefully filling out the Healthnet Prior Authorization form is essential for ensuring that your patient's medication requests are processed smoothly and efficiently. Each detail matters, especially when it comes to facilitating necessary treatments. Below are the steps you should follow to complete the form. Be sure to provide accurate and complete information to prevent any delays in the authorization process.
- Begin by entering the Patient Name in the designated field.
- Next, fill in the Prescriber Name.
- Input the Member/Subscriber Number.
- Provide the Fax number to which the form should be sent.
- Include the Phone number for contact.
- Enter the Date of Birth of the patient.
- List the Office Contact person for further communication.
- Input the Group Number.
- Include the NPI (National Provider Identifier) number.
- Document the State Lic ID for the prescriber.
- Fill in the Address, City, State, and ZIP code for the patient.
- Enter the Primary Phone number.
- If applicable, provide the Specialty/facility name.
- Specify the Drug Name and Strength as prescribed.
- Detail the Directions/SIG for administering the medication.
- Attach any pertinent medical history or information that supports the patient's case.
- Choosing between initial or continuing therapy, answer Q1. If it's continuing therapy, also include the start date.
- Indicate the patient's diagnosis in Q2 and check the relevant box.
- For Q3, provide any additional supporting clinical statements or notes regarding the patient's treatment.
- Answer Q4 by choosing how the medication will be supplied.
- If applicable to Q5, provide the necessary J-codes for Buy and Bill procedures.
- Sign and date the form where indicated for the prescriber’s signature.
After you have filled in all the required information, review the form once more to ensure accuracy. Once satisfied, fax the completed form to the designated fax number provided. This process is crucial in obtaining prompt approval for the necessary treatment your patient requires.
What You Should Know About This Form
What is the Healthnet Prior Authorization form?
The Healthnet Prior Authorization form is a request submitted by healthcare providers to gain approval for certain medications, specifically blood clotting disorder medications like FEIBA or NovoSeven. This form is necessary when prescribed treatments require review to ensure the patient meets the coverage criteria.
Who needs to fill out the Healthnet Prior Authorization form?
The form must be completed by the prescribing physician or healthcare provider. They need to provide detailed information about the patient’s condition, treatment plans, and relevant medical history to support the authorization request.
What information is required on the Prior Authorization form?
The form requires various details including the patient’s name, date of birth, member number, and the prescriber’s information. It also asks about the specific diagnosis, whether the request is for initial or continuing therapy, and any supporting clinical statements or medical history. Additionally, information about how the medication will be supplied must be provided.
What happens if I leave information blank on the form?
If any information is left blank or is illegible, it may delay the review process. Complete and clear responses ensure the healthcare provider can promptly assess the request and provide a faster decision regarding medication coverage.
How can the completed form be submitted?
The completed Healthnet Prior Authorization form should be faxed back to the designated number, which is 877-503-7231. It’s important to ensure the form is fully completed before submission to avoid any delays.
What should I do if my authorization request is denied?
If an authorization request is denied, the provider can appeal the decision. This typically involves reviewing the denial reason, gathering additional evidence or documentation, and resubmitting the request. Communication with Healthnet's customer service for clarification and guidance can also be beneficial in these situations.
Who can I contact for questions about the Prior Authorization process?
If there are any questions or uncertainties about the Prior Authorization process, healthcare providers can reach out to the Healthnet customer service number at 855-264-4964. They can provide guidance, answer questions, and assist with the authorization request steps.
Common mistakes
Completing the Healthnet Prior Authorization form requires attention to detail. One common mistake people make is leaving sections blank. Providing all requested information is crucial for a smooth review process. Missing details can delay the approval of necessary treatments, leading to negative consequences for patients.
Another frequent error involves providing illegible handwriting. Clear, readable printing is essential. If the information cannot be easily understood, it may cause further delays as the reviewer tries to interpret the details. This can be particularly impactful when it comes to essential information like patient names or medication details.
Not specifying the patient's diagnosis is also a mistake that can hinder the authorization process. The form requires an indication of the diagnosis, but sometimes individuals fail to check the appropriate box or provide sufficient details. Accurate information about the patient's condition helps in assessing the necessity of the requested treatment.
Additionally, failing to attach relevant supporting clinical statements can be detrimental. The form asks for pertinent medical history that could support the authorization request. Omitting this information may lead to a denial of coverage since the reviewer lacks the context needed to make an informed decision.
Finally, neglecting to ensure that all required signatures and dates are included can lead to complications. The prescriber must sign and date the form, confirming their agreement with the request. Missing these items can result in the form being returned for correction, further delaying the process.
Documents used along the form
When navigating the healthcare system, especially concerning medications that require prior authorization, a few other important forms and documents often accompany the Healthnet Prior Authorization form. Understanding these documents can streamline the approval process and enhance communication between providers and insurers.
- Clinical Notes or Records: These documents provide detailed information about the patient's medical history, diagnosis, treatment plans, and any previous therapies. They support the authorization request by demonstrating medical necessity and justifying the prescribed treatment.
- Medication Administration Record (MAR): This document tracks all medications administered to the patient. It includes dates, times, dosages, and administration routes, which can help confirm the history of treatment and adherence to prescribed therapies.
- Insurance Eligibility Verification: This form confirms the patient’s insurance coverage and benefits. It's essential to ensure that the requested medication is covered under the patient's current health plan before submitting a prior authorization request.
- Referral Form: In certain cases, a referral from a primary care physician to a specialist is necessary. This document outlines the necessity for the patient to see a specialist, which may be relevant to the prior authorization request for specific treatments or medications.
- Pertinent Lab Results: Recent lab tests or diagnostic imaging results can substantiate a patient's condition. Including these results with the prior authorization request can strengthen the case for approval by showing current health status.
- Formulary Coverage Criteria Documentation: This provides details about the specific medication's coverage guidelines as outlined by the insurance company. It can help in understanding alternative therapies and their coverage status, ensuring that the best options are considered.
- Appeal Letter (if applicable): If a prior authorization request is denied, an appeal letter can explain why the medication is essential. This letter should detail the patient's medical history and treatment needs and reference any relevant clinical guidelines.
Having these forms ready can significantly aid both patients and providers in getting the necessary approvals for medications. By ensuring that all relevant documents are included, the process can be more efficient, minimizing delays and improving patient care outcomes.
Similar forms
- Medicare Prior Authorization Forms: These forms are similar in that they require detailed patient and treatment information for approval of certain medical services or medications. Both emphasize the importance of complete and clear information to avoid delays.
- Insurance Pre-Certification Requests: Like the Healthnet form, these documents require a diagnosis and supporting clinical statements to justify the need for services before they are rendered.
- Medication Prior Authorization Forms: These forms specifically address requests for prescription medications and often require similar patient demographics and treatment history to process the authorization.
- Surgical Authorization Forms: Similar to the Healthnet form, these documents request details about the patient's health status and the planned procedure, requiring approval from the insurance provider in advance.
- Durable Medical Equipment (DME) Authorization Requests: These documents collect similar information on the patient’s needs and medical justification for requesting specific equipment or supplies.
- Behavioral Health Service Authorization Requests: Just like the Healthnet form, this type requires personal information about the patient and an explanation of the medical necessity for therapy or interventions.
- Home Health Care Service Requests: These forms require information about the patient’s medical condition and proposed care plan, ensuring the coverage of home health services is warranted.
Dos and Don'ts
When filling out the Healthnet Prior Authorization form, there are important steps to take to ensure a smooth process for medication approval. Here’s a list of things you should and shouldn't do.
- Do: Ensure all patient and prescriber information is filled out completely. Missing details can lead to delays.
- Do: Attach any relevant medical history or documents that support the authorization request. This can strengthen your case.
- Do: Double-check your answers, especially the details regarding the patient's diagnosis and medication needs.
- Do: Use clear and legible handwriting if you’re filling out the form manually, or type the information if possible.
- Don't: Leave any questions blank. If an item doesn’t apply, indicate it accordingly.
- Don't: Forget to sign and date the form. An unsigned form will not be processed.
- Don't: Submit the form without confirming the correct fax number. Incorrect submissions can cause unnecessary delays.
- Don't: Include unnecessary personal details that are not relevant to the medication request. Stick to the needed information.
Misconceptions
Here are five common misconceptions about the Healthnet Prior Authorization form:
- Myth 1: Prior authorization is always required for all medications. Many people think that every medication requires prior authorization. However, only specific drugs, such as certain blood clotting disorder medications, need this approval.
- Myth 2: Filling out the form is a simple process without consequences. While the form may seem straightforward, incomplete or illegible information can lead to delays. It is crucial to fill it out carefully.
- Myth 3: Doctors have no role in the authorization process. This is not true. The prescribing physician’s input is essential. They need to provide supporting information for the request to be considered.
- Myth 4: If the request is denied, there's no way to appeal. Many people believe that a denial is final. In fact, a denial can often be challenged through an appeal process to further evaluate the case.
- Myth 5: All prior authorization requests are handled in the same timeframe. The response time can vary. Urgent requests may be expedited, while standard requests might take longer, depending on specific cases and documentation.
Key takeaways
Filling out the Healthnet Prior Authorization form accurately is crucial for a smooth approval process. Here are some key takeaways to guide you:
- Complete Information: Ensure all fields are filled out legibly. Missing or unclear information can delay the review process significantly.
- Diagnosis Details: Clearly indicate the patient's diagnosis from the provided options. This helps in assessing the urgency and need for the medication.
- Supporting Documents: Attach any relevant medical history or documentation that can support your request. This includes treatment failures, lab results, or clinic notes.
- Initial vs. Continuing Therapy: Specify if the request is for initial or continuing therapy. If it is continuing, include the treatment start date for context.
- Pharmacy Options: Decide how the medication will be supplied and check the appropriate option. This makes processing your authorization easier.
- Confidentiality Matters: Remember that the information on this form is confidential. Ensure it is shared only with authorized recipients to protect patient privacy.
- Signature Requirement: Don't forget to sign the form and include the date. An unsigned form will not be processed.
By keeping these points in mind, you can help ensure that the authorization process runs smoothly and efficiently. Your diligence can lead to timely access to necessary treatments for your patients.
Browse Other Templates
The Meeting App - Participants should be aware that AA does not accept liability for the use of this form.
Saco River Education - Access to the course is valid for six months, providing ample time for students to complete their studies.