Fill Out Your History And Physical Form
The History and Physical (H&P) form plays a crucial role in patient care, particularly in hospital settings. It serves as a comprehensive tool for healthcare providers to gather essential information regarding a patient's medical history and current health status. The form typically starts with patient identification details, including the patient's name, age, and admission date, as well as the reason for the visit, commonly referred to as the chief complaint. Allergies and current medications are also noted, setting the stage for contextual understanding of the patient's health. Following this, the detailed history of present illness provides insights into the ongoing medical issue, while past medical and surgical history allows clinicians to understand prior health events that could impact current treatment. In addition to this foundational data, the form includes sections on social and family histories, which can highlight environmental factors and hereditary conditions. The comprehensive review of systems (ROS) further aids in identifying any additional symptoms that may not have been previously disclosed. These components culminate in the physical exam and assessment sections, allowing healthcare providers to formulate an informed treatment plan tailored to the patient's unique needs. Overall, the H&P form not only facilitates effective diagnosis and management but also encourages collaboration within the healthcare team, ensuring all providers have access to vital patient information.
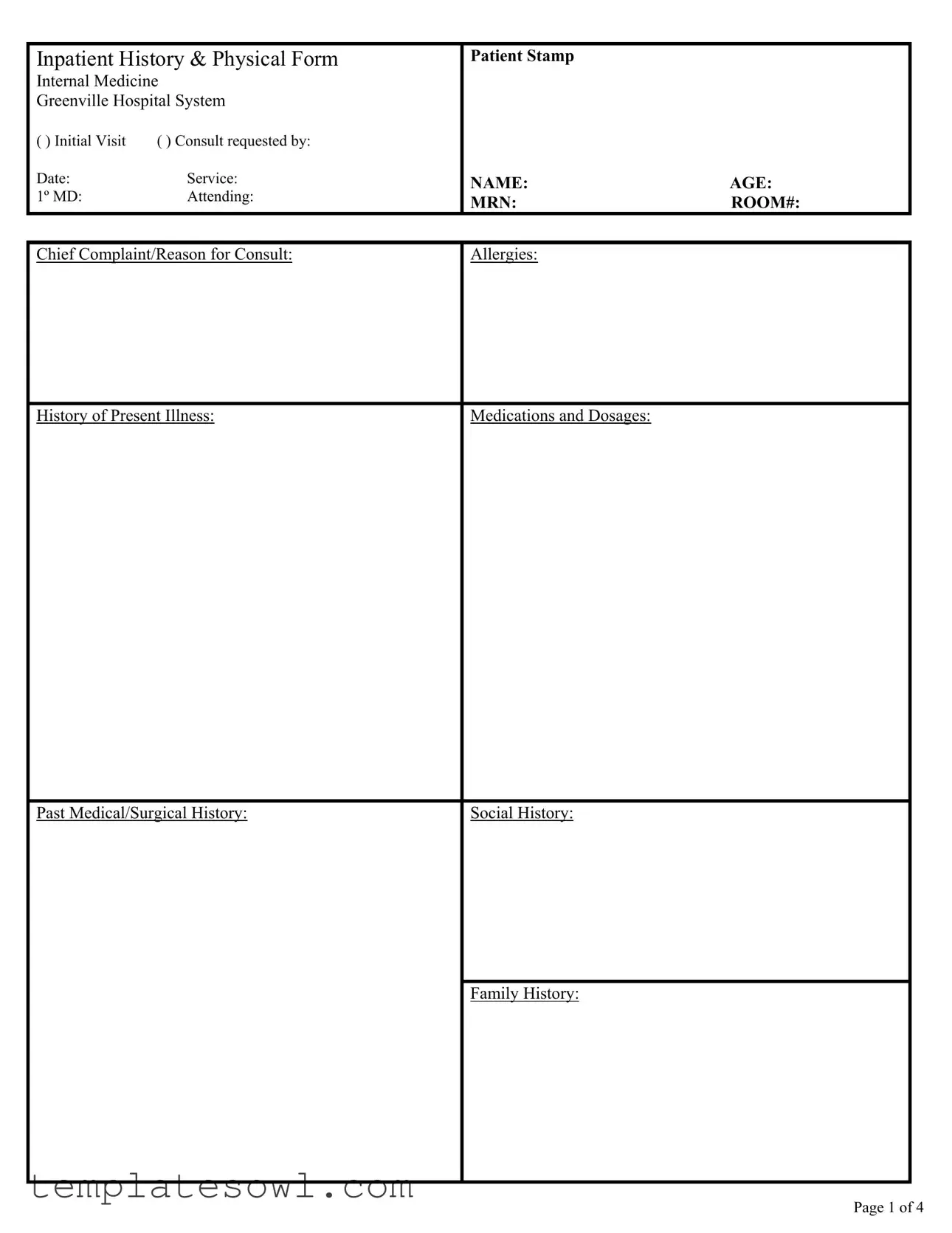
History And Physical Example
Inpatient History & Physical Form |
Patient Stamp |
|
||
Internal Medicine |
|
|
||
Greenville Hospital System |
|
|
||
( ) Initial Visit |
( ) Consult requested by: |
|
|
|
Date: |
Service: |
NAME: |
AGE: |
|
1º MD: |
Attending: |
|||
MRN: |
ROOM#: |
|||
|
|
|||
Chief Complaint/Reason for Consult:
Allergies:
History of Present Illness:
Medications and Dosages:
Past Medical/Surgical History:
Social History:
Family History:
Page 1 of 4
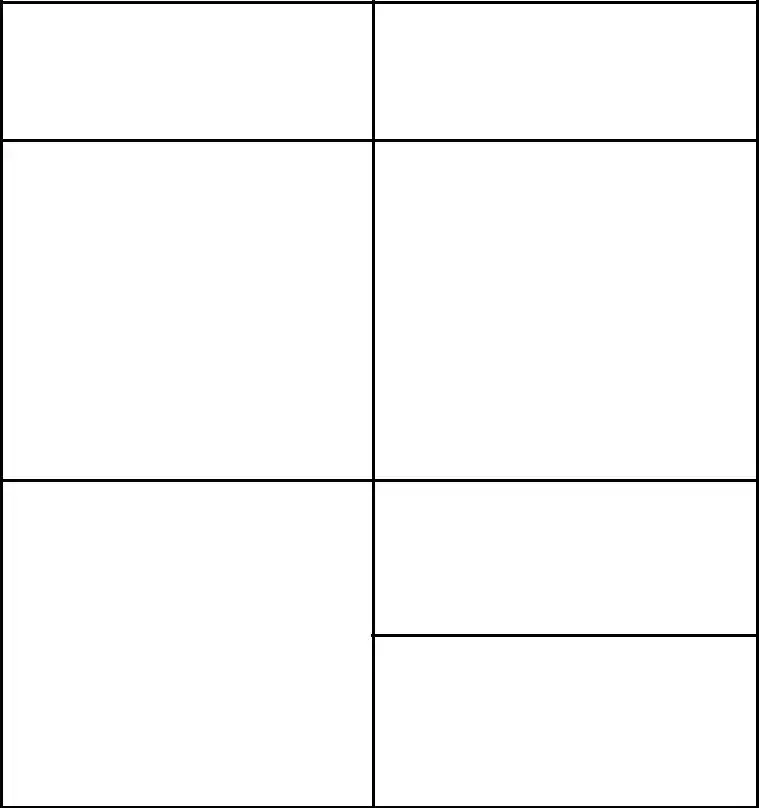
Comprehensive Review of Systems
ROS NOT OBTAINABLE BECAUSE
Patient Stamp
Constitutional: |
|
Genitourinary: |
|
|
YES NO |
DESCRIBE |
YES NO |
DESCRIBE |
|
Fever, sweats or chills |
|
Dysuria, frequency or urgency |
||
|
Menstrual irregularities |
|
||
Fatigue, anorexia, weight loss or gain |
|
|||
LMP ___________________ |
||||
Weakness |
|
|||
|
Frequent UTI’s |
|
||
|
|
|
||
|
|
Pain/Hematuria |
|
|
Skin: |
|
Musculoskelatal: |
Rashes, no skin breakdown |
|
Muscle aches, arthralgias or arthritis |
|
|
|
|
|
Neurologic: |
|
|
Mental status changes |
Head: |
|
|
|
Headaches |
|
Headache |
|
|
|
Dizziness |
|
Visual changes |
|
|
|
Weakness or numbness |
|
Earache, sinus problems, sore throat |
|
|
|
Seizures |
|
Cough, snoring or mouth ulcers |
|
|
|
Ataxia |
|
|
|
|
|
|
Hematopoietic: |
|
|
Lymphadenopathy |
|
|
Bleeding tendencies |
|
|
|
Cardiovascular: |
|
Psychiatric: |
Chest pain or palpitations |
|
History of anxiety or depression |
Syncope |
|
Hallucinations/Delusions |
Edema |
|
|
|
|
|
|
|
Endocrine: |
|
|
History of diabetes |
|
|
History of thyroid problems |
|
|
|
|
|
Other Symptoms: |
Respiratory: |
|
|
Shortness of breath |
|
|
Cough or sputum production |
|
|
Dyspnea on exertion orthopnea |
|
|
Pleuritic chest pain |
|
|
|
|
|
Gastrointestinal: |
|
|
Heartburn, dysphagia |
|
|
Nausea or vomiting |
|
|
Diarrhea or constipation |
|
|
Melena or BRBPR |
|
|
Hematemesis |
|
|
Abdominal pain |
|
|
Page 2 of 4
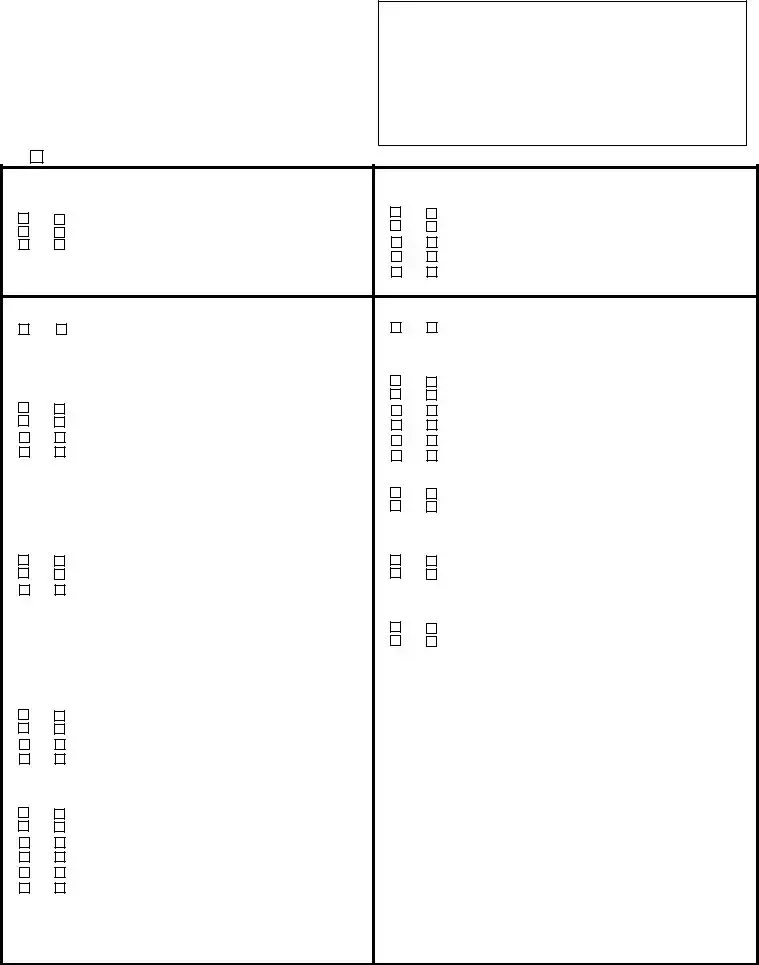
Patient Stamp
Physical Exam |
|
|
Labs and Studies |
||
Vitals: |
|
|
|
CBC: |
|
Wt: |
Temp: |
BP: |
P: |
|
|
HT: |
Resp: |
Sat: |
|
|
|
Constitutional: |
nl general appearance |
|
|
|
|
|
|
|
|
|
|
Head: |
|
|
BMP: |
|
|
|
|
PERRLA |
|
|
|
|
|
EOMI |
|
|
|
|
|
nl sclera |
|
|
|
|
|
Vision |
|
|
|
Ears, Nose, Mouth & Throat: |
|
CXR: |
|
||
|
|
nl inspection of nasal |
|
|
|
|
|
mucosa, septum, turbinates, |
|
|
|
|
|
teeth, gums & oropharynx |
|
|
|
|
|
nl ear canal and T |
|
|
|
|
|
|
|
|
|
Neck: |
|
nl neck appearance & |
|
EKG: |
|
|
|
jugular veins |
|
|
|
|
|
Thyroid not palpable, |
|
|
|
|
|
|
|
|
|
Lymph Nodes |
|
nl neck, supraclavicular |
|
|
|
|
|
or axillary adenopathy |
|
|
|
|
|
|
|
|
|
Skin/Extremities: |
Rashes, lesions or ulcers |
|
|
|
|
|
|
Digits & nails |
|
|
|
|
|
Edema |
|
|
|
Breast Evaluation: |
No skin changes |
|
|
|
|
|
|
No nipple discharge |
|
|
|
|
|
No lumps/masses |
|
|
|
|
|
Fibrocystic changes |
|
|
|
Respiratory: |
|
Chest symmetric, nl chest |
|
|
|
|
|
Expansion & respiratory effort |
|
|
|
|
|
nl auscultation |
|
|
|
|
|
nl chest percussion & |
|
|
|
|
|
palpation |
|
|
|
Cardiovascular: |
Reg rhythm |
|
|
|
|
|
|
No murmur, gallop or rub |
|
|
|
|
|
Periph vasc no by ovserv & |
|
|
|
|
|
palpation |
|
|
|
Gastrointestinal: |
No tenderness or masses |
|
|
|
|
|
|
Liver & spleen not felt |
|
|
|
|
|
nl bowel sounds |
|
|
|
|
|
Heme negative stool |
|
|
|
Musculoskeletal: |
nl muscle strength, movement & |
Neurologic: |
Alert and oriented |
||
|
|
tone, no focal atrophy |
|
|
nl reflexes upper and lower |
|
|
nl gait & station |
|
|
extremities |
|
|
|
|
|
Cranial nerves intact |
no pelvic exam |
|
Psychiatric: |
|
||
|
|
nl testes |
|
|
nl mood/affect |
Page 3of 4
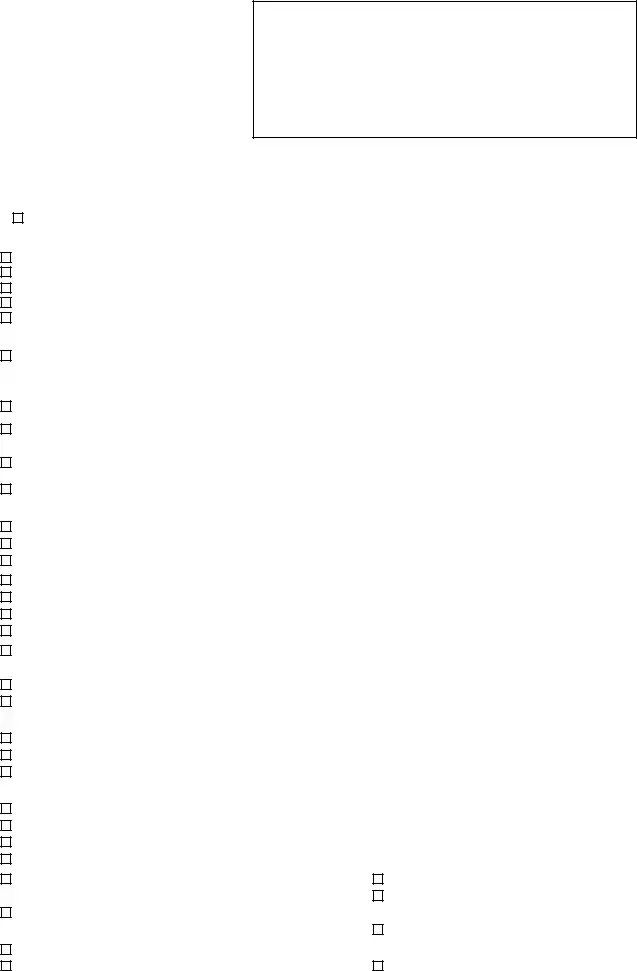
Patient Stamp
Assessment:
Plan:
Attending HPI:
Attending PE:
Attending Assessment and Plan:
Resident signature: |
MD |
PGY1, PGY2, PGY3 Date: |
Pager: |
/1439 |
|
Resident name printed: |
Dictated by: |
Intern Pager: |
/1872 |
||
Attending signature: |
|
Date: |
|
. |
|
Attending: Ansari Atkisson Bowers Bruch Call Chang Cochrane Curran Ferraro Fuller Gilroy Hayes Kelly Knight Latham McCraw McFarland Meyer
Page 4 of 4
Form Characteristics
| Fact Name | Details |
|---|---|
| What is a History and Physical Form? | This document compiles a patient's medical history and the results of a physical examination. |
| Purpose of the Form | It aids healthcare providers in making informed medical decisions for patient care. |
| Common Usage | This form is typically used in inpatient settings for initial visits and consultations. |
| Legal Requirement | Many states require a History and Physical Form to be completed before surgery, dictated by state healthcare laws. |
| Components Include | The form includes sections for patient history, current medications, allergies, and physical examination findings. |
| Governing Law Example | In California, the Health and Safety Code specifies requirements for medical records and documentation. |
| Confidentiality | Like all medical records, the History and Physical Form is protected under HIPAA regulations. |
| Who Completes the Form? | A licensed healthcare provider, such as a physician, typically completes the form. |
| Integration with Electronic Records | Many healthcare facilities now integrate this form into electronic health record systems for easier access and storage. |
| Review Process | The form undergoes review by attending physicians for accuracy and completeness, ensuring high-quality patient care. |
Guidelines on Utilizing History And Physical
Filling out the History and Physical form is an essential step in ensuring comprehensive patient care. This document gathers vital information that will aid healthcare professionals in diagnosing and treating patients effectively. The following steps will guide you through the process of completing this form accurately.
- Begin with Patient Information: Enter the patient stamp located at the top of the form. Fill in the patient’s name, age, date, and medical record number (MRN). Include the room number if applicable.
- Consult Request: Indicate whether this is an initial visit or a consult. Record the name of the physician requesting the consult and the service they provide.
- Chief Complaint: Clearly state the chief complaint or the reason for the patient’s consultation. This should summarize the primary issue.
- Allergies: List any known allergies the patient may have. Be specific about reactions.
- History of Present Illness: Provide detailed information about the current health issue. Include onset, duration, and any pertinent information related to the complaint.
- Medications: Document all medications the patient is currently taking, along with their dosages.
- Past Medical/Surgical History: Detail any significant past medical or surgical issues the patient has experienced.
- Social History: Note lifestyle factors that could affect the patient’s health, such as smoking, alcohol use, and exercise habits.
- Family History: Record any relevant family medical history that could impact the patient’s condition or treatment.
Next, move on to the Comprehensive Review of Systems (ROS), where various body systems will be evaluated. This section includes checkboxes for observations and descriptions that help pinpoint any additional concerns or conditions that need addressing.
- Constitutional: Check relevant boxes and describe any symptoms such as fever, fatigue, or weight changes.
- Dermatological: Note any skin-related issues, rashes, or lesions.
- Neurologic and Psych: Document any neurological symptoms and mental health concerns.
- Cardiovascular and Respiratory: Indicate any heart or lung-related issues, including chest pain or difficulty breathing.
- Gastrointestinal: Record any GI symptoms like heartburn, nausea, or abdominal pain.
- Musculoskeletal: Note any muscle and joint pain or other musculoskeletal issues.
After completing the review of systems, you will proceed with the physical exam section, performing assessments as outlined in the form, and documenting results.
- Vitals: Record the patient’s weight, temperature, blood pressure, pulse, respiratory rate, and oxygen saturation levels.
- Physical Examination: Complete evaluations for each body system, noting any abnormalities or concerns detected during the exam.
Once all sections are filled out, it's crucial to provide a comprehensive assessment and plan of care. This ensures the attending physician can quickly grasp the patient’s situation and formulate subsequent treatment strategies.
- Assessment: Summarize your findings and concerns from the history and physical examination.
- Plan: Outline the next steps for diagnosis and treatment, including any tests or referrals needed.
- Signatures: Ensure both the resident and attending physician sign and date the form before submission.
With each of these steps, you're making a significant contribution to the patient's healthcare journey. Detailed and accurate documentation can greatly enhance the quality of care they receive.
What You Should Know About This Form
What is the purpose of the History and Physical (H&P) form?
The History and Physical form serves as a comprehensive document that provides medical professionals with essential information about a patient's medical history and current health status. This form collects a range of details, including the patient's chief complaint, medical history, social factors, and a physical examination. By aggregating this information, healthcare providers can make informed decisions regarding diagnoses, treatment plans, and ongoing care.
Who is responsible for completing the H&P form?
What sections are included in the H&P form?
The H&P form encompasses several key sections that cover various aspects of the patient's health. Initially, it captures identification information such as the patient's name, age, and medical record number (MRN). The document then details the chief complaint, allergies, medications, and both past medical and surgical histories. In addition, the form includes a comprehensive review of systems (ROS) and a physical examination section, which collectively offer a thorough overview of the patient's current health.
How is the Review of Systems (ROS) conducted?
The Review of Systems is a systematic inquiry where various body systems are evaluated for symptoms. Healthcare providers typically ask specific questions about common health issues related to each system, such as cardiovascular, respiratory, gastrointestinal, and neurological concerns. This section can either confirm the presence of symptoms or indicate that they are not present, helping to identify potential areas of concern for further investigation.
Why is the social and family history section important?
The social and family history is crucial in understanding factors that might influence a patient’s health. Social history may include lifestyle factors such as tobacco use, alcohol consumption, and exercise, while family history looks at genetic predispositions to certain conditions. These aspects can significantly affect the management of a patient's care and inform preventative measures.
What role does the assessment and plan section play?
The assessment and plan section summarizes the healthcare provider's evaluation of the patient's condition based on the history and physical examination findings. Here, the provider outlines a strategy for treatment, which may include further tests, referrals, or specific interventions. It is a critical component that guides the patient's ongoing care and outlines the next steps for their health management.
How often should the H&P form be updated?
The H&P form should be updated during significant changes in a patient's condition or upon admission to a new healthcare facility. For outpatients, it is generally updated at each visit, particularly for new complaints or changes in health status. Regular updates ensure that the care team has the most current and relevant information to support patient care effectively.
Common mistakes
When completing the History and Physical form, individuals often overlook critical components that can impact patient care. One common mistake is failing to provide complete and accurate information about the **chief complaint**. This section should clearly express the primary reason for the patient visit. Without this clarity, medical professionals may struggle to diagnose effectively or provide appropriate care.
Another frequent error is neglecting to update the **medications and dosages**. Patients sometimes forget to mention any over-the-counter medications or supplements. Omitting these can lead to dangerous drug interactions or overlooked vital information regarding the patient’s health. Completeness in this section is key for safe medical practice.
Additionally, many individuals skip detailing their **past medical and surgical history** thoroughly. This section should not just list prior procedures but also include dates and any complications. A lack of detail here may result in healthcare providers missing critical factors that could affect treatment decisions or overall patient management.
Finally, mistakes can occur in the **family history** section. Patients might either underestimate its importance or fail to recall relevant details about family health issues. This information can be crucial for identifying hereditary conditions or risks that may influence the patient’s current health. Comprehensive family history aids in preventive care and personalized treatment planning.
Documents used along the form
The History and Physical (H&P) form is essential in documenting a patient's clinical information at the time of an initial visit or consult. Several other forms and documents are commonly utilized alongside the H&P to provide a more comprehensive view of the patient's medical status. Below are descriptions of six such forms and documents.
- Consent Form: This document secures the patient's permission for treatment, procedures, or participation in research. It ensures that patients are informed of their rights and potential risks involved in their medical care.
- Medication Reconciliation Form: Used to compile an accurate list of the patient’s current medications. This form helps prevent medication errors, ensuring that all prescriptions are accounted for and appropriately managed.
- Progress Notes: These notes track a patient's ongoing treatment and response to therapy. They serve to communicate changes in the patient's condition, guiding clinical decision-making and care plans.
- Discharge Summary: Created at the end of a patient’s stay, this document summarizes the care provided, important findings, and recommendations for follow-up care. It is crucial for continuity of care as the patient transitions to outpatient settings.
- Lab and Study Orders: These forms request specific laboratory tests or imaging studies. Properly filled-out orders ensure that necessary diagnostic tests are conducted in a timely manner, aiding in the care process.
- Referral Form: Used when a patient needs to see a specialist. This form communicates pertinent medical history and reasons for the referral, ensuring specialists have the information they need to provide appropriate care.
Collectively, these documents enhance patient care, ensuring that medical staff have access to all relevant information needed for informed decision-making and effective treatment. Understanding and utilizing these forms improves the overall healthcare experience for patients and providers alike.
Similar forms
The History and Physical (H&P) form serves as a foundational document in patient care. It encompasses critical patient information, including medical history and examination findings. Several other documents share similarities with the H&P form, primarily in their purpose of documenting patient health information. These documents are outlined below:
- Consultation Report: This document provides detailed information about a patient's condition from the perspective of a specialist. Like the H&P, it includes a review of the patient's medical history and findings from the examination.
- Progress Notes: Progress notes track a patient's ongoing care and response to treatment. They summarize previous assessments and incorporate updates similar to how the H&P gathers comprehensive patient information.
- Discharge Summary: This outlines the patient's condition at the time of discharge, highlighting the treatment received and any follow-up plans. It includes a synthesis of medical history akin to that found in the H&P.
- Emergency Room Report: This document details the care provided during an emergency visit, including the patient's history and physical examination. It serves a similar role in capturing acute medical information.
- Preoperative Assessment: Conducted before surgery, this document includes the patient's medical history and physical examination results to evaluate surgical risk, paralleling the H&P's comprehensive nature.
- Physical Therapy Initial Evaluation: This captures the patient’s medical history and physical examination in the context of rehabilitation, sharing the H&P's focus on physical assessment.
- Radiology Report: While primarily focused on imaging findings, these reports often reference relevant medical history and patient symptoms, making them similar in content to the H&P.
- Medication Reconciliation Form: This document consolidates current medications, allergies, and history, aligning with the H&P's components of medication and allergy documentation.
- Specialist Referral Form: This provides information necessary for a referred provider, often incorporating patient history and relevant examination findings, akin to the H&P structure.
- Family History Document: This focuses specifically on the medical histories of family members, an aspect also present in the H&P, recognizing the importance of family medical background in patient assessment.
Each of these documents serves distinct purposes within the healthcare system but maintains a shared goal of comprehensive patient care and monitoring.
Dos and Don'ts
When completing the History and Physical form, it is important to follow certain guidelines. Here are ten things to keep in mind:
- DO ensure all sections are completed fully, providing necessary details for each item.
- DON'T leave any blank fields unless instructed otherwise. Incomplete forms can lead to misunderstanding.
- DO list allergies clearly along with specific reactions to each allergen.
- DON'T generalize symptoms. Be specific about symptoms and their durations.
- DO include a comprehensive history of medications, including dosages and frequency.
- DON'T forget to mention any past medical or surgical history relevant to the current situation.
- DO write legibly or type to avoid any misinterpretation of the information provided.
- DON'T use abbreviations or slang that might confuse the healthcare providers.
- DO check for accuracy before submitting the form to prevent errors in the patient’s records.
- DON'T submit the form without ensuring it is signed by the appropriate healthcare professional.
Following these guidelines will enhance the quality of care received by the patient and ensure clarity in communication among healthcare providers.
Misconceptions
Misconceptions about the History and Physical (H&P) form can lead to misunderstandings about its purpose and use in medical settings. Here are some of the most common myths:
- The H&P form is only for new patients. Many believe that this form is exclusively for initial visits. However, it is equally important for follow-up visits and consultations. Each time a patient is seen, an updated H&P can provide essential context for ongoing care.
- Completing the H&P is just a formality. Some people think that filling out the H&P is a routine task without much significance. In reality, it is a critical document that informs the healthcare provider’s diagnosis and treatment plan.
- All components of the H&P must be filled out every time. There is a common belief that every section of the H&P needs to be completed for every visit. While thoroughness is important, not all sections will necessarily be relevant at every appointment. Providers should focus on what is clinically pertinent for that visit.
- Any healthcare professional can complete the H&P. It is a misconception that any member of the healthcare team can fill out this form. Only qualified professionals, such as physicians or specifically trained medical staff, are authorized to complete and sign the H&P.
- Patients should never see the H&P form. Some patients may think they should never interact with this document. However, providing transparency can enhance the patient-provider relationship. Patients should feel encouraged to review and discuss the contents of their H&P.
- The H&P form is only about physical health. There is a belief that the H&P focuses solely on physical conditions. In truth, it encompasses a comprehensive view that includes mental, emotional, and social health, thus offering a holistic assessment of patient well-being.
- The H&P is irrelevant after discharge. After leaving a hospital or clinic, some individuals assume that the H&P becomes outdated. Yet, this document can be vital for future healthcare providers, especially in emergency situations. It should be accessible for reference as part of the patient's medical history.
Understanding these misconceptions is essential for both patients and healthcare providers. By clarifying the role of the H&P form, we can ensure better communication and care.
Key takeaways
- Accuracy is crucial. Provide precise information regarding the patient's medical history to ensure effective diagnosis and treatment.
- Comprehensive documentation. Include all relevant details, such as allergies and medications, as this can impact care decisions.
- Prioritize the chief complaint. Clearly state the patient's primary concern, as it guides the focus of the history and physical examination.
- Use clear language. Avoid medical jargon when filling out the form to ensure all healthcare providers can understand the information.
- Verify past medical history. A thorough review of the patient's past surgeries and medical conditions enhances clinical understanding.
- Incorporate family and social history. These sections provide valuable context that can influence the patient's health risks.
- Conduct a detailed review of systems. Address all organ systems to identify any overlooked health concerns.
- Finalize with a well-structured assessment and plan. The conclusions reached should reflect the information documented, guiding future care directions.
Browse Other Templates
Big R Jobs - All answers should be truthful to avoid consequences.
To Take a Case to a Higher Court - Verification can be done through surveys and affidavits to confirm compliance.
Employee Self Evaluation Form - Assess if you have time for activities you enjoy.