Fill Out Your Home Health Audit Form
The Home Health Audit form plays a crucial role in ensuring that home health care services meet established standards. It is designed to facilitate the review of various aspects of patient care and administrative procedures. Key areas include patient admission documentation, such as the completion of referral sheets and physician orders, ensuring timely initiation of care, and verifying face-to-face encounter requirements. It evaluates whether all medical records support proper diagnosis coding and medication management, including the assessment of any potential interactions. Furthermore, it checks if patient agreements, consent forms, and emergency preparedness plans are complete. The audit form requires verification of plan of care components, including regular progress assessments and supervision of caregivers. It emphasizes maintaining accurate clinical notes and documentation, which are vital for compliance and quality assurance. Ultimately, this comprehensive checklist acts as a tool for improving patient outcomes and maintaining regulatory compliance within home health care settings.
Home Health Audit Example
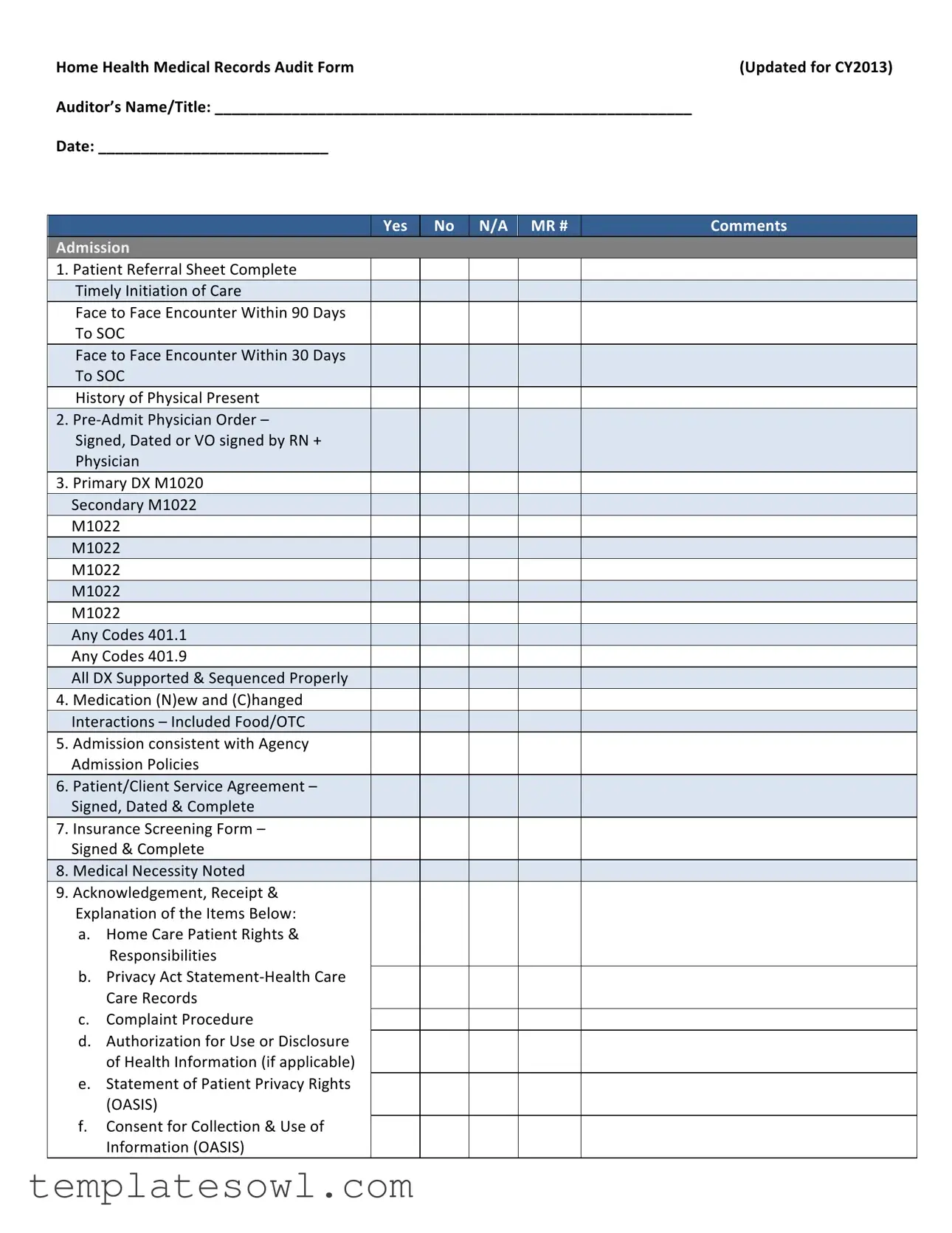
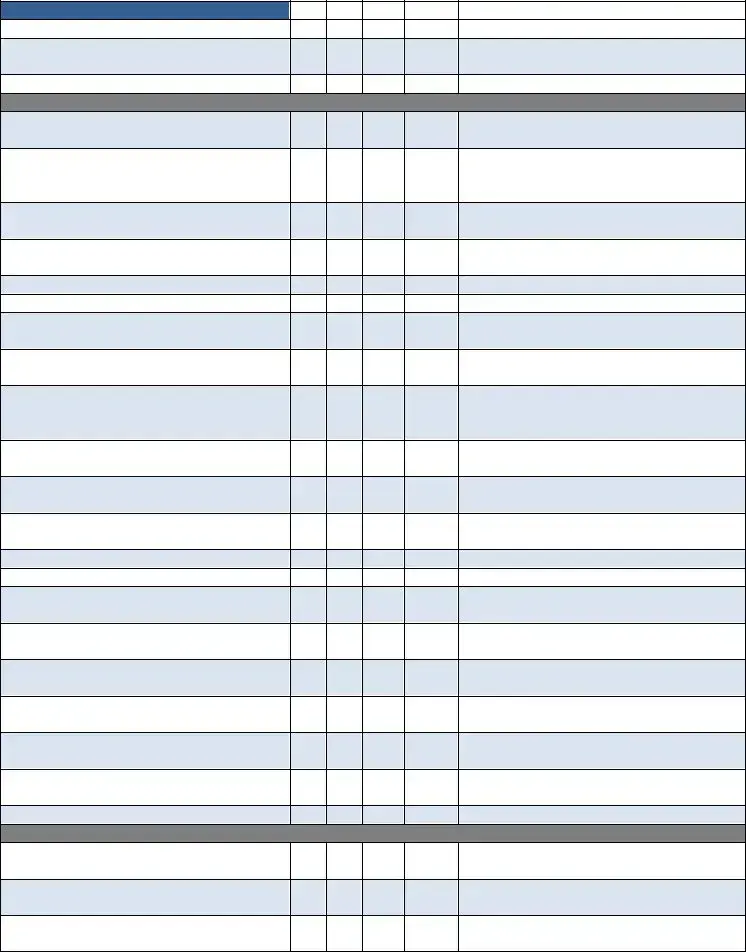
Home Health Medical Records Audit Form |
(Updated for CY2013) |
Auditor’s Name/Title: ________________________________________________________ |
|
Date: ___________________________ |
|
Yes
No
N/A MR #
Comments
Admission
1.Patient Referral Sheet Complete Timely Initiation of Care
Face to Face Encounter Within 90 Days To SOC
Face to Face Encounter Within 30 Days To SOC
History of Physical Present
2.Pre‐Admit Physician Order –
Signed, Dated or VO signed by RN + Physician
3.Primary DX M1020 Secondary M1022 M1022
M1022
M1022
M1022
M1022
Any Codes 401.1 Any Codes 401.9
All DX Supported & Sequenced Properly
4.Medication (N)ew and (C)hanged Interactions – Included Food/OTC
5.Admission consistent with Agency Admission Policies
6.Patient/Client Service Agreement – Signed, Dated & Complete
7.Insurance Screening Form – Signed & Complete
8.Medical Necessity Noted
9.Acknowledgement, Receipt & Explanation of the Items Below:
a.Home Care Patient Rights & Responsibilities
b.Privacy Act Statement‐Health Care Care Records
c.Complaint Procedure
d.Authorization for Use or Disclosure of Health Information (if applicable)
e.Statement of Patient Privacy Rights (OASIS)
f.Consent for Collection & Use of Information (OASIS)
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
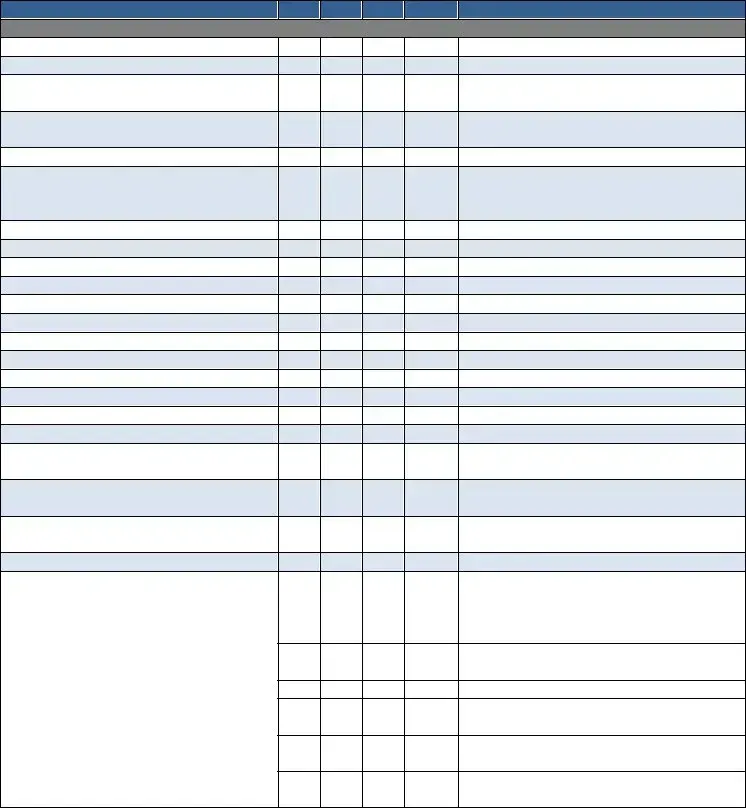
g.Emergency Preparedness Plan/Safety Instructions
h.Advance Directives & HHABN
10. Complete Post Evaluation –
D/C Summary Report by RN/PT/OT/ST on:
a. Start of Care
b. Resumption of Care
c. Recertification
Plan of Care 485
11.Plan of Care Signed & Dated by Physician Within 30 Working Days or State Specific days‐ ________
12.Diagnoses Consistent with Care Ordered
13.Orders Current
14. Focus of Care Substantiated
15.Daily Skilled Nurse Visit Frequencies with Indication of End Point
16. Measurable Goals for Each Discipline
17. Tinetti or TUG Completed at SOC
18. Recertification Plan of Care Signed &
Dated Within 30 Days or State Required
Time
19.BiD Insulin Visits Documented with Vision, Musculoskeletal Need, Not Willing/Capable Caregiver. MSW Every Episode
20. Skilled Nurse Consult
Medication Profile Sheet
21.Medication Profile Consistent with the 4 485
22. Medication Profile Updated at
Recertification, ROC, SCIC, Initialed &
Dated
23.Medication Profile Complete with Pharmacy Information
Physician Orders/Change Verbal Orders
24. Change/Verbal Orders Include Disciplines, Goals, Frequencies, Reason for Change, Additional Supplies as Appropriate
25.Change Orders Signed & Dated by Physician Within 30 Working Days
OASIS Assessment Form
26. Complete, Signed & Dated by:
___________________________
27.M2200 Answer Meets the Threshold for a Medicare High Case Mix Group
28. M1020 & M1022 Diagnoses & ICD‐9 are Consistent with the Plan of Care
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
29.All OASIS Assessments Were Exported Within 30 Days
30. OASIS Recertifications Were Done
Within 5 Days of the End of the Episode
31.All OASIS Were Reviewed for Consistency in Coordination with the Discipline Who Completed the Form
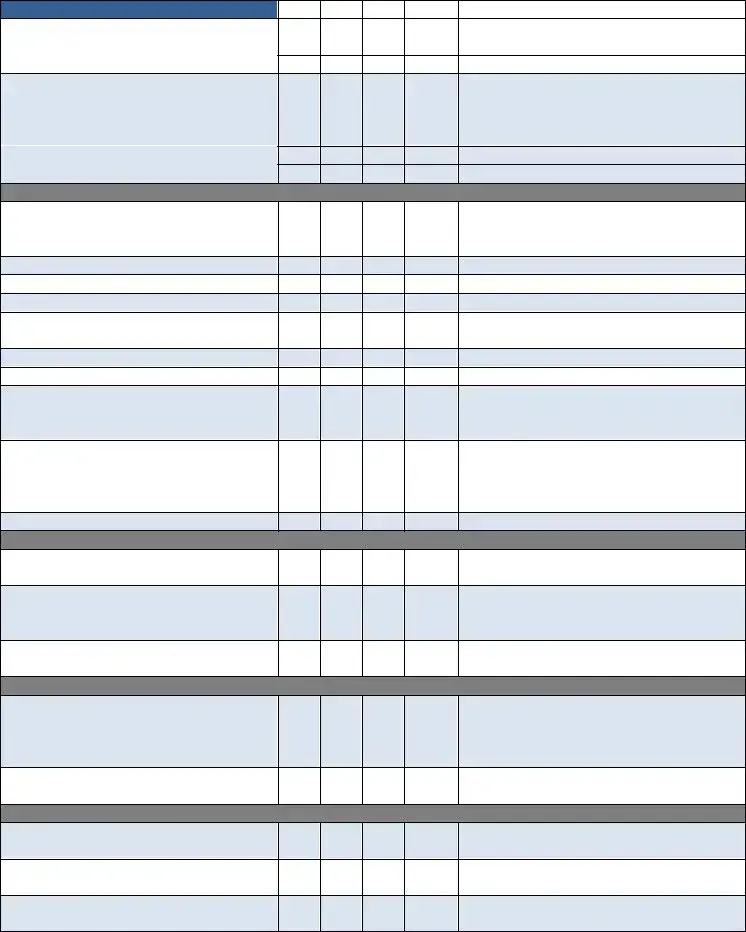
Skilled Nursing Clinical Notes
32. Visit Frequencies & Duration are Consistent with Physician Orders
33.Orders Written for Visit Frequencies/ Treatment Change
34. Homebound Status Supported on Each Visit Note
35.Measurable Goals for Each Discipline with Specific Time Frames
36. Frequency of Visits Appropriate for Patient’s Needs & Interventions Provided
37. Appropriate Missed Visit (MV) Notes
38. Skilled Care Evident on Each Note
39. Evidence of Coordination of Care
40. Every Note Signed & Dated
41. Follows the Plan of Care (485)
42. Weekly Wound Reports are Completed
43. Missed Visit Reports are Completed
44. Pain Assessment Done Every Visit with Intervention (If Applicable)
45.Abnormal Vital Signs Reported to Physician & Case Managers
46. Evidence of Interventions with Abnormal Parameters/Findings
47.Skilled Nurse Discharge Summary/ Instructions Completed
48. LVN Supervisory Visit Every 30 Days by Registered Nurse
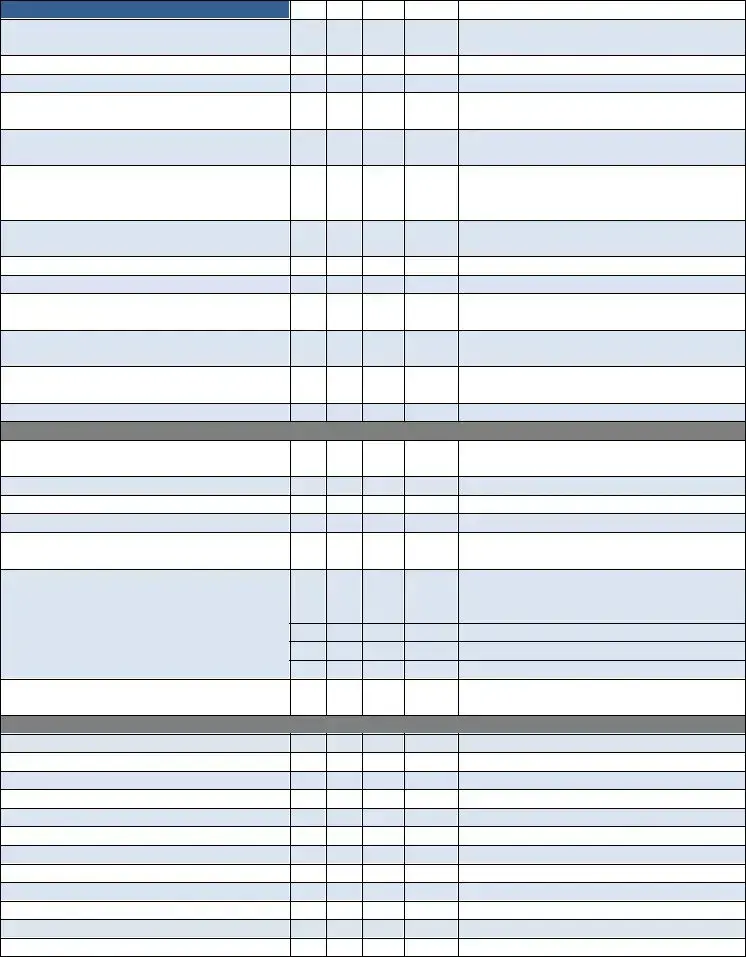
Certified Home Health Aide
49.Visit Frequencies & Duration Consistent with Physician Orders
50. Personal Care Instructions Documented,
Signed & Dated
51.Personal Care Instructions Modified as Appropriate
52. Notes Consistent with Personal Care Instructions Noted on the CHHA Assignment Sheet Completed by the RN/PT/ST/OT
53.Notes Reflect Supervisor Notification of Patient Complications or Changes
54. Visit Frequencies Appropriate for Patient Needs
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
55. Each Note Reflects Personal Care Given
56. Supervisory Visits at Least Every 14 Days by RN or PT
57. Every Note Signed & Dated
PT
58. Assessment Includes Evaluation,
Care Plan & Visit Note
59.Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
60. Visit Frequencies/Duration Consistent with Physician Orders
61.Evidence of Need for Therapy/Social Service
62. Appropriate Missed Visit (MV) Notes
63. Notes Consistent with Physician Orders
64. Evidence of Skilled Service(s) Provided
in Each Note
65.Treatment/Services Provided Consistent with Physician Orders & Care Plan
66. Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
67.Specific Evaluation & “TREAT” Orders Prior to Care
68. Verbal Orders for “TREAT” Orders Prior to Care
69.Homebound Status Validated in Each Visit Note
70. Notes Reflect Progress Toward Goals
71. Evidence of Discharge Planning
72. Evidence of Therapy Home Exercise
Program
73.Discharge/Transfer Summary Complete with Goals Met/Unmet
74. Assessment & Evaluation performed by Qualified Therapist Every 30 Days
75.Supervision of PTA/OTA at Least Every 2 Weeks
76. Qualified Therapy Visit 13th Visit (11, 12, 13)
77.Qualified Therapy Visit 19th Visit (17, 18, 19)
78. Every Visit Note Signed & Dated
SLP
79.Assessment Includes Evaluation, Care Plan & Visit Note
80. Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
81.Visit Frequencies/Duration Consistent with Physician Orders
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
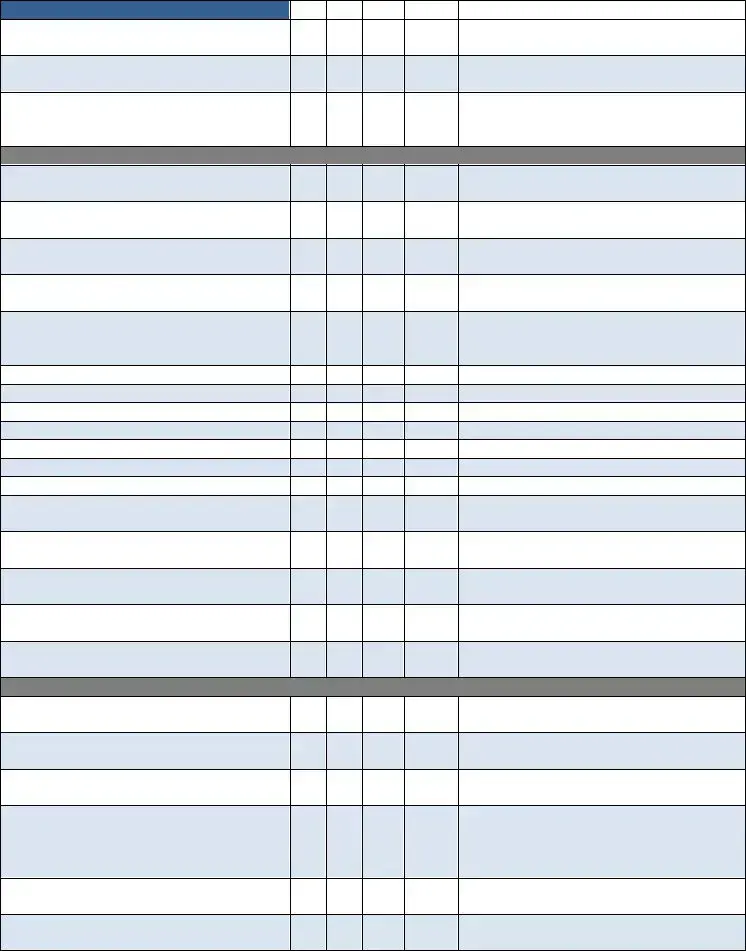
82. Evidence of Need for Therapy/Social Service
83. Appropriate Missed Visit (MV) Note
84. Notes Consistent with Physician Orders
85.Evidence of Skilled Service(s) Provided in Each Note
86. Treatment/Services Provided Consistent with Physician Orders & Care Plan
87.Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
88. Homebound Status Validated in Each Visit
Note
89. Notes Reflect Progress Toward Goals
90. Evidence of Discharge Planning
91.Evidence of Therapy Home Exercise Program
92. Discharge/Transfer Summary Complete with Goals Met/Unmet
93.Supervision of PTA/OTA at Least Every 2 Weeks
94. Every Visit Note Signed & Dated
Miscellaneous
95.Progress Summary Completed(30‐45Days) Each Episode Signed & Dated
96. Field Notes are Submitted & Complete
97. Chart in Chronological Order
98. Chart in Order per Agency Policy
99.Patient Name & Medical Records Number on Every Page
100. Physician Orders are Completed/ Updated for Clinical Tests Such as:
a. Coumadin: Protime/INR
b. Hemoglobin A1C
c. CBC, Metabolic Panel, CMP
d. Others: _______________________
101.Communication with Physician Regarding Test Results
Process Measures:
Timely Initiation of Care
Influenza Received
PPV Ever Received
Heart Failure
DM Foot Care & Education
Pain Assessment
Pain Intervention
Depression Assessment
Medication Education
Falls Risk Assessment
Pressure Ulcer Prevention
Pressure Ulcer Risk Assessment
Additional Comments/Recommendations ‐
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
THE FOLLOWING IS APPLICABLE FOR QUARTERLY MEDICAL REVIEW REPORT
REVIEWED AND SIGNED BY THE FOLLOWING DISCIPLINARY REPRESENTATIVE
______________________________________ |
______________________________________ |
Registered Nurse |
Occupational Therapist (If Applicable) |
______________________________________ |
______________________________________ |
Physical Therapist (If Applicable) |
Speech Language Pathologist (If Applicable) |
______________________________________ |
______________________________________ |
Medical Director |
MSW (If Applicable) |
MR # ______________________
Form Characteristics
| Fact Name | Description |
|---|---|
| Audit Purpose | The Home Health Audit form assesses compliance with health care regulations and patient care standards, ensuring quality service delivery. |
| Updating Year | This form was last updated for calendar year 2013, emphasizing the need for up-to-date practices in home health care. |
| Auditor Information | The auditor must fill in their name and title, along with the date of the audit, ensuring accountability in the review process. |
| Face to Face Requirement | Completion of a face-to-face encounter within 90 days of the start of care is mandatory, reinforcing the importance of direct patient assessment. |
| Patient Rights Acknowledgment | Patients must sign an acknowledgment of their rights, which includes privacy statements and complaint procedures, safeguarding their rights. |
| Medication Management | The audit checks for proper documentation of medications, including changes and interactions, critical for patient safety. |
| Plan of Care Requirements | The plan of care must be signed and dated by a physician within 30 working days, ensuring that all medical directions are current and observed. |
| OASIS Assessment | All OASIS assessments must be completed, signed, and exported within specified timeframes to meet Medicare requirements. |
| Documentation Consistency | Each visit note must consistently reflect provided services and interventions, supporting quality assurance and effective care delivery. |
| State-Specific Considerations | Some items may vary based on state-specific laws governing home health care regulations, making it important for agencies to stay updated. |
Guidelines on Utilizing Home Health Audit
Filling out the Home Health Audit form is an important task that requires attention to detail. This process involves reviewing various aspects of patient care to ensure compliance with healthcare standards. Once the form is completed, it will need to be submitted to the appropriate department for review. Here are the steps to guide you in accurately filling out the form.
- Begin by entering the Auditor’s Name/Title at the top of the form.
- Next, fill in the Date next to the auditor’s name.
- For each question, review the criteria under the Admission section, and select Yes, No, or N/A as appropriate.
- In the MR # column, write the medical record number for reference.
- Provide any relevant comments next to each criterion as needed for clarification.
- Move to the next sections, such as OASIS Assessment Form and Skilled Nursing Clinical Notes, and repeat the process of responding to the requirements.
- Ensure to fill in all applicable criteria under each category, checking for consistency across the sections.
- For questions about Treatment/Services or Progress Summary, document significant details that showcase compliance with care standards.
- Finally, check that each page has the Patient Name and Medical Records Number to maintain organization.
- Once completed, review the form to ensure accuracy before submission.
What You Should Know About This Form
What is the Home Health Audit Form used for?
The Home Health Audit Form is designed to ensure compliance with regulations and best practices in home health care. It covers various aspects of patient care, medical records, and documentation to verify that services are being provided correctly and efficiently. This helps maintain the quality of care and ensures that patients receive the services they need in a timely manner.
Who should complete the Home Health Audit Form?
The audit form should be completed by trained auditors or quality assurance staff within a home health agency. These individuals are usually responsible for reviewing patient records and ensuring that all requirements are met according to regulatory standards and agency policies.
How often should the Home Health Audit Form be used?
The frequency of audits may vary by agency policies, but it is generally recommended to conduct audits regularly, such as quarterly or bi-annually. This ongoing process helps identify areas for improvement and ensures that care quality is continuously assessed and enhanced.
What information is required on the Home Health Audit Form?
The form requires detailed information about various aspects of patient care. This includes patient referrals, physician orders, diagnoses, medication profiles, signed consent forms, and specific assessments, among other items. Each section must be reviewed thoroughly and completed accurately to capture a comprehensive understanding of the patient's care.
What happens if discrepancies are found during the audit?
If discrepancies are discovered during the audit, it is crucial to address them immediately. This may involve further investigation, corrective actions, or adjustments to processes. The goal is to improve care quality and ensure that all required documentation is accurate and complete.
Is training available for those conducting the audit?
Yes, many home health agencies provide training programs for staff involved in auditing processes. These programs aim to educate auditors on the requirements of the Home Health Audit Form, compliance standards, and best practices for reviewing medical records.
Can the audit results impact patient care?
Absolutely. The results of the audit can highlight areas where patient care may not meet standards. This feedback can lead to initiatives aimed at improving service delivery, ensuring patients receive appropriate interventions and care in a timely manner.
What are the implications of not completing the audit properly?
Failing to complete the audit accurately may result in compliance issues, potential sanctions from regulatory bodies, or diminished quality of care for patients. Documenting the findings ensures accountability and supports continuous improvement within the home health agency.
How are issues identified during the audit communicated?
Issues uncovered during the audit are typically documented in a report that outlines specific findings. This report is then communicated to relevant personnel, including management, to facilitate necessary actions and improve care delivery. Regular meetings and reviews may also be held to discuss corrective measures.
Common mistakes
Completing the Home Health Audit form can seem straightforward, yet many individuals encounter challenges that lead to errors. One common mistake is overlooking the Patient Referral Sheet. This document should be filled out completely. An incomplete referral sheet can delay the initiation of care and impact patient outcomes.
Another frequent error relates to the Pre-Admit Physician Order. It is essential that this document is not only signed and dated but also that the verbal orders, if applicable, are properly acknowledged by a registered nurse and the physician. Incomplete or missing signatures can hinder the audit process.
Using the correct diagnosis codes is crucial. When filling out sections M1020 and M1022, many make the mistake of either misplacing or misclassifying the primary and secondary diagnosis codes. All diagnoses must be supported and sequenced correctly to ensure compliance with Medicare requirements.
Additionally, some individuals fail to document medication changes accurately. The form requires a detailed account of new and changed medications, including food and over-the-counter (OTC) interactions. Omitting this information can result in unsafe care practices.
A signed and dated Patient/Client Service Agreement is pivotal, but some tend to forget this step. An incomplete service agreement may exhibit negligence in care provision and can have serious legal implications for the agency.
When it comes to the OASIS Assessment Form, problems often arise. Some forget to review all assessments for consistency in coordination with the discipline responsible for completing them. This oversight not only affects the patient's care plan but may also complicate the audit review.
Documentation of skilled nurse visit frequencies must align with physician orders. Mistakes occur when visit notes don't reflect the frequency and duration appropriately. Discrepancies here can signal issues in providing consistent care to patients.
Finally, many individuals neglect the importance of signature and date on every note. This seemingly minor detail is critical for accountability and ensuring that documentation aligns with care procedures. Missing signatures can raise red flags during the audit process and hinder credibility.
Documents used along the form
The Home Health Audit form is an important document used to evaluate the quality and compliance of home health care services. However, it is often accompanied by several other forms and documents that provide additional context and necessary information regarding patient care. Below is a list of related documents commonly used alongside the Home Health Audit form, each one serving a unique purpose.
- Patient Referral Sheet: This document is essential as it outlines the reasons for referral to home health services. It includes the patient’s medical background, specific needs, and any requests made by the referring physician, ensuring that the home health agency has all the pertinent information for initiating care.
- Service Agreement: This is a signed document between the patient and the agency that outlines the services to be provided, the rights of the patient, and the responsibilities of both parties. It is crucial for establishing mutual understanding before care begins.
- OASIS Assessment Form: The Outcome and Assessment Information Set (OASIS) is used to collect information on patients’ health status and outcomes at various points in their care. It plays a critical role in determining reimbursement and quality measures in home health care.
- Physician Orders: These are specific instructions provided by a physician regarding the treatment and care the patient should receive. This document ensures that the home health staff is following the prescribed care plan accurately.
- Skilled Nursing Clinical Notes: These notes are made by the nursing staff during home visits and detail the care provided, the patient’s condition, and any changes observed. They serve as a record of ongoing treatment and facilitate communication among the care team.
These documents, when used in conjunction with the Home Health Audit form, help create a comprehensive picture of patient care and ensure compliance with regulations and best practices in home health services. Proper documentation is vital for not only providing quality care but also for effective communication among healthcare providers, which ultimately benefits the patient.
Similar forms
The Home Health Audit form shares similarities with various essential healthcare documents. Each of the following documents serves as a crucial component in patient care assessment and management.
- Patient Care Plan: This document outlines the specific goals and interventions for individual patients, similar to how the Home Health Audit ensures patient needs are met through structured plans of care.
- Medication Administration Record (MAR): Like the Home Health Audit, this record tracks medication orders and administration, ensuring accuracy and compliance with physician directives.
- OASIS Assessment Form: Both forms document patient assessments and outcomes, focusing on meeting regulatory requirements and improving care delivery.
- Skilled Nursing Visit Notes: These notes provide detailed patient interactions and care measures, reflecting the requirements outlined in the Home Health Audit for documenting skilled services.
- Physician Orders: These documents direct patient treatment plans and are closely monitored in both the Home Health Audit and ongoing patient care management.
- Patient Admission Forms: Admission documentation captures essential patient information upon entry into care, paralleling how the Home Health Audit assesses initial compliance and readiness.
- Treatment Progress Notes: Both documents track patients' progress and adjust care plans accordingly, ensuring ongoing evaluation of treatment effectiveness.
- Patient Discharge Summary: Like the Home Health Audit, this summary records essential information and follow-up steps for continued care after discharge.
- Home Health Aide Assignment Sheet: This sheet details the tasks and schedules for home health aides, analogous to the structured approach in the Home Health Audit to ensure quality service delivery.
- Emergency Preparedness Plans: Both documents emphasize the importance of safety and preparedness in care settings, ensuring that protocols are in place for potential emergencies.
Dos and Don'ts
When filling out the Home Health Audit form, there are several important considerations to keep in mind. Following these guidelines can help ensure that the form is completed accurately and efficiently.
- Do ensure all sections of the form are completed in detail to avoid any gaps in information.
- Do double-check that all necessary signatures are obtained, especially from the healthcare provider.
- Do provide clear and concise comments where indicated to promote understanding of the patient's status.
- Do review the documentation for consistency, ensuring that care ordered aligns with patient needs and goals.
- Don’t rush through the form; take the time needed to fill it out properly to avoid errors.
- Don’t use any abbreviations or jargon that might confuse others reviewing the form.
- Don’t neglect to include important updates or changes in patient care or condition as they arise.
Misconceptions
Misconception 1: The Home Health Audit form is only for large agencies.
This is not accurate. The form can benefit agencies of all sizes. Smaller agencies also need to ensure compliance with regulations. Completing the audit helps identify areas needing improvement, regardless of agency size.
Misconception 2: Completing the form is optional and does not impact patient care.
In reality, completing the Home Health Audit form is crucial. Regular audits help maintain high standards for patient care. They identify discrepancies that can lead to better outcomes for patients. Skipping this process can put patient safety at risk.
Misconception 3: The audit only focuses on paperwork and does not assess actual care.
This is a misunderstanding. While documentation is vital, the audit reviews care practices too. It considers how well the care aligns with established plans and goals. Actual patient care is assessed as part of the overall evaluation.
Misconception 4: If the audit shows issues, the agency will face severe penalties immediately.
This is misleading. While serious issues may lead to consequences, audits primarily focus on improvement. Many agencies have the opportunity to correct deficiencies. A proactive approach can help agencies enhance their care practices and avoid penalties in the future.
Key takeaways
Filling out and using the Home Health Audit form requires attention to detail. Here are six key takeaways to keep in mind:
- Complete Information: Ensure that all sections are fully completed. Missing or incomplete data can lead to audits not meeting standards.
- Timelines Matter: Familiarize yourself with important timelines. For instance, certain encounters and evaluations must occur within specified days of the start of care or recertification.
- Documentation Consistency: Keep all documentation consistent. Double-check that medications, diagnoses, and care plans align with what is documented in the patient's records.
- Collaboration is Key: Engage with all team members involved in patient care. Effective communication ensures that everyone is aware of changes and updates to the patient's care plan.
- Follow Agency Policies: Adhere to your agency's specific policies and procedures. Each agency may have unique requirements that must be met during the audit process.
- Regular Reviews: Conduct regular reviews of the forms and documentation. This practice helps identify areas that need improvement before an official audit occurs.
Browse Other Templates
What Does Sole Physical Custody Mean - Provides a clear structure for future custody discussions.
UMWA Address Change Form,Address Update Request Form,Change of Residence Application,Miner's Address Modification Form,Widow's Address Adjustment Request,Health and Retirement Funds Address Notification,Miner/Widow Information Update Form,Address Cor - Accurate information is critical for successful address updates.
Injury/Incident Report Form Daycare - Report serious injuries that necessitate urgent action.