Fill Out Your Hospital Discharge Form
The Hospital Discharge form serves as a vital document that captures essential information necessary for a smooth transition from hospital to home or other care settings. It requires detailed input from medical professionals, ensuring the patient’s readiness for discharge is clearly documented. Key components of the form include the patient's identification details, the date services should end, and specific elements needed for discharge planning. Among these are physician notes reflecting readiness for discharge, a description of the discharge plan discussed with both the attending provider and the patient or family, and relevant therapy notes if applicable. Importantly, the form also addresses Medicare coverage policies, emphasizing compliance with regulations regarding hospital services. Additional sections demand thorough documentation of the patient's medical history, diagnosis, treatment, and current condition, as well as the follow-up care necessary post-discharge. Each form requires the signature and contact information of the provider completing it, ensuring accountability and continuity of care. This comprehensive approach not only safeguards the patient’s health but also assists healthcare providers in maintaining standards set forth by insurance protocols.
Hospital Discharge Example
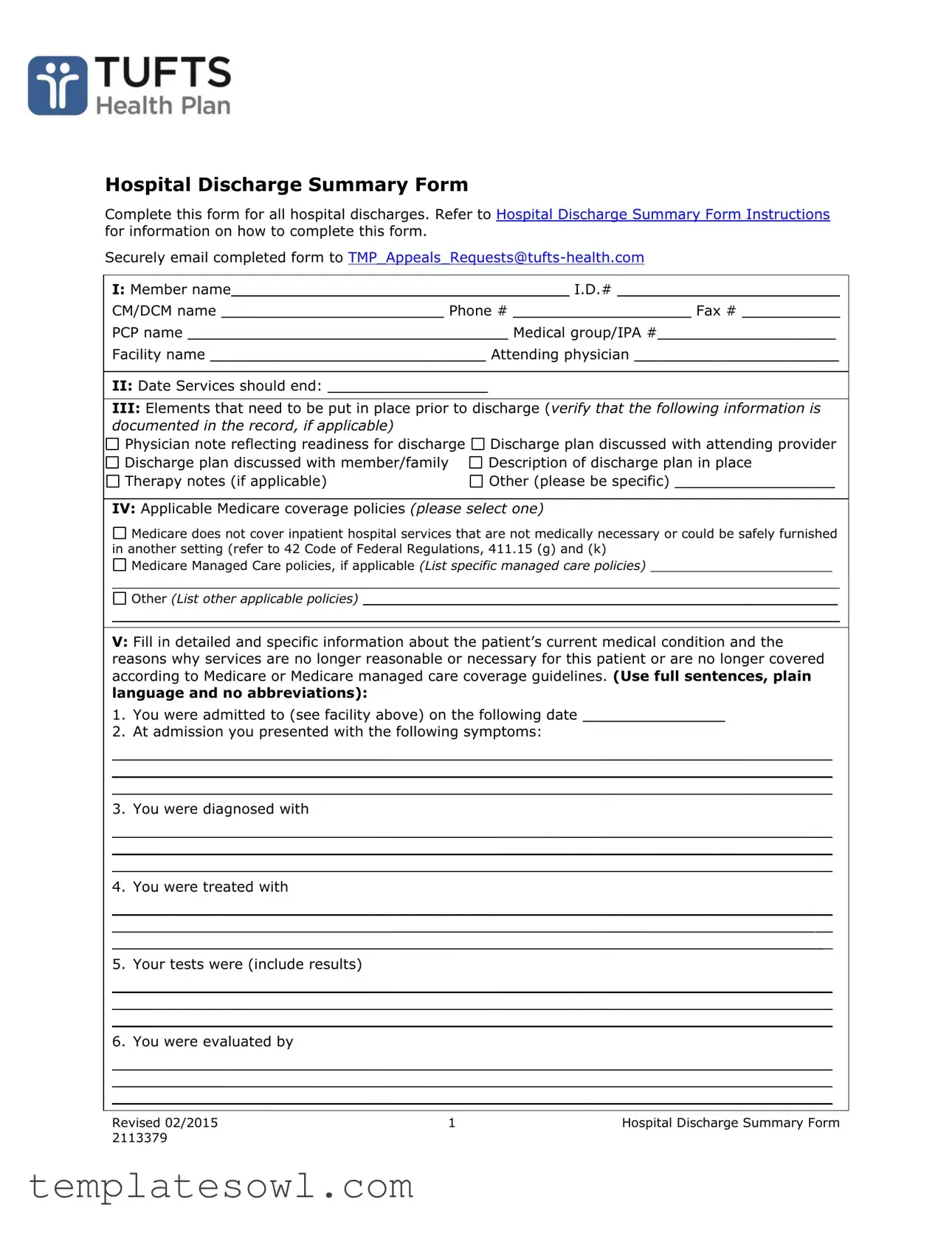
Hospital Discharge Summary Form
Complete this form for all hospital discharges. Refer to Hospital Discharge Summary Form Instructions for information on how to complete this form.
Securely email completed form to
I:Member name______________________________________ I.D.# _________________________
CM/DCM name _________________________ Phone # ____________________ Fax # ___________
PCP name ____________________________________ Medical group/IPA #____________________
Facility name _______________________________ Attending physician _______________________
II:Date Services should end: __________________
III:Elements that need to be put in place prior to discharge (verify that the following information is documented in the record, if applicable)
Physician note reflecting readiness for discharge |
Discharge plan discussed with attending provider |
Discharge plan discussed with member/family |
Description of discharge plan in place |
Therapy notes (if applicable) |
Other (please be specific) __________________ |
IV: Applicable Medicare coverage policies (please select one)

 Medicare does not cover inpatient hospital services that are not medically necessary or could be safely furnished in another setting (refer to 42 Code of Federal Regulations, 411.15 (g) and (k)
Medicare does not cover inpatient hospital services that are not medically necessary or could be safely furnished in another setting (refer to 42 Code of Federal Regulations, 411.15 (g) and (k)

 Medicare Managed Care policies, if applicable (List specific managed care policies) _______________________
Medicare Managed Care policies, if applicable (List specific managed care policies) _______________________
____________________________________________________________________________________________

 Other (List other applicable policies) ____________________________________________________________
Other (List other applicable policies) ____________________________________________________________
____________________________________________________________________________________________
V:Fill in detailed and specific information about the patient’s current medical condition and the reasons why services are no longer reasonable or necessary for this patient or are no longer covered according to Medicare or Medicare managed care coverage guidelines. (Use full sentences, plain language and no abbreviations):
1.You were admitted to (see facility above) on the following date ________________
2.At admission you presented with the following symptoms:
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
3. You were diagnosed with
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
4. You were treated with
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
5. Your tests were (include results)
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
6. You were evaluated by
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
Revised 02/2015 |
1 |
Hospital Discharge Summary Form |
2113379 |
|
|
7. You are now (list current treatment plan and/or state the medical issue is resolved)
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
8.Your provider feels that your condition has improved and that the care you need now could safely be provided in/at
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
9. Your discharge plan and
_________________________________________________________________________________
_________________________________________________________________________________
_________________________________________________________________________________
VI: Printed name of person completing the form __________________________________________
Signature of person completing the form ________________________________________________
Phone # ___________________________________ Fax # _________________________________
Provider Relations
Revised 02/2015 |
2 |
Hospital Discharge Summary Form |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Form | The Hospital Discharge Summary Form is designed to document the details of a patient's discharge from a hospital, ensuring all necessary information is recorded for continued care. |
| Submission Method | Once completed, the form must be securely emailed to TMP_Appeals_Requests@tufts-health.com for processing and confirmation of discharge details. |
| Medicare Coverage Guidelines | According to 42 Code of Federal Regulations, 411.15 (g) and (k), Medicare does not cover inpatient hospital services that are not medically necessary. |
| Required Information | Specific elements, such as the physician’s readiness for discharge and the patient’s current medical condition, need to be documented to validate the discharge plan. |
Guidelines on Utilizing Hospital Discharge
Once you have completed the Hospital Discharge Summary Form, ensure that all required sections are accurately filled out. This process is vital for a smooth transition of care and facilitates your follow-up services. After the form is completed, it needs to be sent securely via email to the provided address.
- Fill in the Member's name and I.D. number at the top of the form.
- Include the CM/DCM name, phone number, and fax number.
- Record the Primary Care Provider (PCP) name and their medical group/IPA number.
- Enter the facility name where the patient was treated and the name of the attending physician.
- Write the date services should end.
- Document whether a physician note reflects readiness for discharge.
- Confirm if the discharge plan has been discussed with both the attending provider and the member/family.
- Provide a description of the discharge plan in place and any relevant therapy notes.
- Indicate other pertinent information, if applicable.
- Select the applicable Medicare coverage policies and provide details for each selection.
- Fill in detailed information about the patient’s current medical condition and reasons for the discharge.
- List the date of admission and the symptoms presented at that time.
- State the diagnosis received during the hospital stay.
- Document treatments administered during the patient’s time in the hospital.
- Include results from tests conducted during their stay.
- Write the name of the evaluators during the hospital stay.
- Describe the current treatment plan or confirm if the medical issue has resolved.
- State where the patient’s ongoing care can be safely provided.
- Outline the discharge plan and follow-up care instructions.
- Print the name of the individual completing the form and obtain their signature.
- Provide the phone number and fax number of the person completing the form.
After completing these steps, make sure to review the form for accuracy before emailing it to the designated address.
What You Should Know About This Form
What is the purpose of the Hospital Discharge form?
The Hospital Discharge form is used to summarize a patient’s hospital stay and outline the necessary information for their safe transition to the next phase of care. It ensures that all pertinent details regarding the patient’s discharge are documented and communicated effectively amongst healthcare providers.
Who should complete the Hospital Discharge form?
The form should be completed by a healthcare professional involved in the patient’s care, such as the attending physician or discharge planner. This ensures that the information is accurate and reflects the latest updates on the patient's condition and treatment plan.
How do I submit the completed Hospital Discharge form?
Once the form is completed, it must be securely emailed to TMP_Appeals_Requests@tufts-health.com. Ensure that all sections are filled out accurately to prevent delays in processing.
What information is required on the Hospital Discharge form?
The form requires various details, including the patient’s name, ID number, the attending physician’s name, facility name, and a detailed account of the patient’s current medical condition and discharge plan. Each section must be carefully filled out to provide a comprehensive overview of the patient’s care.
What elements need to be in place before discharge?
Before discharge, the following elements must be verified: a physician's note documenting readiness for discharge, discussion of the discharge plan with the provider and the patient/family, a clear description of the discharge plan, therapy notes if needed, and any other relevant information. This helps ensure that the patient is truly ready to leave the hospital.
What if the patient’s condition changes before discharge?
If a patient’s condition changes, the discharge plan must be reassessed. Any necessary modifications should be documented on the form, along with updated information reflecting the patient's new condition and needs.
What are applicable Medicare coverage policies?
This section of the form requires identifying and selecting applicable Medicare coverage policies. Indicate whether services were not medically necessary or if they could have been safely provided in another setting. Clarity in this section is vital for compliance with Medicare guidelines.
What kind of follow-up care should be included in the discharge plan?
The discharge plan should include specific details about follow-up appointments, medications, therapy requirements, and any other care needed post-discharge. This ensures patients have a clear understanding of their next steps after leaving the hospital.
How can I verify the form is completed correctly?
To verify correctness, review each section of the form carefully. Make sure all required fields are filled out with accurate and detailed information. It may also be helpful to have another healthcare professional review the form before submission to catch any potential errors.
Common mistakes
Completing a Hospital Discharge form can be a daunting task, and it’s easy to make mistakes along the way. One common error is neglecting to provide complete and accurate member information. Failing to fill in the member's name, ID number, or other identifying details can lead to delays in processing the discharge. Information should be clear and precise to ensure proper communication between healthcare providers and insurers.
Another mistake often made is rushing through the medical condition details. The section requires a thorough explanation of the patient’s status. Using brief phrases or omitting critical information can confuse the attending physician and the clinical team reviewing the discharge. It’s important to describe the patient's symptoms, diagnosis, and response to treatment in full sentences to create a complete picture of their care.
Failure to verify the discharge plan with both the attending provider and the patient is another major slip. Before leaving the hospital, it is essential to have a clear discharge plan in place. This includes discussing care needs with the patient and their family. If this step is missed, patients may leave without understanding their follow-up care, which can lead to unnecessary complications or readmissions.
Many individuals overlook the importance of listing applicable Medicare coverage policies properly. Ignoring this section or failing to specify relevant policies can create problems with insurance claims later on. It’s vital to understand the insurance coverage details that relate to the discharge, ensuring that services rendered are covered and avoiding potential financial burdens for the patient.
Finally, it’s critical not to forget to sign and date the form before submission. A lack of signature or an incomplete date can render the document invalid, further delaying the discharge process. By ensuring every section of the form is completed accurately and comprehensively, patients can facilitate a smooth transition from hospital to home.
Documents used along the form
The Hospital Discharge Summary Form is a critical document used when a patient is ready to leave a hospital. However, several other forms and documents accompany it to ensure a smooth transition from hospital care to home or another facility. Here’s a brief overview of some commonly used documents that work in conjunction with the Hospital Discharge Summary Form.
- Discharge Instructions: This document provides detailed guidelines for patients and their families about post-discharge care. It includes information about medications, follow-up appointments, and warning signs to monitor.
- Medication Reconciliation Form: This form helps to ensure that patients leave the hospital with a complete and accurate list of medications. It outlines any changes made during the hospital stay and serves to prevent medication errors post-discharge.
- Referral Form: A referral form may be required if the patient needs to see a specialist after leaving the hospital. It ensures that the necessary information is passed smoothly between the primary care physician and the specialist.
- Home Health Care Plan: For patients who will require ongoing care at home, this document outlines the services that will be provided, including personal care, therapy, and medical equipment needs.
- Follow-Up Appointment Scheduling: This document records the details of any follow-up appointments that the patient needs after discharge. It often includes the date, time, and location of the appointment, along with any necessary instructions.
- Patient Education Materials: These materials offer information on managing the patient’s condition, including lifestyle changes, nutritional advice, and resources for further support.
- Insurance Authorization Forms: Depending on the patient's insurance, this document may be necessary to ensure that post-discharge services are covered, providing the required approvals for care after leaving the hospital.
Utilizing these forms in conjunction with the Hospital Discharge Summary ensures that patients are equipped with the necessary resources and information as they transition from hospital care back to their homes or other settings. This coordinated approach not only enhances patient safety but also promotes better health outcomes.
Similar forms
- Patient Discharge Instruction Sheet: Similar to the Hospital Discharge form, this document provides guidelines and instructions for patients upon leaving a healthcare facility. It outlines necessary aftercare, medication instructions, and when to seek further medical attention, ensuring continuity of care post-discharge.
- Transfer Summary Form: This form, used when transferring a patient from one facility to another, shares a similar purpose. It documents the patient's condition, treatment history, and specific needs, allowing the receiving facility to provide appropriate care without interruptions.
- Release of Information Authorization: Patients may need to complete this form, permitting healthcare providers to share their medical information with other entities. Like the Hospital Discharge form, it is essential for maintaining clear communication and ensuring all parties involved in the patient’s care are informed about their health status.
- Continuity of Care Document (CCD): This electronic document captures a patient's health summary and ongoing care needs. Similar to the Hospital Discharge form, it facilitates transitions between healthcare providers and settings, ensuring everyone involved has access to the same comprehensive information.
- Home Health Care Plan: When a patient is discharged but requires ongoing support at home, this document outlines the care they need. It mirrors the Hospital Discharge form as it provides detailed instructions on services required, ensuring a smooth recovery process.
- Patient Follow-Up Care Plan: This plan lays out the steps a patient should take after discharge, including follow-up appointments and treatment regimens. Like the Hospital Discharge form, it emphasizes the importance of managing ongoing health needs and preventing complications.
- Medication Reconciliation Form: This form lists all medications a patient should continue after discharge. Its purpose aligns with the Hospital Discharge form, as both documents emphasize the importance of proper medication management for continuous care.
- Informed Consent Form: Before certain procedures, patients typically sign this document to confirm their understanding of the treatment. It shares similarities with the Hospital Discharge form in that both ensure patients are informed about their health decisions and care plans before leaving the facility.
- Palliative Care Plan: For patients with chronic or terminal conditions, this plan outlines ongoing care preferences and end-of-life decisions. It is akin to the Hospital Discharge form in that it addresses the need for comprehensive communication regarding patient health and care continuity.
- Emergency Contact and Caregiver Information Form: This document designates contacts and caregivers who can manage health decisions after discharge. It serves a similar role to the Hospital Discharge form by ensuring that the patient's support system is informed and prepared to assist correctly.
Dos and Don'ts
When filling out the Hospital Discharge form, careful attention to detail is crucial. Here are four guidelines to follow as well as common pitfalls to avoid:
- Do ensure accuracy. Double-check that all patient information is correct, including name, identification number, and contact details.
- Do provide detailed medical history. Clearly outline the patient's current medical condition and the reasons for discharge, using complete sentences without abbreviations.
- Do verify necessary documentation. Confirm that all required elements, such as the physician's note and discharge plan, are included in the record.
- Do follow submission guidelines. Send the completed form securely to the specified email address to maintain confidentiality.
- Don't rush through the process. Take the time needed to complete the form thoroughly to avoid mistakes.
- Don't leave sections blank. Ensure that all applicable areas are filled out entirely, as omissions could delay the discharge process.
- Don't use medical jargon. Write in plain language to ensure clarity for all parties involved.
- Don't ignore Medicare policies. Understand and select the appropriate coverage policies relevant to the patient's care during the discharge process.
Misconceptions
Misconceptions about the Hospital Discharge Form can lead to misunderstandings and complications in the discharge process. Here are some common misconceptions explained:
- The form is only needed for certain patients. Many believe the Hospital Discharge Form is required solely for specific cases. In reality, it needs to be completed for all hospital discharges to ensure comprehensive documentation.
- Only doctors can fill out the form. Some think that only physicians are authorized to complete the form. However, any qualified staff member can fill it out, provided they have the necessary information and understanding of the patient's case.
- The form is optional and not crucial. There’s a misconception that the form can be overlooked. In fact, it’s a critical part of the discharge process. It ensures that all aspects of the patient's care and discharge plan are clearly documented.
- Discharge planning doesn’t need to occur until the patient is ready to leave. Some assume discharge planning is a last-minute task. In truth, it should begin as soon as the patient is admitted. Early planning helps ensure a smooth transition out of the hospital.
- The form does not need to be sent securely. A common belief is that emailing the form is sufficient without any security measures. However, protecting patient information is essential. The form must be emailed securely to comply with privacy regulations.
- Medicare coverage policies are not relevant to the form. Many people assume that coverage policies do not apply to discharge forms. On the contrary, documenting applicable Medicare policies is crucial to ensure the services provided are covered.
- Once the form is filled out, it doesn’t need to be reviewed. Some think the form only has to be completed and submitted. In reality, it should be reviewed for accuracy and completeness to avoid any issues later.
- Family members do not need to be involved in the discharge plan. There is a misconception that family members are not important in the discharge process. Engaging family in discussions about the discharge plan is vital for ensuring proper understanding and continuity of care.
Understanding these misconceptions can help ensure a smoother discharge process and better outcomes for patients.
Key takeaways
When using the Hospital Discharge form, attention to detail is crucial. Here are some key takeaways to ensure the process is smooth and effective:
- Complete All Sections: Every part of the form must be filled out accurately. This includes patient information, discharge plans, and applicable Medicare policies.
- Verify Readiness for Discharge: Confirm that the physician's note indicates readiness for discharge. This helps prevent premature discharges and ensures patient safety.
- Document Clear Discharge Plans: Outline the discharge plan thoroughly, including therapy notes and follow-up care instructions. This documentation aids in continuity of care.
- Email the Completed Form Securely: The completed form should be sent securely to the designated email address. This is important for maintaining patient confidentiality.
- Use Plain Language: When detailing the patient's condition and treatment, use clear and straightforward language. Avoid abbreviations to enhance understanding.
- Include Detailed Patient History: Provide comprehensive details about the patient's medical history, symptoms, diagnosis, and treatment. This information is vital for proper follow-up and care.
Browse Other Templates
Social Security Tax Form - Tax information included on this form is confidential and should be protected.
Da7652 - Information on automatic promotions and their relation to medical qualifications is included in the form.