Fill Out Your Hospital Discharge Papers Form
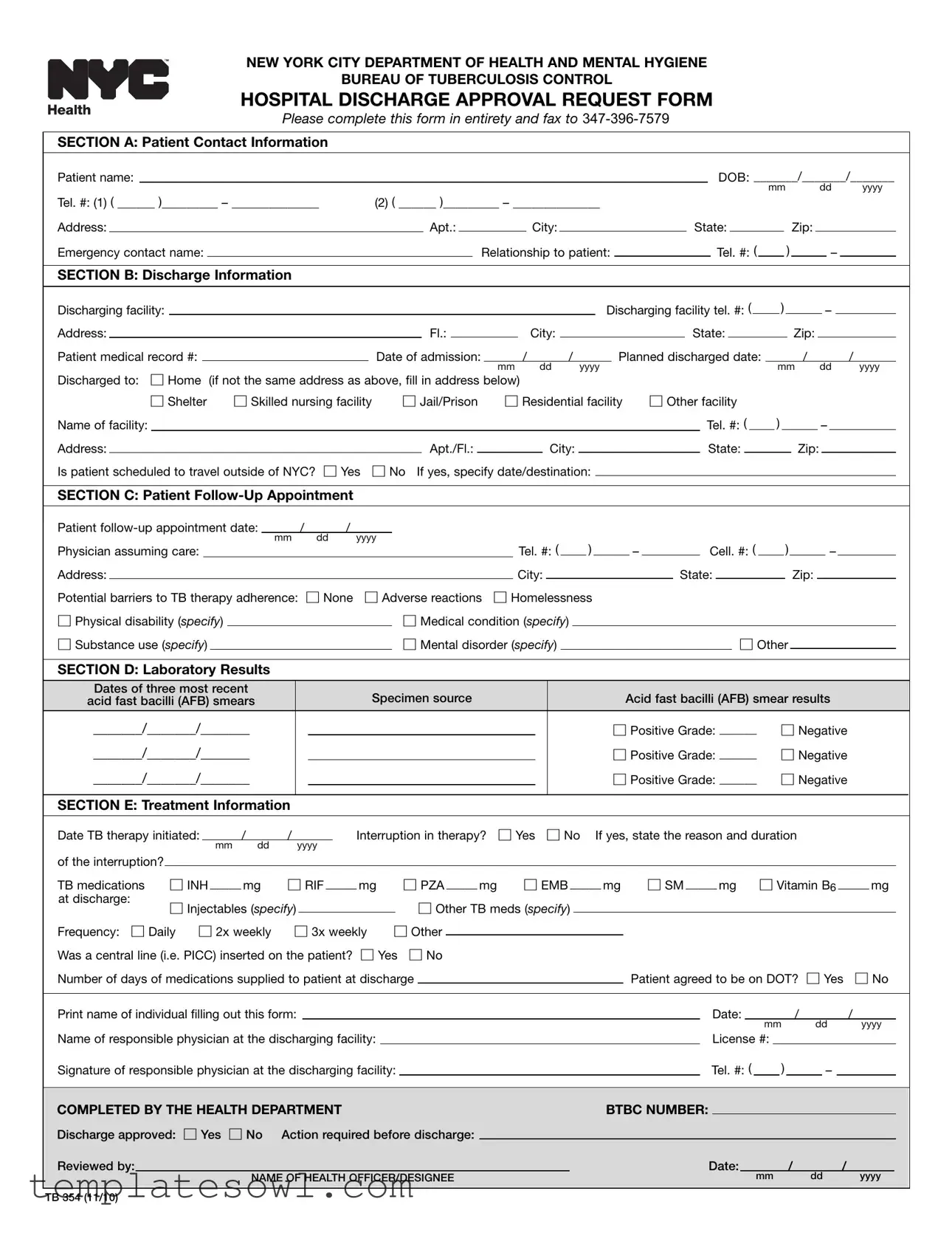
The Hospital Discharge Papers form, formally known as the Hospital Discharge Approval Request Form (TB 354), serves a crucial purpose within the framework of public health, particularly pertaining to the management of tuberculosis (TB) cases in New York City. This form requires comprehensive patient details, including contact information and medical history, to ensure continuity of care upon discharge. It encompasses sections dedicated to discharge information, such as the facility's name and the patient's planned discharge date, as well as the location to which the patient will be transferred. Notably, the form also addresses follow-up appointments and potential barriers to adherence with TB therapy. Laboratory results must be reported, particularly the outcomes of the most recent acid fast bacilli (AFB) smear tests, which are vital for determining the patient's infectious status. Additionally, the form captures treatment details, including the medications prescribed, dosages, and any interruptions in therapy. Completing and submitting the form is mandated by the New York City Health Code, ensuring that all necessary health protocols are followed prior to discharging individuals diagnosed with infectious TB. This process not only safeguards the health of the patient but also contributes to the broader public health goal of controlling TB transmission within the community.
Hospital Discharge Papers Example
NEW YORK CITY DEPARTMENT OF HEALTH AND MENTAL HYGIENE
BUREAU OF TUBERCULOSIS CONTROL
HOSPITAL DISCHARGE APPROVAL REQUEST FORM
Please complete this form in entirety and fax to
SECTION A: Patient Contact Information
|
|
Patient name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DOB: _______/_______/_______ |
|
|
|||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||
|
|
Tel. #: (1) ( ______ )_________ – ______________ |
|
(2) ( ______ )_________ – ______________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Apt.: |
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
Emergency contact name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Relationship to patient: |
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
SECTION B: Discharge Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discharging facility tel. #: ( |
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fl.: |
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
Patient medical record #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of admission: |
|
|
/ |
|
/ |
|
|
|
|
|
|
Planned discharged date: |
|
|
/ |
|
|
|
|
|
|
|
|
|
|
|
/ |
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||||||||||||||||
|
|
Discharged to: |
☐ Home (if not the same address as above, fill in address below) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
☐ Shelter |
☐ Skilled nursing facility |
|
|
|
|
☐ Jail/Prison |
|
☐ Residential facility |
|
|
☐ Other facility |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Name of facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Apt./Fl.: |
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
|
Is patient scheduled to travel outside of NYC? |
☐ Yes ☐ No If yes, specify date/destination: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION C: Patient |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
Patient |
|
/ |
|
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
Physician assuming care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
|
) |
|
|
|
|
|
– |
|
|
|
|
|
Cell. #: ( |
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
Potential barriers to TB therapy adherence: ☐ None |
☐ Adverse reactions |
☐ Homelessness |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
☐ Physical disability (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Medical condition (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
☐ Substance use (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Mental disorder (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION D: Laboratory Results |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
Dates of three most recent |
|
|
|
|
|
|
|
|
|
|
|
Specimen source |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acid fast bacilli (AFB) smear results |
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
acid fast bacilli (AFB) smears |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION E: Treatment Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Date TB therapy initiated: |
|
/ |
|
|
/ |
|
|
|
|
|
|
Interruption in therapy? |
|
☐ Yes |
|
☐ No |
|
|
If yes, state the reason and duration |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
|
|
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
of the interruption? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
☐ RIF _____ mg |
|
|
|
|
☐ PZA _____ mg |
|
|
☐ EMB _____ mg |
|
|
☐ SM _____ mg ☐ Vitamin B6 _____ mg |
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
TB medications |
|
|
☐ INH _____ mg |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
at discharge: |
|
|
☐ Injectables (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
☐ Other TB meds (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
Frequency: ☐ Daily ☐ 2x weekly |
|
☐ 3x weekly |
|
|
☐ Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
Was a central line (i.e. PICC) inserted on the patient? |
☐ Yes ☐ No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
Number of days of medications supplied to patient at discharge |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient agreed to be on DOT? ☐ Yes |
☐ No |
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Print name of individual filling out this form: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
/ |
|
|
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
|
yyyy |
|
|
||||||||||||||||||||||||
|
|
Name of responsible physician at the discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
License #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
|
Signature of responsible physician at the discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMPLETED BY THE HEALTH DEPARTMENT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BTBC NUMBER: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||
|
|
Discharge approved: ☐ Yes |
☐ No |
Action required before discharge: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
Reviewed by: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: |
|
/ |
|
|
/ |
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF HEALTH OFFICER/DESIGNEE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
|
|
|
|
|
|
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TB 354 (11/10)
Guidelines for How to Complete and Submit the Mandatory TB
Hospital Discharge Approval Request Form (TB 354)
As of June 16, 2010, Article 11 of the New York City Health Code mandates health care providers to obtain approval from the New York City Department of Health & Mental Hygiene (DOHMH) before discharging infectious TB patients from the hospital.
Discharge of an Infectious (sputum smear positive) Tuberculosis Patient
Health care providers must submit a Hospital Discharge Approval Request Form (TB 354) at least 72 hours prior to the anticipated discharge date. The DOHMH will review the form and approve or request additional information before the patient can be discharged from the health care facility.
Weekday
Weekend and Holiday Discharge: All arrangements for discharge should be made in advance when weekend or holiday discharge is anticipated.
For detailed information about hospital admission and discharge of TB patients, please refer to the New York City Department of Health and Mental Hygiene, Bureau of TB Control Policies and Protocols manual available online at
Instructions for Completing the Hospital Discharge Approval Request Form (TB 354)
Section A Patient contact information: Provide the patient’s contact information including patient’s name, a verified address and telephone numbers. In addition, include a name of an emergency contact, the contact’s relationship to the patient and the contact’s verified phone number.
Section B Discharge information: Provide the name and phone number of the discharging facility, the medical record number of the patient at the facility, date the patient was admitted, planned discharge date, and the location to which the patient is being discharged. If the patient will be discharged to a location other than the patient’s address listed in Section A, a facility name (if applicable), address and phone number must be provided. If the patient plans to travel, provide the date and destination.
Section C Patient
Section D Laboratory results: Report the results of the three most recent acid fast bacilli (AFB) smears including the date of specimen collection, specimen source, and AFB smear results and/or grade.
Section E Treatment information: Fill in the date TB treatment was initiated. If there were any treatment interruptions, indicate the reason and number of days treatment was stopped. Check the box next to each prescribed drug and state dosages for each drug. Write in drugs and dosages for drugs not specified. Specify the treatment frequency by checking one of the three boxes, or writing in a different treatment schedule. State whether the patient will have a central line inserted at the time of discharge. If TB medication will be supplied to the patient at discharge, write the number of days for which the medication will be supplied. State whether the patient agreed to be on directly observed therapy (DOT).
After Section E, the name of the person completing the form should be printed and the authorized physician at the discharging facility must print and sign their name, and provide their medical license number and telephone number.
Forms should be faxed to the DOHMH at
If you have questions about completing the form, please call 311 and ask to speak to a Bureau of Tuberculosis Control physician.
To fulfill State requirements for communicable disease reporting, health care providers must report all suspected or confirmed TB cases to the Health Department via Reporting Central (formerly Universal Reporting Form (URF)). Instructions for reporting a case of tuberculosis can be found at
NOTE: A discharge approval request form does not substitute required case reports.
TB 354 (11/10)
Form Characteristics
| Fact Title | Details |
|---|---|
| Purpose | The Hospital Discharge Approval Request Form is essential for ensuring the safe discharge of tuberculosis (TB) patients from healthcare facilities in New York City. |
| Compliance Requirement | As mandated by Article 11 of the New York City Health Code, health care providers must obtain approval from the New York City Department of Health & Mental Hygiene (DOHMH) prior to discharging infectious TB patients. |
| Submission Timeline | Providers must submit the discharge request at least 72 hours before the planned discharge date to allow for review and approval. |
| Approval Notification | The DOHMH typically reviews submissions made during weekdays and notifies providers of approval or additional requirements within 24 hours. |
| Weekend/Holiday Protocol | For discharges anticipated on weekends or holidays, providers should arrange approvals in advance to avoid delays in patient care. |
| Patient Information | Critical patient details, including follow-up appointments and potential barriers to treatment adherence, must be included in the form to ensure effective continuity of care. |
| Additional Resources | For further guidance on the process, healthcare providers can refer to the New York City Department of Health and Mental Hygiene's Bureau of TB Control Policies and Protocols manual online. |
Guidelines on Utilizing Hospital Discharge Papers
After filling out the Hospital Discharge Papers, the next step is to ensure that the completed form is submitted to the appropriate health authorities before the patient's discharge. This process involves checking the accuracy of the information and ensuring timely submission to avoid any delays in discharge.
- Start with Section A: Fill in the patient's contact information. Enter the patient's name, date of birth, and telephone numbers. Provide the address and emergency contact information, including the contact's name, relationship to the patient, and their phone number.
- Move to Section B: Enter discharge information. Include the name and phone number of the discharging facility, the patient’s medical record number, admission date, and planned discharge date. Specify the discharge location, and if it differs from the address in Section A, provide additional details about the facility.
- In Section C: Add the patient’s follow-up appointment date, including the physician assuming care along with their contact information. Indicate any potential barriers to TB therapy adherence by checking the appropriate boxes.
- Proceed to Section D: Document the laboratory results. List the dates and results for the three most recent acid fast bacilli (AFB) smear tests.
- Complete Section E: Fill in the date TB therapy began. Report any interruptions in therapy, along with the reason and duration. List the prescribed TB medications along with their dosages. Also, indicate if a central line was inserted, how many days of medication will be supplied at discharge, and if the patient agreed to be on directly observed therapy (DOT).
- Print the name of the individual who filled out the form. Obtain the name, license number, and signature of the responsible physician at the discharging facility.
- Finally, fax the completed form to the Department of Health at 347-396-7579. Make sure to do this well ahead of the planned discharge date to ensure compliance with health mandates.
What You Should Know About This Form
What is the Hospital Discharge Papers form?
The Hospital Discharge Papers is a form that healthcare providers must complete when discharging a patient with infectious tuberculosis (TB) from a hospital. It is submitted to the New York City Department of Health & Mental Hygiene to obtain approval for discharge. The form gathers essential information about the patient, their treatment, and follow-up care, ensuring a safe transition from hospital to home or another facility.
Who needs to complete this form?
This form must be completed by healthcare providers in charge of the patient's care. This typically includes doctors and hospital staff who are responsible for the discharge process. It is essential to ensure all sections are filled accurately to avoid any delays in discharge approval.
What information is required in the form?
The form requires various details, including patient contact information, discharge information, follow-up appointment details, laboratory results, and treatment information. Personal identifiers such as the patient's name, date of birth, and discharge destination must be included. Accurate records of TB treatments and any potential barriers to therapy adherence must also be submitted.
How long before discharge should the form be submitted?
The form must be submitted at least 72 hours prior to the anticipated discharge date. This allows the Department of Health sufficient time to review and approve the discharge or request any additional information as needed.
What if I want to discharge a patient on a weekend or holiday?
For weekend or holiday discharges, it is crucial to arrange everything in advance. The discharge plan should be prepared ahead of time and submitted to the Bureau of Tuberculosis Control during regular business hours to facilitate timely processing. Inadequate preparation may prevent discharge from occurring on those days.
What happens after the form is submitted?
After submission, the Bureau of Tuberculosis Control reviews the discharge plan and notifies the provider of approval or any additional information required. This feedback typically occurs within 24 hours for weekday submissions.
Are there specific follow-up care requirements for discharged patients?
Yes, the form requires information about follow-up appointments with another healthcare provider. Ensuring the patient has a scheduled visit is vital for their continued care and monitoring of TB treatment adherence. Additionally, potential barriers to following this treatment plan should be noted on the form.
What should I do if I have questions about the form?
If you have questions regarding the completion of the Hospital Discharge Papers, contact 311 and request to speak with a physician from the Bureau of Tuberculosis Control. They can provide assistance and clarify any confusion regarding the form and its requirements.
Is this form sufficient for reporting TB cases?
No, the Hospital Discharge Papers does not replace the required communicable disease case reports. Healthcare providers must still report all suspected or confirmed TB cases to the Health Department via Reporting Central. Specific guidelines for this reporting can be found on the New York City Department of Health's website.
Common mistakes
Filling out the Hospital Discharge Papers form accurately is crucial for ensuring patient continuity of care. However, common mistakes can lead to delays in discharge or complications in patient management.
One frequent error is incomplete patient contact information. Individuals often omit crucial details, such as the full address or accurate phone numbers. Providing complete and verified information is essential for effective communication after discharge.
Another common mistake involves incorrect discharge information. This includes failing to specify the correct discharging facility or not including the medical record number. Any discrepancies in this section can hinder follow-up care or lead to miscommunication among healthcare teams.
Omitting the planned discharge date is also an issue. Missing this deadline can lead to administrative delays, impacting patient readiness for transition to other care settings. Ensuring that all dates are filled in completely is vital for a seamless discharge process.
Another area for potential errors is the decision of discharge location. It is important to accurately indicate whether the patient is going home or to another facility. Not specifying this can lead to misunderstandings regarding the patient’s post-discharge environment.
Failing to schedule a follow-up appointment is another oversight that can jeopardize patient care. The follow-up appointment date must be recorded clearly, along with the physician's details who will take over care. Missing this information can interfere with essential ongoing treatment.
In the section for laboratory results, people often forget to include all three recent AFB smear results. Each result should include the specimen source and a clear indication of whether it was positive or negative. Neglected details can obscure a patient’s current TB status.
Regarding treatment, it is vital to indicate whether there was an interruption in therapy. Not specifying the reason for the interruption can lead to confusion and negates the patient's treatment history. This section must be completed carefully to communicate the patient’s adherence to therapy.
Dosages of TB medications frequently contain errors. Individuals may forget to list dosages or mistakenly check boxes without providing the corresponding information. This oversight can significantly affect the treatment plan and medication management.
Lastly, neglecting to have the form signed by the responsible physician is another critical mistake. Without proper authorization, the discharge paperwork becomes invalid. It is essential to ensure that the physician completes all required sections and signs the document before submission.
Documents used along the form
The Hospital Discharge Papers form is essential for ensuring a smooth transition from hospital to home or another facility. This paperwork conveys vital information necessary for further patient care and ongoing treatment. Alongside the Hospital Discharge Papers, several additional documents may be required to facilitate a comprehensive discharge process. Below is a list of common forms that are often associated with this procedure.
- Patient Transfer Form: This document provides details about the transfer of a patient from one healthcare facility to another. It includes the patient's medical background and current condition, ensuring continuity of care.
- Follow-Up Care Plan: Designed to outline the next steps in a patient's care, this plan may specify follow-up appointments, medications, and other essential recommendations to support recovery.
- Medication Reconciliation Form: This form lists all medications the patient is taking, including dosages. It helps prevent errors and ensures that the patient understands their medication regimen post-discharge.
- Consent for Release of Information: Patients often need to sign this form, allowing their medical information to be shared with other healthcare providers or facilities involved in their ongoing care.
- Home Care Assessment Form: If the patient requires home healthcare services, this document evaluates their needs for at-home support, including nursing and therapy services.
- Emergency Contact Information Form: This simple form collects information about individuals who should be contacted in case of an emergency post-discharge, ensuring the patient has a support system in place.
While the discharge process may seem complex, each form serves a significant purpose in facilitating proper care. Understanding the role of these documents can ensure a more seamless transition, allowing patients to focus on their recovery with peace of mind.
Similar forms
- Patient Admission Form: Similar to the Hospital Discharge Papers, the Patient Admission Form collects essential information about the patient's background and medical history at the time of their entry into the healthcare facility. This form includes personal contact details, medical history, and the purpose of the admission.
- Medical History Form: This document is used to compile comprehensive information about the patient's past health conditions, surgeries, and medications. Like the Hospital Discharge Papers, it is critical for ensuring the continuity of care, allowing healthcare providers to make informed decisions during treatment.
- Treatment Plan: A Treatment Plan outlines the approach for the patient’s care during their hospitalization. This document parallels the Hospital Discharge Papers as both serve to provide critical information about the patient's medical treatment and planned procedures, ensuring a safe transition to post-discharge care.
- Follow-Up Care Instructions: Following discharge, patients receive written instructions about their follow-up care, medications, and any necessary lifestyle changes. This document is similar to the Hospital Discharge Papers, as it emphasizes ongoing treatment and potential barriers to adherence, helping to ensure patient safety and health outcomes.
- Referral Form: A Referral Form is utilized when a patient needs to see a specialist after discharge. This document shares important medical information, much like the Hospital Discharge Papers, to ensure the specialist is informed and prepared for the patient's specific needs.
Dos and Don'ts
When filling out the Hospital Discharge Papers form, it's essential to approach the task with care to ensure that all necessary information is included accurately. Here is a list of guidelines on what you should and shouldn't do:
- Do provide complete patient contact information. Ensure you include the patient’s full name, date of birth, correct address, and emergency contact details.
- Do submit the form at least 72 hours prior to discharge. This ensures the Department of Health has adequate time to review the information and approve the discharge.
- Do check for any potential barriers to therapy adherence. Identifying issues such as homelessness or substance use helps in planning proper follow-up care.
- Do verify all phone numbers and addresses. Double-checking this information minimizes errors and avoids delays in the discharge process.
- Don't leave sections of the form blank. Incomplete forms can lead to rejection or delays in processing.
- Don't forget to include the physician's details. Ensure that the responsible physician's name, license number, and signature are correctly filled out.
- Don't submit the form without confirming all entries. Review the form for spelling errors, inaccurate dates, or missing information before faxing it to the Department of Health.
- Don't assume verbal communication is enough. Always fax the completed discharge papers as required, even if you’ve discussed the discharge with health officials.
Misconceptions
Understanding the Hospital Discharge Papers is crucial for patients and healthcare providers. However, several misconceptions can lead to confusion. The following are common misunderstandings regarding the Hospital Discharge Approval Request Form (TB 354):
- Discharge Papers are Optional: Some individuals believe that submitting discharge papers is optional. In reality, the submission of these forms is required by the New York City Health Code for patients with infectious tuberculosis.
- Doctors Handle Everything: Patients may think their doctors will take care of all paperwork. However, patients should ensure that their healthcare provider submits the discharge request at least 72 hours prior to discharge.
- All Patients are Discharged Immediately: There is a misconception that once a patient is ready, they will be discharged immediately. Approval is needed, and this can take up to 24 hours for review unless submitted during weekends or holidays.
- Discharge to Any Location is Allowed: Some patients may believe they can be discharged to any address. The form requires specific details on the discharge location, and only certain types of facilities are permitted.
- Follow-Up Appointments are Not Important: Many people view follow-up appointments as a suggestion. They are vital for continued care, and their scheduling must be documented in the discharge papers.
- Discharge Papers are for the Hospital's Convenience: Some may think the paperwork benefits the hospital alone. These forms protect patient health by ensuring adequate follow-up and treatment plans for tuberculosis.
- Delay in Discharge is a Hospital Error: Patients often feel frustrated when discharge is delayed. Yet, these delays can be due to the necessary process of obtaining approval from the Department of Health.
Awareness of these misconceptions can enhance understanding of the Hospital Discharge Approval Request Form and improve communication between patients and healthcare providers. Addressing and clarifying these points fosters a supportive discharge process.
Key takeaways
Key Takeaways for Hospital Discharge Papers
- Fill out the form completely before submission. Incomplete forms can delay discharge approval.
- Submit the Hospital Discharge Approval Request Form at least 72 hours before the planned discharge date.
- For weekday discharges, fax the form to the Bureau of TB Control between 8 AM and 5 PM.
- Expect to receive approval or requests for additional information within 24 hours of submission.
- For weekend or holiday discharges, plan and submit your discharge paperwork well in advance.
- Provide accurate patient contact details, including emergency contact information.
- Clearly state any potential barriers to TB therapy adherence on the form.
- Remember that the discharge approval request does not replace the requirement for reporting TB cases to the Health Department.
Browse Other Templates
Mi Tierra Coffee - Indicate if you graduated from high school or college.
California Health Insurance Penalty Exemptions - The form covers exemptions for income levels below the filing threshold.
California Initial Statement of Information - Failure to file this statement on time results in a penalty of $250.