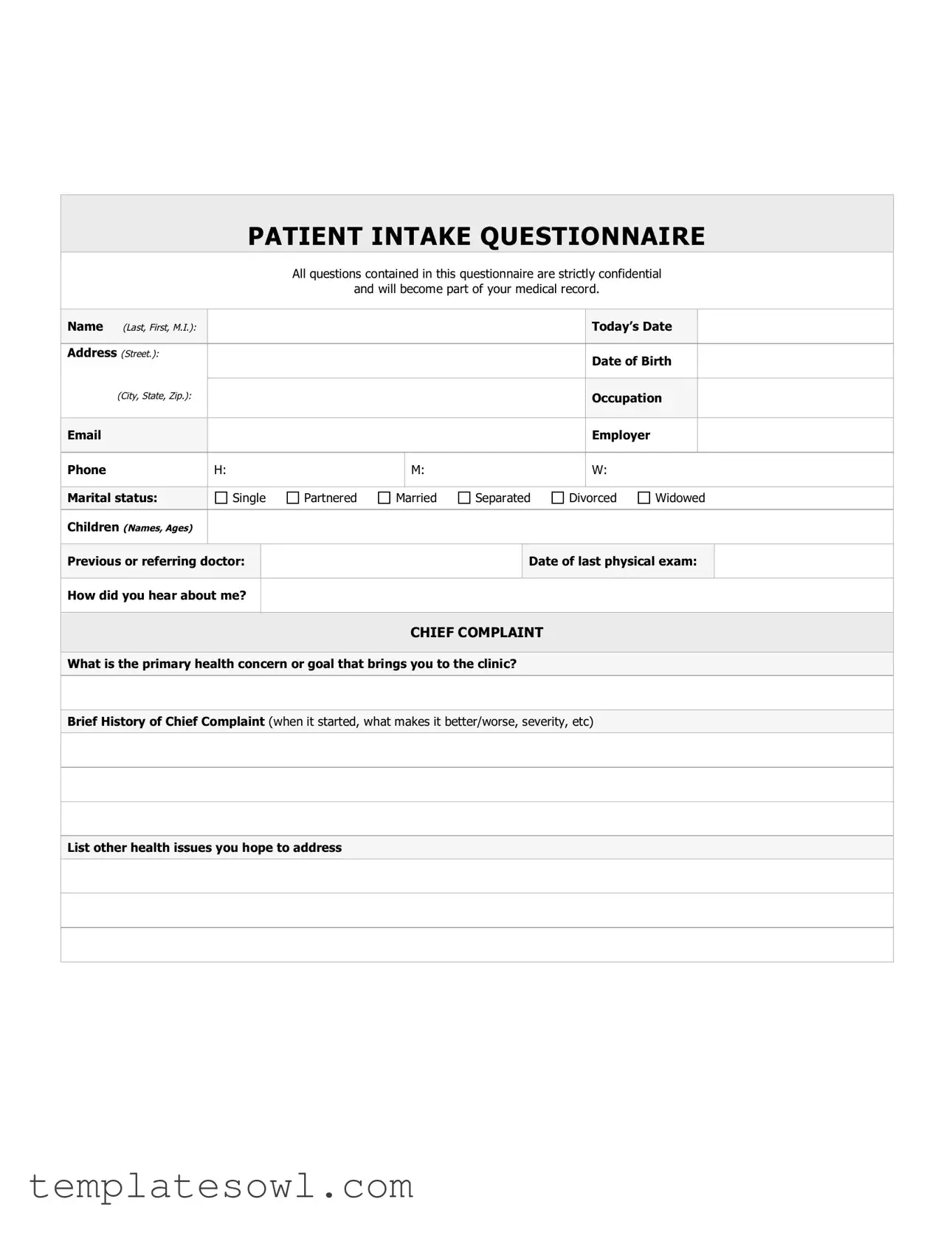
Fill Out Your Hospital Intake Sheet Form
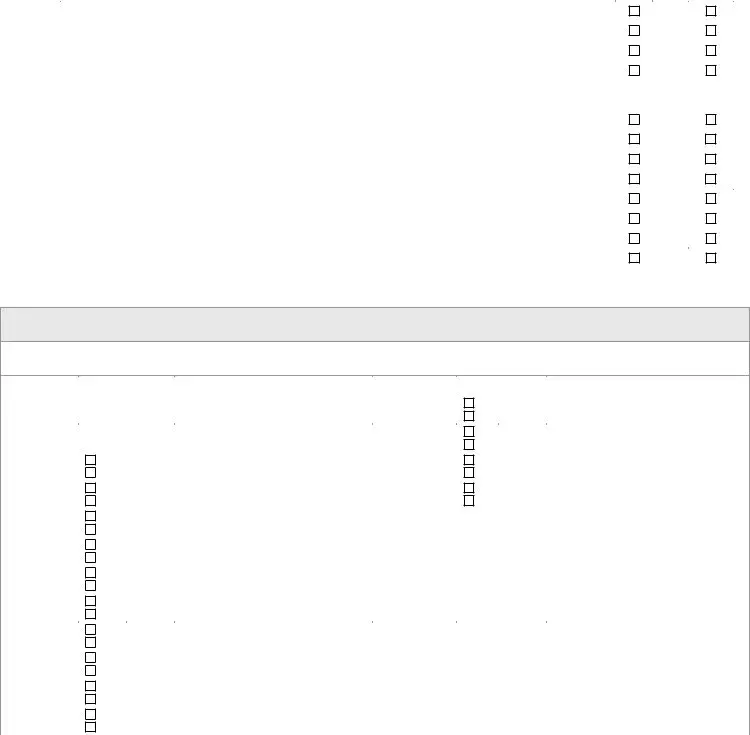
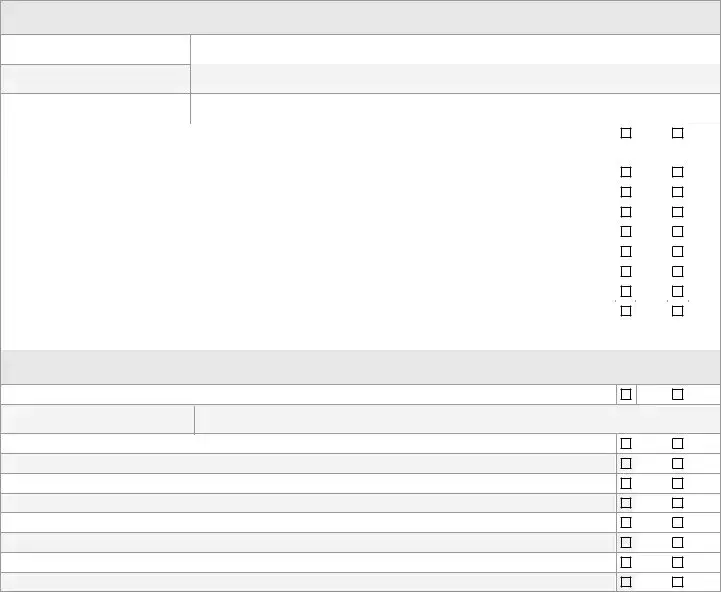
The Hospital Intake Sheet is an essential document used by medical facilities to gather crucial information about a patient before they receive care. Capturing a range of details, this form assists healthcare providers in understanding a patient’s medical background and current health concerns. Patients fill out personal information such as their name, address, and contact details, alongside their date of birth and occupation. The form also prompts patients to indicate their marital status and any children they may have, offering a holistic view of their personal life. The chief complaint section allows patients to articulate the main health issue driving them to seek treatment, and the brief history of this complaint enables providers to better assess the situation. Furthermore, the personal health history section includes crucial data about past medical conditions, surgeries, and current medications, ensuring that healthcare providers have a complete picture of the patient's health. Health habits and personal safety inquiries shed light on lifestyle choices, including exercise routines, diet, and substance use, all of which can impact health outcomes. Family health history, especially for deceased relatives, provides insights into genetic predispositions. For women and men, there are sections tailored to gather specific health information, including reproductive health. This comprehensive approach ensures that the patient's medical record reflects a detailed and accurate account of their health history, thus allowing for more informed and effective care.
Hospital Intake Sheet Example
|
|
|
PATIENT INTAKE QUESTIONNAIRE |
|||||||||||||
|
|
|
|
|
All questions contained in this questionnaire are strictly confidential |
|||||||||||
|
|
|
|
|
and will become part of your medical record. |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Name (Last, First, M.I.): |
|
|
|
|
|
|
|
|
|
|
Today’s Date |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Address (Street.): |
|
|
|
|
|
|
|
|
Date of Birth |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
(City, State, Zip.): |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
Occupation |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Employer |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Phone |
H: |
|
|
M: |
|
|
|
W: |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Marital status: |
|
Single |
Partnered |
Married |
Separated |
Divorced |
Widowed |
||||||||
Children (Names, Ages) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
||||||||
|
Previous or referring doctor: |
|
|
|
|
|
Date of last physical exam: |
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How did you hear about me? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
CHIEF COMPLAINT |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the primary health concern or goal that brings you to the clinic? |
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||||||
|
Brief History of Chief Complaint (when it started, what makes it better/worse, severity, etc) |
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
List other health issues you hope to address |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
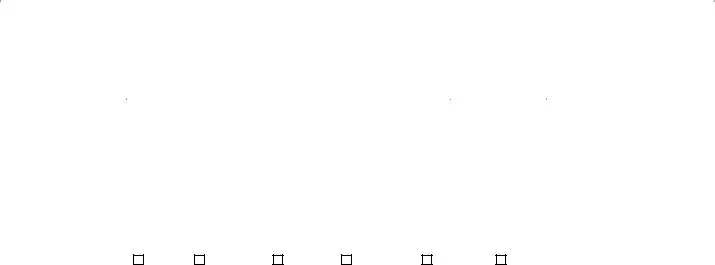
PERSONAL HEALTH HISTORY
List any other medical problems that other doctors have diagnosed
Surgeries
Year |
Reason |
|
|
Hospital
Other hospitalizations
Year |
Reason |
Hospital |
|
Have you ever had a blood transfusion? |
|
Yes |
|
No |
|
|
|
|
|
|
|
|
|
List your prescribed drugs and |
|
|
|
|
|
|
|
|
|
|
|
|
Name the Drug
Strength
Frequency Taken
Allergies
Name the Drug |
Reaction You Had |
|
|
|
|
|
|
Any Other Allergies |
|
|
|
|
|
HEALTH HABITS AND PERSONAL SAFETY
ALL QUESTIONS CONTAINED IN THIS QUESTIONNAIRE ARE OPTIONAL AND WILL BE KEPT STRICTLY CONFIDENTIAL.
Exercise Describe exercise activities: the frequency, intensity, time and type of activity. For example (twice weekly beginner 1 hour yoga classes)
Activities Describe your interests, hobbies, spiritual practices, things you do to relax
Diet |
Are you dieting? |
|
Yes |
|
No |
|
If yes, are you on a physician prescribed medical diet? |
|
Yes |
|
No |
|
|
|
|
|
|
#of meals you eat in an average day? What Have you eaten in the last 24 hours?
If the above dietary recall is atypical for you, describe a typical day here.
List your favorite healthy foods
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Caffeine |
None |
|
Coffee |
|
|
Tea |
|
Cola |
|
|
|
|
|
|
|
|
|
|
Number of cups/cans per day? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Alcohol |
Do you drink alcohol? |
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
If yes, what kind? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How many drinks per week? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you concerned about the amount you drink? |
|
|
|
|
Yes |
|
No |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Have you considered stopping? |
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
Have you ever experienced blackouts? |
|
|
|
|
|
|
|
Yes |
|
No |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Are you prone to “binge” drinking? |
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
||
|
Do you drive after drinking? |
|
|
|
|
|
|
|
|
Yes |
|
No |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
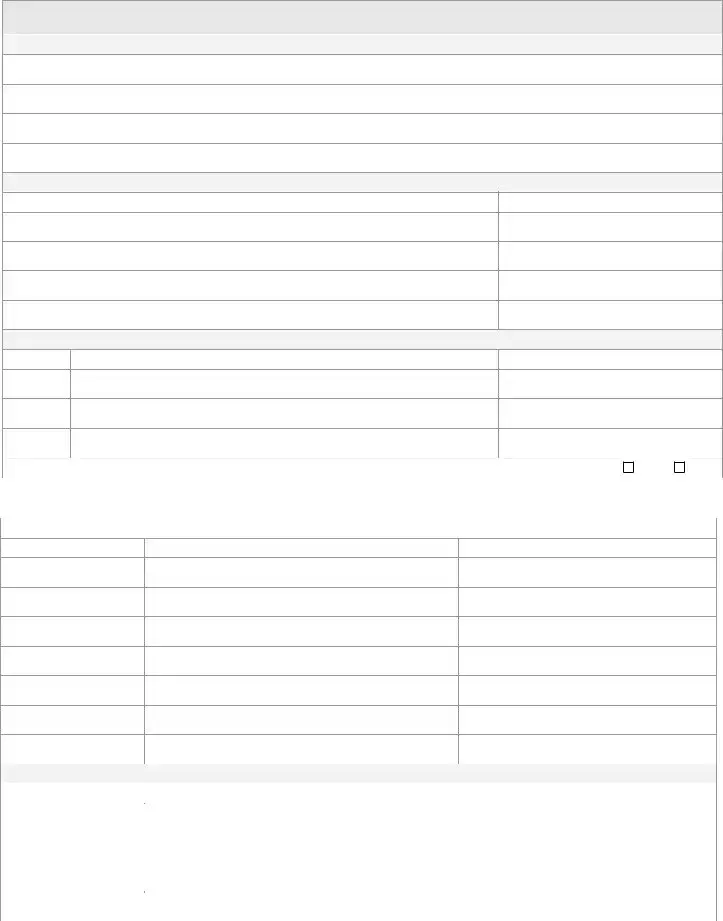
Tobacco |
Do you use tobacco? |
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
No |
|
|
|
Cigarettes – pks./day: |
|
Chew - #/day: |
Pipe - #/day: |
|
Cigars - #/day: |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
# of years: |
|
Or year quit: |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Drugs |
Do you currently use recreational or street drugs? |
|
Yes |
|
No |
||
|
|
|
|
|
|
|
|
|
Have you ever given yourself street drugs with a needle? |
|
Yes |
|
|
No |
|
Sex |
Are you sexually active? |
|
Yes |
|
No |
||
|
If yes, are you trying for a pregnancy? |
|
Yes |
|
|
No |
|
|
If not trying for a pregnancy list contraceptive or barrier method used: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Any discomfort with intercourse? |
|
Yes |
|
|
No |
|
Personal |
Do you live alone |
|
Yes |
|
|
No |
|
Safety |
|
|
|
|
|
|
|
Do you have traction stickers or bathtub mat? |
|
Yes |
|
|
No |
||
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
Do you have a fire extinguisher? |
|
Yes |
|
|
No |
|
|
Do you have frequent falls? |
|
Yes |
|
No |
||
|
|
|
|
|
|
||
|
Do you have vision or hearing loss? |
|
Yes |
|
|
No |
|
|
Do you have an Advance Directive or Living Will? |
|
Yes |
|
No |
||
|
|
|
|
|
|
||
|
Do you wear a seatbelt? |
|
Yes |
|
|
No |
|
|
|
|
|
|
|
|
|
FAMILY HEALTH HISTORY
FOR DECEASED RELATIVES MARK A LETTER “D” AND THEIR AGE AT DEATH, SPECIFY CAUSE OF DEATH IF KNOWN
|
AGE |
SIGNIFICANT HEALTH PROBLEMS |
|
AGE |
SIGNIFICANT HEALTH PROBLEMS |
||
|
|
|
|
|
|
|
|
Father |
|
|
|
Children |
M |
|
|
|
|
|
F |
|
|
||
|
|
|
|
|
|
|
|
Mother |
|
|
|
|
M |
|
|
|
|
|
|
F |
|
|
|
|
|
|
|
|
|
|
|
Sibling(s) |
M |
|
|
|
M |
|
|
F |
|
|
|
F |
|
|
|
|
|
|
|
|
|
||
|
M |
|
|
|
M |
|
|
|
F |
|
|
|
F |
|
|
|
M |
|
|
|
|
|
|
|
F |
|
|
Grandmother |
|
|
|
|
M |
|
|
Maternal |
|
|
|
|
F |
|
|
|
|
|
|
|
M |
|
|
|
|
|
|
|
F |
|
|
Grandfather |
|
|
|
|
M |
|
|
Maternal |
|
|
|
|
F |
|
|
|
|
|
|
|
M |
|
|
|
|
|
|
|
F |
|
|
Grandmother |
|
|
|
|
M |
|
|
Paternal |
|
|
|
|
F |
|
|
|
|
|
|
|
M |
|
|
|
|
|
|
|
F |
|
|
Grandfather |
|
|
|
|
M |
|
|
Paternal |
|
|
|
|
F |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
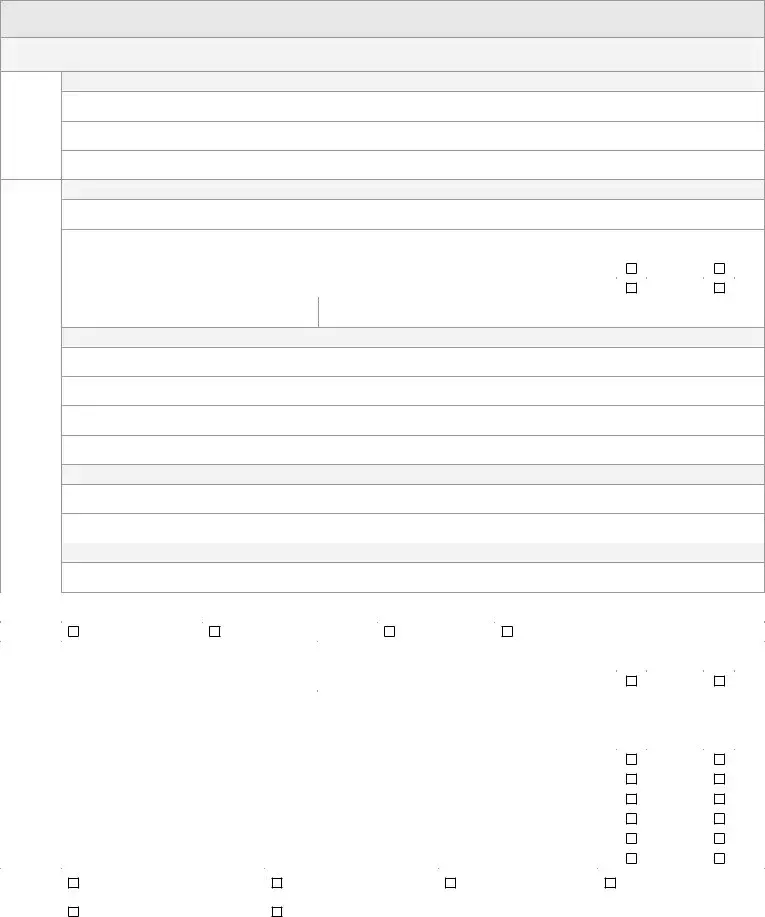
WOMEN ONLY
Age at onset of menstruation:
Date of last menstruation:
Period every how many days?
Heavy periods, irregularity, spotting, pain, or discharge? |
|
|
|
Yes |
|
No |
||
Number of pregnancies: |
|
|
Number of live births: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you pregnant or breastfeeding? |
|
|
|
Yes |
|
No |
||
Have you had a D&C, hysterectomy, or Cesarean? |
|
|
|
Yes |
|
No |
||
|
|
|
|
|
|
|
|
|
Any urinary tract, bladder, or kidney infections within the last year? |
|
|
|
Yes |
|
No |
||
Any blood in your urine? |
|
|
|
Yes |
|
No |
||
|
|
|
|
|
|
|
|
|
Any problems with control of urination? |
|
|
|
Yes |
|
No |
||
Any hot flashes or sweating at night? |
|
|
|
Yes |
|
No |
||
|
|
|
|
|
|
|||
Do you have menstrual tension, pain, bloating, irritability, or other symptoms at or around time of period? |
|
Yes |
|
No |
||||
Experienced any recent breast tenderness, lumps, or nipple discharge? |
|
|
|
Yes |
|
No |
||
|
|
|
|
|
|
|
|
|
Date of last pap? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MEN ONLY
Do you usually get up to urinate during the night?
If yes, # of times:
Do you feel pain or burning with urination?
Any blood in your urine?
Do you feel burning discharge from penis?
Has the force of your urination decreased?
Have you had any kidney, bladder, or prostate infections within the last 12 months?
Do you have any problems emptying your bladder completely?
Any difficulty with erection or ejaculation?
Any testicle pain or swelling?
|
Yes |
|
No |
|
Yes |
|
No |
|
|
||
|
|
|
|
|
Yes |
|
No |
|
Yes |
|
No |
|
|
|
|
|
Yes |
|
No |
|
Yes |
|
No |
|
|
|
|
|
Yes |
|
No |
|
Yes |
|
No |
|
|
|
|
|
Yes |
|
No |
|
|
|
|
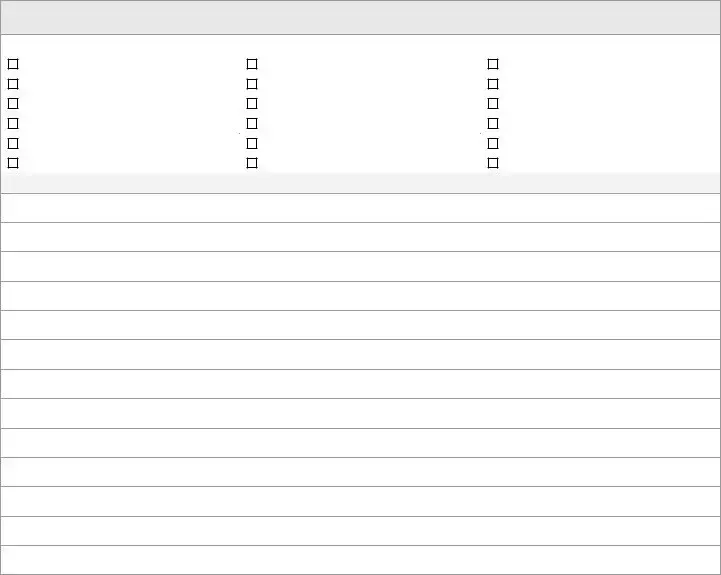
OTHER PROBLEMS
Check if you have, or have had, any symptoms in the following areas to a significant degree and briefly explain in the space below.
Skin |
Chest/Heart |
Recent changes in: |
Head/Neck |
Back |
Weight |
|
|
|
Ears |
Intestinal |
Energy level |
Nose |
Bladder |
Ability to sleep |
|
|
|
Throat |
Bowel |
Other pain/discomfort: |
Lungs |
Circulation |
Other odd symptom |
|
|
|
Use this space to elaborate on the above chart or for anything else you would like to add not addressed in this form.
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | The Hospital Intake Sheet gathers essential information from patients to create a comprehensive medical record. |
| Confidentiality | All information provided in the questionnaire is confidential and will be protected as part of the patient's medical record. |
| Patient Identification | Includes personal details such as name, date of birth, address, and contact information. |
| Health Concerns | Patients are asked to state their primary health concern and provide a brief history related to it. |
| Personal Health History | This section collects past medical problems, surgeries, and hospitalizations for better understanding of the patient's health background. |
| Medication List | Patients need to list all prescribed and over-the-counter medications, detailing their names, strengths, and frequencies. |
| Health Habits | Patients are given the option to disclose habits such as diet, exercise, and substance use, promoting holistic care. |
| Family Health History | Information regarding significant health issues of family members helps uncover hereditary conditions. |
| Women’s Health | Specific questions address issues relevant to female patients, including menstrual and pregnancy history. |
| Men’s Health | Similar to women, this section includes questions pertinent to male patients’ urinary and sexual health. |
Guidelines on Utilizing Hospital Intake Sheet
Completing the Hospital Intake Sheet is a crucial step in ensuring that your healthcare provider has all the information needed for your care. After you fill out the form, be prepared to discuss your responses during your appointment. This will help the medical staff better understand your health history and current concerns.
- Patient Information: Fill in your name (last, first, M.I.), today's date, and address (street, city, state, zip).
- Provide your date of birth, occupation, email, employer, and phone numbers (home, mobile, work).
- Indicate your marital status by checking the corresponding box.
- List the names and ages of your children, if any.
- Fill in the name of your previous or referring doctor and the date of your last physical exam.
- Explain how you heard about the clinic.
- Chief Complaint: Describe your primary health concern and provide a brief history, noting when it started and what affects it.
- List any other health issues you would like to address.
- Personal Health History:
What You Should Know About This Form
What is the purpose of the Hospital Intake Sheet form?
The Hospital Intake Sheet form gathers important information about a patient's health history, current medications, personal habits, and family background. This data will help the healthcare provider understand the patient's medical needs, enabling a more tailored and effective treatment plan. All information is kept strictly confidential and becomes part of the patient's medical record.
What types of questions are included on the form?
The form includes various sections, such as personal information, chief complaint, personal health history, health habits, family health history, and specific questions for women and men. Patients provide details about their primary health concern, past medical issues, surgeries, medications, exercise habits, diet, alcohol and tobacco use, safety measures at home, and family health background.
Is the information provided confidential?
Yes, all answers given on the Hospital Intake Sheet are strictly confidential. This means the healthcare provider will not disclose any of the information to outside parties without the patient’s consent. The data provided will only be used for medical purposes and included in the patient's medical record.
Do I have to answer all the questions on the form?
No, responding to questions in the Hospital Intake Sheet is optional for most sections. Patients are encouraged to provide as much information as they feel comfortable sharing, as this will assist healthcare providers in delivering the best possible care.
Can I request to see my completed Hospital Intake Sheet?
Absolutely. Patients have the right to request and review their completed Hospital Intake Sheet form. It is part of their medical record, and they can discuss any of the information with their healthcare provider to understand how it impacts their treatment options.
What happens after I submit the Hospital Intake Sheet form?
Once the form is submitted, the healthcare provider will review the information to assess the patient's health needs. This review helps guide the initial consultation and subsequent treatment decisions. Patients may be contacted for additional information or clarification if needed.
Common mistakes
Filling out a Hospital Intake Sheet can seem straightforward, yet many individuals make mistakes that can hinder their medical care. One common mistake is failing to provide complete contact information. This information is crucial for hospitals to follow up on appointments or reach out in case of medical emergencies. Omitting phone numbers or providing incorrect details can create significant communication gaps.
Another frequent error is not disclosing all medications. Patients often forget to list over-the-counter drugs or supplements. This oversight can lead to dangerous interactions with prescribed medications. It is always vital to mention every substance that is taken regularly.
Additionally, individuals sometimes leave the chief complaint section vague. Clearly articulating the primary health concern helps medical staff understand the urgency and focus of care required. A detailed description, including when the issue started and any aggravating factors, enhances the ability of healthcare providers to assist effectively.
The section regarding personal health history is also commonly mishandled. Many people underestimate the importance of past surgeries or hospitalizations. Each patient's medical history is unique, and previous conditions might influence current health strategies. Missing this information can mislead healthcare providers about a patient's overall health status.
People might also misrepresent their dietary habits. Entering inaccurate information about meals and alcohol consumption can distort health assessments. Being honest about one's diet allows healthcare professionals to recommend appropriate dietary changes or interventions.
Some patients do not discuss family health history in depth. This section is critical for identifying potential hereditary issues. All relevant information about family medical conditions, especially those that are significant, should be included.
Lastly, many fail to address personal safety measures. For instance, not indicating whether they have a fire extinguisher or traction stickers in the bathroom can present risks. Highlighting safety measures can help healthcare providers recommend lifestyle changes to enhance patient safety.
Documents used along the form
The Hospital Intake Sheet is essential for capturing a patient's comprehensive medical history and health concerns upon their first visit to a clinic. However, it often accompanies several other forms that gather additional information necessary for effective healthcare delivery. Below is a concise description of five commonly used forms alongside the Hospital Intake Sheet.
- Consent to Treatment Form: This document indicates that a patient grants permission for healthcare providers to administer medical treatment. It clarifies the scope of care and ensures that patients understand what services they will receive.
- Insurance Information Form: This form collects details about the patient's health insurance coverage. It includes information such as the provider's name, policy number, and any copayments required, which facilitates billing and manages payment processes for medical services.
- Medical Release Form: Patients often complete this form if they wish to allow healthcare providers to share their medical information with another physician or institution. It explicitly states what information can be shared and which parties are authorized to receive it.
- Patient Health History Form: This document gathers more detailed information about the patient's past medical history, family health history, and current medications. It serves to paint a fuller picture of the patient's health, making it easier for providers to diagnose and treat them accurately.
- Emergency Contact Form: In case of a medical emergency, this form specifies whom to contact. Including names, relationship status, and phone numbers of emergency contacts ensures timely communication with family or friends should urgent situations arise.
Collectively, these forms not only enhance the quality of healthcare services but also foster a transparent relationship between patients and healthcare professionals. By ensuring that all pertinent information is available, healthcare providers can deliver more tailored and efficient care.
Similar forms
The Hospital Intake Sheet is a critical document used to gather essential information from patients at the time of their admission. It serves as a comprehensive overview of a patient's health history and current concerns. Below are eight documents similar to the Hospital Intake Sheet, each serving a unique purpose while addressing patient information and medical history.
- New Patient Registration Form: This form collects basic information about the patient such as name, contact details, insurance information, and emergency contacts, providing an initial overview of the patient’s background.
- Medical History Questionnaire: Similar in nature, this document delves deeper into a patient's previous medical conditions, treatments, surgeries, and allergies, forming a more detailed medical profile.
- Vineland Adaptive Behavior Scales: While focused on specific developmental and behavioral issues, this document gathers crucial information about a patient’s functional capabilities, which complements personal and health history.
- Patient Referral Form: Used in cases where a patient is referred to a specialist, this form includes details about the referring physician's observations and the specific reasons for the referral, much like the chief complaint section in the Intake Sheet.
- Medication Reconciliation Form: This document ensures accurate medication information by capturing details about current medications, dosages, and administration frequency, paralleling the medication section of the Intake Sheet.
- Consent for Treatment Form: This form requires patients to acknowledge their understanding and consent to receive medical services. It is similar in that it addresses patient autonomy and health-related decision-making.
- Insurance Information Form: While primarily focused on insurance details, it shares the purpose of collecting vital information necessary for patient processing and billing, akin to the financial aspects included in a broader Intake Sheet.
- Advance Directive Form: This document allows patients to express their healthcare wishes in advance. Similar to the Intake Sheet, it emphasizes the importance of understanding patient preferences in medical care.
Dos and Don'ts
When filling out the Hospital Intake Sheet form, it's helpful to keep a few things in mind. Consider the following dos and don'ts:
- Do: Provide accurate personal information, including your full name and contact details.
- Do: List all current medications, both prescribed and over-the-counter.
- Do: Be honest about your medical history and any health concerns.
- Do: Take your time to thoroughly complete each section of the form.
- Do: Inform your healthcare provider about any allergies you have.
- Don't: Skip questions thinking they are unimportant; each question serves a purpose.
- Don't: Provide vague answers; specificity helps your healthcare provider.
- Don't: Leave the form incomplete; ensure all sections are filled out as best as you can.
- Don't: Feel embarrassed about any health issues; confidentiality is maintained.
Misconceptions
Misconceptions about the Hospital Intake Sheet can lead to confusion and concerns among patients. Here are seven common misconceptions clarified:
- All information is shared publicly. Many patients worry that their information may be shared outside of healthcare settings. In reality, all answers provided in the questionnaire are strictly confidential and become part of the patient's medical record.
- The questions are mandatory for all patients. Some patients believe that they must answer every question. However, many questions are optional. Patients can choose not to disclose information that they are uncomfortable sharing.
- Only medical history is relevant. The misconception exists that only past medical issues matter in the intake form. In truth, lifestyle choices, familial health history, and current health habits are equally important for providing comprehensive care.
- Completing the form takes a long time. Some individuals assume that filling out the hospital intake sheet is a lengthy endeavor. While the form may seem extensive, it can often be completed in a relatively short period, especially with preparation.
- The intake sheet is only for new patients. Patients may think that only new patients need to fill out an intake form. However, existing patients may need to update their information during visits to ensure that their health records remain accurate and up to date.
- Your responses could lead to immediate treatment decisions. Some fear that disclosing certain health habits or conditions will result in immediate action or consequences. Healthcare professionals use this information for a better understanding of overall health and to plan future care rather than making instant decisions.
- The information is not critically assessed. There is a misconception that the intake sheet is merely a formality. In truth, healthcare providers carefully review this information to tailor treatments and make informed decisions regarding patient care.
Key takeaways
When filling out the Hospital Intake Sheet form, keep these key points in mind:
- Confidentiality Matters: All information provided is confidential and will be part of your medical record. Be honest to ensure the best care.
- Complete Personal Details: Fill in your name, address, and contact information accurately. This helps the clinic reach you if needed.
- Primary Health Concerns: Clearly state your chief complaint. This is crucial for the provider to understand why you’re visiting.
- Thorough Health History: Include all past and current medical issues and medications. This helps in creating a complete health profile.
- Answer Optional Sections: Questions about lifestyle and habits are optional but can provide valuable insights into your overall health.
- Family Medical History: Share details about relatives’ health. This information can highlight potential genetic health risks.
- Be Honest About Habits: Whether it’s regarding diet, exercise, or substance use, transparency allows for better guidance and care from health professionals.
Browse Other Templates
1046 Form - Mandatory fields include personal and employment details for processing.
Computershare Investor Center - The new account type must be specified for successful transfer completion.