Fill Out Your Icu Flowsheet Form
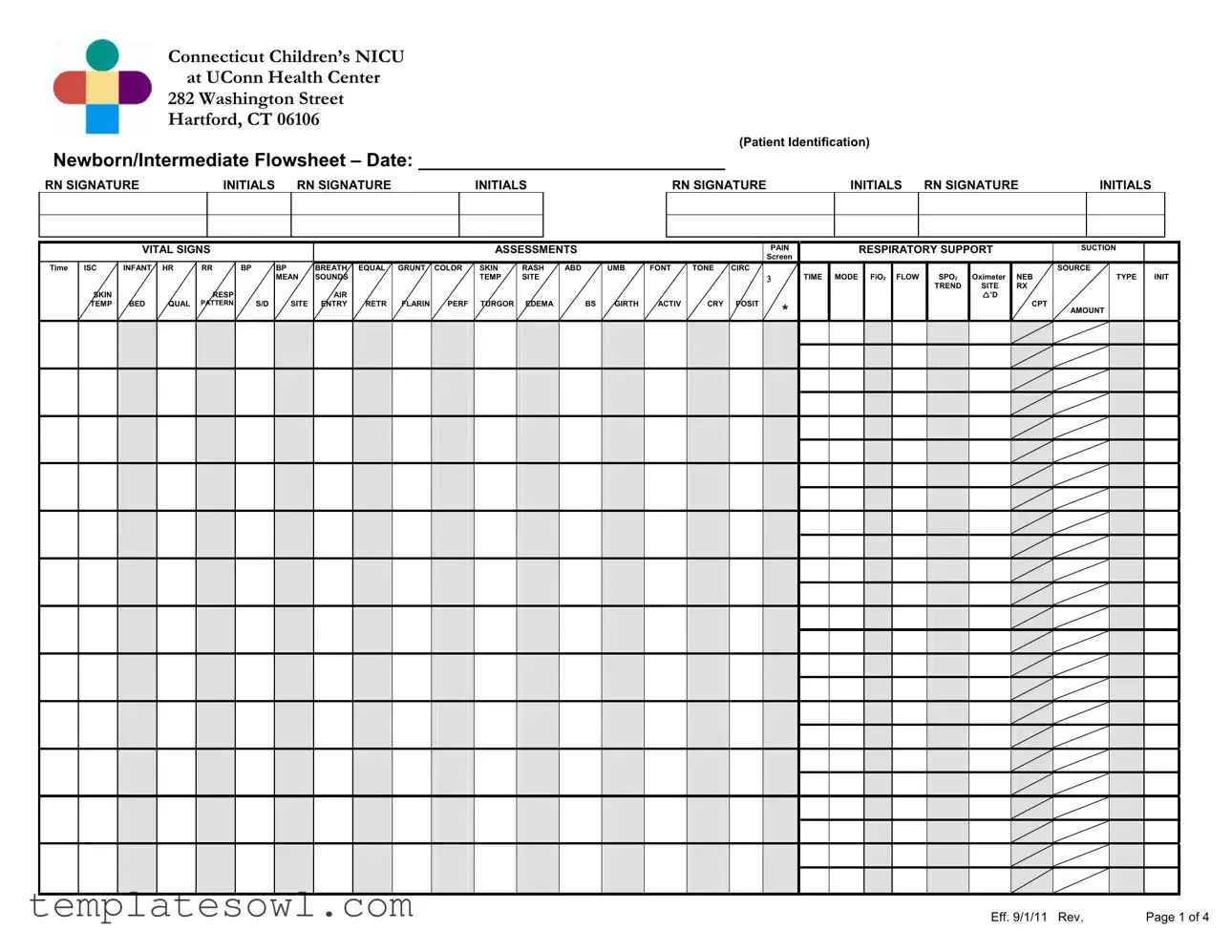
The ICU Flowsheet form is an essential document used in the neonatal intensive care unit (NICU) at Connecticut Children’s NICU, located at the UConn Health Center. This comprehensive form is meticulously designed to track a wide array of critical patient information related to newborns and intermediate care. It captures vital signs such as heart rate, respiratory rate, blood pressure, and temperature, ensuring healthcare providers can continuously monitor the physical status of each infant. In addition to vital signs, the form provides sections for recording assessments, addressing pain management, respiratory support, and suction needs. The form includes protocols for developmental assessments, guidelines for feeding, and protocols for various therapeutic interventions like phototherapy and IV therapy. Furthermore, a significant feature of the flowsheet is the shift safety section, which emphasizes the importance of alarms, equipment setup, and hygiene practices to ensure a safe patient environment. Acknowledging the crucial role of parent communication, the form also includes records for family education, weight tracking, and blood gas results, all fundamental for informed decision-making in patient care.
Icu Flowsheet Example
Connecticut Children’s NICU
at UConn Health Center
282 Washington Street
Hartford, CT 06106
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Patient Identification) |
|
|
|
|
|
|
|
|
|
|||||||
Newborn/Intermediate Flowsheet – Date: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
RN SIGNATURE |
|
|
INITIALS |
|
RN SIGNATURE |
|
|
|
|
INITIALS |
|
|
|
RN SIGNATURE |
|
|
|
INITIALS |
RN SIGNATURE |
|
INITIALS |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
VITAL SIGNS |
|
|
|
|
|
|
|
|
|
ASSESSMENTS |
|
|
|
|
|
PAIN |
|
|
RESPIRATORY SUPPORT |
|
SUCTION |
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Screen |
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Time |
ISC |
INFANT |
HR |
RR |
BP |
BP |
BREATH |
EQUAL |
GRUNT |
COLOR |
SKIN |
RASH |
ABD |
UMB |
FONT |
TONE |
CIRC |
|
|
|
|
|
|
|
|
|
|
|
SOURCE |
|
|
||||||||
|
|
|
|
|
|
|
MEAN |
SOUNDS |
|
|
|
|
|
TEMP |
SITE |
|
|
|
|
|
|
|
TIME |
MODE |
FiO2 |
FLOW |
|
SPO2 |
Oximeter |
NEB |
|
|
TYPE |
INIT |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TREND |
SITE |
RX |
|
|
|
|
|
|
SKIN |
|
|
|
RESP |
|
|
|
AIR |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
’D |
|
|
|
|
|
|
|
TEMP |
BED |
QUAL |
PATTERN |
S/D |
SITE |
ENTRY |
RETR |
FLARIN |
PERF |
TURGOR |
EDEMA |
BS |
GIRTH |
ACTIV |
CRY |
POSIT |
* |
|
|
|
|
|
|
|
|
|
CPT |
AMOUNT |
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Eff. 9/1/11 Rev. |
Page 1 of 4 |
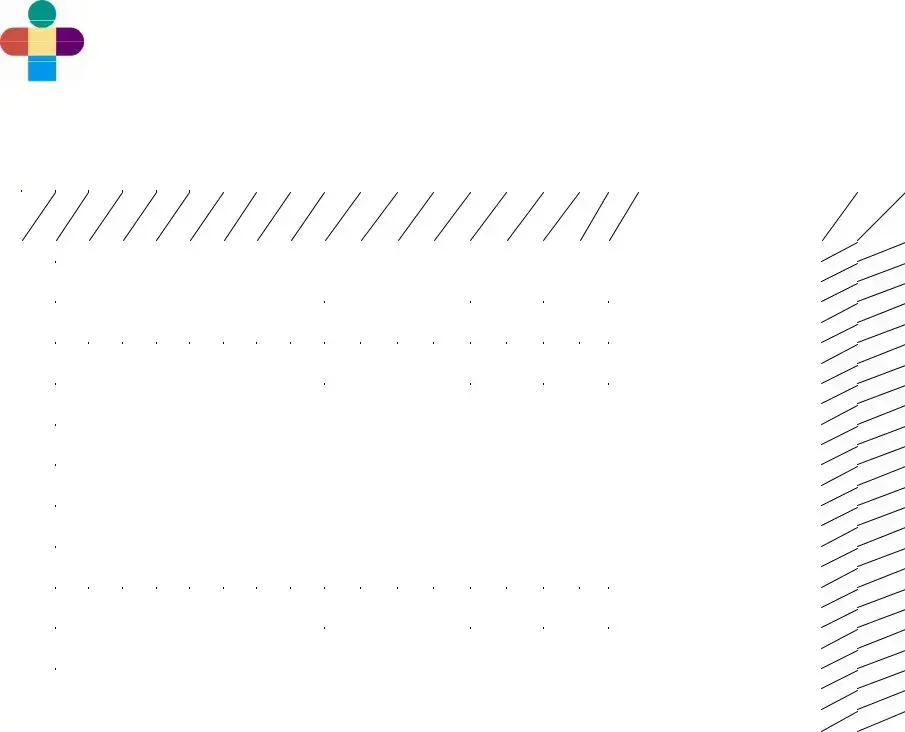
Connecticut Children’s NICU
at UConn Health Center
282 Washington Street
Hartford, CT 06106
(Patient Identification)
Newborn/Intermediate Flowsheet – Date:
Standards of Care |
SHIFT |
Care of the Infant with:
Admission to the Newborn Nursery
Apnea/ Bradycardia /Periodic Breathing
Breastfeeding/Breast Pumping
Bronchodilators
Cardiorespiratory Monitor
Central Lines
Circumcision
Developmental Assessment and Care
Discharge Planning: Neonatal
Feeding: NG/OG/Continuous/Intermittent
GE Reflux
Grieving
Hospitalized Infant: Care of the Family
IV Therapy
Kangaroo Care
Pain Screening and Assessment
Phototherapy/Biliblanket
Pulse Oximetry
Skin Care: Neonatal
Steroids
Supplemental Oxygen
Thermoregulation
Well Newborn
Other:
PATIENT AND FAMILY TEACHING RECORDS:
Family Education of the hospitalized Infant
BPD
Others:
SHIFT
SAFETY:
ALARMS:
HR: HIGH / LOW
RR: HIGH/Apnea > 20 sec.
Pulse Oximetry: Low
Security Sensor On:
EQUIPMENT:
Resuscicard
Bag/Mask & O2 Flow
Suction
ID & Blood Bracelet
Evacuation Pack & ID
PHOTOTHERAPY:
Photo Tx Intensity
Eye Patches
Serum Bili Level
HYGIENE:
Bath/Linens
Cord Care
Circ. Care
Nares Care
Mouth Care
PARENT COMMUNICATION:
WEIGHT: |
KG |
LB |
Birth Weight:
Yesterday:
Today:
Wt change:
Length:OFC:
Corrected Gestational Age:
Mom’s Room #
Care Level:
Physician:
BLOOD GAS RESULTS
Time |
Site |
pH |
pCO2 |
pO2 |
BE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
LAB TESTS/RESULTS
Time |
Site |
Gluc |
HCT |
TESTS AND RESULTS |
|
Meter |
|||||
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
STOOL/URINE RESULTS
COMMENTS:
Eff. 9/1/11 Rev. |
Page 2 of 4 |

Connecticut Children’s NICU
at UConn Health Center
282 Washington Street
Hartford, CT 06106
(Patient Identification)
Newborn/Intermediate Flowsheet – Date:
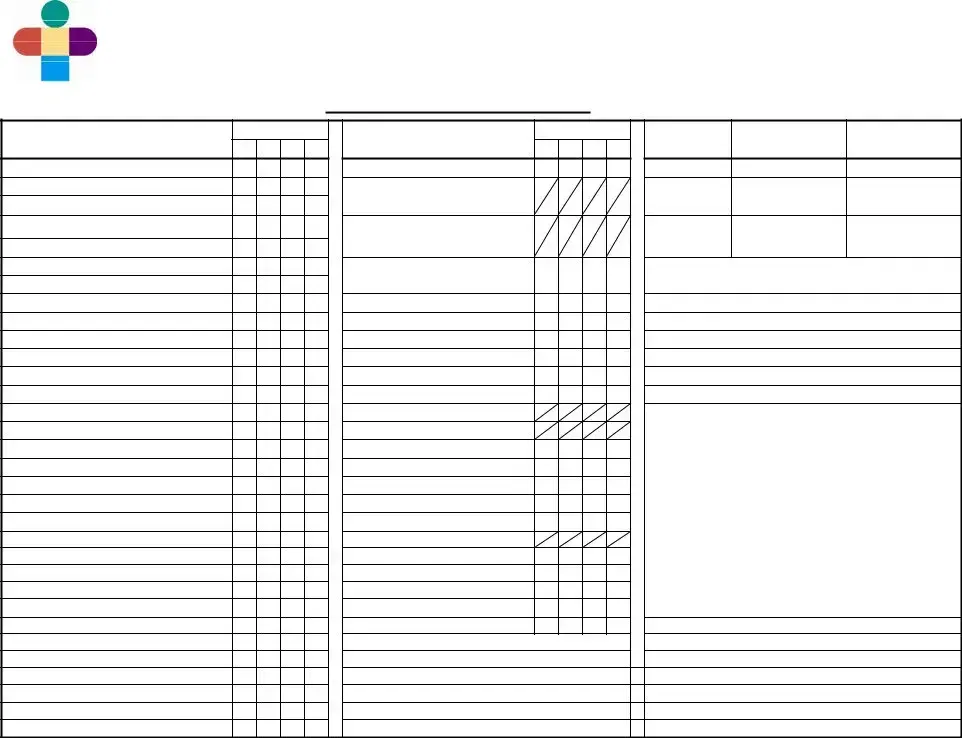
GENERAL
R – Right
L – Left
- Done
-- Absent
+ - Present - Increased - Decreased
‡- Asymmetrical = - Equal
- Changed
BED
I – Isolette
OC – Open Crib
OW – Open Warmer
HR QUALITY
R – Regular
I – Irregular
M – Murmur
RESP. PATTERN
R – Regular
IR – Irregular
S – Shallow
PB – Periodic
Breathing
BP SITE
LA – Left Arm RA – Right Arm
LL– Left Calf RL – Right Calf LT – Left Thigh RT – Right Thigh
BREATH SOUNDS
Cr – Crackles
C – Clear
CO – Coarse
W – Wheeze
S – Stridor
AIR ENTRY
G – Good
L – Limited
T – Tight
EQUALITY
++- Bilaterally RorL - Diminished - Diminished
bilaterally
RETRACTIONS
M – Minimal
MO – Moderate
S – Severe
GRUNTING |
UMBILICAL |
POSITION/MISC |
STOOL COLOR |
ORAL(PO) FEEDING DESCRIPTION |
||
A – Audible w/naked |
CORD |
P - Prone |
M – Meconium |
|
|
|
|
ear |
O - Off |
S – Supine |
Y – Yellow |
BEHAVIOR BEFORE FEEDING |
|
S – Stethescope only |
D - Dry |
R - Rt. Side Down |
G – Green |
1 |
Infant awakens on own signaling |
|
Int - Intermittent |
W - Wet |
L - Lt. Side Down |
B – Brown |
|
hunger with crying or fussing; shows |
|
|
|
Cl - Clamped |
HOB - Head of Bed Up |
FB – FRANK BLOOD |
|
hunger cues (rooting, sucking, |
COLOR |
DG - Drainage |
HOB - Head of Bed |
|
|
searching, hand to mouth). |
|
P - Pink |
R – Erythema |
Down |
CONSISTENCY |
2 Infant awakens on own, may remain |
||
W – Pale |
confined to |
IS – Infant Seat |
S – Soft |
|
quietly alert, drowsy or begin fussing or |
|
D – Dusky |
stump |
SW – Swaddled |
W - Watery |
|
moving, may show some hunger cues |
|
C – Cyanotic |
Rt – Erythema |
SG – Swing |
P – Pasty |
|
(rooting, sucking, searching, hand to |
|
J – Jaundiced |
extended to |
H – Held |
SD – Seedy |
|
mouth). |
|
PL – Plethoric |
abdominal |
|
Mu – Mucous |
3 |
Infant awakens with |
|
M – Mottled |
wall |
OXYGEN MODE |
|
|
begins to show hunger cues (rooting, |
|
A |
|
I – Isolette |
ENTERAL FEEDS |
|
sucking, searching, show hand to |
|
|
|
FONTANELLE |
H – Hood |
MODE |
|
mouth, fussing). |
PERFUSION |
S – Soft, Flat |
NC – Nasal Cannula |
Po – Nipple |
4 |
Infant awakens with |
|
N – CRT < 3 sec. |
F – Full |
MT – Mist tent |
BF – Breastfeeding |
|
appears quietly awake or somewhat |
|
A – CRT > 3 sec. |
T – Tense |
TC – Trach Collar |
CNG – Continuous |
|
drowsy with limited hunger cues |
|
|
|
B – Bulging |
CPT |
Nasogastric |
|
(rooting, sucking, searching, hand to |
SKIN TEMP |
D – Depressed |
P – Percussion |
NG/OG – Gavage |
|
mouth). |
|
W – Warm |
|
V – Vibration |
|
5 |
Infant remains asleep or drowsy. |
|
C – Cool |
ACTIVITY |
|
IV SITE CHECK |
6 |
Infant appears to have limited |
|
H – Hot |
++ - Active, Alert |
SUCTION SOURCE |
W – Warm |
|
physiological stamina required to |
|
D - Diaphoretic |
+ - Active to stim |
O – Oral |
C – Cool |
|
sustain control and endurance for |
|
|
|
L - Lethargic |
N- Nares |
E – Edematous |
|
feeding attempt. |
TURGOR |
S - Sleeping |
|
R – Erythematous |
BEHAVIOR DURING BOTTLE FEEDING |
||
G – Good |
NC - Non- |
SUCTION AMOUNT |
N – |
1 |
Energetic with steady, coordinated |
|
F – Fair |
consolable |
S – Small |
|
|||
P – Poor |
Q – Quiet |
Mo – Moderate |
|
to no in resp. effort or color; easily |
||
C - Crepitus |
|
L – Large |
Bl – Blanched |
|
maintains tone, posture, remains calm |
|
|
|
TONE |
|
|
|
and completes feeding. |
RASH SITE |
N - Normal |
TYPE |
IV LOCATION |
2 |
Initially energetic with steady, |
|
PA – Perianal |
- Hypertonic |
Th – Thin |
RAc – Right Antecubital |
|
coordinated |
|
PN – Perineal |
- Hypotonic |
Tk – Thick |
LAc – Left Antecubital |
|
challenges |
|
G – Generalized |
J - Jittery |
C – Clear |
RF – Right Foot |
|
coordination, in resp. effort, color, |
|
T – Trunk |
C – Clonus |
W – White |
LF – Left Foot |
|
tone, posture or state) with support, is |
|
|
|
|
Y – Yellow |
RH – Right Hand |
|
able to complete feeding. |
EDEMA |
CRY |
G – Green |
LH – Left Hand |
3 Initially slow to start or passive; has |
||
G – Generalized |
L - Lusty, |
BRB – Bright Red Blood |
RW – Right Wrist |
|
challenges (with |
|
Ex – Hands and Feet |
Vigorous |
P – Plugs |
LW – Left Wrist |
|
coordination, resp. effort, color, tone, |
|
PO – Periorbital |
W - Weak |
Br – Brown |
RAk – Right Ankle |
|
posture or state); needs support |
|
|
|
Hi - |
|
LAk – Left Ankle |
|
throughout and may or may not |
ABDOMINAL |
A - Appropriate |
ASPIRATE TYPE |
S – Scalp |
|
complete feeding. |
|
S – Soft |
for age |
M – Mucous |
B – Broviac |
4 |
Initially energetic or slow to start; |
|
ND – |
F – Formula |
PQ – |
|
becomes disorganized; shows |
||
Ts – Tense |
Q - Quiet |
B – Bilious |
|
|
instability (in |
|
Tn – Tender |
|
FB – Frank Blood |
BLOOD GAS SITE |
|
coordination, resp. effort, color, tone, |
|
DC – Discolored |
PAIN SCREEN |
CG – Coffee Ground |
HS – Heel Stick |
|
posture or state); is unable to complete |
|
D – Distended |
pain screen |
A – Air |
VS – Venous Stick |
|
feeding. |
|
F – Full |
|
FS – Finger Stick |
5 |
(*) Concerning feeding behaviors or |
||
|
|
“triggers” for pain |
DISPOSITION |
Art – Arterial Stick |
|
oral motor patterns; may appear |
BOWEL SOUNDS |
*Refer to pain |
A – Aspirate |
|
|
disinterested or upset with feeding |
|
- |
- Absent |
assessment |
D- Discarded |
CIRC |
|
attempts or may awaken but is unable |
+ |
- Present, Active |
scale |
R- Ref |
CL – Clean |
|
to coordinate |
- Decreased |
|
|
DG – Drainage |
|
|
|
- Hyperactive |
|
|
BL - Bleeding |
|
|
|
BEHAVIOR DURING BREASTFEEDING
1Latches on without difficulty with strong, steady and rhythmic sucks; briefly pauses and readily resumes sucking; frequent,
coordinated suck- swallowing heard
2Latches on without difficulty with strong, steady and rhythmic sucks; briefly pauses
and resumes sucking without help; some swallowing heard.
3 Latches on with minimum difficulty; sucks are short and quick without steady rhythm; pauses and needs help to resume sucking; occasional swallowing heard.
4Roots or licks; latches on with difficulty; briefly maintains latchon or does not suck;
no swallowing heard.
5 Roots or licks; unable to latch on for breastfeeding attempt.
6No effort (sleepy, lacks energy, has no interest, cries, squirms, or pushes away) despite much assistance, unable to successfully attempt breastfeeding.
RESPONSE TO FEEDING
1Appears satiated and comfortable; becomes relaxed, quietly interactive or sleepy without
physiologic changes.
2Becomes tired and fatigued from feeding; has minimal in HR, resp, color or tone.
3Exhausted or taxed by feeding; has changes in resp, color, loss of tone or other
physiologic signs (hiccups, grunts/sounds, cough/choke, head bobbing, O2 sats)
resulting from efforts to feed.
4Has difficulty settling; appears uncomfortable following feeding (shifting within position, straining, spitting, fussiness and/or increased respiratory effort).
SUPPORTS
OB - Occasional Breaks/Pauses
FB - Frequent Breaks/Pauses
PH - Pacing Help
BU - Frequent Burps
FA
SP - Sidelying Position
OP - Other Position
CS - Chin/Cheek Support
OX - Oxygen
EN - Environment
Other - Specify
TYPE OF NIPPLE |
|
|
Y - Yellow |
SF- Slow Flow |
|
R - Red |
P - Playtex |
|
N - Nuk |
H - Haeberman |
|
G – Gerber Premie |
SL=Slit |
|
Eff. 9/1/11 Rev. |
Page 3 of 4 |
|
Connecticut Children’s NICU
at UConn Health Center
282 Washington Street
Hartford, CT 06106
(Patient Identification)
Newborn/Intermediate Flowsheet – Date:
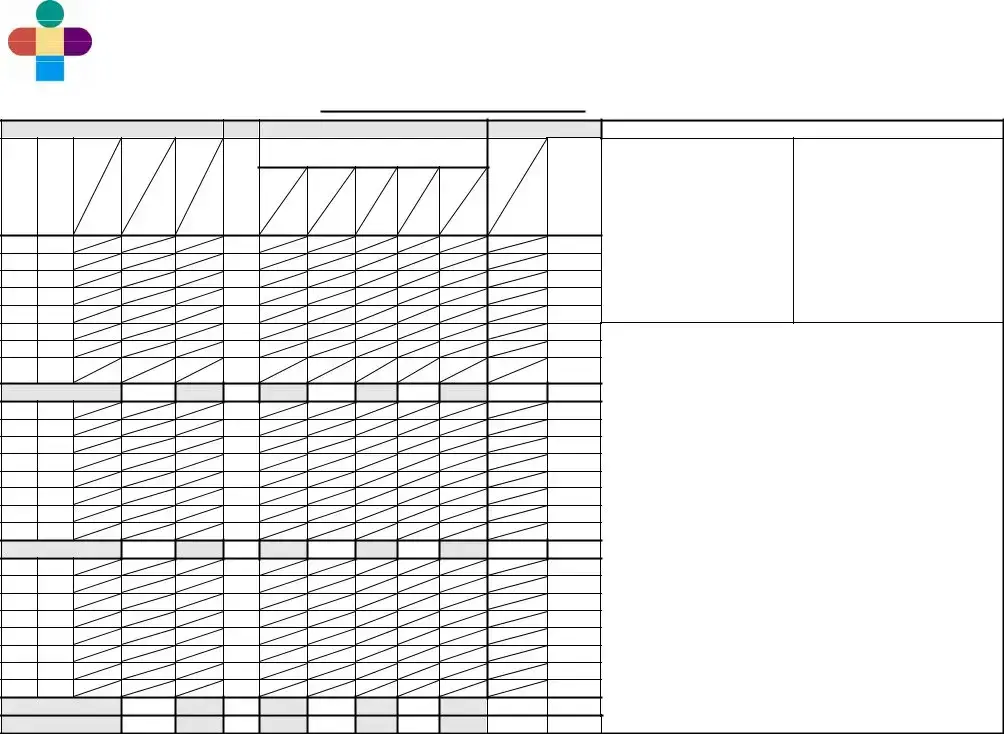
|
|
ENTERAL INTAKE |
|
|
|
PARENTERAL INTAKE |
|
|
OUTPUT |
||||
|
|
|
|
|
|
|
Solution: |
|
|
|
|
|
|
|
|
MODE |
TOTAL |
|
|
E |
|
|
|
|
|
URINE |
STOOL |
T |
F |
|
|
|
|
M |
|
|
|
|
|
|
AMT |
I |
O |
|
|
ASP |
|
E |
Dext% |
Total |
IL |
Total |
Site |
|
COLOR |
M |
R |
|
|
|
S |
|
CONSIS |
||||||
|
|
|
|
|
|
|
|
|
|||||
|
|
AMT |
|
|
|
|
|
|
|
||||
E |
M |
|
|
|
I |
|
|
|
|
|
|
|
|
|
|
|
Type |
|
|
|
|
|
|
|
|||
|
U |
|
|
|
S |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
L |
RATE |
Hourly |
|
|
|
Rate |
|
|
|
|
|
|
|
A |
|
Bolus |
|
|
|
|
|
|
|
URINE |
|
|
|
|
|
|
|
|
Hourly |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
W/STOOL |
|
|
|
|
|
|
|
|
|
|
|
Rate |
Hourly |
Location |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
FORMULA
SUPPLEMENTS
FORMULA TYPE/CALORIE
#1__________________________
#2__________________________
#3__________________________
ORAL (PO) FEEDING DESCRIPTION * See Codes
T |
Behavior |
Attempt |
Behavior |
Response |
|
|
Type |
||
I |
Before |
PO |
During |
to |
Duration |
Supports |
of |
||
M |
|||||||||
|
|
Feeding |
|
|
|
|
|||
E |
Feeding |
Y/N |
Feeding |
|
|
Nipple |
|||
|
|
|
|
||||||
|
|
|
BOTTLE BREAST |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMMENTS:_______________________________________________________
__________________________________________________________________
__________________________________________________________________
__________________________________________________________________
__________________________________________________________________
Eff. 9/1/11 Rev. |
Page 4 of 4 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Facility Name | The flowsheet is utilized at Connecticut Children’s NICU, part of UConn Health Center, located in Hartford, Connecticut. |
| Purpose | This form is designed to document vital signs, assessments, and nursing interventions for newborns and infants undergoing care in the NICU. |
| Parameters Monitored | Parameters include vital signs such as heart rate, respiratory rate, blood pressure, and assessments of pain, respiratory support, and blood gas results. |
| Patient Information | The form includes specific sections for patient identification, allowing for accurate tracking and management of each infant’s care. |
| Standards of Care | The flowsheet outlines specific standards of care including assessments for apnea, bradycardia, breastfeeding support, and IV therapy. |
| Family Involvement | There is a dedicated section for family education and communication to ensure that families are actively involved in the care of their hospitalized infant. |
| Legal Compliance | In Connecticut, the use of this form is governed by state regulations set forth by the Department of Public Health, ensuring adherence to patient care standards. |
| Team Collaboration | Nursing signatures and initials are required throughout the form, promoting accountability and teamwork among healthcare providers. |
| Outcome Tracking | The flowsheet also serves as a tool for ongoing assessment, allowing healthcare professionals to track changes over time and guide care decisions. |
| Versioning | The form has been effective since September 1, 2011, with revisions made as necessary to reflect current best practices and protocols in neonatal care. |
Guidelines on Utilizing Icu Flowsheet
Understanding how to complete the Icu Flowsheet form is essential for accurate documentation and quality care in a neonatal intensive care setting. This form requires detailed information about the newborn's medical status, assessments, and responses throughout their stay in the nursery. Following these steps will help ensure that all necessary data is captured efficiently.
- Start by entering the patient identification details at the top of the form, including the newborn's name and relevant identifiers.
- Record the date for accurate tracking of the newborn’s progress over time.
- Next, fill in the RN signature and initials for each nurse monitoring the patient, ensuring complete accountability.
- List vital signs, assessments, and pain evaluations systematically. Make sure to document heart rate, respiratory rate, blood pressure, temperature, and any notable observations about breath sounds or skin conditions.
- Document any respiratory support provided, including the mode of support and the percent of oxygen delivered (FiO2), making notes on progress or changes in oxygen saturation.
- Complete the segments related to feeding. For both enteral and parenteral intake, specify the types of solutions administered, rates, and details about urine and stool output. All values should be noted clearly and accurately.
- Detail the infant's activity levels and their responses to feeding attempts, capturing behaviors before, during, and after feeding.
- Record any lab test results. Include details such as time, site, and specific test results to keep a comprehensive medical record.
- Finally, add any additional comments or observations that may provide further insights into the infant's condition.
Following these steps closely will help medical staff maintain a comprehensive understanding of the infant’s care, ensuring that all data related to assessments and treatments are recorded effectively. Keep the lines of communication open with parents and other caregivers, as their insights can inform care decisions.
What You Should Know About This Form
What is the purpose of the ICU Flowsheet form?
The ICU Flowsheet form is designed to document and track vital information related to the care of newborns and infants in a neonatal intensive care unit (NICU). It provides a comprehensive way for healthcare providers to record vital signs, assessments, and treatments as part of the infant's clinical management. By maintaining detailed records, staff can ensure continuity of care and monitor any changes in the patient's condition.
What types of information are recorded on the flowsheet?
The flowsheet captures a wide range of information, including vital signs such as heart rate, respiratory rate, blood pressure, and temperature. It also includes assessments such as skin color, muscle tone, and behavioral indicators like crying or lethargy. Furthermore, it documents various treatments, such as breastfeeding or bottle feeding, medication administration, and respiratory support. This array of data aids in evaluating the infant’s health and response to care.
How do healthcare providers use the flowsheet during their shifts?
Healthcare providers use the flowsheet as a real-time tool throughout their shifts to record observations and interventions. Each vital sign check is entered, along with any assessments and actions taken for the infant's care, such as medications given or feeding responses. This systematic documentation supports effective communication among the care team and helps ensure that all staff members are up-to-date on the infant’s status.
Can parents access the information recorded on the flowsheet?
While the primary users of the ICU Flowsheet are healthcare providers, parents may have access to some information recorded in the flowsheet during communication with the care team. Parents should feel encouraged to ask about their child’s care, as the information in the flowsheet can aid in understanding their infant’s condition and treatment plan.
What are the key assessments included in the flowsheet?
The flowsheet includes various key assessments, such as pain assessment, respiratory support needs, feeding reactions, and neurological status. It assesses indicators like weight, behavioral responses to feeding, and any signs of distress. These assessments help practitioners monitor the infant’s well-being and adapt interventions as needed.
What is the significance of documenting vital signs and assessments accurately?
Accurate documentation of vital signs and assessments is crucial for patient safety and effective care. It helps identify trends that might indicate deterioration or improvement in the infant’s condition. Consistent and precise records also fulfill legal requirements and support quality assurance practices within the healthcare facility.
What training do staff need to effectively use the ICU Flowsheet?
Staff members working in the NICU typically undergo training that covers the use of the ICU Flowsheet. This training includes understanding how to capture vital signs and assessments correctly and the significance of each data point. Ongoing education is often provided to ensure that staff remain proficient in using the forms as part of patient care.
How often should the flowsheet be updated?
The flowsheet should be updated regularly, often with each shift change or as new assessments and treatments are administered. For critically ill infants, updates may be needed even more frequently to capture ongoing changes in their condition. Timely documentation ensures that all members of the care team have the most current information available.
What happens to the flowsheet at the time of discharge?
At the time of discharge, the completed flowsheet becomes part of the patient’s medical record. This documentation serves as a summary of care provided during the hospital stay and is crucial for continuity of care. Subsequent healthcare providers may refer to the flowsheet to understand treatment history and any ongoing needs for the infant following discharge.
Common mistakes
Completing the ICU Flowsheet form requires careful attention to detail. One common mistake is failing to accurately document the patient identification. This section is essential for ensuring the correct information is associated with the right individual. Missing or incorrect patient identifiers can lead to serious complications in treatment and care.
Another critical error is neglecting to update the vital signs entries. These measurements are vital indicators of a patient's current health status. If vital signs are not recorded accurately or in a timely manner, healthcare providers may miss significant changes, impacting patient outcomes.
People often make the mistake of omitting comments and observations that provide context to the data entered. These narratives are crucial as they can highlight changes in behavior or response to treatments. When comments are disregarded or poorly written, important insights into the patient's condition may be lost.
Inconsistencies in the signatures of nursing staff present another challenge. All entries require clear acknowledgment from the nursing staff on duty. Missing or unreadable signatures can cause confusion about who is responsible for which entries, which becomes problematic during follow-up and reviews.
The abbreviation used in the flowsheet can also lead to misunderstandings. Many medical terms and abbreviations may not be universally understood. It is crucial to either spell out uncommon terms or ensure that all nursing staff are trained on what each abbreviation denotes to avoid sensational misinterpretations.
Lastly, neglecting to keep the flowsheet updated with the most current information can have severe ramifications. The flowsheet is a dynamic document that should reflect real-time patient data. When entries lag or are not tracked diligently, it can influence treatment decisions made by the healthcare team.
Documents used along the form
The ICU Flowsheet form is an essential document in neonatal intensive care units. It is used to track the various vital signs, assessments, and care provided to newborns. Several other documents complement this form, providing a comprehensive view of a patient’s status, treatments, and family interactions. Below are five key forms that are often used alongside the ICU Flowsheet.
- Admission Assessment Form: This document collects initial patient information at the time of admission. It includes details such as the patient’s medical history, current medications, and allergic reactions. This record helps the healthcare team create a baseline for the newborn’s care.
- Care Plan: The care plan outlines specific goals for the patient based on their condition and needs. It includes interventions that the healthcare team will execute. Regular updates to this plan are made to reflect the patient’s progress or changing needs.
- Medication Administration Record (MAR): The MAR tracks all medications given to the newborn, including dosages and timing. This form ensures that medications are administered safely and allows the nursing staff to monitor any potential side effects closely.
- Discharge Summary: When a newborn is ready for discharge, this document summarizes their hospital stay. It includes key medical information, follow-up appointments, and discharge instructions for parents or guardians.
- Family Communication Log: This log keeps a record of interactions with the family regarding the newborn's care. It includes discussions about the baby’s condition, education on procedures, and emotional support provided to the family during their stay.
These forms together ensure that all aspects of the newborn's care are documented effectively. They help create a clearer picture for the medical team and support better decision-making for patient care. Comprehensive record-keeping is essential for maintaining high standards in neonatal care.
Similar forms
The ICU Flowsheet form is a comprehensive tool used for tracking the care and vital signs of infants in a neonatal intensive care unit. Several other documents share similar functions, facilitating patient monitoring and care management. Here are five documents that are similar to the ICU Flowsheet form:
- Patient Vital Signs Chart: This document tracks vital signs like heart rate, respiratory rate, and blood pressure over time. Similar to the ICU Flowsheet, it provides essential data to monitor the patient’s condition and detect any changes that require medical attention.
- Nursing Assessment Flow Sheet: This form outlines the assessments made by nursing staff during their shifts. Like the ICU Flowsheet, it captures detailed observations and notes on the patient's physical and emotional state, aiding in the overall assessment of care needs.
- Medication Administration Record (MAR): This document logs all medications given to the patient, including dosage and timing. It shares the same function as the ICU Flowsheet in tracking treatments, ensuring accuracy in medication management and preventing potential errors.
- Fluid Balance Chart: This chart monitors the patient's fluid intake and output, crucial for ensuring hydration and medication delivery. The similarity to the ICU Flowsheet lies in its ability to provide a comprehensive view of a patient’s status and fluid needs.
- Neonatal Feeding Record: This document details feeding attempts, methods, and any concerns during feedings. It serves a similar purpose as the ICU Flowsheet by tracking crucial aspects of an infant’s nutrition and growth, thereby playing a vital role in patient care planning.
Dos and Don'ts
- Do clearly write down all vital signs as they are measured.
- Don't leave any sections blank; all information is important.
- Do double-check your dates and times for accuracy.
- Don't forget to sign and initial each entry you make.
- Do ensure that the patient's identification information is complete.
- Don't use shorthand that may not be universally understood.
- Do take your time to provide detailed notes on assessments.
- Don't rely on memory; always verify details before recording.
- Do communicate any changes in the patient's condition as soon as they occur.
Misconceptions
Misunderstandings can often lead to confusion, especially regarding crucial forms like the ICU Flowsheet. Here is a list of common misconceptions about the Newborn/Intermediate Flowsheet used in the NICU at Connecticut Children's:
- The flowsheet is just a formality. Many believe that the ICU Flowsheet is merely an administrative task. In reality, it serves to document vital patient information and enhances communication among the care team, significantly impacting patient outcomes.
- All staff complete the flowsheet the same way. A common assumption is that every nurse or staff member interprets and fills out the flowsheet identically. Each caregiver may have different experiences and insights into a patient’s needs, which can affect the documentation.
- The flowsheet only records vital signs. While essential for monitoring, the ICU Flowsheet encompasses much more. It also includes assessments of behavior, feeding responses, and pain levels, providing a comprehensive view of the infant’s health.
- Any entries on the flowsheet are acceptable. Some may think that informal notes or abbreviations are sufficient. However, accurate and standardized entries are critical for clarity and continuity of care.
- It is not necessary to involve parents in the process. People might presume that documenting care is solely the responsibility of the healthcare team. Including parents and encouraging their insights fosters a collaborative environment, promoting a holistic approach to the infant’s care.
- The flowsheet is only for medical staff. Many believe that only nurses and doctors utilize the ICU Flowsheet. In truth, various health care professionals, including nutritionists and social workers, reference it to provide comprehensive support for both the infant and family.
- Retroactive entries are permissible without restriction. Some assume they can easily modify the flowsheet after the fact. Rather than facilitating this practice, protocols typically exist to ensure accuracy and accountability, minimizing discrepancies in the patient’s record.
Understanding these common misconceptions can help mitigate confusion and enhance the care given to vulnerable patients in the NICU.
Key takeaways
Here are some important points to consider when filling out and using the ICU Flowsheet form:
- Accurate Patient Identification: Ensure that patient identification details are filled out correctly at the top of the form. This information is crucial for accurate record-keeping.
- Document Vital Signs: Regularly assess and record vital signs, including heart rate, respiratory rate, and blood pressure. Consistency in monitoring is key to patient care.
- Multidisciplinary Use: This form is designed for use by various healthcare professionals, such as nurses and physicians, to track patient progress and treatment plans effectively.
- Room for Comments: Utilize the comments section for additional notes. This can include observations about patient behavior, response to treatment, or deviations from expected outcomes.
- Follow Care Standards: Adhere to the standards of care outlined in the form for specific conditions. These guidelines help ensure that best practices are followed during patient care.
- Regular Updates: Update the form regularly to reflect the latest patient status and interventions. Timely updates are essential for effective team communication and decision-making.
- Training and Education: Familiarize yourself with the codes and abbreviations used in the form. Training on how to use this document can improve accuracy and efficiency in patient care.
Browse Other Templates
Rut 50 Tax Information - Filing mistakes can be costly, so double-check all figures and calculations before submission.
How to Get a Resale Certificate in Ct - A completed certificate can enhance a business's credibility with suppliers.
Transcript Request Form,Official Transcript Application,Durham Tech Transcript Order,Student Record Request,Durham Tech Transcript Application,Transcript Release Form,Transcript Issuance Request,Academic Record Request,Transcript Retrieval Form,Durha - A student ID number is required for processing your request.