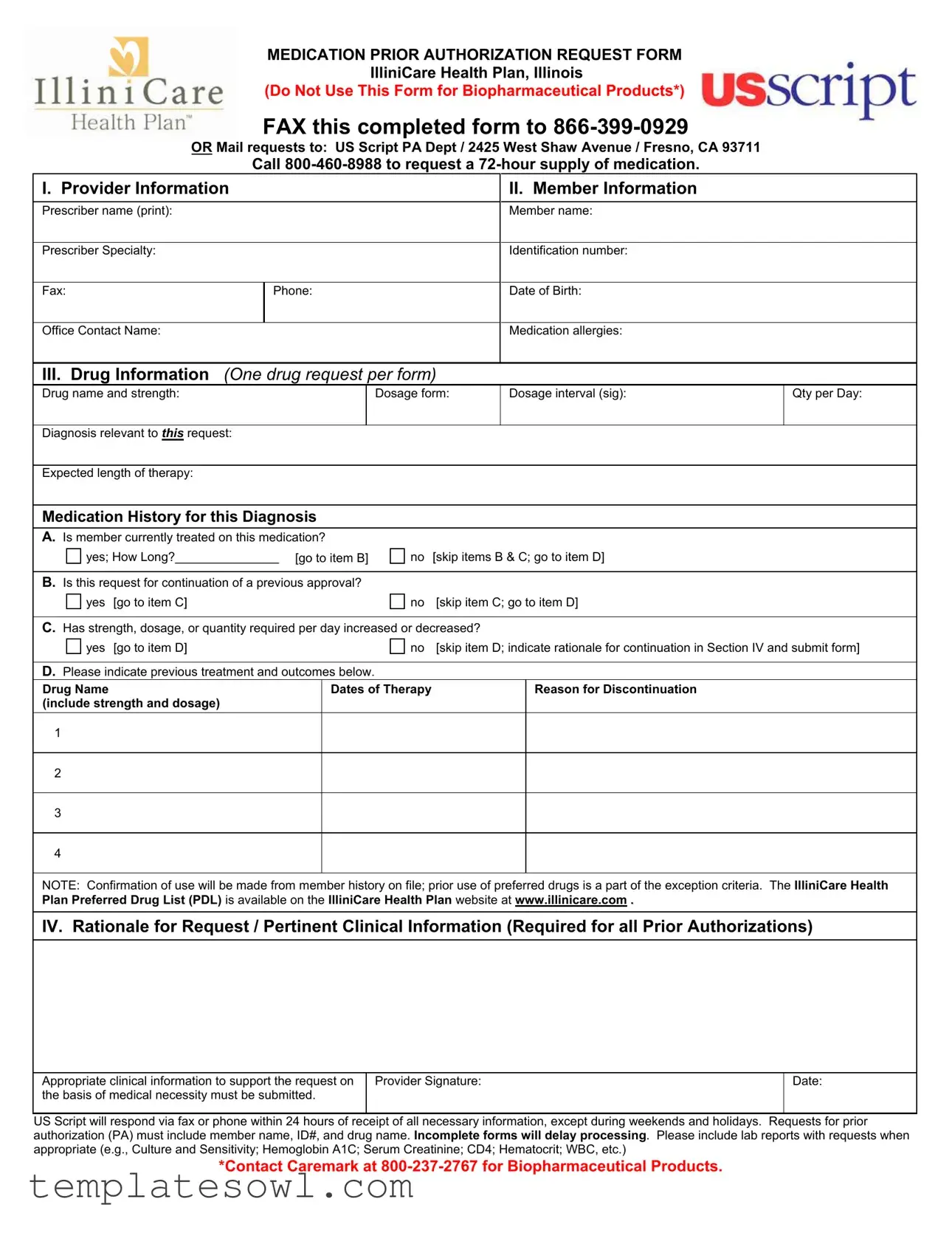
Fill Out Your Illinicare Prior Authorization Form
The Illinicare Prior Authorization form is a critical document within the IlliniCare Health Plan, designed to facilitate the approval process for specific medications. It is essential that healthcare providers understand the key sections of this form to ensure accurate and timely submissions. The form requires detailed information from both the provider and the member, including the prescriber's contact details and the member's identification number and medical history. It focuses on one drug per request, capturing the medication name, dosage, and relevant diagnosis. Close attention should be paid to the medication history to provide context for the request, particularly whether the member has previously been treated with the medication or if there have been changes in dosage or quantity. Rationale for the request must include crucial clinical details supporting medical necessity, further strengthening the application. Providers should also attach any relevant lab reports, as these documents may expedite the decision-making process. Understanding these elements can significantly impact the smooth processing of medication requests, helping ensure that patients obtain the necessary treatments without unnecessary delays.
Illinicare Prior Authorization Example
MEDICATION PRIOR AUTHORIZATION REQUEST FORM
IlliniCare Health Plan, Illinois
(Do Not Use This Form for Biopharmaceutical Products*)
FAX this completed form to
OR Mail requests to: US Script PA Dept / 2425 West Shaw Avenue / Fresno, CA 93711
Call
I. Provider Information |
|
|
II. Member Information |
|
|||||
|
|
|
|
|
|
|
|
|
|
Prescriber name (print): |
|
|
Member name: |
|
|||||
|
|
|
|
|
|
|
|
|
|
Prescriber Specialty: |
|
|
Identification number: |
|
|||||
|
|
|
|
|
|
|
|
|
|
Fax: |
|
Phone: |
|
|
Date of Birth: |
|
|||
|
|
|
|
|
|
|
|
|
|
Office Contact Name: |
|
|
Medication allergies: |
|
|||||
|
|
|
|
|
|
||||
III. Drug Information (One drug request per form) |
|
|
|
||||||
Drug name and strength: |
|
Dosage form: |
Dosage interval (sig): |
Qty per Day: |
|||||
|
|
|
|
|
|
|
|
||
Diagnosis relevant to THIS request: |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
Expected length of therapy: |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
Medication History for this Diagnosis |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
A. Is member currently treated on this medication? |
|
|
|
|
|
||||
yes; How Long?_______________ [go to item B] |
no |
[skip items B & C; go to item D] |
|
||||||
|
|
|
|
|
|
|
|||
B. Is this request for continuation of a previous approval? |
|
|
|
|
|
||||
yes |
[go to item C] |
no |
[skip item C; go to item D] |
|
|||||
|
|
|
|
|
|||||
C. Has strength, dosage, or quantity required per day increased or decreased? |
|
|
|
||||||
yes |
[go to item D] |
no |
[skip item D; indicate rationale for continuation in Section IV and submit form] |
||||||
|
|
|
|
|
|
|
|||
D. Please indicate previous treatment and outcomes below. |
|
|
|
|
|
||||
Drug Name |
|
|
Dates of Therapy |
|
|
Reason for Discontinuation |
|
||
(include strength and dosage) |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NOTE: Confirmation of use will be made from member history on file; prior use of preferred drugs is a part of the exception criteria. The IlliniCare Health Plan Preferred Drug List (PDL) is available on the IlliniCare Health Plan website at www.illinicare.com .
IV. Rationale for Request / Pertinent Clinical Information (Required for all Prior Authorizations)
Appropriate clinical information to support the request on |
Provider Signature: |
Date: |
the basis of medical necessity must be submitted. |
|
|
|
|
|
US Script will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends and holidays. Requests for prior authorization (PA) must include member name, ID#, and drug name. Incomplete forms will delay processing. Please include lab reports with requests when appropriate (e.g., Culture and Sensitivity; Hemoglobin A1C; Serum Creatinine; CD4; Hematocrit; WBC, etc.)
*Contact Caremark at
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to request prior authorization for medications through the IlliniCare Health Plan in Illinois. |
| Submission Methods | The completed form can be faxed to 866-399-0929 or mailed to US Script PA Dept at the designated address. |
| Request for 72-hour Supply | To request a 72-hour supply of medication, call 800-460-8988. |
| Required Information | Important details include provider information, member information, medication details, and clinical rationale. |
| Medication Request Limitations | This form is not to be used for biopharmaceutical products. Separate contact with Caremark is required for those requests. |
| Response Time | US Script will respond within 24 hours upon receipt of complete and necessary information, excluding weekends and holidays. |
| Validity of Previous Treatments | The form asks about the member's previous treatment history, including outcomes and reasons for discontinuation. |
| Criteria for Approval | Prior use of preferred drugs is one of the exception criteria for approval; details are available on the IlliniCare Health Plan website. |
| Clinical Information | All prior authorization requests require clinical information that supports medical necessity to be considered for approval. |
Guidelines on Utilizing Illinicare Prior Authorization
Completing the Illinicare Prior Authorization form requires careful attention to detail. Ensure all relevant information is accurate, as this will facilitate a timely response from the health plan. After filling out the form, you’ll need to submit it either via fax or mail, depending on your preference.
- Provide the Prescriber Information: Fill in your name, specialty, fax number, phone number, and office contact name.
- Complete the Member Information: Enter the member's name, identification number, and date of birth. Don’t forget to note any medication allergies.
- Detail the Drug Information: Specify the drug name and strength, dosage form, dosage interval, quantity per day, and relevant diagnosis.
- Indicate the Expected Length of Therapy: Clearly state how long the member is expected to be on this medication.
- Provide Medication History: Answer whether the member is currently being treated with this medication, and complete items B, C, and D as applicable.
- Rationale for Request: Offer appropriate clinical information to justify the necessity of the medication.
- Sign the Form: The prescriber must sign and date the form to validate the request.
- Submit the Form: Fax it to 866-399-0929 or mail it to US Script PA Dept / 2425 West Shaw Avenue / Fresno, CA 93711.
Please ensure that all fields are thoroughly filled out to avoid processing delays. Additional documentation, such as lab reports, should be included when relevant.
What You Should Know About This Form
What is the purpose of the Illinicare Prior Authorization form?
The Illinicare Prior Authorization form is used to request approval for specific medications under the IlliniCare Health Plan. This process ensures that prescribed medications meet the criteria for medical necessity and align with the health plan's coverage policies. Authorization is typically required before certain medications can be dispensed, allowing healthcare providers to demonstrate the need for a specific medication based on a patient’s medical history and current treatment plan.
How should I submit the Illinicare Prior Authorization form?
Once the form is completed, it can be submitted either by fax or by mail. To fax the request, send it to 866-399-0929. If you prefer to mail the form, it should be addressed to US Script PA Dept, 2425 West Shaw Avenue, Fresno, CA 93711. In urgent situations, providers can call 800-460-8988 to request a 72-hour supply of medication while awaiting prior authorization.
What information is required to complete the Illinicare Prior Authorization form?
Key elements of the form include provider and member information, details about the requested drug, and pertinent clinical information supporting the need for the medication. Specifically, providers must indicate the member’s diagnosis, medication history, and expected length of therapy. If there are any medication allergies, these should also be noted. To facilitate timely processing, all necessary and relevant information must be submitted accurately. Incomplete forms can lead to processing delays.
What can I expect after submitting the Illinicare Prior Authorization form?
After submission, US Script will review the request and respond via fax or phone within 24 hours, provided all necessary information is included. If the request is deemed incomplete or requires further information, the response may be delayed. It is important for providers to include lab reports and other relevant clinical documentation when appropriate, as this can support the request and assist in expediting the approval process.
Common mistakes
Completing the Illinicare Prior Authorization form can be a crucial step in ensuring that members receive necessary medications in a timely manner. However, there are common mistakes that can hinder this process. Understanding these pitfalls could prevent delays and complications.
One frequent error stems from incomplete provider information. It’s vital to fill out all sections related to the prescriber accurately. Missing the prescriber’s name, fax number, or phone details can lead to significant hold-ups in processing the request. Each piece of information plays a role in establishing proper communication between the provider and the authorization team.
Another common mistake is neglecting member information. The member’s identification number and date of birth must be clearly written. These details are essential for verifying eligibility and ensuring that the request corresponds to the right individual. A small oversight here could result in an immediate rejection of the authorization request.
When it comes to drug information, only one drug should be requested per form. Submitting multiple requests on one form can lead to confusion and potential rejections. This is a critical step that many may overlook, thinking it may save time. However, following the guideline of one request per form enhances clarity.
Additionally, failing to provide an adequate diagnosis relevant to the request is a recurring issue. This information must clearly link the medication to the condition being treated. A vague or incomplete diagnosis can easily lead to back-and-forth communication that delays approval.
A key mistake relates to the medication history section. When indicating whether the member is currently treated with the medication, it’s important to answer this accurately. An incorrect answer may require further clarification and could cause unnecessary delays in approval.
In the rationale for the request, it's also critical to include comprehensive clinical information. Requests often lack the necessary supporting documentation, which can slow down the process significantly. Providing lab reports when appropriate is essential, as it offers the back-up needed for the medical necessity of the medication.
Finally, a common oversight is the omission of the prescriber’s signature and date. Not completing this section may result in the form being deemed invalid and returned for correction. Ensuring that this final step is included is crucial for the timely processing of the request.
By avoiding these mistakes, individuals can help streamline the prior authorization process, ensuring quicker access to medications that the member may desperately need. Keeping each section thorough and accurate will facilitate an efficient review and response from Illinicare Health Plan.
Documents used along the form
When navigating the healthcare system, having the right documentation is essential for obtaining approval for medications. The IlliniCare Prior Authorization form is critical, but other forms and documents are often used in conjunction with it. Each serves a unique purpose that can help streamline the approval process.
- Medication History Record: This document details the member's past medication use. It includes information on previous prescriptions, dosages, and any adverse reactions. Providing this record helps illustrate the member's treatment history, supporting the case for the request.
- Clinical Notes: Providers use these notes to document the patient's medical condition and how it relates to the requested medication. This document might be necessary for demonstrating medical necessity and explaining why the prescribed drug is appropriate for the member’s diagnosis.
- Lab Results: Specific lab reports, such as blood tests or biopsies, may be needed to back up the authorization request. These can include results from tests like Hemoglobin A1C or serum creatinine, which provide valuable clinical information to aid in the decision-making process.
- Drug Utilization Review (DUR): This review examines a patient's medication history against their current medications to prevent potential drug interactions or harmful effects. It offers insight into the appropriateness of the requested medication based on the member’s overall treatment plan.
- Patient Consent Form: In some cases, obtaining consent from the member for sharing their medical information may be necessary. This document ensures that the provider can lawfully communicate no sensitive information related to the authorization request.
Having these accompanying documents can significantly speed up the prior authorization process and increase the chances of a positive outcome. When preparing a submission, ensure that all relevant information is included and clear to facilitate an efficient review by the payer.
Similar forms
The Illinicare Prior Authorization form serves a specific purpose in the healthcare landscape. Several other documents share similarities in function and purpose. Here’s a brief overview of five such documents:
- Medicare Prior Authorization Form: This form is designed for Medicare beneficiaries seeking pre-approval for certain medical services or procedures. Like the Illinicare form, it requires detailed patient and provider information and aims to ensure medical necessity is established before treatment begins.
- Medicaid Prior Authorization Request: Similar to the Illinicare form, this document is used by Medicaid recipients to obtain prior authorization for specific medications or services. It includes sections for medication history and clinician justification to demonstrate that the proposed treatment meets medical criteria.
- Commercial Insurance Prior Authorization Form: Many commercial health plans have their own prior authorization forms. These documents typically require similar elements, such as patient demographic details, medical history, and specifics about the proposed treatment or medication to secure necessary approval.
- Non-Formulary Drug Exception Request: This document is often utilized when a provider requests a medication not listed on the insurance company’s formulary. Much like the Illinicare form, it seeks to prove that the non-formulary drug is medically necessary for the patient’s treatment.
- Durable Medical Equipment (DME) Prior Authorization Form: This form is related to the request for authorization for durable medical equipment. It emphasizes the need for clinical justification similar to the Illinicare prior authorization request, ensuring that equipment is needed for patient health and safety.
These documents, while tailored to different aspects of patient care, all share a commitment to ensuring that treatments are justified, necessary, and aligned with best practices in patient health management.
Dos and Don'ts
When filling out the Illinicare Prior Authorization form, certain practices can help ensure a smooth submission process. Here is a list of important dos and don’ts:
- Do provide all required information clearly, including prescriber and member details.
- Do include relevant clinical information to support the medical necessity of the request.
- Do ensure the form is complete, filling in all sections as instructed.
- Do submit any pertinent lab reports that may assist in the approval process.
- Don’t leave any sections blank, as incomplete forms may delay processing.
- Don’t use this form for biopharmaceutical products; a different process is required.
- Don’t forget to fax or mail the completed form to the correct address.
- Don’t skip the rationale section; it is necessary for all prior authorizations.
Misconceptions
1. All medications require prior authorization. This is not true. Only specific medications, typically those that are high-cost or potentially misused, need prior authorization.
2. You can submit multiple drug requests on one form. This misconception is incorrect. The Illinicare Prior Authorization form is designed for one drug request per submission. Submit a separate request for each medication.
3. Submitting a completed form guarantees approval. While the form is a necessary step, it does not guarantee that the medication will be authorized. The approval relies on medical necessity and other criteria.
4. You can submit the form via email. This is a misconception. The only accepted methods for submitting the form are via fax or mail.
5. Approval can take a long time, delaying treatment. This is misleading. If all necessary information is provided, Illinicare typically responds within 24 hours. Delays often occur from incomplete submissions.
6. The provider's signature is optional. This is false. A provider's signature is required on the form to validate the request and confirm medical necessity.
7. You need to include lab reports for every request. Not every request requires lab reports. Only include them when appropriate or requested to support the clinical information.
8. Patients cannot check the status of their authorization. Patients can inquire about the status. Calling the customer service number allows for updates on authorization requests.
9. The Prior Authorization process is the same for all health plans. This is a common misconception. Each health plan may have different requirements, processes, and forms, so it's essential to follow the specific procedures for Illinicare.
Key takeaways
Understanding the Illinicare Prior Authorization form is crucial for ensuring timely access to medication. Here are nine key takeaways for effective completion and use of the form:
- Submit via fax or mail: You can send the completed form by faxing it to 866-399-0929 or mailing it to the specified address in Fresno, CA.
- Provide accurate provider information: Include the prescriber’s name, specialty, contact details, and any relevant office contact information.
- Member information is essential: Fill in the member's name, identification number, and date of birth correctly to avoid processing delays.
- One drug per request: Ensure you fill out only one drug per form. Multiple requests need separate forms.
- Accurate drug details: Clearly indicate the drug name, dosage, and quantity per day as well as any relevant diagnosis for the request.
- Rationale is required: Provide necessary clinical information to support the request based on medical necessity.
- Complete the medication history: Note whether the member is currently on the medication and provide details about previous treatments and outcomes.
- Timeliness of response: US Script typically responds within 24 hours, but requests submitted during weekends or holidays may take longer.
- Include supporting documents: Attach lab reports when relevant, such as Culture and Sensitivity results or serum levels, to strengthen the request.
By adhering to these guidelines, you can enhance the likelihood of a smooth prior authorization process. Always keep communication lines open with the member and the prescriber to ensure all needed information is provided.
Browse Other Templates
Form P17 Notice of Renunciation - The renunciation is a formal legal statement affecting the decedent's estate distribution.
Mortgage Itemized Fee Worksheet Excel - The worksheet simplifies the assessment of costs for assigning funds appropriately at closing.