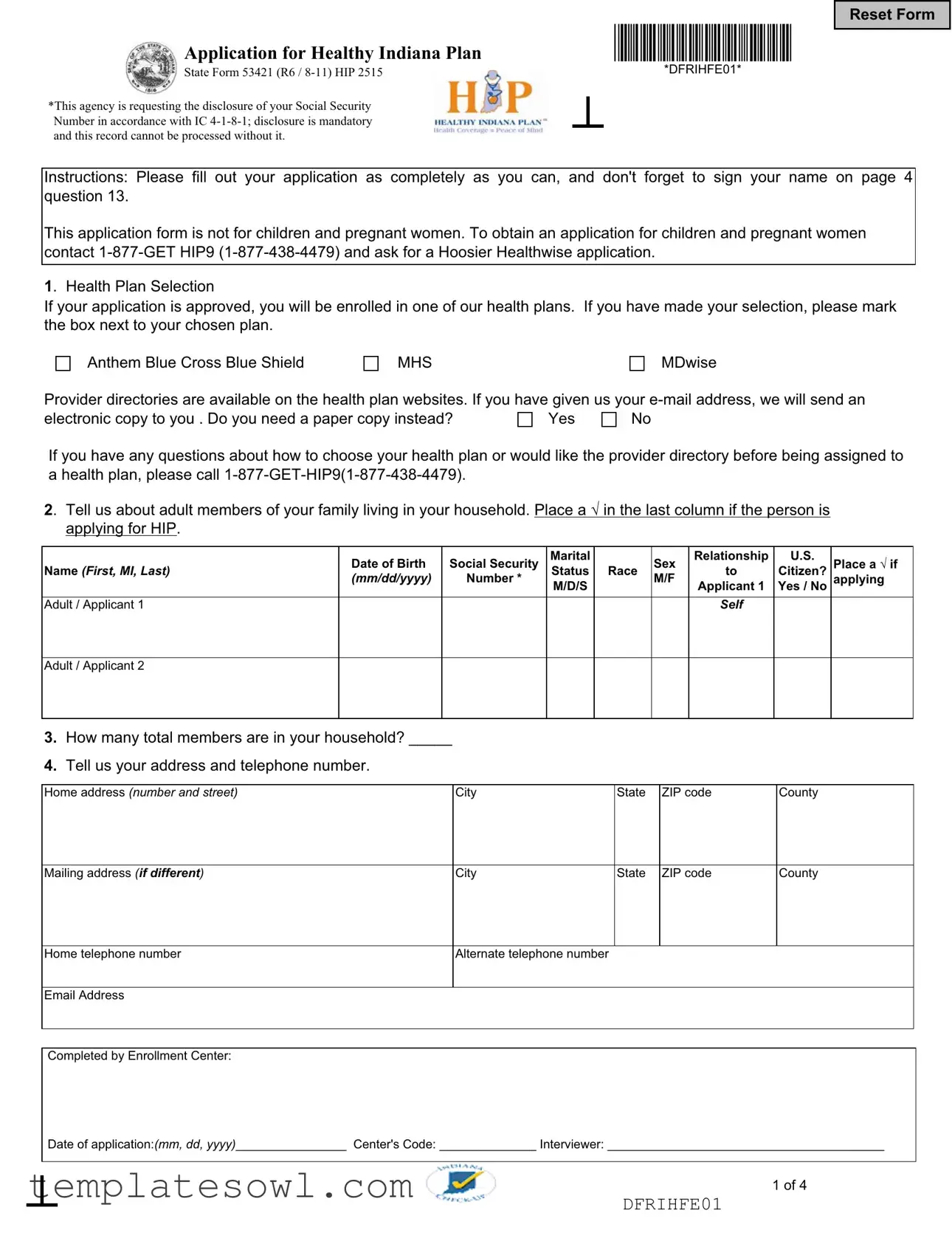
Fill Out Your Indiana 53421 Form
The Indiana 53421 form, officially titled the Application for Healthy Indiana Plan (HIP), serves as a crucial tool for uninsured adults in Indiana who are seeking access to healthcare coverage. This application is specifically designed for individuals who are 19 years and older, excluding children and pregnant women, who have separate application processes. Applicants must accurately fill out the form, which requires personal details such as name, date of birth, and Social Security Number—a mandatory disclosure for processing the application. The form also facilitates health plan selection, where applicants can indicate their preferred health plan from options including Anthem Blue Cross Blue Shield, MHS, and MDwise. Importantly, the application requires information about household members, income details, and prior health coverage status to determine eligibility for the Health Indiana Plan’s range of services. Additionally, the form mandates responses to several health screening questions aimed at assessing applicants’ specific healthcare needs. This thorough collection of information ensures that applicants receive appropriate health coverage tailored to their circumstances. Finally, applicants are reminded to provide necessary signatures and required documentation to expedite the processing of their applications, further emphasizing the importance of accuracy and completeness in this essential health initiative.
Indiana 53421 Example
Application for Healthy Indiana Plan
State Form 53421 (R6 /
*This agency is requesting the disclosure of your Social Security Number in accordance with IC
Reset Form
*DFRIHFE01*
Instructions: Please fill out your application as completely as you can, and don't forget to sign your name on page 4 question 13.
This application form is not for children and pregnant women. To obtain an application for children and pregnant women contact
1. Health Plan Selection
If your application is approved, you will be enrolled in one of our health plans. If you have made your selection, please mark the box next to your chosen plan.
Anthem Blue Cross Blue Shield
MHS
MDwise
Provider directories are available on the health plan websites. If you have given us your
electronic copy to you . Do you need a paper copy instead? |
Yes |
No |
If you have any questions about how to choose your health plan or would like the provider directory before being assigned to a health plan, please call
2. Tell us about adult members of your family living in your household. Place a applying for HIP.
|
Date of Birth |
Social Security |
Marital |
|
Sex |
Relationship |
U.S. |
Place a |
Name (First, MI, Last) |
Status |
Race |
to |
Citizen? |
||||
|
(mm/dd/yyyy) |
Number * |
M/D/S |
|
M/F |
Applicant 1 |
Yes / No |
applying |
Adult / Applicant 1 |
|
|
|
|
|
Self |
|
|
|
|
|
|
|
|
|
|
|
Adult / Applicant 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3.How many total members are in your household? _____
4.Tell us your address and telephone number.
Home address (number and street) |
City |
State |
ZIP code |
County |
|
|
|
|
|
|
|
Mailing address (if different) |
City |
State |
ZIP code |
County |
|
|
|
|
|
|
|
Home telephone number |
Alternate telephone number |
|
|
|
|
|
|
|
|
|
|
Email Address |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Completed by Enrollment Center: |
|
|
|
|
|
Date of application:(mm, dd, yyyy)________________ Center's Code: ______________ Interviewer: ________________________________________
1 of 4
DFRIHFE01
*DFRIHFE02*
Application for Healthy Indiana Plan
State Form 53421 (R6 /
5.Tell us about children living in your home.
|
Date of Birth |
Social Security |
Applicant 1 is |
Applicant 2 is a |
|
Sex |
U.S. Citizen? |
|
|
a caregiver of |
caregiver of |
|
|||||
Name (First, MI, Last) |
(mm/dd/yyyy) |
Number * |
Race |
M/F |
Yes / No |
|||
this child |
this child |
|||||||
|
|
|
|
|
|
|||
|
|
|
Yes/No |
Yes/No |
|
|
|
|
Child 1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 1 Relation to Applicant 1: |
|
|
Child 1 Relation to |
Applicant 2: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 2 Relation to Applicant 1: |
|
|
Child 2 Relation to |
Applicant 2: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 3 Relation to Applicant 1: |
|
|
Child 3 Relation to |
Applicant 2: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child 4 Relation to Applicant 1: |
|
|
Child 4 Relation to |
Applicant 2: |
|
|
|
|
|
|
|
|
|
|
|
|
6.Do all of the applicants live in Indiana?
Yes
No
7. Does either of the applicants pay someone to care for a dependant child or a disabled/elderly adult so that a household
member can work, look for a job or go to school? |
Yes |
No |
If yes, does the person for whom the expense is being paid live in the household?
Yes
No
If no, go on to the next item. If yes, enter
Applicant Number
Name of person being cared for
How often paid
Amount paid
Name of care provider
Address of provider (number and street, city, state, and ZIP code)
8.Complete this section for each applicant who is not a citizen of the United States.
1. |
Lawful Permanent Resident |
3. Granted Political Asylum |
5. Parolee |
7. Undocumented |
2. |
Refugee |
4. Cuban/Haitian Entrant |
6. Amerasian |
8. Other (specify) __________ |
Applicant Number
Document Number
Immigration Status
(number from above)
Status Date
(mm/dd/yy)
Country of origin
Date of entry into the U.S.
(mm/dd/yy)
2 of 4
DFRIHFE02
*DFRIHFE03*
Application for Healthy Indiana Plan
State Form 53421 (R6 /
9.For each applicant please provide the following information.
|
Place a if |
Place a if |
Applicant has |
Covered by |
Date applicant last |
Why was health insurance lost? Please write one |
||
|
Blind or |
Pregnant |
access to health |
health insurance |
had health insurance |
of these reasons below; Loss of employment, |
||
|
Disabled |
|
insurance at |
now including |
including Medicare |
Could not afford, Coverage limit reached, |
||
|
|
|
employer |
Medicare |
|
(mm/dd/yy) |
Company ended coverage, |
|
|
|
|
(check one for |
(check one for |
|
dropped insurance, Divorce, Cobra expired, Other |
||
|
|
|
each applicant) |
each applicant) |
|
|
||
|
|
|
|
|
|
|
|
|
Applicant 1 |
|
|
Yes |
No |
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
Applicant 2 |
|
|
Yes |
No |
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
10.Tell us how much total work income the applicant(s) earn.
Applicant 1 |
Applicant 2 |
|
|
Start date (mm/dd/yy) |
Start date (mm/dd/yy) |
|
|
End date (mm/dd/yy) |
End date (mm/dd/yy) |
|
|
Amount of gross pay per period ($) |
Amount of gross pay per period ($) |
How often paid? |
Weekly |
|
Monthly |
How often paid? |
Weekly |
|
Monthly |
||
|
Twice a month |
Other: _______________ |
|
Twice a month |
Other: _______________ |
||||
|
|
|
|
|
|
|
|
|
|
Hours worked per week |
|
|
|
|
Hours worked per week |
|
|
|
|
|
|
|
|
|
|
|
|
||
Is person |
Yes |
|
No |
Is person |
Yes |
No |
|
||
|
|
|
|
|
|
|
|
|
|
Do hours vary? |
|
Yes |
|
No |
Do hours vary? |
|
Yes |
No |
|
|
|
|
|
|
|
||||
Name of employer and telephone number |
|
|
Name of employer and telephone number |
|
|
||||
11.Tell us if you or family members receive other income from the types listed here. If your family has no income, initial here: _______.
A) SSI |
F) Military Allotment |
K) Interest Payments |
O) Child Support |
B) Social Security |
G) Unemployment |
L) Educational Income |
P) Employment |
C) Veteran's Benefits |
H) Alimony |
M) Cash from Friends, |
income from |
D) Railroad Retirement |
I) Sick Benefits |
Relatives, etc. |
children |
E) Pension |
J) Strike Benefits |
N) Worker's |
Q) Other:____________ |
|
|
Compensation |
|
Who receives the payments?
(applicant number or child number)
What type of payments?
(Use letter code from above.)
How Often are Payments
Received?
When did Payments Begin?
Amount of the
Payments ($)
DFRIHFE03 |
3 of 4 |
|
*DFRIHFE04*
Application for Healthy Indiana Plan
State Form 53421 (R6 /
12. Health Screening Questions
(These questions must be answered in order for your application to be considered complete.)
To the best of your ability, please answer either “Yes” or “No” to the following questions by checking the appropriate answer. This information is being collected to determine whether you will be eligible for the Enhanced Services Plan. This plan will provide a high degree of coordinated medical care for persons with specialized health care needs. If you are otherwise found to be eligible for HIP, you cannot be denied coverage based on a medical condition. Answering “Yes” to any of the following questions will not prevent you from obtaining health coverage.
For each question below, check only one answer for each applicant. |
Applicant 1 |
Applicant 2 |
|
||
a. In the last three years have you been diagnosed or actively treated for an internal |
|
|
|
|
|
Cancer? This includes but is not limited to cancers of the: brain; head or neck; throat; |
Yes |
No |
Yes |
No |
|
esophagus; larynx; lung; breast; stomach; intestines; colon; pancreas; liver or biliary |
|
||||
|
|
|
|
|
|
tract; ovary; prostate; testicles; bladder; bone; or blood. |
|
|
|
|
|
|
|
|
|
|
|
b. Have you ever been the recipient of an organ transplant including heart, lung, liver, |
Yes |
No |
Yes |
No |
|
kidney or bone marrow? |
|
||||
|
|
|
|
|
|
c. Are you currently on a transplant waiting list for one of the above organs or been advised |
Yes |
No |
Yes |
No |
|
that you will require such a transplant within the next 12 months? |
|
||||
|
|
|
|
|
|
d. Have you ever been diagnosed with or otherwise told by a medical professional that you |
Yes |
No |
Yes |
No |
|
have HIV, AIDS or the virus that causes AIDS? |
|
||||
|
|
|
|
|
|
e. Do you take or have you ever taken medication for HIV, AIDS, or the virus that causes |
Yes |
No |
Yes |
No |
|
AIDS? |
|
||||
|
|
|
|
|
|
f. Have you ever been diagnosed with aplastic anemia? |
Yes |
No |
Yes |
No |
|
|
|
||||
|
|
|
|
|
|
g. Do you require frequent blood transfusions due to a medical condition? |
Yes |
No |
Yes |
No |
|
|
|
||||
|
|
|
|
|
|
h. Have you ever been diagnosed with or are you being actively treated for hemophilia, or |
|
|
|
|
|
other rare bloodstream diseases including Von Willebrand's disease, or congenital factor |
Yes |
No |
Yes |
No |
|
VIII disorder? |
|
|
|
|
|
|
|
|
|
|
|
All information collected will be treated as confidential pursuant to 470 IAC
13.Signature Required Please read carefully, then sign and date below.
I certify under penalty of perjury, that all the information I have provided is complete and correct to the best of my knowledge and belief.
Applicant 1 signature: ______________________________________ Date: (mm/dd/yy): _________________
Applicant 2 signature: ______________________________________ Date: (mm/dd/yy): _________________
Signature of witness if signed with “X”: ____________________________________________________________
14.Do you want to register to vote ?
Yes
No |
Your answer will not affect your eligibility for health coverage. |
4 of 4
DFRIHFE04

*DFRIGAE01*
Information to Get You Started
Enclosed is your application for the Healthy Indiana Plan, a health coverage program for uninsured adults age 19 through 64. The steps to follow in applying for HIP are explained below.
Step 1: Complete and sign the application.
Answer ALL questions truthfully and completely to the best of your knowledge, including the Health Screening Questions. Use only black or blue pen.
Gather and copy any of the documents listed below as proof of the information on your application.
Sending these papers with your application will help us process it faster. Write your name and Social Security Number on all copies of documents that you send with your application.
To provide |
Send for each person applying … |
|
proof of… |
||
Identity |
Valid driver’s license or state or student photo ID card. If you have someone acting on your |
|
|
behalf, that person will need to provide proof of his or her identity also. |
|
|
|
|
US citizenship |
Legal birth certificate, Certificate of Naturalization, Certificate of Citizenship, U.S. passport if it |
|
|
was issued with no restrictions. |
|
|
|
|
Money |
Wages: Pay stubs, paychecks, statement from employer(s) for the most current month; |
|
received by |
Employment termination: A statement from last employer giving dates of employment and |
|
applicant, |
reason for termination. |
|
spouse, and |
||
dependent |
||
Child Support, Social Security, VA, SSI, Workers’ Compensation, disability, sick pay, |
||
children in the |
||
home |
unemployment, or other benefits: court order, award letter or other proof of payment from |
|
|
the source of the income. |
|
|
Loans, gifts, or contributions: Promissory note; loan agreement; or statement from person |
|
|
providing the money that includes the person’s name, address, phone number, signature, and |
|
|
date. |
|
|
|
|
Guardianship |
If someone has legal authority to act on your behalf, provide a copy of the Power of Attorney, |
|
or Power of |
Guardianship Order, Court Order, or similar documents. |
|
Attorney |
|
|
|
|
|
Immigration |
If you are not a US citizen, a copy of your alien registration card, permanent resident card, or |
|
Status |
other documentation from the Bureau for Citizenship and Immigration Services (formerly the |
|
|
INS). |
|
|
|
Step 2: Return the application to us. If you choose to send by fax, be sure to fax both sides of the application pages and any additional documents. You can return your completed application and other documents to us by:
Mailing them to the Document Center at: FSSA Document Center / PO Box 1630 / Marion, IN 46952; or
Faxing them to the Document Center at
Dropping them off at a local FSSA DFR office. To find a local office, please go to our Web site at www.in.gov/fssa/dfr or call toll free
Step 3: Cooperate with requests for more information or interviews. We will contact you by telephone or mail if we need additional information or documentation to complete your application. Please respond quickly to requests for additional information so that we can process your application.
|
DFRIGAE01 |
*DFRIGAE02*
IMPORTANT INFORMATION ABOUT THE HEALTHY INDIANA PLAN
Keep this information for your records. Do not send it in with your application.
Benefits under the Plan
HIP provides health insurance coverage to eligible adults. Enrolled members keep their HIP benefits for 12 continuous months even if income or family size changes. Members must live in Indiana and have no other access to health insurance coverage. Benefits are provided through private health insurance companies and also the State’s Enhanced Services Plan (ESP) for members who have complex medical needs. You can choose your health plan on the first page of the application, or you can call the HIP Line at
HIP members have a POWER account of $1100 that will be used to pay for their initial health care expenses. The State will contribute to the account and members pay a small percentage of their income (2% - 5%) according to a sliding scale based on family income. When an application is approved, the new member is notified in writing of the amount of the POWER payment.
Your POWER account payment will stay the same during your
Failure to pay may result in termination from the program, and once terminated due to failure to pay, a person cannot come back to the program for
For Additional Information about the Healthy Indiana Plan, call us at
1(877)
Your Rights and Responsibilities as a HIP Applicant and Member
1.Once your signed application is received, federal rules allow 45 days for a decision to be made on your eligibility. We will send you a written Notice explaining whether or not you qualify for HIP. You may appeal and have a fair hearing if you disagree with any decision on your eligibility or if your application is not processed in 45 days.
2.Information you give on the application is kept confidential under state and federal law.
3.A Social Security number (SSN) must be given for each applicant who can legally have a number. An applicant who does not have a number must apply for one. Your SSN will be used to check information kept by the Social Security Administration, the Internal Revenue Service, Workforce Development and other state and federal agencies. We ask for the SSNs of family members not applying for HIP for identification purposes; however you are not required to provide the number.
DFRIGAE02

*DFRIGAE03* |
|
|
|
|
|
|
4.Eligibility for benefits is considered without any regard to race, color, sex, age, disability or national origin. We ask about your
5.Certain information given on your application, such as your income must be verified. If you cannot get the necessary papers, you will need to sign a release form so that we can get them for you.
6.You must provide accurate information. A person who gives false information or misrepresents the truth is committing a crime and can be prosecuted under federal law or state law, or both. The value of benefits received by a person who was not entitled to receive them is subject to recovery by the State.
7.IF YOU MOVE, please tell us your new address so that important mail about your application and membership will reach you without delay. Also, you must tell us if you get health insurance from another source such as Medicare, or if your employer offers health insurance coverage.
8.The immigration status of
9.Your rights to payments for medical care are assigned to the State of Indiana if you are found eligible for HIP. This includes rights to medical support and payment for any medical care that you have on behalf of yourself or your children receiving Hoosier Healthwise/Medicaid.
10.If you believe that you have been discriminated against and wish to file a complaint, you may do so by contacting the Department of Health and Human Services, Regional Manager, Region V, Office for Civil Rights, 233 N. Michigan Ave., Suite 240, Chicago, Illinois, 60601. You may call the Regional Office at (800)
DFRIGAE03
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Title | Application for Healthy Indiana Plan State Form 53421 |
| Governing Law | Indiana Code IC 4-1-8-1 mandates disclosure of Social Security numbers in applications. |
| Eligibility | This application is specifically for adults aged 19 to 64. It does not cover children or pregnant women. |
| Email Communication | Applicants can receive electronic copies of their application or documents if they provide an email address. |
| Health Plan Enrollment | If approved, applicants will be enrolled in a selected health plan, which includes options like Anthem Blue Cross Blue Shield and MHS. |
| Caregiver Expenses | The form allows applicants to report caregiver expenses for dependent children or disabled/elderly adults. |
| Signature Requirement | A signature is mandatory for the application to be considered complete, affirming the truthfulness of the information provided. |
Guidelines on Utilizing Indiana 53421
Filling out the Indiana form 53421 is an important step towards obtaining health coverage through the Healthy Indiana Plan. It’s crucial to provide accurate and complete information to ensure a smooth application process. After submitting the form, you may need to respond to any requests for additional information or documentation that may arise during the review of your application.
- Gather necessary documents: Collect proof of identity, citizenship, and any income sources. This includes documents like a valid driver’s license, birth certificate, pay stubs, or tax returns.
- Use blue or black pen: Gently fill out the application form, making sure to write clearly and legibly throughout.
- Complete each section: Accurately fill in the details for health plan selection, family members residing in your household, and any relevant income details for each applicant.
- Answer health screening questions: Carefully respond to the health screening section, checking either “Yes” or “No” for each applicant’s status regarding health conditions.
- Check residency and care expenses: Indicate whether all applicants live in Indiana and provide details about any payments made for child care or care for dependent adults.
- Sign your name: On page 4, don’t forget to sign and date the application. Your signature certifies that the information provided is accurate.
- Initial if no income: If applicable, initial the space confirming that your family has no income.
- Prepare mailing materials: Place the filled-out application and any photocopied documents into an envelope for mailing, or prepare it for faxing if preferred.
- Return the application: Send your completed application to the FSSA Document Center via mailing, faxing, or deliver it in person at a local office.
Following these steps will help promote an efficient review process for your Healthy Indiana Plan application, placing you one step closer to securing health care coverage.
What You Should Know About This Form
What is the purpose of the Indiana 53421 form?
The Indiana 53421 form, officially titled "Application for Healthy Indiana Plan," is designed for uninsured adults, aged 19 through 64, to apply for health coverage under the Healthy Indiana Plan (HIP). The form requires applicants to provide personal details, including household composition, income information, and any health-related conditions that may affect eligibility. Proper completion of this form allows individuals to receive necessary health coverage if they qualify based on the provided information.
Who should complete the Indiana 53421 form?
The form is intended for adults who do not have health insurance. It is not applicable for children or pregnant women. Those interested in health coverage for children or pregnant women should contact the Indiana Family and Social Services Administration (FSSA) to request a different application specific to those groups, namely the Hoosier Healthwise application. The form must be filled out by individuals who are seeking health coverage for themselves, including necessary demographic and financial information.
What information is required on the Indiana 53421 form?
Applicants must provide several details to complete the Indiana 53421 form. Key information includes personal identification such as name, date of birth, and Social Security number. Additionally, applicants need to identify all adults and children living in the household, their relationship to the applicant, and their citizenship status. Financial information such as income levels, employer information, and any other benefits received should also be reported. The application includes questions related to medical history, which help determine eligibility for specific health coverage plans under HIP.
What happens after submitting the Indiana 53421 form?
Once the form is submitted via mail, fax, or in person, the information will be reviewed by the FSSA. It is important for applicants to respond promptly to any requests for additional information or documentation that may arise during the processing of their application. If the application is approved, individuals will be enrolled in one of the available health plans, and they will receive further details regarding their coverage options and benefits.
Common mistakes
Filling out the Indiana 53421 form, or Application for Healthy Indiana Plan, can be straightforward if you avoid common mistakes. One typical error is not providing a Social Security Number. The form explicitly states that disclosing your Social Security Number is mandatory. Failing to include it will result in your application not being processed.
Another frequent mistake is neglecting to mark your health plan selection. If you skip marking a box next to your chosen plan, it causes delays in enrollment. Furthermore, not signing the application can halt the entire process. Ensure that you sign your name on page 4, question 13, as this step is crucial.
People often make errors regarding household information. It's essential to provide accurate data for all adult members living in your household. Missing or incorrect information about family members can lead to further complications. Each family member’s relationship to the applicant must also be clear to avoid confusion.
A common oversight occurs when applicants misinterpret the health screening questions. Inaccurately answering these questions, or failing to provide clear answers, may affect eligibility for the Enhanced Services Plan. Review these questions carefully before submitting your form.
Some applicants incorrectly state their living arrangements. If any applicants do not reside in Indiana, you must answer “No” to the question about Indiana residency. Providing incorrect residency information can lead to outright disqualification from the program.
Income reporting is another area where mistakes happen. Ensure that you clearly indicate total earnings without neglecting any sources of income. Omitting income details can lead to significant errors in evaluating eligibility and might stall the application.
Finally, not including required supporting documents is a frequent misstep. When submitting the form, include any requested proof of identity, income, or immigration status. A missing document can delay processing and may result in a need for resubmission.
Documents used along the form
The Indiana 53421 form, known as the Application for Healthy Indiana Plan, serves as a crucial document for individuals seeking health coverage in Indiana. Along with the Indiana 53421 form, several other forms and documents may be necessary to ensure a comprehensive application process. Here’s an overview of some commonly associated documents.
- Hoosier Healthwise Application - This application is intended for children and pregnant women who are seeking health coverage under Indiana's Medicaid program. It ensures that families can access necessary healthcare services for their dependents.
- Proof of Identity Documents - Applicants must submit documents to confirm their identity, such as a driver’s license, state ID, or passport. These documents help verify the applicant's identity and eligibility for the program.
- Income Verification Documents - Pay stubs or tax returns may be necessary to establish the household income level. This information is crucial in determining eligibility for the Healthy Indiana Plan.
- Immigration Status Documentation - Non-citizens must provide proof of their immigration status, such as an alien registration card or permanent resident card. This documentation helps determine eligibility for specific health coverage options.
- Guardianship Documents - If someone is applying on behalf of another individual, a Power of Attorney or similar legal document must be provided. This ensures that the representative has the authority to complete the application process.
Gathering and submitting these documents along with the Indiana 53421 form can streamline the application process. Being thorough and organized will significantly enhance the likelihood of timely approval for health coverage.
Similar forms
-
Medicaid Application (Form 2021): Similar to the Indiana 53421 form, the Medicaid Application collects personal data, income, and household member information for individuals seeking health insurance assistance from the state. It also requires disclosure of Social Security numbers and citizenship status.
-
Application for Food Assistance (Form 1330): This form requests detailed information about applicants' household income, expenses, and family members. Like the Indiana 53421, it ensures that applicants meet certain eligibility criteria for government aid.
-
Temporary Assistance for Needy Families (TANF) Application: Also requiring personal information and social security numbers, this application helps determine eligibility for financial assistance programs for low-income families, paralleling aspects of the Indiana 53421 form.
-
Supplemental Nutrition Assistance Program (SNAP) Application: Similar in its function to the Indiana 53421, this form collects information on family size, income, and expenses to determine eligibility for food assistance.
-
Indiana Works Health Coverage Application: This application, much like the Indiana 53421, is designed to enroll low-income adults in health insurance. It collects similar data on gross income and household composition.
-
Low-Income Home Energy Assistance Program (LIHEAP) Application: Like the Indiana 53421 form, the LIHEAP application requires applicants to provide income details and household information to determine eligibility for energy assistance.
-
Child Care Assistance Application: This document requests information about household income and children’s ages, making it similar in structure to the Indiana 53421. Both assessments focus on determining eligibility based on family circumstances.
-
Hoosier Healthwise Application: This form is specifically for children and pregnant women, contrasting with the Indiana 53421. However, both forms share a similar approach in gathering household details and social security information.
-
Indiana State Department of Health Immunization Records Request Form: While focused on health documentation, this request also requires similar personal data from individuals, such as names and dates of birth.
-
Emergency Assistance Application: This form assists individuals facing crises and requests financial information comparable to those required in the Indiana 53421. It assesses eligibility based on immediate and critical needs.
Dos and Don'ts
When filling out the Indiana 53421 form, here are some essential dos and don’ts to keep in mind:
- Do read the instructions carefully before starting.
- Do provide your Social Security Number, as it is mandatory for processing.
- Do fill out the application as completely as possible.
- Do ensure you sign the application on page 4 at question 13.
- Do mark your health plan selection clearly if applicable.
- Don’t forget to provide accurate birth dates and Social Security numbers for all applicants.
- Don’t leave any questions unanswered; all questions must be addressed.
- Don’t submit the application without including necessary documents, as this may delay processing.
- Don’t ignore requests for additional information from the agency after submission.
Misconceptions
- Misconception 1: The Indiana 53421 form is applicable for children and pregnant women.
- Misconception 2: All health plan selections are available to applicants on the Indiana 53421 form.
- Misconception 3: Providing a Social Security Number is optional on the Indiana 53421 form.
- Misconception 4: Completing the health screening questions is not essential for application approval.
This form is specifically designed for adults aged 19 to 64. For children and pregnant women, a different application called the Hoosier Healthwise application must be requested by contacting 1-877-GET HIP9 (1-877-438-4479).
While applicants can indicate their preferred health plan, not all plans may be available in every situation. Upon approval of the application, each applicant will be enrolled in one of the health plans based on eligibility criteria and availability.
In fact, the disclosure of a Social Security Number is mandatory for processing. This requirement is in accordance with specific state laws. Not providing this information will result in the inability to process the application.
The health screening questions are crucial. They determine whether the applicant qualifies for the Enhanced Services Plan, which offers coordinated medical care for those with specialized health care needs. All health screening questions must be answered to consider the application complete.
Key takeaways
Ensure you fill out the Indiana 53421 form completely. Missing information can delay processing.
Sign your application on page 4, question 13. An unsigned application cannot be processed.
This application is for individuals aged 19 to 64 only. Children and pregnant women need a different application.
Choose your health plan carefully. If approved, you'll be enrolled in one of the selected plans, like Anthem or MDwise.
Provide accurate Social Security Numbers for all applicants. This is mandatory for processing the application.
List all household members, including their relationship to you, in the appropriate sections of the form.
Answer all health screening questions honestly. Your answers will aid in determining eligibility for the Enhanced Services Plan.
Attach any required documentation to support your application, such as proof of identity and income. This can speed up processing.
Return your completed form through the designated methods: fax, mail, or drop-off at a local office. Each method has specific instructions to follow.
Browse Other Templates
Adult Adoption Georgia - The form supports both natural and adoptive parents' acknowledgment in the adoption process.
What Is New York Sales Tax - The DTF-95 is not intended for changing your business entity type, so it's important to follow the proper procedures for that.
Maintenance Work Order Form - Provide visual aids or photographs if possible to clarify the issue.