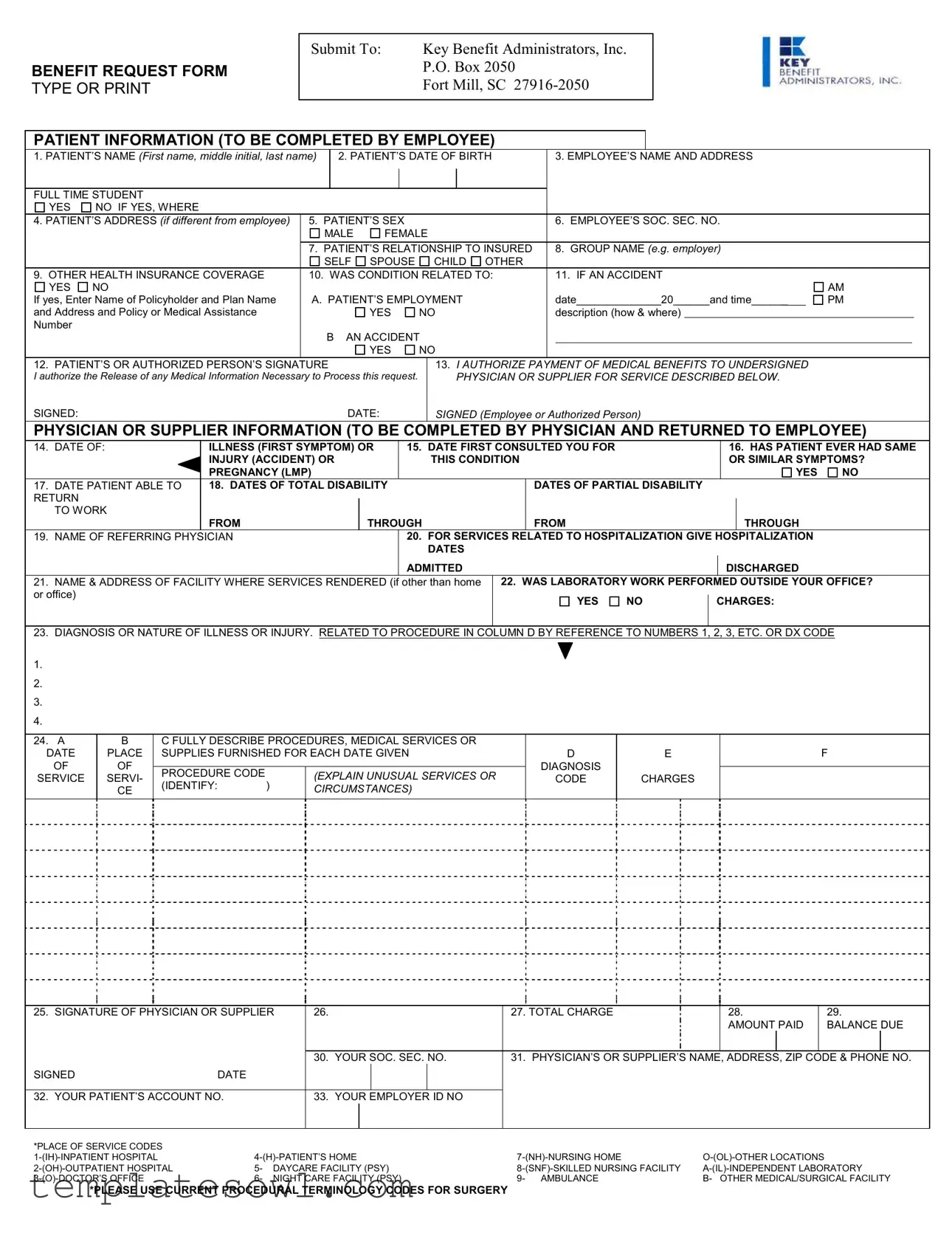
Fill Out Your Key Benefit Request Form
Understanding the Key Benefit Request form is essential for employees seeking medical benefits for themselves or their dependents. This form is structured to collect necessary information in two main sections: Patient Information and Physician or Supplier Information. In the first section, the employee provides details about the patient, including their name, date of birth, and relationship to the employee, as well as answers to questions about their sex, employment status, and any other health insurance coverage. It also requires the employee's social security number to establish eligibility for benefits. The second section is dedicated to the physician or supplier, who must detail the patient's health condition, diagnosis, and the treatment prescribed. Information about hospitalization, disability dates, and diagnostic codes is required to process the request accurately. Additionally, signatures from both the patient (or an authorized individual) and the physician or supplier are required to authorize the release of medical information necessary for processing. This comprehensive approach ensures that all relevant aspects of the patient's medical situation are captured for timely and effective claim management.
Key Benefit Request Example
BENEFIT REQUEST FORM TYPE OR PRINT
Submit To: |
Key Benefit Administrators, Inc. |
|
P.O. Box 2050 |
|
Fort Mill, SC |
|
|
PATIENT INFORMATION (TO BE COMPLETED BY EMPLOYEE)
1. PATIENT’S NAME (First name, middle initial, last name) |
|
2. PATIENT’S DATE OF BIRTH |
|
3. EMPLOYEE’S NAME AND ADDRESS |
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FULL TIME STUDENT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO IF YES, WHERE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. PATIENT’S ADDRESS (if different from employee) |
5. PATIENT’S SEX |
|
|
|
6. EMPLOYEE’S SOC. SEC. NO. |
|
|
|
||||||||
|
|
MALE |
FEMALE |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
7. PATIENT’S RELATIONSHIP TO INSURED |
|
8. GROUP NAME (e.g. employer) |
|
|
|
|||||||||
|
|
SELF |
SPOUSE |
CHILD OTHER |
|
|
|
|
|
|
|
|
||||
9. OTHER HEALTH INSURANCE COVERAGE |
10. WAS CONDITION RELATED TO: |
|
11. IF AN ACCIDENT |
|
|
|
||||||||||
YES |
NO |
|
|
|
|
|
|
|
|
|
|
|
|
AM |
||
If yes, Enter Name of Policyholder and Plan Name |
A. PATIENT’S EMPLOYMENT |
|
date______________20______and time______ |
PM |
||||||||||||
and Address and Policy or Medical Assistance |
|
|
|
YES |
NO |
|
description (how & where) |
|
|
|
|
|
||||
Number |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
AN ACCIDENT |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
YES |
NO |
|
|
|
|
|
|
|
|
||
12. PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE |
|
|
|
13. I AUTHORIZE PAYMENT OF MEDICAL BENEFITS TO UNDERSIGNED |
|
|
|
|||||||||
I authorize the Release of any Medical Information Necessary to Process this request. |
|
PHYSICIAN OR SUPPLIER FOR SERVICE DESCRIBED BELOW. |
|
|
|
|||||||||||
SIGNED:DATE:
SIGNED (Employee or Authorized Person)
PHYSICIAN OR SUPPLIER INFORMATION (TO BE COMPLETED BY PHYSICIAN AND RETURNED TO EMPLOYEE)
14. |
DATE OF: |
ILLNESS (FIRST SYMPTOM) OR |
15. DATE FIRST CONSULTED YOU FOR |
|
|
|
16. HAS PATIENT EVER HAD SAME |
|||||
|
|
INJURY (ACCIDENT) OR |
|
THIS CONDITION |
|
|
|
OR SIMILAR SYMPTOMS? |
||||
|
|
PREGNANCY (LMP) |
|
|
|
|
|
|
|
|
YES |
NO |
17. |
DATE PATIENT ABLE TO |
18. DATES OF TOTAL DISABILITY |
|
|
DATES OF PARTIAL DISABILITY |
|
|
|
|
|
||
RETURN |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
TO WORK |
|
|
|
|
|
|
|
|
|
|
|
|
|
FROM |
THROUGH |
|
FROM |
|
|
|
|
THROUGH |
|
|
19. |
NAME OF REFERRING PHYSICIAN |
|
20. FOR SERVICES RELATED TO HOSPITALIZATION GIVE HOSPITALIZATION |
|
||||||||
|
|
|
|
DATES |
|
|
|
|
|
|
|
|
|
|
|
|
ADMITTED |
|
|
|
|
|
DISCHARGED |
|
|
21. |
NAME & ADDRESS OF FACILITY WHERE SERVICES RENDERED (if other than home |
22. WAS LABORATORY WORK PERFORMED OUTSIDE YOUR OFFICE? |
||||||||||
or office) |
|
|
|
|
YES |
NO |
|
CHARGES: |
|
|||
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
23.DIAGNOSIS OR NATURE OF ILLNESS OR INJURY. RELATED TO PROCEDURE IN COLUMN D BY REFERENCE TO NUMBERS 1, 2, 3, ETC. OR DX CODE
1.
2.
3.
4.
24. A |
B |
C FULLY DESCRIBE PROCEDURES, MEDICAL SERVICES OR |
|
|
|
||
DATE |
PLACE |
SUPPLIES FURNISHED FOR EACH DATE GIVEN |
D |
E |
F |
||
OF |
OF |
|
|
|
DIAGNOSIS |
|
|
PROCEDURE CODE |
|
(EXPLAIN UNUSUAL SERVICES OR |
|
|
|||
SERVICE |
SERVI- |
|
CODE |
CHARGES |
|
||
(IDENTIFY: |
) |
|
|||||
|
CE |
CIRCUMSTANCES) |
|
|
|
||
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
25. SIGNATURE OF PHYSICIAN OR SUPPLIER |
26. |
|
|
|
|
27. TOTAL CHARGE |
|
28. |
|
|
29. |
|
||
|
|
|
|
|
|
|
|
|
|
AMOUNT PAID |
|
BALANCE DUE |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
30. |
YOUR SOC. SEC. NO. |
31. PHYSICIAN’S OR SUPPLIER’S NAME, ADDRESS, ZIP CODE & PHONE NO. |
|||||||||
SIGNED |
DATE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
32. YOUR PATIENT’S ACCOUNT NO. |
|
33. |
YOUR EMPLOYER ID NO |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*PLACE OF SERVICE CODES |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
5- DAYCARE FACILITY (PSY) |
|||||||||||||
|
6- NIGHT CARE FACILITY (PSY) |
9- AMBULANCE |
B- OTHER MEDICAL/SURGICAL FACILITY |
|||||||||||
*PLEASE USE CURRENT PROCEDURAL TERMINOLOGY CODES FOR SURGERY
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Submission | The Key Benefit Request form must be submitted to Key Benefit Administrators, Inc. at their Fort Mill, SC address. |
| Patient Information | The form requires detailed patient information, including the patient's name, date of birth, sex, and relationship to the insured. |
| Insurance Authorization | The employee or authorized person must sign to authorize payment of medical benefits and the release of necessary medical information. |
| Physician's Section | The physician must complete a section that includes information on the patient's condition, dates of visits, and diagnosis. |
| Charges and Payment | The form requires the physician to list charges associated with services rendered and provide details on any amounts paid and the balance due. |
Guidelines on Utilizing Key Benefit Request
Completing the Key Benefit Request form is essential for the processing of requests related to medical benefits. Follow these steps to ensure that all necessary information is properly filled out, which will help facilitate a timely review.
- Patient Information
- Enter the patient’s full name, including first name, middle initial, and last name.
- Provide the patient’s date of birth.
- Include the employee’s name and mailing address.
- Indicate if the patient is a full-time student and, if yes, specify where.
- If the patient’s address is different from the employee’s, fill in the patient’s address.
- Mark the patient’s sex (male or female).
- Fill in the employee’s Social Security number.
- Describe the patient’s relationship to the insured (self, spouse, child, or other).
- Complete the group name, typically the employer’s name.
- Note any other health insurance coverage the patient may have.
- Indicate whether the condition is related to an accident.
- If it was an accident, enter the name of the policyholder and plan name.
- Document the patient’s employment details.
- Provide the date and time of the accident if applicable.
- Gather the signature of the patient or authorized person.
- Physician or Supplier Information
- Record the date of the first symptom or illness.
- Provide the date when the patient first consulted the physician.
- Indicate whether the patient has ever had the same injury or similar symptoms.
- Fill in the date when the patient was able to return to work.
- List the dates of total and partial disability.
- Note the name of the referring physician.
- For hospitalization services, include the dates admitted and discharged.
- Document the name and address of the facility where services were rendered, if it differs from the home or office.
- Clarify if laboratory work was performed outside the physician’s office.
- Detail the diagnosis or nature of illness or injury.
- Describe the procedures, medical services, or supplies furnished, along with the applicable diagnosis codes.
- Collect the physician's or supplier's signature.
- Summarize the total charges, the amount paid, and the balance due.
- Fill in the physician's or supplier's name, address, ZIP code, and phone number.
What You Should Know About This Form
What is the Key Benefit Request form?
The Key Benefit Request form is a document that employees must complete to request medical benefits for covered services. This form collects essential information about the patient, their relationship to the insured, and details of the medical services received.
Who should fill out the form?
The form should be filled out by the employee who is the insured party. It requires information about the patient, who may be the employee themselves, a spouse, a child, or another dependent.
Where do I submit the completed form?
Once you have completed the Key Benefit Request form, submit it to Key Benefit Administrators, Inc. at their address: P.O. Box 2050, Fort Mill, SC 27916-2050. Make sure to double-check that all sections are filled out correctly before sending it off!
What patient information is required on the form?
You will need to provide the patient’s full name, date of birth, sex, address, and the employee's Social Security number. Additionally, kindly indicate the patient’s relationship to the insured and any other health insurance coverage they might have.
What information does the physician need to complete?
The physician must complete several sections related to the patient’s illness or injury. This includes details like the dates of illness, dates of visit, history of the condition, and the diagnosis. They must also provide total charges for the services rendered.
Is there a deadline for submission?
What if I need help filling out the form?
If you need assistance, don't hesitate to reach out to your employer’s HR department or the Key Benefit Administrators directly. They can guide you through the process and clarify any questions about the necessary information.
What happens after I submit the form?
After submission, Key Benefit Administrators will review the request. They will process the claim and determine the benefits that are applicable. If they require further information, they may contact you or your healthcare provider.
How will I know if my claim was approved?
You will typically receive a notification regarding the status of your claim via mail or electronically, depending on the preference you've indicated on your forms. This notification will detail any approvals and payments or will explain any reasons for denial.
What should I do if my claim is denied?
If your claim is denied, review the explanation provided in the notification. You can often appeal the decision. Follow the guidelines outlined in the correspondence, and don’t hesitate to contact Key Benefit Administrators for clarity on the process.
Common mistakes
Filling out the Key Benefit Request form can seem straightforward, but many people make common mistakes that can delay the approval process. One major error is failing to provide complete patient information. It is essential to include all relevant details, such as the patient's full name, date of birth, and social security number. Incomplete information might lead to processing delays or rejections.
Another frequent mistake involves skipping the section about the patient's relationship to the insured. Clearly indicating whether the patient is a spouse, child, or another relative helps the administrators understand the context of the request. Omitting this detail can create confusion and extend the review period.
Not checking the boxes for health insurance coverage and accident-related queries is also a common oversight. If there is other coverage that could contribute to the payment, this must be noted. Additionally, if a condition is related to an accident, clearly marking "yes" and providing necessary details can prevent issues later in the claims process.
Many individuals also neglect to sign the form. A signature is a crucial requirement, as it authorizes the release of medical benefits and verifies that the information provided is accurate. Without a signature, the form may be returned, causing unnecessary delays.
Misunderstanding the instructions regarding the physician or supplier section is another common error. Physicians must fill this out accurately. Any incorrect dates or details about the patient's condition can lead to questions from administrators, delaying payment.
Additionally, individuals often confuse the sections asking for service descriptions and procedure codes. It is vital to provide thorough explanations to assist administrators in understanding the services rendered. Failure to be specific can result in requests for additional information or outright denials.
One should also watch out for missing total charges and payments. Providing a clear breakdown of costs, including any payments made, helps ensure that the correct balance due is calculated. Missing this information can extend the processing time while administrators seek clarification.
Lastly, procrastination is a mistake that many make. Submitting the form promptly can expedite the approval process. Delays in submission can lead to complications, especially if a deadline must be met for benefits to apply. Being proactive can make a significant difference in the outcome.
Documents used along the form
When submitting a Key Benefit Request form, there are several other forms and documents that may be used alongside it to ensure a comprehensive submission. Each document serves a specific purpose in the claims process, helping to provide the necessary information for benefit evaluation.
- Claim Form: A general form used by patients to submit claims for medical services and benefits. This document consolidates essential details about the patient, provider, and services received.
- Explanation of Benefits (EOB): A statement from the insurance company detailing what services were covered, the amount paid, and any balance owed by the patient. This helps clarify how benefits were applied to a claim.
- Patient Medical History Form: A document that records a patient's medical history, including past illnesses, treatments, and surgeries. It provides important context for the current medical issue being addressed.
- Authorization Form: A document that grants permission for the release of a patient’s medical information to the insurance company or third-party payer. This is crucial for processing claims.
- Referral Form: Often required when a patient is referred to a specialist. This form details the reason for referral and aids in ensuring that claims related to specialized care are processed appropriately.
- Provider Invoice: An itemized bill from a healthcare provider that outlines the services rendered and their costs. This document supports the claims process by providing a clear breakdown of expenses.
- Disability Verification Form: A document that confirms a patient’s disability status if the claim is related to disability benefits. This may be required for certain insurance claims.
- Accident Report Form: If the claim is related to an accident, this form provides details about the incident, including dates and circumstances, to establish the background of the condition being treated.
- Pre-Authorization Request: A form submitted to the insurance company to obtain approval for specific treatments or procedures before they occur. This is often necessary for more costly or specialized care.
- Continuation of Care Form: This document summarizes ongoing treatment needs when a patient is transitioning between care providers or levels of care, ensuring that necessary services are not interrupted.
Collectively, these forms and documents facilitate a smoother claims process when the Key Benefit Request form is submitted. Properly filling out and including these additional documents can significantly increase the chances of a successful benefit claim.
Similar forms
Insurance Claim Form: This document serves a similar purpose by requesting payment for medical services from an insurance company. Like the Key Benefit Request form, it requires details about the patient, the medical provider, and the nature of the medical care received.
Medical Authorization Form: Both forms need patient consent for the release of medical information. This authorization is essential for processing requests for benefits or payments, ensuring privacy compliance while allowing for necessary data sharing.
Patient Registration Form: Similar to the Key Benefit Request, this document collects important patient information, such as demographics and insurance details. Both forms are foundational for managing patients’ medical records and facilitating care delivery.
Referral Form: A referral form is often required in medical practices to initiate consultations with specialists. Like the Key Benefit Request, it gathers essential patient information and the nature of the condition, establishing a basis for treatment or reimbursement.
Medicare/Medicaid Application: Those seeking benefits from government programs complete this form, much like the Key Benefit Request. Both forms involve detailed patient and service information to establish eligibility for coverage and payment.
Medical History Form: This document collects extensive information about a patient's medical history and conditions, similar to how the Key Benefit Request form gathers relevant health details to assess the eligibility for benefits.
Treatment Plan: A treatment plan outlines the proposed medical treatment and is often accompanied by financial requests. This document, like the Key Benefit Request, includes conditions, diagnostics, and prognosis, providing context for why benefits are sought.
Dos and Don'ts
When filling out the Key Benefit Request form, it’s important to be careful and thorough. Here are some guidelines to help ensure success:
- Do double-check all patient information for accuracy, including names and dates of birth.
- Do provide a detailed description of the illness or injury, which helps in processing the request.
- Do include your or the patient’s Social Security number to avoid delays.
- Do sign and date the form to validate it and allow for timely processing.
- Don't leave any required fields blank as this can lead to rejection of the request.
- Don't use abbreviations or shorthand language that might confuse the reviewing staff.
- Don't submit without reviewing all information for clarity and completeness.
Misconceptions
Here are some common misconceptions about the Key Benefit Request form, along with clarifications for each:
- The form is only for major surgeries. This form can be used for a wide range of medical services, not just major surgeries. It also applies to regular office visits, treatments, and diagnostic tests.
- You need a lawyer to fill it out. While legal assistance can be beneficial for various situations, completing this form typically does not require legal expertise. Employees can fill it out using provided guidelines.
- Only the physician should complete the form. While part of the form does require physician input, employees must also complete sections related to their personal and patient information.
- The form is too complicated to understand. Many people find the form straightforward. It is organized systematically, guiding users through each section to provide the necessary information clearly.
- Submitting the form guarantees payment. Completing the form does not guarantee payment. Approval depends on the specifics of the insurance policy and the medical services rendered.
- The form must be filled out perfectly to be accepted. While accuracy is important, minor errors can often be corrected after submission. It is advisable to double-check for mistakes before sending it in.
- Only full-time employees can request benefits. Dependents covered under an employee's healthcare plan may also be eligible for benefit requests, regardless of the employee's status.
- All medical issues require the same documentation. Different conditions may require various supporting documents. Always check what is necessary for each specific case.
- The form can be submitted electronically or by mail. It must be submitted by mail, as per the instructions on the form. Ensure it is sent to the correct address to avoid delays in processing.
Key takeaways
Filling out the Key Benefit Request form can seem daunting, but understanding its key components can make the process smoother. Here are nine essential takeaways:
- Incomplete Forms May Cause Delays: Ensure that every section of the form is filled out completely. An incomplete submission can lead to unnecessary holdups in processing your request.
- Accurate Patient Information is Vital: Provide accurate patient details, including full name, date of birth, and address. This information is necessary to verify insurance eligibility and benefits.
- Relationship to Insured: Clearly indicate the patient’s relationship to the insured individual. This helps in assessing coverage options effectively.
- Other Insurance Coverage: If applicable, disclose any other health insurance coverage. This can affect how benefits are coordinated and can maximize coverage options.
- Document Medical History: When filling out the section on prior illnesses or injuries, be honest and thorough. This might impact the processing of your current claim.
- Signature Requirements: Both the patient (or authorized person) and the physician need to sign the form. Without these signatures, your request cannot be processed.
- Detailed Medical Information Needed: Provide all relevant dates and descriptions of the medical condition or injuries. This aids in determining the legitimacy and extent of the claim.
- Charges and Payment Information: Clearly outline all charges, ensuring that they align with the services provided. Knowing the billing amount can help avoid surprises.
- Submit Timely: Send the completed form to Key Benefit Administrators promptly. Meeting submission deadlines can prevent disruptions in benefit coverage.
By following these guidelines, you will enhance your chances of a successful and timely benefits request. Remember to keep a copy of the completed form for your records.
Browse Other Templates
Utah Employer Id - New business name changes require accompanying documentation from the Department of Commerce as indicated.
Dme Form - Efficient monitoring of service costs is facilitated through this form.