Fill Out Your Massachusetts Molst Form
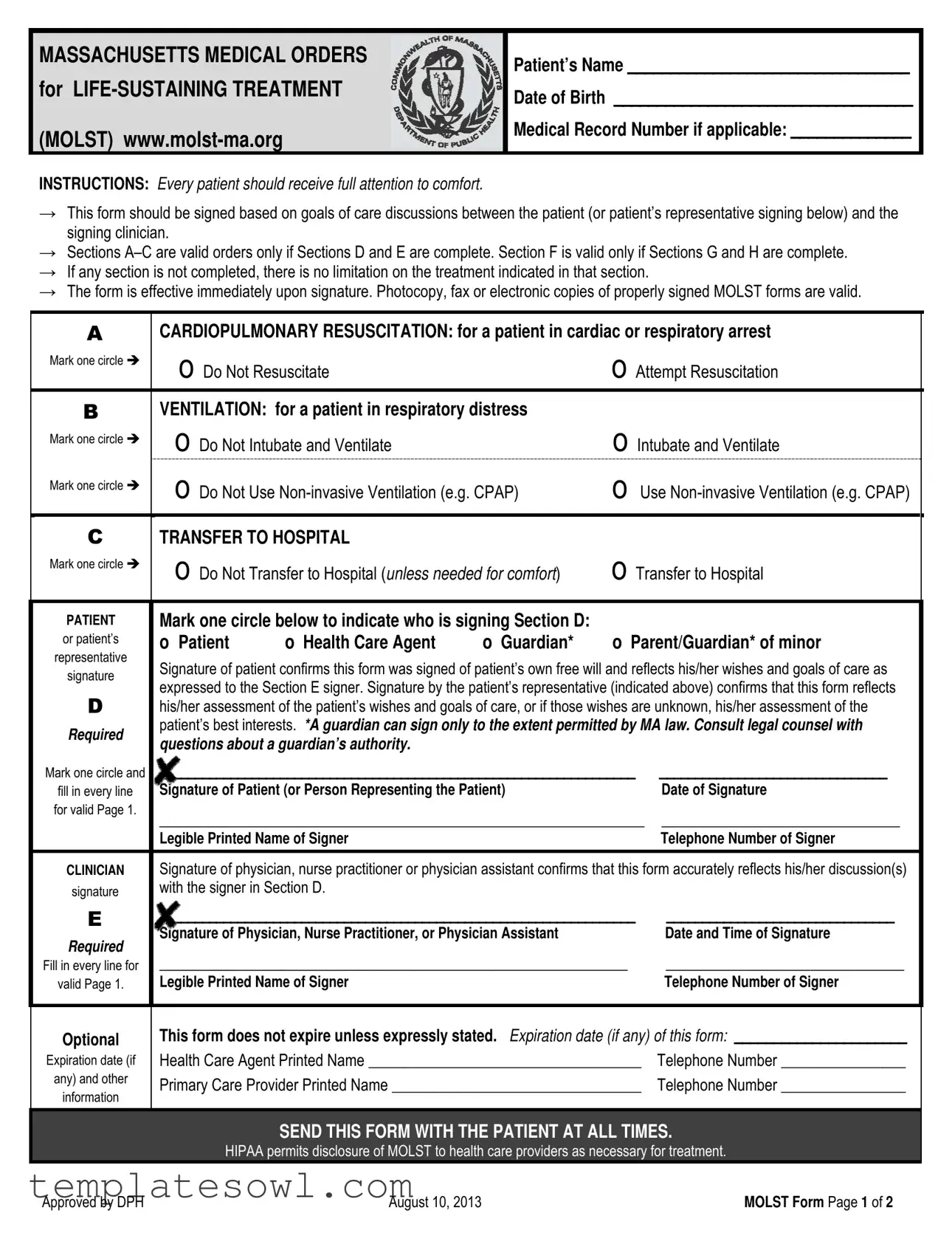
The Massachusetts Medical Orders for Life-Sustaining Treatment (MOLST) form serves as a crucial tool in facilitating conversations about end-of-life care between patients and healthcare providers. It allows individuals to express their preferences for medical treatment in a clear and legally binding manner. The form is organized into several sections that outline specific medical orders based on the patient's wishes, including choices related to resuscitation, ventilation, and hospital transfer. Importantly, sections A through C of the form become valid only when sections D and E are complete, ensuring that patient intentions are thoroughly documented and respected. For those unable to sign, a designated representative may do so, affirming their understanding of the patient's desires. Each section must be meticulously filled out since any omissions may lead to unintended treatment limitations. This form becomes effective immediately upon signature, and its widespread recognition by emergency medical personnel across Massachusetts underscores the importance of using the correct version printed on bright or fluorescent pink paper. Overall, the MOLST form embodies a comprehensive approach to guiding healthcare decisions in alignment with patients' values and goals.
Massachusetts Molst Example
MASSACHUSETTS MEDICAL ORDERS for
(MOLST)
Patient’s Name _________________________________
Date of Birth ___________________________________
Medical Record Number if applicable: ______________
INSTRUCTIONS: Every patient should receive full attention to comfort.
→This form should be signed based on goals of care discussions between the patient (or patient’s representative signing below) and the signing clinician.
→Sections
→If any section is not completed, there is no limitation on the treatment indicated in that section.
→The form is effective immediately upon signature. Photocopy, fax or electronic copies of properly signed MOLST forms are valid.
ACARDIOPULMONARY RESUSCITATION: for a patient in cardiac or respiratory arrest
Mark one circle |
o Do Not Resuscitate |
o Attempt Resuscitation |
|
|
|||
B |
VENTILATION: for a patient in respiratory distress |
|
|
Mark one circle |
o Do Not Intubate and Ventilate |
o Intubate and Ventilate |
|
|
|
||
Mark one circle |
o Do Not Use |
o Use |
|
|
|
||
|
|
|
|
CTRANSFER TO HOSPITAL
Mark one circle |
o Do Not Transfer to Hospital (unless needed for comfort) |
o Transfer to Hospital |
||||
|
||||||
|
|
|
|
|||
PATIENT |
Mark one circle below to indicate who is signing Section D: |
|
|
|||
or patient’s |
o Patient |
o Health Care Agent |
o Guardian* |
o Parent/Guardian* of minor |
||
representative |
||||||
Signature of patient confirms this form was signed of patient’s own free will and reflects his/her wishes and goals of care as |
||||||
signature |
||||||
expressed to the Section E signer. Signature by the patient’s representative (indicated above) confirms that this form reflects |
||||||
|
||||||
D |
his/her assessment of the patient’s wishes and goals of care, or if those wishes are unknown, his/her assessment of the |
|||||
Required |
patient’s best interests. *A guardian can sign only to the extent permitted by MA law. Consult legal counsel with |
|||||
questions about a guardian’s authority. |
|
|
|
|||
|
|
|
|
|||
Mark one circle and |
___________________________________________________________________ |
________________________________ |
||||
fill in every line |
Signature of Patient (or Person Representing the Patient) |
|
Date of Signature |
|||
for valid Page 1. |
_________________________________________________________ |
____________________________ |
||||
|
||||||
|
Legible Printed Name of Signer |
|
|
Telephone Number of Signer |
||
|
|
|||||
CLINICIAN |
Signature of physician, nurse practitioner or physician assistant confirms that this form accurately reflects his/her discussion(s) |
|||||
signature |
with the signer in Section D. |
|
|
|
||
E |
___________________________________________________________________ |
________________________________ |
||||
Required |
Signature of Physician, Nurse Practitioner, or Physician Assistant |
|
Date and Time of Signature |
|||
|
|
|
|
|
||
Fill in every line for |
_______________________________________________________ |
____________________________ |
||||
valid Page 1. |
Legible Printed Name of Signer |
|
|
Telephone Number of Signer |
||
|
|
|
|
|
|
|
Optional
Expiration date (if
any) and other
information
This form does not expire unless expressly stated. Expiration date (if any) of this form: ______________________
Health Care Agent Printed Name ___________________________________ |
Telephone Number ________________ |
Primary Care Provider Printed Name ________________________________ |
Telephone Number ________________ |
SEND THIS FORM WITH THE PATIENT AT ALL TIMES.
HIPAA permits disclosure of MOLST to health care providers as necessary for treatment.
Approved by DPH |
August 10, 2013 |
MOLST Form Page 1 of 2 |
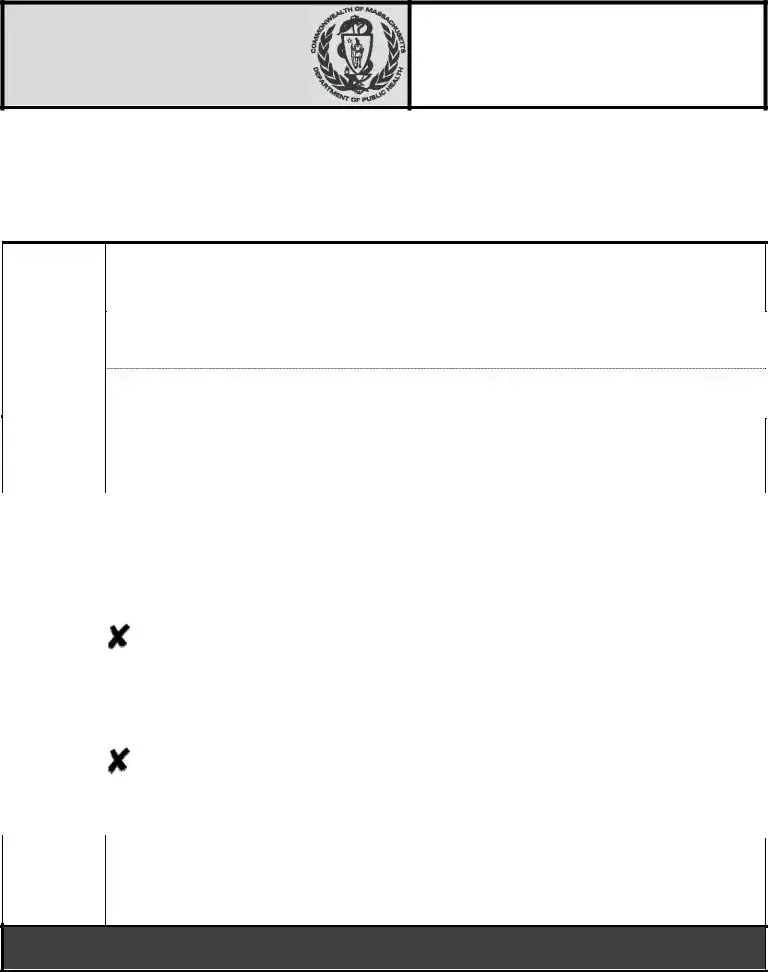
Patient’s Name: ______________________ Patient’s DOB ___________ Medical Record # if applicable__________________
FStatement of Patient Preferences for Other
INTUBATION AND VENTILATION
Mark one circle |
O Refer to Section B |
on |
|
O Use intubation and ventilation as marked |
|
O Undecided |
|
||
|
Page 1 |
|
|
in Section B, but short term only |
|
|
O Did not discuss |
|
|
|
|
|
|
|
|
||||
|
|
||||||||
Mark one circle |
O Refer to Section B |
on |
|
O Use |
|
O Undecided |
|
||
|
|
|
|||||||
|
Page 1 |
|
|
Section B, but short term only |
|
|
O Did not discuss |
|
|
|
DIALYSIS |
|
|
|
|
|
|
|
|
Mark one circle |
O No dialysis |
|
|
O Use dialysis |
|
|
|
O Undecided |
|
|
|
|
O Use dialysis, but short term only |
|
|
O Did not discuss |
|
||
|
|
|
|
|
|
|
|||
|
ARTIFICIAL NUTRITION |
|
|
|
|
|
|
|
|
Mark one circle |
O No artificial nutrition |
|
O Use artificial nutrition |
|
|
O Undecided |
|
||
|
|
|
|
||||||
|
|
|
|
O Use artificial nutrition, but short term only |
|
O Did not discuss |
|
||
|
ARTIFICIAL HYDRATION |
|
|
|
|
|
|
|
|
Mark one circle |
O No artificial hydration |
|
O Use artificial hydration |
|
|
O Undecided |
|
||
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
O Use artificial hydration, but short term only |
|
O Did not discuss |
|
||
|
Other treatment preferences specific to the patient’s medical condition and care |
________________________________ |
|
||||||
|
_______________________________________________________________________________________________ |
|
|||||||
|
_______________________________________________________________________________________________ |
|
|||||||
|
|
|
|
|
|
||||
PATIENT |
Mark one circle below to indicate who is signing Section G: |
|
|
|
|
||||
or patient’s |
o Patient |
o Health Care Agent |
o Guardian* |
o Parent/Guardian* of minor |
|
||||
representative |
|
||||||||
|
|
|
|
|
|
|
|
|
|
signature |
Signature of patient confirms this form was signed of patient’s own free will and reflects his/her wishes and goals of care as |
|
|||||||
|
expressed to the Section H signer. Signature by the patient’s representative (indicated above) confirms that this form reflects |
|
|||||||
G |
his/her assessment of the patient’s wishes and goals of care, or if those wishes are unknown, his/her assessment of the |
|
|||||||
patient’s best interests. *A guardian can sign only to the extent permitted by MA law. Consult legal counsel with |
|
||||||||
Required |
|
||||||||
questions about a guardian’s authority. |
|
|
|
|
|
||||
|
|
|
|
|
|
||||
Mark one circle and |
_______________________________________________________ |
____________________________ |
|
||||||
Signature of Patient (or Person Representing the Patient) |
|
|
Date of Signature |
|
|||||
fill in every line |
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
for valid Page 2. |
_______________________________________________________ |
____________________________ |
|
||||||
|
Legible Printed Name of Signer |
|
|
|
|
|
Telephone Number of Signer |
|
|
|
|
|
|||||||
CLINICIAN |
Signature of physician, nurse practitioner or physician assistant confirms that this form accurately reflects his/her |
|
|||||||
signature |
discussion(s) with the signer in Section G. |
|
|
|
|
|
|||
H |
_______________________________________________________ |
____________________________ |
|
||||||
Signature of Physician, Nurse Practitioner, or Physician Assistant |
|
|
Date and Time of Signature |
|
|||||
|
|
|
|
||||||
Required |
_______________________________________________________ |
____________________________ |
|
||||||
Fill in every line for |
|
||||||||
Legible Printed Name of Signer |
|
|
|
|
|
Telephone Number of Signer |
|
||
valid Page 2. |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional Instructions For Health Care Professionals
→Follow orders listed in A, B and C and honor preferences listed in F until there is an opportunity for a clinician to review as described below.
→Any change to this form requires the form to be voided and a new form to be signed. To void the form, write VOID in large letters across both sides of the form. If no new form is completed, no limitations on treatment are documented and full treatment may be provided.
→
→The patient or health care agent (if the patient lacks capacity), guardian*, or parent/guardian* of a minor can revoke the MOLST form at any time and/or request and receive previously refused
Consult legal counsel with questions about a guardian’s authority.
Approved by DPH |
August 10, 2013 |
MOLST Form Page 2 of 2 |
IMPORTANT INFORMATION ABOUT MASSACHUSETTS MOLST
The Massachusetts MOLST form is a MA DPH‐approved standardized medical order form for use by licensed Massachusetts physicians, nurse practitioners and physician assistants.
While MOLST use expands in Massachusetts, health care providers are encouraged to inform patients that EMTs honor MOLST statewide, but that systems to honor MOLST may still be in development in some Massachusetts health care institutions.
PRINTING THE MASSACHUSETTS MOLST FORM
⎯Do not alter the MOLST form. EMTs have been trained to recognize and honor the standardized MOLST form. The best way to assure that MOLST orders are followed by emergency medical personnel is to download and reproduce the standardized form found on the MOLST web site.
⎯Print original Massachusetts MOLST forms on bright or fluorescent pink paper for maximum visibility.
Astrobrights® Pulsar Pink* is the color highly recommended for original MOLST forms. EMTs are trained to look for the bright pink MOLST form before initiating life‐sustaining treatment with patients.
⎯Print the MOLST form (pages 1 and 2) as a double‐sided form on a single sheet of paper.
⎯Provide an electronic version of the downloaded MOLST form to your institution’s forms department or to personnel responsible for copying/providing forms in your institution.
FOR CLINICIANS: BEFORE USING MOLST
MOLST requires a physician, nurse practitioner, or physician assistant signature to be valid. This signature confirms that the MOLST accurately reflects the signing clinician’s discussion(s) with the patient. The MOLST form should be filled out and signed only after in‐depth conversation between the patient and the clinician signer.
Before using MOLST:
⎯Access the Clinician Checklist for Using MOLST with Patients at: http://www.molst‐ma.org/health‐ care‐professionals/guidance‐for‐using‐molst‐forms‐with‐patients.
⎯Listen to MOLST Overview for Health Professionals at: http://www.molst‐ma.org/molst‐training‐line.
⎯Access the MOLST website at: http://www.molst‐ma.org periodically for MOLST form updates.
⎯For more information about Massachusetts MOLST or the Massachusetts MOLST form, visit http://www.molst‐ma.org.
* Astrobrights® Pulsar Pink paper can be purchased from office suppliers, including:
Staples ‐ Item #491620 Wausau™ Astrobrights® Colored Paper, 8 1/2" x 11", 24 Lb, Pulsar Pink, in stores or at http://www.staples.com, and
Office Depot – Item #420919 Astrobrights® Bright Color Paper, 8 1/2 x 11, 24 Lb, FSC Certified Pulsar Pink, in stores or at http://www.officedepot.com.
August 10, 2013 |
MOLST Instructions Page 1 of 1 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | The Massachusetts MOLST form is designed to communicate a patient's preferences regarding life-sustaining treatment. |
| Governing Law | The MOLST form is governed by Massachusetts General Laws, Chapter 201D. |
| Who Can Sign | Patients or their representatives, including health care agents or guardians, can sign the form. |
| Immediate Effect | The MOLST form takes effect immediately after being signed by the patient or their representative. |
| Emergency Medical Services | Emergency Medical Technicians (EMTs) are trained to honor the MOLST form during emergencies. |
| Validity of Copies | Photocopies, faxes, or electronic versions of the signed MOLST are considered valid. |
| Completion Requirement | Sections A–C are only valid if Sections D and E are also completed appropriately. |
| Expiration | The MOLST form does not have a set expiration date unless specifically noted on the form. |
| Visibility | Original MOLST forms should be printed on bright or fluorescent pink paper for easy identification. |
Guidelines on Utilizing Massachusetts Molst
Filling out the Massachusetts MOLST form requires thoughtful consideration and collaboration between the patient and their healthcare provider. This process ensures that the patient's wishes regarding medical treatment are clearly articulated and respected. By following these detailed steps, you can successfully complete the form, enabling effective communication regarding life-sustaining treatment preferences.
- Begin by entering the Patient’s Name, Date of Birth, and Medical Record Number (if applicable) at the top of the form.
- Discuss the patient's goals of care with them or their representative to understand their preferences fully.
- In Section A, mark one circle to indicate if the patient wants Do Not Resuscitate or Attempt Resuscitation.
- In Section B, choose the desired options for Ventilation (Intubation and Ventilation vs. Do Not Intubate and Ventilate). Additionally, decide about use of non-invasive ventilation.
- In Section C, indicate whether the patient should Transfer to Hospital or Not Transfer (unless for comfort).
- Proceed to Section D and indicate the person signing this section (Patient, Health Care Agent, Guardian, or Parent/Guardian of a minor).
- Ensure the signer provides their signature, date of signature, and legible printed name in the designated fields.
- In Section E, have the clinician sign the form, verifying the accuracy of the discussions had regarding the patient's wishes.
- In Section F, address any other treatment preferences such as Dialysis, Artificial Nutrition, and Artificial Hydration. Mark circles as needed to indicate the patient's wishes.
- Once again, indicate who is signing for Section G, using the same options as Section D.
- Complete Section G by having the signer provide their signature, date, and printed name.
- Next, have the clinician sign Section H, ensuring they confirm the discussions held with the signer.
- Gather any necessary contact information for a Health Care Agent and Primary Care Provider if applicable.
- Make sure to send the completed form with the patient at all times.
Completing the MOLST form is only the beginning of ensuring that a patient's healthcare preferences are respected. Once filled out, it is important to regularly revisit the discussions surrounding care goals to ensure they align with the patient’s evolving wishes and needs.
What You Should Know About This Form
What is the Massachusetts MOLST form?
The Massachusetts Medical Orders for Life-Sustaining Treatment (MOLST) form is a standardized medical order that helps communicate a patient’s preferences regarding life-sustaining treatments. This form is designed for use by licensed healthcare professionals like physicians, nurse practitioners, and physician assistants in Massachusetts. It ensures that a patient’s wishes are honored in emergency and healthcare settings.
Who can complete and sign the MOLST form?
The MOLST form can be completed and signed by a patient, a healthcare agent, a guardian, or a parent or guardian of a minor. The signer must ensure that the form accurately reflects the patient’s wishes and goals for care. The signature by a clinician confirms that they have discussed the form with the signer, thereby validating it.
How does the MOLST form differ from an advance directive?
An advance directive typically outlines a person's wishes for healthcare decisions and designates an agent to make those decisions on their behalf. In contrast, the MOLST form is a physician's medical order that provides specific instructions for healthcare providers concerning immediate medical treatment. MOLST is often utilized when a patient has a serious medical condition or is near the end of life.
Is the MOLST form legally binding?
Yes, the MOLST form is legally binding once it is signed by the patient and their healthcare provider. It is effective immediately upon signature, and healthcare professionals are obligated to follow the orders as indicated on the form, as long as it is completed correctly.
What happens if a MOLST form is incomplete?
If any section of the MOLST form is not completed, there are no limitations on the treatment provided in that section. This means healthcare providers can proceed with full treatment unless expressly indicated otherwise in the form. Completing all necessary sections is crucial to ensure that the patient's wishes are respected.
Can the MOLST form be changed or revoked?
A patient or their representative can change or revoke the MOLST form at any time. If a change is needed, the previous form must be voided, indicating this clearly by writing "VOID" across both sides. A new form can then be completed to reflect the updated wishes of the patient.
Where should the MOLST form be kept?
The MOLST form should accompany the patient at all times and be presented to healthcare providers as needed. Making sure that EMTs and healthcare facilities have access to the form is essential for honoring the patient’s treatment preferences, especially in emergency situations.
What should be done if the MOLST form is not honored?
If the MOLST form is not honored, patients or their representatives should contact the healthcare institution's administration or file a complaint with the relevant health department. Ensuring that the MOLST form is recognized is critical for safeguarding patient rights and wishes in medical treatment scenarios.
Is there a specific paper that should be used for the MOLST form?
Yes, it is recommended to print the Massachusetts MOLST form on bright or fluorescent pink paper to ensure maximum visibility. Emergency medical personnel are trained to look for this bright pink color when identifying the MOLST form, making it a crucial factor in ensuring the form is honored.
Common mistakes
Completing the Massachusetts MOLST (Medical Orders for Life-Sustaining Treatment) form is a critical task that requires attention to detail. Unfortunately, many people make mistakes when filling out this important document. Here are seven common errors to avoid.
One frequent mistake is not completing all relevant sections. Sections A through C only hold validity if Sections D and E are fully filled out. If even a single section is left incomplete, the treatment indicated may not apply. This means patients might unwittingly opt for full treatment when they intended to choose otherwise. Always ensure that all sections are properly filled in before submitting.
Another common issue arises from the failure to fully understand the role of the signing clinician. It is essential that the clinician's signature follows an in-depth discussion about the patient's wishes. Without this understanding, the form may not accurately reflect the patient's goals of care, leading to potentially unwanted medical interventions.
People also often forget to specify who is signing on behalf of the patient. Is it the patient, a health care agent, or a guardian? This distinction is crucial because different rules apply to various representatives. Always mark the appropriate circle to clarify who has the authority to sign the form, as it can impact the legal validity of the document.
Additionally, individuals frequently neglect to provide legible printed names. An illegible name can lead to confusion and complications, particularly in emergency situations where quick decision-making is vital. Ensure that all signatures and corresponding printed names are clear and easy to understand.
Another common oversight involves the expiration date. If an expiration date is necessary, it must be explicitly stated on the form. Forgetting to include this information can lead to misunderstandings regarding the validity of the MOLST when it's needed most.
Using the wrong paper is a less obvious but significant error as well. The MOLST form should be printed on bright or fluorescent pink paper to ensure maximum visibility. If the form is printed on standard white paper, it might not be recognized by emergency medical personnel, which can jeopardize a patient’s care.
Lastly, failing to communicate updates or changes to health care providers can lead to serious complications. The patient's preferences should be revisited as their medical condition evolves. If a patient's wishes change, ensuring that this is accurately captured in an updated MOLST form is essential. Regular discussions with the care team can prevent confusion and ensure that the patient’s current preferences are honored.
Being mindful of these common mistakes can help ensure that the MOLST form accurately reflects a patient’s wishes. This careful attention to detail allows for better patient care and helps honor the individual's rights and preferences in life-sustaining treatment decisions.
Documents used along the form
The Massachusetts MOLST form is an important document that conveys a patient's preferences regarding life-sustaining treatments. In addition to this form, several other related documents can enhance care planning and communication. Below is a list of forms often used alongside the MOLST form, each serving a distinct purpose in the healthcare process.
- Advance Directive: This document allows individuals to specify their preferences for medical treatment in situations where they cannot communicate. It typically includes a living will and a durable power of attorney for healthcare.
- Health Care Proxy: A health care proxy designates a specific person to make medical decisions on behalf of a patient if they become unable to do so. This document ensures that decisions align with the patient’s wishes.
- Living Will: A living will outlines specific medical treatments a person wishes to receive or refuse in case of terminal illness or incapacitation. It provides guidance to family members and healthcare providers.
- Do Not Resuscitate (DNR) Order: This order communicates a patient’s wish not to receive CPR or other resuscitative measures in the event of a cardiac or respiratory arrest. Unlike the MOLST form, it typically applies specifically to resuscitation efforts.
- Physician Orders for Life-Sustaining Treatment (POLST): Similar to the MOLST, this form provides healthcare professionals with medical orders based on a patient’s preferences for life-sustaining treatments. It is designed for individuals with serious illnesses.
- Patient Release of Information Form: This document allows a patient to authorize the sharing of their medical information with healthcare providers or family members. Ensuring that the right people have access to important health information is vital for coordinated care.
Each of these documents plays a significant role in ensuring that a patient's healthcare preferences are respected and documented. When used together, they create a comprehensive approach to advance care planning, making it easier for patients and their loved ones to navigate difficult medical decisions.
Similar forms
The Massachusetts MOLST (Medical Orders for Life-Sustaining Treatment) form shares similarities with several other documents that cater to patients' medical preferences and end-of-life decisions. Here’s a list of nine such documents:
- Advance Directive: This document allows individuals to outline their medical preferences and appoint a healthcare proxy, similar to the MOLST, which also emphasizes patient wishes regarding treatment.
- Living Will: Like the MOLST, a living will provides instructions about the types of medical treatment a person wants or doesn’t want, focusing on end-of-life care.
- Durable Power of Attorney for Health Care: This document enables a person to designate someone else to make healthcare decisions on their behalf, akin to how a healthcare agent can be appointed in the MOLST.
- Do Not Resuscitate (DNR) Order: Much like the MOLST, a DNR order communicates preferences regarding resuscitation efforts in case of cardiac arrest, ensuring that patient wishes are respected.
- Physician Orders for Life-Sustaining Treatment (POLST): Similar in name and function, POLST forms are used in several states to specify patient treatment preferences, just like the MOLST form does in Massachusetts.
- Emergency Medical Services (“EMS”) Protocol: EMS protocols often include guidelines for honoring patient directives such as MOLST when responding to emergencies.
- End-of-Life Care Plan: This comprehensive plan outlines medical treatments and support a patient wishes to receive at the end of their life, resonating with the goals of care expressed in the MOLST.
- Patient Advocate Designation: This allows individuals to appoint someone to advocate for their medical interests, paralleling the role of healthcare agents in a MOLST form.
- Healthcare Preferences Communication: This informal agreement or document allows individuals to communicate their healthcare preferences to family and teams, akin to the discussions that inform a MOLST form.
Dos and Don'ts
- Do have a thorough discussion with the patient about their wishes before filling out the form.
- Do ensure that all relevant sections of the form are complete.
- Do use the standardized MOLST form downloaded from the official website.
- Do print the form on bright or fluorescent pink paper for visibility.
- Do include signatures from both the patient (or their representative) and the clinician.
- Don’t change any part of the MOLST form as it is standardized and recognized by EMTs.
- Don’t leave any section incomplete; it could lead to unintended treatment decisions.
- Don’t use a previously filled-out form; always complete a new, valid form.
- Don’t assume that verbal permissions are enough—document everything in writing.
- Don’t forget to send a copy of the form with the patient at all times for continuity of care.
Misconceptions
- MOLST forms only apply in hospitals. Many people believe that MOLST forms are only valid in hospital settings. In reality, these forms are recognized and honored by Emergency Medical Technicians (EMTs) throughout Massachusetts, regardless of where the patient is located.
- Patients must use MOLST forms if they want to refuse treatment. Another common misconception is that a MOLST form is required to refuse life-sustaining treatments. While a MOLST form is an excellent tool for outlining a patient's wishes, individuals can refuse treatments even in the absence of this form. However, having it can ensure those wishes are documented and honored more consistently.
- MOLST forms are permanent and cannot be changed. Some people think that once a MOLST form is signed, it cannot be modified or revoked. This is not true. Patients or their authorized representatives can revoke or change a MOLST form at any time, allowing for adjustments as their treatment preferences evolve.
- Anyone can complete a MOLST form. A final misconception is that anyone can fill out a MOLST form. However, it is crucial that this form be completed and signed by a licensed clinician, such as a physician, nurse practitioner, or physician assistant. Their signature ensures that the patient’s wishes are accurately reflected and understood following detailed discussions.
Key takeaways
Here are some key takeaways regarding the Massachusetts MOLST form:
- The MOLST form is an official document that outlines a patient’s preferences for life-sustaining treatment.
- Patients, or their authorized representatives, must sign the form after discussing it with a clinician.
- Sections A-C are considered valid only if Sections D and E are completed.
- The form is effective immediately upon being signed and can be copied or faxed for use.
- Health care providers are required to honor the preferences stated in the form until it is reviewed by a clinician.
- The MOLST form should be printed on bright pink paper to improve visibility for EMTs and other providers.
- A guardian can sign the form only within the limits of Massachusetts law; seeking legal advice is recommended if there are questions.
- The MOLST form does not expire unless an expiration date is explicitly stated within it.
- Patients or their representatives can revoke the MOLST form at any time or request previously refused treatments.
- Regular discussions about care preferences should occur as a patient's health condition changes.
This overview aims to provide clarity and assurance regarding the proper use of the Massachusetts MOLST form.
Browse Other Templates
How Much Does It Cost to Transfer a Title in Pa - Different registration periods are available: one year or two years.
Dd Form 2860 Example - Applicants must carefully complete the entire form and provide accurate information.