Fill Out Your Medco Health Form
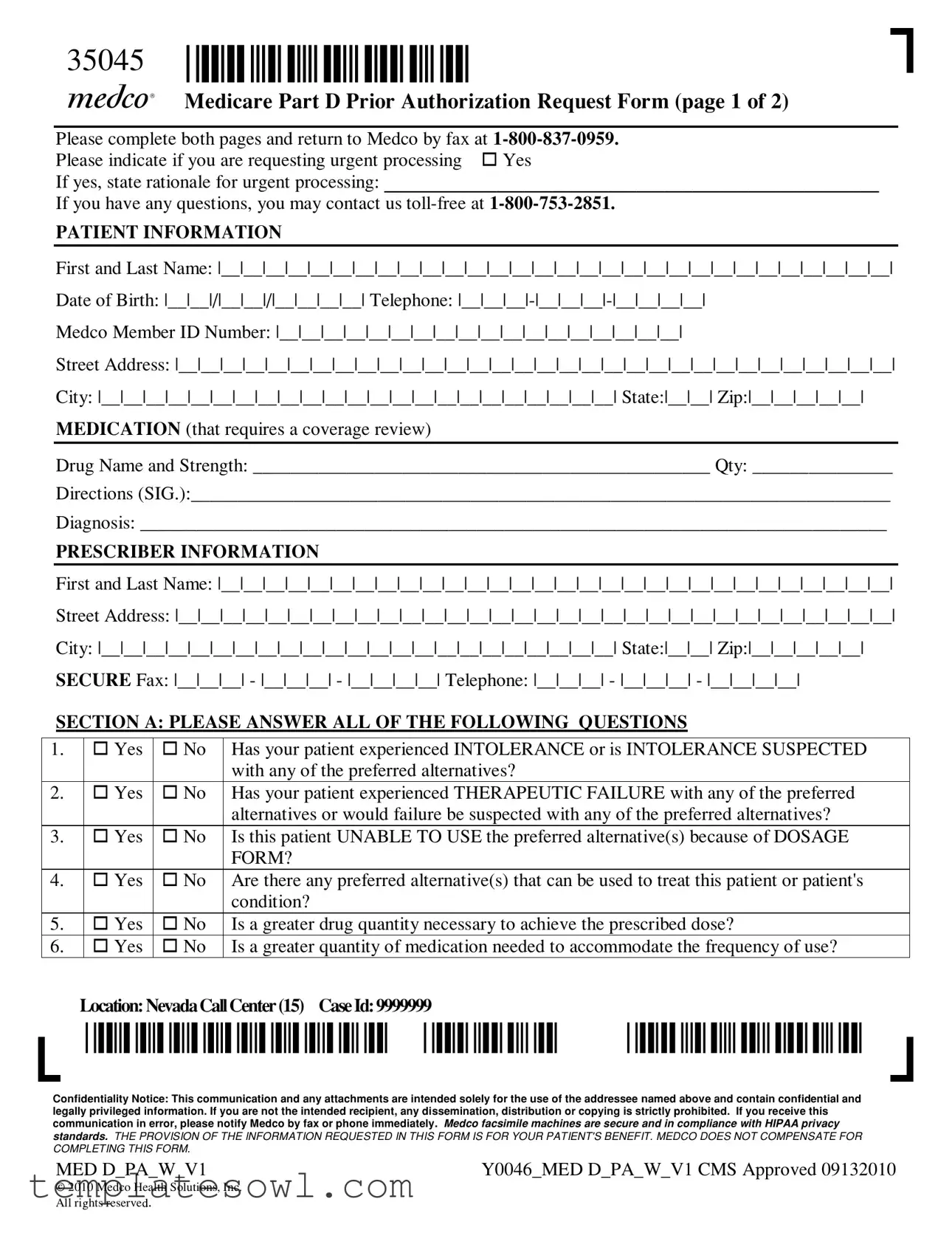
The Medco Health form is an essential tool for patients and healthcare providers seeking prior authorization for medications covered under Medicare Part D. It consists of two pages in which users must provide critical patient and prescriber information, including names, medical history, and medication details. Sections within the form address various crucial questions that determine the necessity and appropriateness of the requested medication. For instance, providers must indicate if the patient has experienced any intolerance to preferred alternatives or if therapeutic failure with those alternatives has occurred. Additional sections specifically target patients using immunosuppressant medications and chemotherapy agents, requiring further clarification of treatment rationale. By faxing the completed form to Medco, healthcare providers initiate the review process, which is crucial for ensuring patients receive the medications they require. Prompt and accurate completion of the form helps facilitate a smoother approval process, benefiting patients and their ongoing healthcare plans.
Medco Health Example
35045 |
*35045* |
|
|
Medicare Part D Prior Authorization Request Form (page 1 of 2) |
|
|
||
Please complete both pages and return to Medco by fax at |
||
Please indicate if you are requesting urgent processing |
Yes |
|
If yes, state rationale for urgent processing: _____________________________________________________
If you have any questions, you may contact us
PATIENT INFORMATION
First and Last Name: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
Date of Birth: |__|__|/|__|__|/|__|__|__|__| Telephone:
Medco Member ID Number: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
Street Address: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
City: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__| State:|__|__| Zip:|__|__|__|__|__| MEDICATION (that requires a coverage review)
Drug Name and Strength: _________________________________________________ Qty: _______________
Directions (SIG.):___________________________________________________________________________
Diagnosis: ________________________________________________________________________________
PRESCRIBER INFORMATION
First and Last Name: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
Street Address: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
City: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__| State:|__|__| Zip:|__|__|__|__|__|
SECURE Fax: |__|__|__| - |__|__|__| - |__|__|__|__| Telephone: |__|__|__| - |__|__|__| - |__|__|__|__|
SECTION A: PLEASE ANSWER ALL OF THE FOLLOWING QUESTIONS
1. |
Yes |
No |
Has your patient experienced INTOLERANCE or is INTOLERANCE SUSPECTED |
|
|
|
with any of the preferred alternatives? |
2. |
Yes |
No |
Has your patient experienced THERAPEUTIC FAILURE with any of the preferred |
|
|
|
alternatives or would failure be suspected with any of the preferred alternatives? |
3. |
Yes |
No |
Is this patient UNABLE TO USE the preferred alternative(s) because of DOSAGE |
|
|
|
FORM? |
4. |
Yes |
No |
Are there any preferred alternative(s) that can be used to treat this patient or patient's |
|
|
|
condition? |
5. |
Yes |
No |
Is a greater drug quantity necessary to achieve the prescribed dose? |
6. |
Yes |
No |
Is a greater quantity of medication needed to accommodate the frequency of use? |
Location:NevadaCallCenter(15) CaseId:9999999
*9999999* *15* *35045*
Confidentiality Notice: This communication and any attachments are intended solely for the use of the addressee named above and contain confidential and legally privileged information. If you are not the intended recipient, any dissemination, distribution or copying is strictly prohibited. If you receive this communication in error, please notify Medco by fax or phone immediately. Medco facsimile machines are secure and in compliance with HIPAA privacy standards. THE PROVISION OF THE INFORMATION REQUESTED IN THIS FORM IS FOR YOUR PATIENT'S BENEFIT. MEDCO DOES NOT COMPENSATE FOR COMPLETING THIS FORM.
MED D_PA_W_V1 |
Y0046_MED D_PA_W_V1 CMS Approved 09132010 |
© 2010 Medco Health Solutions, Inc. All ri hts reserve
hts reserve .
.
35045 *35045*
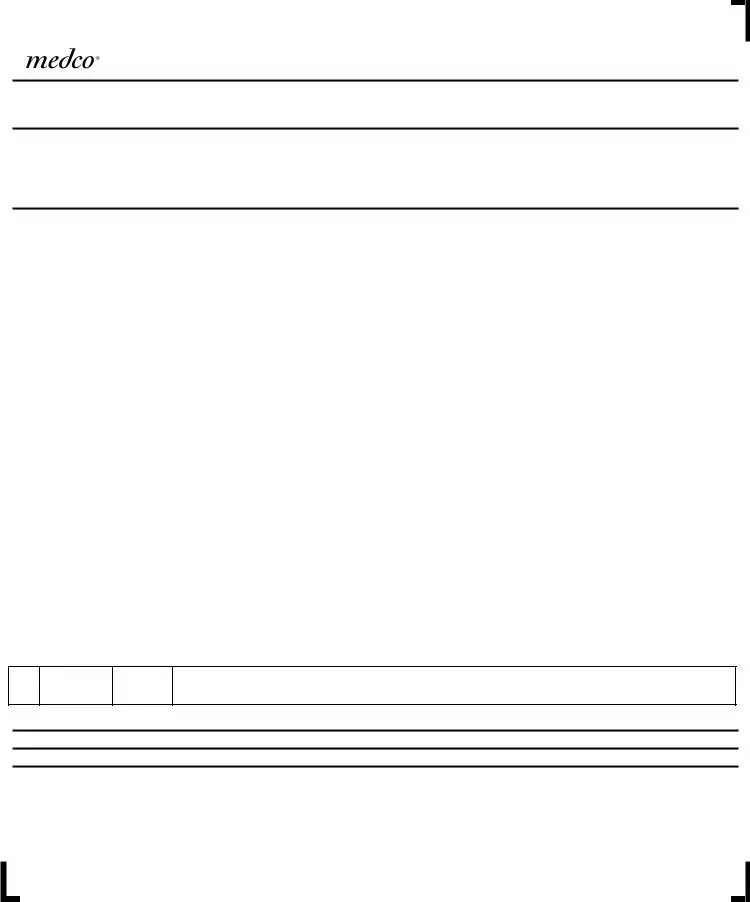
Medicare Part D Prior Authorization Request Form (page 2 of 2)
PLEASE
First and Last Name: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
Medco Member ID Number: |__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|__|
MEDICATION (that requires a coverage review)
Drug Name and Strength: ____________________________________________________________________
Diagnosis: _______________________________________________________________________________
SECTION B: PLEASE ANSWER ALL OF THE FOLLOWING QUESTIONS
1. |
|
Yes |
No |
Is the prescriber a |
|
2. |
|
Yes |
No |
Unknown |
Is this patient currently enrolled in Part B coverage? |
|
|
|
|
|
|
3. |
|
Yes |
No |
Unknown/ |
Has coverage been denied under the Part B benefit? |
|
|
|
|
pending |
|
4. |
|
Yes |
No |
If YES to question 3, has Part B coverage of this medication been denied because of |
|
|
|
|
|
determination of lack of medical necessity? |
|
5. |
|
Yes |
No |
If YES to question 3, has Part B coverage of this medication been denied because of |
|
|
|
|
|
member ineligibility? |
|
SECTIONC:COMPLETEIFAPPLICABLE:PATIENTSUSINGIMMUNOSUPPRESSANTMEDICATIONS |
|||||
|
|
|
|
|
|
1. |
|
Yes |
No |
Is the immunosuppressant medication being used subsequent to a transplant? |
|
|
If |
you answered YES to question 1, please proceed to questions 2 and 3. |
|||
2. |
|
Yes |
No |
Did the transplant occur at a |
|
|
In accordance with CMS Immunosuppressive Drugs Policy Article (A25366), effective July 2008 |
||||
|
Medicare Part B will cover immunosuppressant agents when used for a transplant if the beneficiary was |
||||
|
enrolled in Part A at the time of the transplant and the transplant occurred at a |
||||
|
whether or not Medicare Part A made payments for the transplant. |
||||
3. |
|
Yes |
No |
Was the patient enrolled in Medicare Part A at the time of the transplant? |
|
|
|
|
|
|
|
SECTIOND:COMPLETEIFAPPLICABLE:PATIENTSUSINGCHEMOTHERAPYAGENTS
1.
Yes
No
Is the patient currently receiving or has the patient previously received the prescribed chemotherapy agent?
SECTIONE:IFAPPLICABLE,PLEASEPROVIDEADDITIONALRATIONALEBELOW
Prescriber's Signature: ________________________________________________________
FAX COMPLETED FORM TO
Location:NevadaCallCenter(15) CaseId:9999999
*9999999* *15* *35045*
Confidentiality Notice: This communication and any attachments are intended solely for the use of the addressee named above and contain confidential and legally privileged information. If you are not the intended recipient, any dissemination, distribution or copying is strictly prohibited. If you receive this communication in error, please notify Medco by fax or phone immediately. Medco facsimile machines are secure and in compliance with HIPAA privacy standards. THE PROVISION OF THE INFORMATION REQUESTED IN THIS FORM IS FOR YOUR PATIENT'S BENEFIT. MEDCO DOES NOT COMPENSATE FOR COMPLETING THIS FORM.
MED D_PA_W_V1 |
Y0046_MED D_PA_W_V1 CMS Approved 09132010 |
© 2010 Medco Health Solutions, Inc. All ri hts reserve
hts reserve .
.
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to request prior authorization for medications under Medicare Part D. |
| Urgent Processing Option | Patients can request urgent processing by stating the rationale for urgency. |
| Contact Information | For questions, individuals can call Medco toll-free at 1-800-753-2851. |
| Patient Information Required | The form requires the patient's name, date of birth, telephone number, and Medco Member ID. |
| Medication Review | Details such as drug name, strength, quantity, and dosage instructions must be clearly stated. |
| Prescriber Information | Prescribers must provide their name, address, and secure fax number. |
| Confidentiality Notice | Confidentiality is stressed; the form contains privileged information and should be handled accordingly. |
| Governing Law | Governed by federal laws related to Medicare, specifically Medicare Part D regulations. |
Guidelines on Utilizing Medco Health
Completing the Medco Health form is a crucial step in the process of obtaining necessary medication for patients. Properly filling it out ensures that the information is accurate and comprehensive, allowing for timely review and approval. Below are detailed steps to successfully complete the form.
- Begin with the Patient Information section. Fill in the patient's first and last name, date of birth, telephone number, and Medco Member ID Number.
- Continue with the patient's street address, city, state, and zip code.
- Next, in the Medication section, write down the drug name and strength. Specify the quantity required and provide directions for use (SIG). Include the diagnosis as well.
- Move to the Prescriber Information section. Enter the prescriber's first and last name, street address, city, state, and zip code. Ensure to include their secure fax number and telephone number.
- In Section A, answer all questions regarding the patient’s experience with preferred alternatives and any additional requirements. Be sure to mark appropriate 'Yes' or 'No' responses.
- Proceed to Section B. Here, confirm the prescriber’s Medicare participation status and the patient's enrollment in Part B coverage by answering the questions provided.
- If applicable, complete Section C for patients using immunosuppressant medications, answering questions about the transplant status and Medicare coverage relevant to the immunosuppressant drug.
- For those using chemotherapy agents, fill out Section D by indicating whether the patient is currently or has previously used the prescribed chemotherapy agent.
- If needed, provide any additional rationale in Section E.
- Finally, ensure the prescriber signs the form at the designated location.
- Fax the completed form to 1-800-837-0959 without a cover sheet. Make sure both pages are included.
Once submitted, you are encouraged to follow up if necessary to avoid delays. Quick action will help your patient receive the needed treatment promptly.
What You Should Know About This Form
What is the Medco Health form used for?
The Medco Health form is primarily a Medicare Part D Prior Authorization Request Form. It is designed for healthcare providers to request approval for specific prescription medications that may not be automatically covered under a patient's current insurance plan. This form facilitates the review process by Medicare so that patients can access necessary medications without unnecessary delays.
How do I complete the Medco Health form?
To complete the Medco Health form, start by filling out the patient information section carefully. Include the patient's full name, date of birth, contact information, and Medco member ID number. Next, list the medication requiring review, noting its name, strength, and the patient's diagnosis. Finally, be sure to provide accurate information in the prescriber information section. After you finish both pages, fax the completed form to 1-800-837-0959.
What information do I need to provide about the medication?
For the medication section, you should include the name and strength of the drug being requested, the quantity needed, and specific directions on how the medication should be used. Additionally, a clear diagnosis is essential to support the request. This information helps ensure that the medications are covered based on necessity and patient health status.
Can anyone fill out this form?
This form is typically filled out by healthcare providers, such as doctors or nurse practitioners, as it requires their professional input and signature. However, patients can assist their prescriber by providing necessary patient information and ensuring all details are accurate before it is submitted.
What if I need urgent processing of this request?
If urgent processing is required, simply indicate this in the form and provide a rationale for why the request is urgent. This ensures that your request is prioritized and handled more quickly by Medco. You can also reach out via their toll-free number if you have any questions or require further assistance.
What happens after I submit the form?
Once the form is submitted via fax, it will be reviewed by Medco Health. They will assess the information provided, including the necessity and appropriateness of the medication for the patient’s condition. You'll receive feedback on the authorization status, which could confirm coverage or request additional information as needed.
How long will it take to get a response?
The response time can vary based on the specifics of the request and urgency indicated. Generally, you should anticipate receiving a decision within a few business days. If the request is marked urgent, it will likely be expedited.
What if the request is denied?
If coverage is denied, the patient or prescriber will typically receive a notification explaining the reason for the denial. In many cases, there may be an opportunity to appeal the decision. Additional documentation or alternative medication options may also be discussed in this scenario to explore alternative paths to securing necessary treatment.
Can I check the status of my request?
Yes, you can check the status of your request by contacting Medco Health's customer service at 1-800-753-2851. They can provide updates on your authorization status and clarify any questions or concerns you may have regarding the process.
Common mistakes
Filling out the Medco Health form requires attention to detail. However, mistakes often occur, leading to delays in authorization. Here are some common errors to watch out for.
One frequent mistake is not providing complete patient information. Each section, including the patient's name, date of birth, and Medicare Member ID Number, must be filled out accurately. Omitting this information can result in processing delays. Ensure all fields, particularly contact details, are correct to facilitate follow-up.
Another common issue arises with medication information. The drug name, strength, and directions must be filled in precisely. Incomplete or unclear entries can result in confusion about the treatment plan. Double-check that the medication matches what the prescriber has indicated. This ensures the right drug is under review, avoiding unnecessary delays.
Many people also overlook the necessity of answering all questions in Sections A and B. Each inquiry is crucial for determining the medical necessity of the requested medication. If these questions are skipped or not answered fully, it may lead to a denial of the authorization request.
Incomplete responses about the patient's current medications or previous therapies can derail the approval process. For instance, failing to mention any intolerances can create complications later. Clearly articulating the reasons for requesting an exception to the preferred alternatives is essential.
Utilizing “unknown” in response to any question should be avoided when possible. Providing specific, factual information about the patient’s coverage and status ensures that Medco can make an informed decision on the authorization request. If the answer is truly unknown, consider reaching out for clarification prior to submission.
Another key mistake is neglecting to re-enter the patient’s information on the second page of the form. This should be a simple step, yet it’s often missed under pressure. Clearly repeating this information guarantees that there are no discrepancies that could lead to further confusion.
Finally, failing to send the completed form without a cover sheet can result in complications. It's vital to adhere to the submission instructions exactly as outlined. Missteps in the faxing process can delay the authorization, impacting patient care.
By recognizing these common pitfalls, you can help ensure that the Medco Health form is filled out correctly and efficiently. This small investment of time and attention to detail significantly benefits patient care and streamlines the authorization process.
Documents used along the form
When submitting the Medco Health form for a Medicare Part D Prior Authorization Request, several other documents may also be needed to support the request. Each of these documents serves a specific purpose and can enhance the approval process. Proper completion and inclusion of these forms can help ensure a smooth communication with Medco and a quicker response.
- Authorization to Release Health Information: This form grants permission for healthcare providers to share patient medical information with Medco. It is essential for complying with privacy regulations.
- Prescriber Statement: This document elaborates on the prescriber’s medical rationale for the requested medication. It may include details about previous treatments and their outcomes.
- Clinical Notes: A summary of the patient's medical history, treatment plan, and any relevant test results. These notes provide context and support for the medication request.
- Claims Denial Letter: If the request follows a denial of medication coverage, this letter explains the previous decision. It highlights the necessity for a review by Medco.
- Medication History: A record of previously prescribed medications and their effectiveness. This helps to show the necessity of the requested medication.
- Patient Consent Form: A form acknowledging the patient’s agreement to the sharing of their medical information. It also informs them of their rights regarding the process.
- Prior Authorization Checklist: A checklist that outlines all required documents and steps in the prior authorization process. This helps ensure nothing is overlooked.
- Medication Administration Record (MAR): A record documenting the administration of medications to the patient. This can illustrate compliance and adherence to prescribed treatments.
Including the right forms along with the Medco Health form is crucial for the success of your prior authorization request. Being thorough in documentation can lead to more efficient handling of the case and may increase the likelihood of a favorable outcome.
Similar forms
The Medco Health form serves a critical function in the healthcare system, particularly regarding Medicare Part D Prior Authorization requests. Several other documents share similarities with this form in terms of structure, purpose, or required information. Below is a list detailing eight documents that are similar to the Medco Health form.
- Medicare Part D Coverage Determination Request Form: Like the Medco Health form, this document is designed to determine whether a specific medication is covered under a patient’s Medicare Part D plan. It includes patient information, medication details, and prescriber details.
- Medicaid Prior Authorization Request Form: This form is used by Medicaid beneficiaries to request prior approval for medications. It typically requires similar information about patients, medications, and reasons for requesting non-preferred medications.
- Drug Utilization Review (DUR) Form: This document helps assess whether the prescribed medications are appropriate, medically necessary, or potentially harmful. It shares the requirement for patient history and medication details.
- Request for Reimbursement Form: When patients seek reimbursement for medications, this form is used. It requests similar information about the patient and medications but focuses on reimbursement rather than prior authorization.
- Formulary Exception Request Form: This form allows patients to request coverage for drugs not included in their health plan’s formulary. It mirrors the Medco Health form in needing patient and medication details, as well as clinical justifications.
- Claim Appeal Form: When health plan members want to appeal a denial of coverage for a medication, they submit this form. The required information aligns closely with the Medco Health form, focusing on patient and prescriber information.
- Clinical Trial Consent Form: While primarily for clinical trials, this form gathers patient information and medication details similar to the Medco Health form. It is crucial for individuals participating in studies that may require prior authorization.
- Patient Assistance Program Application: Many pharmaceutical companies offer assistance programs to help patients obtain medications. This application often requires detailed patient information, drug details, and prescriber information, aligning closely with the requests made in the Medco Health form.
Dos and Don'ts
When filling out the Medco Health form, it’s important to ensure everything is correct and complete. Here’s a list of six important dos and don’ts to follow:
- Do read the form carefully before beginning. Understanding each section will save time.
- Do provide accurate information. Double-check names, dates, and member IDs to avoid delays.
- Do complete all required fields. Missing information can lead to rejection of the request.
- Do submit the completed form via the specified fax number. This ensures it reaches the right department.
- Don’t rush through the form. Take your time to ensure clarity and correctness.
- Don’t forget to ask questions if you are unsure about any section. Help is available through their toll-free number.
Following these tips will help streamline the process and support your patient’s needs effectively.
Misconceptions
When it comes to the Medco Health form, there are several misconceptions that can lead to confusion. Here are five common misunderstandings explained:
- The form is only for urgent requests. Many people believe this form is solely for urgent processing, but that is not true. It can be used for both urgent and non-urgent prior authorization requests. It’s important to indicate your need for urgent processing only when necessary.
- You do not need to fill out both pages of the form. Some individuals think it suffices to fill out just one page. However, both pages are essential for a complete submission. Missing information can delay the approval process.
- Any healthcare provider can submit this form. Not all prescribers can submit this form. The prescriber must be a Medicare-participating provider. This is a crucial detail to ensure that the request is valid and actionable.
- Medco will compensate for completing this form. There is a belief that providers receive compensation for filling out this form. In fact, Medco does not provide any compensation for the completion of prior authorization requests. The aim is solely to benefit the patient.
- Approval is guaranteed if the form is submitted correctly. While completing the form accurately is important, it does not guarantee approval. The request is subject to review based on medical necessity and other criteria, which may result in a denial despite proper submission.
Understanding these common misconceptions can simplify the process for patients and healthcare providers alike. It ensures that everyone involved is on the same page and helps facilitate the necessary approvals more smoothly.
Key takeaways
Filling out the Medco Health Form correctly is essential for ensuring your patient's medication request is processed efficiently.
- Complete both pages of the form and return it by fax to 1-800-837-0959.
- If urgent processing is needed, clearly indicate this and provide a rationale for urgency.
- Include comprehensive patient information. Details such as full name, date of birth, and Medco Member ID Number are crucial.
- Document medication information accurately. This includes the drug name, dosage, quantity, and diagnosis.
- Prescriber information must be complete. Ensure you provide all details to facilitate the review process.
- Answer all questions in Section A and Section B with complete honesty to avoid delays.
- The form requires re-entering patient information on the second page; make sure this is done correctly for consistency.
By following these guidelines, you can help ensure that the authorization process goes smoothly and your patient receives their necessary medications in a timely manner.
Browse Other Templates
Religious Exemption Form Tn 2023 - Your submission of this form illustrates a commitment to upholding your religious convictions.
Laser Therapy for Back Pain - All fields marked are necessary for the authorization to be valid.