Fill Out Your Medication Count Sheet Form
The Medication Count Sheet is a vital tool used in healthcare settings to ensure the accurate tracking and administration of medications. This form is specifically designed to document key aspects of medication management, thereby supporting the safety and well-being of residents. It includes important fields such as the resident's name, the quantity of medication on hand, as well as the date the treatment commenced. Additionally, it captures the specifics of the drug, including its strength, which is essential for effective clinical oversight. Staff members are required to provide their signatures to confirm the administration of medication and the accurate updating of quantities, creating a reliable audit trail. The sections detailing the quantity administered versus the remaining amount are particularly crucial, as they help prevent errors, reduce waste, and ultimately enhance patient care. By utilizing the Medication Count Sheet effectively, healthcare professionals can maintain accountability and ensure a consistent standard of care within their practice settings.
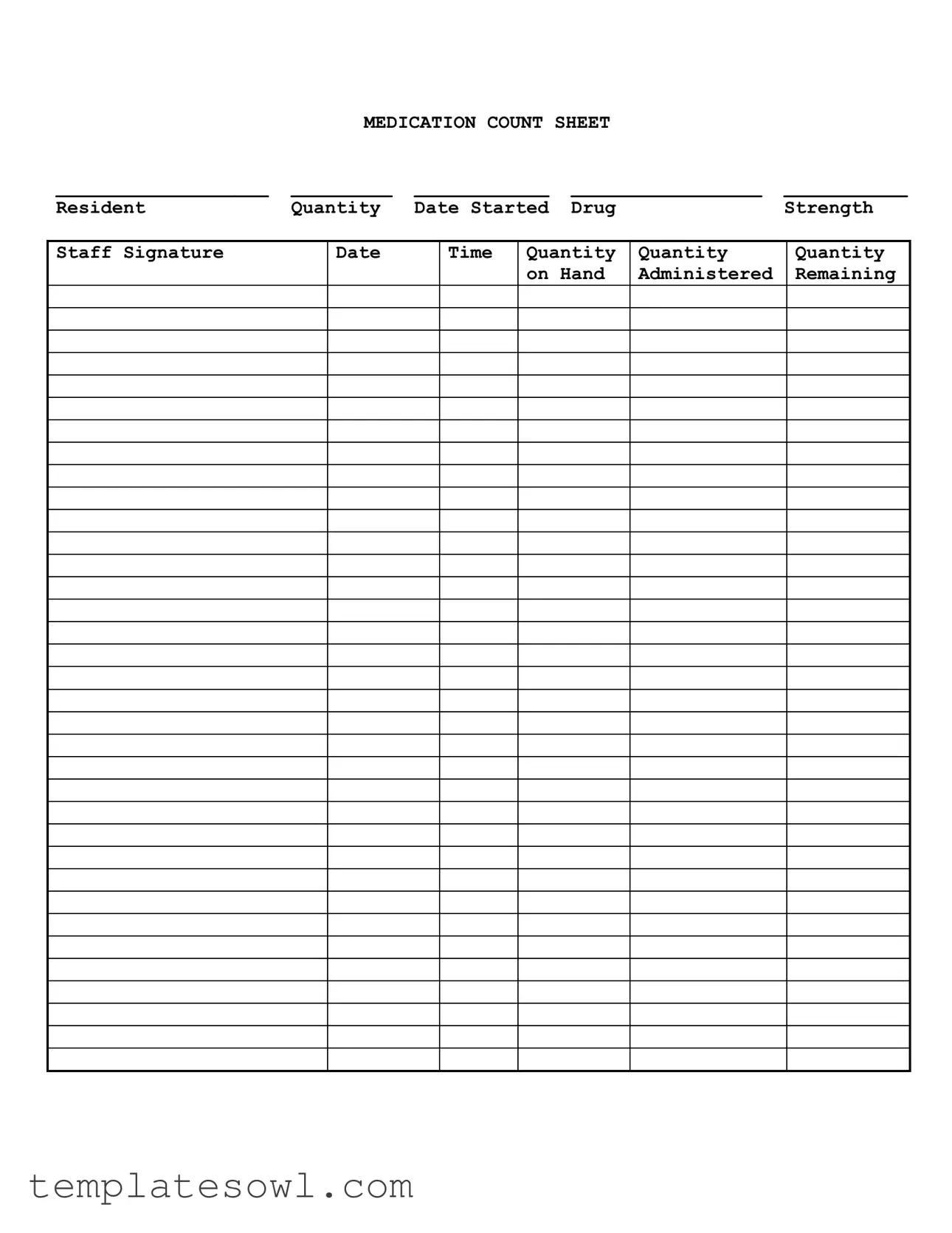
Medication Count Sheet Example
|
MEDICATION COUNT SHEET |
|
||
___________________ |
_________ |
____________ |
_________________ |
___________ |
Resident |
Quantity |
Date Started |
Drug |
Strength |
Staff Signature
Date
Time
Quantity |
Quantity |
Quantity |
on Hand |
Administered |
Remaining |
|
|
|
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Medication Count Sheet is designed to track medication usage and ensure proper inventory management in healthcare settings. |
| Required Fields | Key information includes the resident's name, drug strength, quantity on hand, administered, and remaining medication amounts. |
| Staff Signature | A staff member must sign the form to verify the accurate administration and tracking of medication. |
| Governing Laws | In many states, such as California, the use of Medication Count Sheets is governed by healthcare regulations to ensure patient safety and compliance. |
| Frequency of Updates | The form needs to be updated regularly, especially after each administration, to maintain an accurate count of medications. |
| Importance of Accuracy | Accurate record-keeping is critical in preventing medication errors and ensuring that residents receive their medications as prescribed. |
Guidelines on Utilizing Medication Count Sheet
Filling out the Medication Count Sheet is an essential task for ensuring proper medication management. Accurate record-keeping helps maintain the safety and health of residents. Follow the steps below to complete the form correctly.
- Fill in the resident's name. Write the name of the resident in the designated space at the top of the form.
- Enter the quantity of medication. Specify the starting quantity of the medication in the "Quantity" section.
- Record the date the medication was started. Insert the date when the medication treatment began.
- Name the drug. Clearly write the name of the medication being administered.
- Provide the drug strength. Indicate the strength of the medication as stated on the packaging.
- Have the staff member sign. The staff responsible for this medication should sign the designated "Staff Signature" area.
- Fill out the date and time. Write down the current date and time when the medication is being counted.
- Record the quantity administered. Enter the amount of medication that has been given to the resident on that occasion.
- Calculate the remaining quantity. Deduct the quantity administered from the initial quantity to find what remains and write this in the "Remaining" section.
What You Should Know About This Form
What is the purpose of the Medication Count Sheet?
The Medication Count Sheet is a vital tool used to track and manage medication for residents. It helps ensure that every dose is administered accurately and assists in maintaining an accurate inventory of medications. This transparency is essential for both patient safety and compliance with health regulations.
What information is required on the sheet?
Each Medication Count Sheet must include the resident's identification, the quantity of medication, the date the medication was started, the drug's strength, staff signatures, along with timing details for when medications are administered. Additionally, it tracks quantities on hand, administered, and remaining, creating a full picture of medication usage.
How often should the Medication Count Sheet be updated?
It should be updated each time medication is administered. This practice ensures real-time accuracy and helps prevent discrepancies between what is recorded and what is physically available.
Who is responsible for completing the Medication Count Sheet?
The responsibility typically falls on the licensed staff administering the medication. However, all staff should be trained to understand the sheet's importance and maintain accurate records.
What happens if there is a discrepancy in the medication count?
If discrepancies arise, they must be promptly investigated. Document any missing medications and report the findings to the appropriate supervisor. Steps should be taken to ascertain how the discrepancy occurred and to improve processes to prevent future issues.
Is there a need for signatures on the Medication Count Sheet?
Yes, signatures are essential. They provide accountability and help create a clear audit trail. Staff signatures indicate that the medication was both administered and recorded correctly.
How should the Medication Count Sheet be stored?
These sheets should be stored securely in a way that protects the confidentiality of resident information. Accessible only to authorized personnel, they play a critical role in medication management.
What should I do if the Medication Count Sheet is lost or damaged?
If a sheet is lost or damaged, notify a supervisor immediately. Recreate the information to the best of your ability, noting any gaps. This recordkeeping is crucial for maintaining accountability and ensuring residents receive their medications as prescribed.
Can the Medication Count Sheet be updated electronically?
Yes, if your facility employs electronic health records (EHR), the Medication Count Sheet can be integrated into that system. Electronic updates can provide an efficient and reliable means of tracking medication, as long as strict data privacy measures are followed.
Common mistakes
When completing the Medication Count Sheet form, individuals often overlook essential details, leading to inaccuracies. A common mistake is neglecting to write down the date started for each medication. This information is crucial for tracking how long a medication has been in use. Without it, staff may find it challenging to assess the effectiveness of the treatment or determine when a dosage may need to be adjusted.
Another frequent error is failing to record the strength of the medication. This detail ensures that everyone involved in administering care is aware of the specific dosage being provided. Omitting this information can lead to the distribution of incorrect quantities, potentially jeopardizing the resident's health.
Completing the form without adding the quantity on hand can create significant confusion. This number reflects the amount of medication remaining before administration. When this figure is missing, tracking involves guesswork, which should never be the case when it comes to medication management.
It is not uncommon for staff to forget to document the administered quantity for each medication given. This oversight means that the Medication Count Sheet does not accurately represent what has been dispensed to the resident. Staff may inadvertently assume that the medication has been given, leading to the potential for double dosing.
Another area of error arises when staff fail to sign the form after completing the medication administration. A staff signature is essential as it provides accountability and a traceable log of who administered the medication. Without a signature, it becomes difficult to determine responsibility should any issues arise later.
Some staff members may incorrectly calculate the remaining quantity after medication has been administered. Accurate math is vital for maintaining the correct count of medications on hand. Errors in calculation can lead to stockouts or excess inventory, complicating medication management further.
At times, individuals will write down the date of administration without verifying that it corresponds correctly with the medication being counted. Dates serve as vital checkpoints for tracking when medications were dispensed. Misalignment in dates can create significant gaps in patient care records.
People also sometimes neglect to include the time of administration beside the date. Like the date, the time of administering medications is essential for maintaining proper treatment schedules. Missing this information may cause confusion about whether a medication was given promptly or if it was skipped altogether.
Individuals filling out the form can also forget to review their entries before submitting. A lack of verification increases the risk of errors slipping through unnoticed. A final review can catch mistakes that could otherwise put a resident's health at risk.
Lastly, some staff members may rush through the Medication Count Sheet form due to time constraints. While maintaining a timely schedule is important, completing the form accurately should always take precedence. Rushed entries often lead to various mistakes that can endanger patient safety.
Documents used along the form
The Medication Count Sheet is a crucial document for tracking medication administration in healthcare settings. It ensures that staff can accurately record the amount of medication given to residents, as well as what is on hand at any given time. In addition to the Medication Count Sheet, several other forms and documents are commonly used. These documents work together to promote compliance and ensure safety in medication administration.
- Medication Administration Record (MAR): This document provides a comprehensive list of medications prescribed to a resident, including dosage, schedule, and instructions for administration. It serves as a key reference for staff during medication rounds.
- Medication Receipt Form: This form is used to record the receipt of medications from the pharmacy or supplier. It includes details such as the type of medication, quantity received, and the date of receipt.
- Incident Report Form: In cases where there are discrepancies in medication counts or administration errors, this form captures all relevant details, including what happened, who was involved, and any corrective actions taken.
- Controlled Substance Log: For medications classified as controlled substances, this log tracks the usage and inventory of these drugs. It requires careful attention to ensure compliance with legal regulations.
- Refusal of Medication Form: When a resident refuses medication, this form documents the refusal. It includes information about the resident, the medication in question, and any reasons for the refusal.
- Medication Disposition Form: This form records the disposal of medications that are no longer needed, expired, or have been returned. It ensures that proper procedures are followed for safe disposal.
Using these documents together with the Medication Count Sheet enhances communication among staff and improves overall medication management. Each form plays a specific role in ensuring that medication is administered safely and accurately.
Similar forms
-
Medication Administration Record (MAR): This document tracks the administration of medications to residents over time. Like the Medication Count Sheet, the MAR includes details such as the drug name, dosage, administration times, and staff signatures, providing a comprehensive overview of a patient's medication regimen.
-
Controlled Substance Log: Used specifically for medications classified as controlled substances, this log records the quantity received, administered, and remaining. Similar to the Medication Count Sheet, it ensures strict accountability for these high-risk drugs.
-
Prescription Records: These records document the prescribed medications for each resident, including dosage and administration instructions. Both the Prescription Records and the Medication Count Sheet serve as essential resources for healthcare providers to manage and monitor medication effectively.
-
Incident Report: Although primarily focused on documenting unusual occurrences, incident reports may include details about medication errors or issues. They both aim to improve patient safety and ensure that records are clear and actionable.
-
Daily Shift Report: This document compiles key activities and observations for each shift. Similar to the Medication Count Sheet, it may highlight any discrepancies in medication counts or administration, providing a broader context for patient care.
-
Patient Care Plan: This comprehensive document outlines the overall treatment strategy for each resident. It includes medication management details, aligning closely with the Medication Count Sheet in its aim of ensuring proper medication administration and monitoring.
-
Inventory Management Log: This log tracks medication supplies within a facility, detailing what is on hand and what needs replenishing. Similar to the Medication Count Sheet, it emphasizes accurate tracking to ensure the availability of necessary medications.
-
Medication Effectiveness Report: This report assesses the efficacy of prescribed medications based on resident feedback and clinical outcomes. Both documents aim to optimize the care provided to residents by closely monitoring medication usage and results.
-
Audit Report: Conducted periodically, these reports evaluate compliance with medication management policies. They are closely tied to the Medication Count Sheet as they often highlight discrepancies in medication counts or administration practices.
-
Staff Training Records: Documentation of staff training related to medication administration. These records ensure that staff members are adequately prepared, paralleling the Medication Count Sheet’s role in fostering accuracy in medication administration.
Dos and Don'ts
When filling out the Medication Count Sheet form, it is important to follow certain guidelines to ensure accuracy and compliance. Below are several practices to consider.
- Do double-check the resident's name and medication details before starting.
- Do clearly indicate the quantity administered each time medication is given.
- Do ensure that the date and time are recorded accurately for each entry.
- Do have another staff member verify the counts to prevent discrepancies.
- Don't leave any spaces blank; fill in all fields as required.
- Don't use correction fluid to alter any entries on the form.
- Don't forget to sign the sheet after completing the medication count.
- Don't record medication counts after the fact; entries should be made in real-time.
Misconceptions
Understanding the Medication Count Sheet form is crucial for effective medication management. However, there are several misconceptions that can lead to confusion. Here are some of those misunderstandings explained.
- It is only for nursing staff. Many believe that only nursing personnel are responsible for the Medication Count Sheet. In reality, all staff involved in medication administration should have access to this form.
- It only tracks medication quantity. Some assume that the form is solely for counting medications. While tracking the quantity is essential, it also records important details such as drug strength and administration times.
- It does not require regular updates. A common belief is that once the form is completed, it doesn't need revisiting. In fact, regular updates are vital to ensure accurate tracking of medications.
- Any staff member can sign off on the form. Some assume that any staff member can sign the Medication Count Sheet. However, only authorized personnel should provide their signature, as it verifies that the information is accurate and complete.
- Errors in recording are not a big deal. Some individuals think that minor errors can be overlooked. This is not true, as even small inaccuracies can lead to significant issues in medication management.
- It is not required for all medications. There is a misconception that the Medication Count Sheet is only necessary for certain controlled substances. In fact, all medications given to residents should be recorded to maintain complete accountability.
Clearing up these misconceptions helps ensure the safety and wellbeing of residents. Accurate record-keeping fosters trust and accountability within the healthcare environment.
Key takeaways
The Medication Count Sheet helps ensure accurate tracking of medication inventory. This is crucial for both safety and compliance.
Each entry requires careful documentation of the resident's name and the specific medication being counted.
Always fill in the quantity on hand, which indicates how much medication is currently available.
Record the date started for each medication to maintain an accurate timeline of usage.
Staff signatures are mandatory to verify that the counts were performed correctly and to establish accountability.
Document the date and time of each count to ensure ongoing transparency and prevent discrepancies.
Accurate recording of the quantity administered is essential to maintain accurate records and to address any potential medication errors.
Regularly review the records on the Medication Count Sheet to identify trends or issues that may need to be addressed promptly.
Browse Other Templates
Nj Annulment Forms Pdf - It is a crucial element of the civil litigation process in New Jersey.
Sere Jko - Encourage colleagues or family to engage in this training to broaden safety awareness.
Arizona Health Care - AHCCCS will send a decision notice after reviewing your application.