Fill Out Your Medication Error Form
The Medication Error form is a critical tool designed to ensure patient safety and quality of care within healthcare settings. This form is utilized for documenting all medication incidents, which can include errors made during the prescribing, dispensing, or administration processes. When a pharmacist discovers a medication error, they are responsible for initiating the report and notifying both the physician and the pharmacy manager about any incident that could potentially affect a patient's health or safety. The form collects essential patient information, such as name, address, and date of birth, and it identifies the specifics of the incident, including the nature of the error—whether it involved an incorrect drug, dosage, or administration method. Additionally, it includes sections for detailing contributing factors that led to the error, allowing pharmacists to reflect on circumstances like improper patient identification or misinterpretation of drug orders. Notifying the patient and physician is also documented, ensuring transparent communication about the incident. Ultimately, the form plays a pivotal role in investigating medication discrepancies, promoting accountability, and facilitating improvements in healthcare processes to prevent future errors.
Medication Error Example
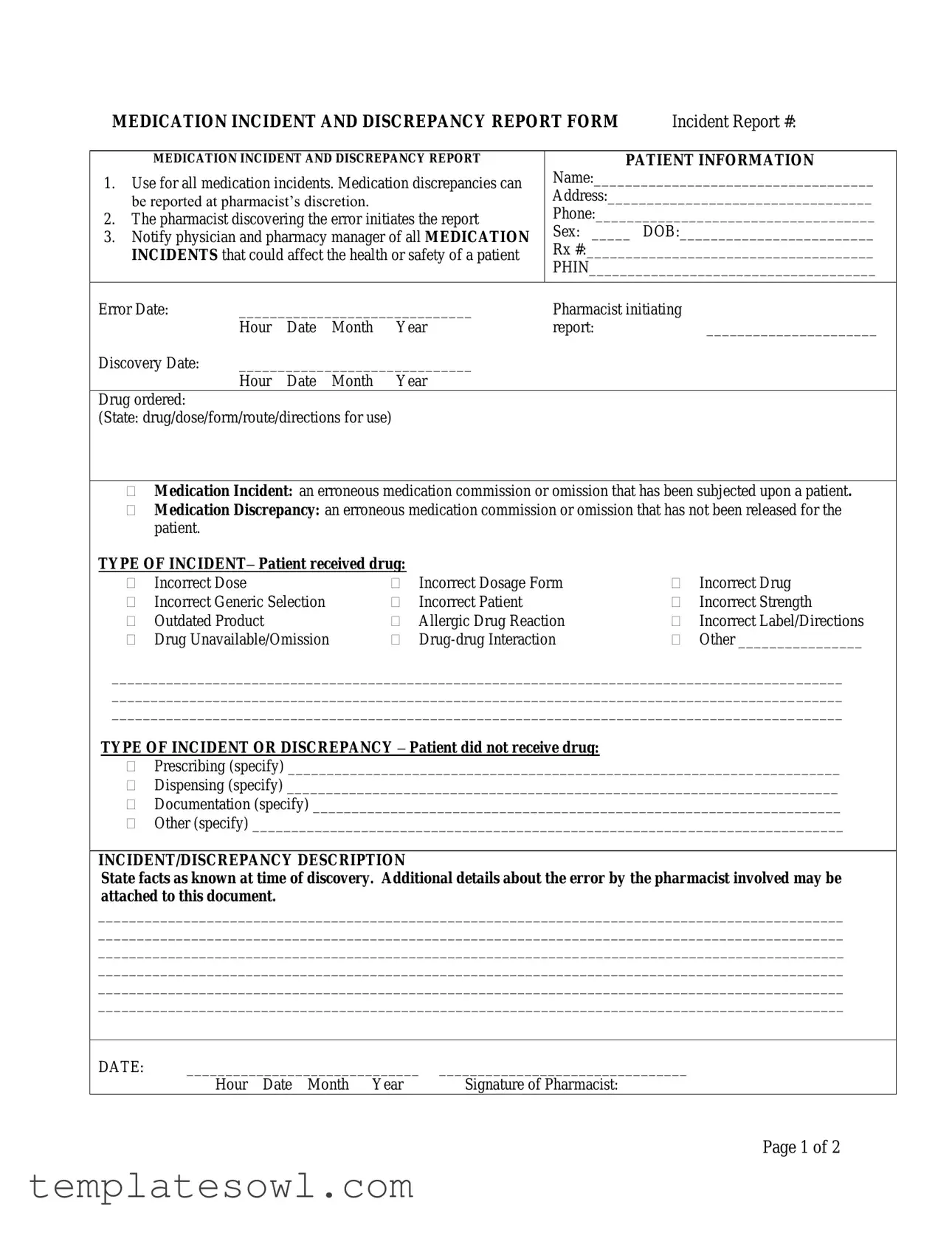
MEDICATION INCIDENT AND DISCREPANCY REPORT FORM |
Incident Report #: |
MEDICATION INCIDENT AND DISCREPANCY REPORT
1.Use for all medication incidents. Medication discrepancies can be reported at pharmacist’s discretion.
2.The pharmacist discovering the error initiates the report
3.Notify physician and pharmacy manager of all MEDICATION INCIDENTS that could affect the health or safety of a patient
PATIENT INFORMATION
Name:____________________________________
Address:__________________________________
Phone:____________________________________
Sex: _____ DOB:_________________________
Rx #:_____________________________________
PHIN_____________________________________
Error Date: |
______________________________ |
Pharmacist initiating |
|
|||
|
Hour |
Date |
Month |
Year |
report: |
______________________ |
Discovery Date: |
______________________________ |
|
|
|||
|
Hour |
Date |
Month |
Year |
|
|
Drug ordered: |
|
|
|
|
|
|
(State: drug/dose/form/route/directions for use) |
|
|
|
|||
Medication Incident: an erroneous medication commission or omission that has been subjected upon a patient.
Medication Discrepancy: an erroneous medication commission or omission that has not been released for the patient.
TYPE OF INCIDENT– Patient received drug: |
|
|
|
||
|
Incorrect Dose |
|
Incorrect Dosage Form |
|
Incorrect Drug |
|
Incorrect Generic Selection |
|
Incorrect Patient |
|
Incorrect Strength |
|
Outdated Product |
|
Allergic Drug Reaction |
|
Incorrect Label/Directions |
|
Drug Unavailable/Omission |
|
|
Other ________________ |
|
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
TYPE OF INCIDENT OR DISCREPANCY – Patient did not receive drug:
Prescribing (specify) _______________________________________________________________________
Dispensing (specify) _______________________________________________________________________
Documentation (specify) ____________________________________________________________________
Other (specify) ____________________________________________________________________________
INCIDENT/DISCREPANCY DESCRIPTION
State facts as known at time of discovery. Additional details about the error by the pharmacist involved may be attached to this document.
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
DATE: |
______________________________ |
________________________________ |
|
Hour Date Month Year |
Signature of Pharmacist: |
Page 1 of 2
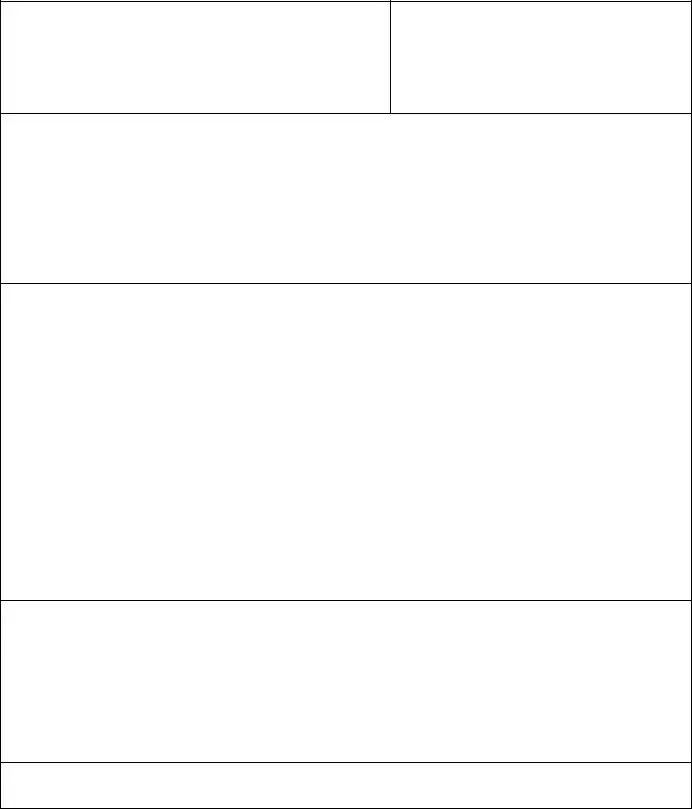
CONTRIBUTING FACTORS
(To be completed by pharmacist responsible)
|
Improper patient identification |
Misread/misinterpreted drug order (include verbal orders) |
|
|
Incorrect transcription |
|
Drug unavailable |
Lack of patient counselling |
|
Other |
|
|
DATE: |
______________________________ |
__________________ |
|
|
||||
|
|
Hour Date Month Year |
Signature |
|
|
|
|||
|
NOTIFICATION – Complete the following information according to Standards of Practice. |
||||||||
1. |
Patient notified: |
|
|
|
|
|
|
|
|
|
|
|
___________________________ |
|
|||||
|
|
|
Hour |
Date |
Month |
Year |
|||
2. |
Physician notified: ____ |
______________________________ |
|
||||||
|
|
Yes/No |
Hour |
Date |
Month |
Year |
|||
|
|
|
|
|
|
|
|
|
|
|
SEVERITY |
|
|
|
|
|
|
|
|
|
|
None |
|
No change in patient’s condition: no medical intervention |
|||||
|
|
Minor |
|
|
|
required |
|
|
|
|
|
Major |
|
Produces a temporary systemic or localized response: does |
|||||
|
|
|
|
|
|
not cause ongoing complications |
|||
|
|
|
|
Requires immediate medical intervention |
|||||
|
OUTCOME OF INVESTIGATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Problem Identification |
|
|
|
Action |
|
|
|
|
|
|
Lack of knowledge |
|
|
Education provided |
||||
|
|
Performance problem |
|
|
Policy/procedure changed |
||||
|
|
Administration problem |
|
|
System changed |
|
|
||
|
|
Other |
|
|
Individual awareness |
||||
|
|
|
|
|
Group awareness |
||||
|
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|||||
|
RESOLUTION OF PROBLEM THAT RESULTED IN THE ERROR BEING MADE: |
||||||||
|
|
|
|
|
|
|
|
||
|
Signature: |
Date: |
Signature: |
Date: |
|||||
|
(Pharmacist filling out the form) |
|
|
|
(Pharmacy Manager) |
||||
PHARMACY USE ONLY
Page 2 of 2
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | This form is intended for reporting all medication incidents, including medication discrepancies, at the pharmacist's discretion. Its use helps improve patient safety and supports quality assurance within the pharmacy. |
| Initiation | The pharmacist who discovers the medication error is responsible for initiating the report. This responsibility underscores the importance of accountability in the medication management process. |
| Notification Requirement | Pharmacists must notify both the physician and the pharmacy manager about any medication incidents that could potentially affect a patient's health or safety. Timeliness in such notifications is critical. |
| Types of Incidents | The form categorizes incidents into two main types: those in which a patient actually received the incorrect medication and those instances where a patient did not receive the prescribed medication. These categories help track different kinds of medication errors. |
| Contributing Factors | Items that may contribute to a medication error, such as improper patient identification or misinterpretation of drug orders, must be identified and documented. This data is vital for improving pharmacy practices and preventing recurrences. |
Guidelines on Utilizing Medication Error
Once you have gathered all necessary information and are prepared to document the details regarding the medication error, follow these steps to complete the Medication Error form accurately. It’s important to provide thorough and precise information to ensure proper communication between all parties involved.
- Begin by locating the Incident Report # field and fill in the report number for this specific incident.
- Ensure that you indicate whether a Medication Incident or Medication Discrepancy has occurred.
- Complete the Patient Information section with the patient’s Name, Address, Phone number, Sex, Date of Birth (DOB), Prescription number (Rx #), and Patient Health Identification Number (PHIN).
- Document the Error Date and Discovery Date of the incident, specifying the Hour, Date, Month, and Year for both.
- Clearly outline the Drug ordered by stating its details (drug/dose/form/route/directions for use).
- In the TYPE OF INCIDENT section, check the appropriate box indicating how the patient received the drug incorrectly.
- If applicable, specify under TYPE OF INCIDENT OR DISCREPANCY if the patient did not receive the drug and provide the relevant details.
- In the INCIDENT/DISCREPANCY DESCRIPTION section, describe the situation clearly, stating all known facts at the time of discovery. Include any additional information about the error if necessary.
- Sign and date the report in the designated area, confirming it was completed by the initiating pharmacist.
- In the CONTRIBUTING FACTORS section, check the boxes that apply. Document any relevant contributing factors you identify.
- Complete the NOTIFICATION section by noting whether the patient and physician were notified, along with the corresponding dates and times.
- Assess the SEVERITY of the incident and select the appropriate option that best describes the patient's condition resulting from the error.
- Finally, address the OUTCOME OF INVESTIGATION FOLLOW-UP and outline any actions taken to resolve the issue caused by the error.
- Include signatures for both the pharmacist filling out the form and the pharmacy manager, along with their respective dates.
Upon completion, ensure that all sections of the form are filled out completely and accurately. This will facilitate an effective response to the incident, helping to address any immediate needs of the patient and to prevent future occurrences.
What You Should Know About This Form
1. What is the purpose of the Medication Error form?
The Medication Error form is designed to report any medication incidents or discrepancies related to patient care. This includes errors made during medication prescribing, dispensing, or administration. This form helps identify issues that could affect a patient’s health and ensures appropriate steps are taken to prevent future occurrences.
2. Who should fill out the Medication Error form?
The form should be initiated by the pharmacist who discovers the medication error or discrepancy. It is their responsibility to document the incident accurately and notify the relevant parties, including the patient’s physician and pharmacy manager.
3. What types of medication incidents can be reported?
Several types of incidents can be reported. These include administering an incorrect dose, using an outdated product, and failing to provide the medication at all. Other instances, such as allergic reactions or drug-drug interactions, are also documented using this form.
4. What happens after the form is submitted?
After the Medication Error form is filled out and submitted, it becomes part of the pharmacy’s records. The pharmacy team will review it to identify contributing factors and develop strategies to prevent similar errors in the future. This may involve additional training for staff or changes to existing policies.
5. Is patient information kept confidential?
Yes, patient information is treated with the utmost confidentiality. The data collected on the Medication Error form is used solely for quality improvement and safety purposes. All staff members are trained to handle sensitive information responsibly.
6. What is the definition of a medication discrepancy?
A medication discrepancy is an erroneous commission or omission of a medication that has not yet been released to the patient. This may involve issues such as incorrect entries in the medication order or a failure to dispense the drug as prescribed.
7. How is severity assessed on the form?
Severity is categorized based on the impact of the incident on the patient’s health. It ranges from no change in condition to the need for immediate medical intervention. This classification helps prioritize response actions and follow-up care.
8. Who is notified about a medication incident?
The form requires documentation of notifications made to both the patient and the physician. It’s essential that these parties are informed promptly to ensure patient safety and enable further medical intervention if necessary.
Common mistakes
Filling out a Medication Error form requires attention to detail. One common mistake is the omission of vital patient information. This includes contact details, birth date, and prescription number, which are crucial for tracking the incident and ensuring the patient's safety.
Another frequent error involves providing incomplete descriptions of the incident. Users may fail to fully describe the type of medication error that occurred, making it difficult for the pharmacy to assess and address the issue effectively. Clear and detailed descriptions enhance understanding and accountability.
Inadequate communication about notification is also an area where mistakes can happen. It is essential to indicate whether the patient and the physician were informed of the incident. Failure to record these notifications could lead to a lack of follow-up and potential harm to the patient.
People often misuse the terms "medication incident" and "medication discrepancy." Confusing these definitions can lead to incorrect reporting. It is crucial to accurately categorize the situation to reflect the severity and impact on the patient’s health.
Another error lies in neglecting to state the severity of the incident adequately. Marking the correct severity level is vital for prioritizing responses and interventions. By misclassifying severity, appropriate care and follow-up may not be provided.
In some cases, individuals fail to document contributing factors. This section is important as it helps in understanding why the error occurred. A lack of detail about factors such as misreading orders or improper identification can hinder future prevention efforts.
Some may rush through the form, leading to legibility issues. Clearly printed information ensures that all parties involved can read and understand the report. Illegible handwriting can result in misunderstandings and complications in the investigation process.
Forgetting to include signatures is another oversight. Both the pharmacist who initiates the report and the pharmacy manager should sign to confirm accountability. The absence of these signatures raises questions regarding the authenticity of the report.
Another common mistake is failing to attach additional details or documents that could provide further context about the error. Supporting documents help to create a clearer picture, facilitating a more thorough investigation and resolution process.
Finally, some people may overlook the importance of follow-up actions. After the initial report, addressing how the problem will be resolved is critical. If this section is left blank, it may result in recurring errors without any learning or improvements to the system.
Documents used along the form
When documenting medication incidents, it's essential to utilize several forms and documents that complement the Medication Error form. These documents provide critical information for improving patient safety and ensuring accountability within the healthcare system. Here’s a list of some key forms that are often used alongside the Medication Error form:
- Incident Report Form: This form provides a general structure for reporting any adverse events or unusual incidents, including medication errors. It collects detailed information about the event, stakeholders involved, and contributing factors, ensuring thorough documentation for future analysis.
- Pharmacy Audit Form: This document is used for regular reviews of pharmacy operations, including medication dispensing and storage processes. By identifying trends, it helps in preventing future incidents, enhancing overall quality assurance in the pharmacy.
- Patient Notification Form: After a medication error has occurred, this form serves to document the notification process to the patient. It outlines the information given to the patient, helping to ensure transparency and accountability.
- Root Cause Analysis Form: This form is used to investigate the underlying reasons for a medication error. It aids in identifying systemic issues that contributed to the incident, fostering a culture of continuous improvement.
- Corrective Action Plan (CAP): Following an incident, a CAP outlines the steps necessary to address the error and prevent recurrence. This plan details specific actions, responsible parties, and timelines for implementation, ensuring accountability and follow-through.
- Pharmacy Manager Review Form: This document captures the manager’s assessment of medication errors and discrepancies. It is used to track actions taken in response to incidents and to evaluate the effectiveness of implemented changes.
- Education and Training Record: This form documents the training and educational interventions provided to staff following a medication error. It helps to ensure that employees are well-informed, ultimately leading to improved patient safety and reduced error rates.
Utilizing these forms in conjunction with the Medication Error form can greatly enhance the overall safety and efficiency of medication management processes. Implementing a rigorous documentation system not only helps to address immediate concerns but also contributes to long-term improvements in patient care.
Similar forms
The Medication Error form serves a vital role in healthcare, particularly in documenting incidents that could affect patient safety. Below are eight other documents that share similarities with the Medication Error form, each serving to track and manage specific types of incidents to ensure patient safety and quality care.
- Incident Report Form: This form is used for documenting any event that is not consistent with the routine operation of a facility, much like the Medication Error form, which captures medication errors. Both forms facilitate accountability and enable organizations to investigate incidents effectively.
- Patient Safety Report: This document focuses on incidents affecting patient care. Similar to the Medication Error form, it helps healthcare providers identify potential risks and implement preventative measures to enhance patient safety.
- Adverse Event Report: Like the Medication Error form, this report documents negative patient reactions to medical care, including medication errors. Both forms aim to improve the quality of care by analyzing incidents and making informed adjustments.
- Quality Improvement Report: This type of report targets the overall improvement of healthcare services. Both it and the Medication Error form collect data that drives change, ensuring safer practices in the administration of medications.
- Pharmacy Audit Report: Similar to the Medication Error form, a pharmacy audit report reviews pharmacy practices, compliance, and medication management. It helps uncover discrepancies and improve practices to minimize errors.
- Root Cause Analysis (RCA) Form: This document seeks to identify the underlying causes of incidents. The Medication Error form often leads to an RCA when a significant medication error occurs, allowing for an in-depth investigation and systemic change.
- Patient Complaint Form: Patients can report concerns or complaints related to their care. Like the Medication Error form, this document collects information that can help healthcare providers address issues and improve overall service quality.
- Medication Reconciliation Form: This form is essential for ensuring patients receive the correct medications. Both forms aim to prevent medication errors, though the reconciliation form focuses on verifying medication lists during transitions in care.
These documents play an important role in maintaining safety standards and ensuring that all incidents are reported, investigated, and resolved effectively. The goal is always to create a safer and more trustworthy healthcare environment for patients.
Dos and Don'ts
When filling out the Medication Error form, consider the following do's and don'ts:
- Do use the form for all medication incidents.
- Do ensure that the report is initiated by the pharmacist who discovered the error.
- Do notify both the physician and pharmacy manager of any incidents affecting patient safety.
- Do include all relevant patient information accurately.
- Don't omit any details regarding the medication incident or discrepancy.
- Don't wait too long to report the incident, as timely reporting is crucial.
- Don't forget to document the contributing factors and resolution measures taken.
Misconceptions
Understanding the Medication Error form is essential for ensuring patient safety and effective communication within healthcare environments. However, several misconceptions can lead to confusion regarding its purpose and functionality. Below are some common misconceptions, along with clarifications:
- Only serious incidents need to be reported. Many believe that only severe medication errors warrant completion of the form. In reality, the form is intended to document all medication incidents, regardless of perceived severity, to prevent future occurrences.
- Only pharmacists can complete the form. While pharmacists play a significant role in initiating the report, anyone aware of the incident can contribute information. This collaborative approach enhances accuracy and thoroughness.
- The form is just for reporting errors, not discrepancies. Some individuals think the form solely focuses on errors that affect patient medication. However, it also allows for the reporting of discrepancies that may not reach the patient but could impact care.
- The incident must be fully resolved before submitting the form. It is a common belief that all investigations need to be complete before a report is filed. On the contrary, the form can be submitted with the available information, promoting immediate action and follow-up.
- Completing the form is a punitive measure. There is a concern that filing a Medication Error form will lead to retribution against staff members. However, the primary purpose of the form is to enhance safety, promote learning, and avoid future errors rather than assigning blame.
- Only incidents affecting patients require reporting. Some may think that only incidents that cause harm need documentation. Yet, reporting any medication incident or discrepancy is important, as it helps identify potential risks before they affect patient care.
Recognizing these misconceptions is vital for fostering a better understanding of the Medication Error form. Clear communication and proper reporting practices enhance patient safety and contribute to a culture of openness in healthcare.
Key takeaways
Understanding how to accurately fill out and use the Medication Error form is crucial for patient safety and quality assurance in healthcare settings. Below are key takeaways that delineate the vital elements of this process.
- Universal Application: The Medication Error form is applicable to all medication incidents. Discrepancies can be reported at the pharmacist's discretion.
- Report Initiation: The pharmacist who discovers the error must initiate the report to ensure timely action.
- Notification Requirement: It is imperative to notify both the physician and pharmacy manager of all medication incidents that could affect patient health or safety.
- Patient Information: Accurate and complete patient information is essential when filling out the form. This includes name, address, phone number, sex, DOB, and relevant RX and PHIN numbers.
- Types of Errors: Specify if the incident involves an erroneous medication commission or omission, stating clearly between medication incidents and discrepancies.
- Incident Description: Provide a clear and factual description of the incident as known during discovery. Additional details may be attached to the form.
- Contributing Factors: The responsible pharmacist should complete this section, identifying factors such as improper patient identification or misinterpreted drug orders.
- Severity Assessment: Classify the severity of the incident, ranging from no impact on the patient's condition to requiring immediate medical intervention.
- Follow-up Actions: Document the outcomes of the investigation, along with any actions taken to resolve the issue and prevent future occurrences.
Immediate attention to these aspects of the Medication Error form can lead to improved safety and accountability in pharmaceutical practices. Prompt and accurate reporting protects patients and enhances overall healthcare quality.
Browse Other Templates
602 Form Printable - Immediate attention to completing the LIC 602A is essential for smooth transitions.
Canon IP100 Setup Guide,Canon IP100 User Manual,Canon IP100 Quick Reference,Canon IP100 Troubleshooting Guide,Canon PIXMA IP100 Instructions,Canon IP100 Helpful Hints,Canon IP100 Operational Guide,Canon IP100 Support Handbook,Canon IP100 Care and Mai - TTY support is available for customers with hearing disabilities.
Ched-unifast Online Scholarship Application Portal - Upon filling out the application, ensure that all entries are clear and legible.