Fill Out Your Medication Incident Report Form
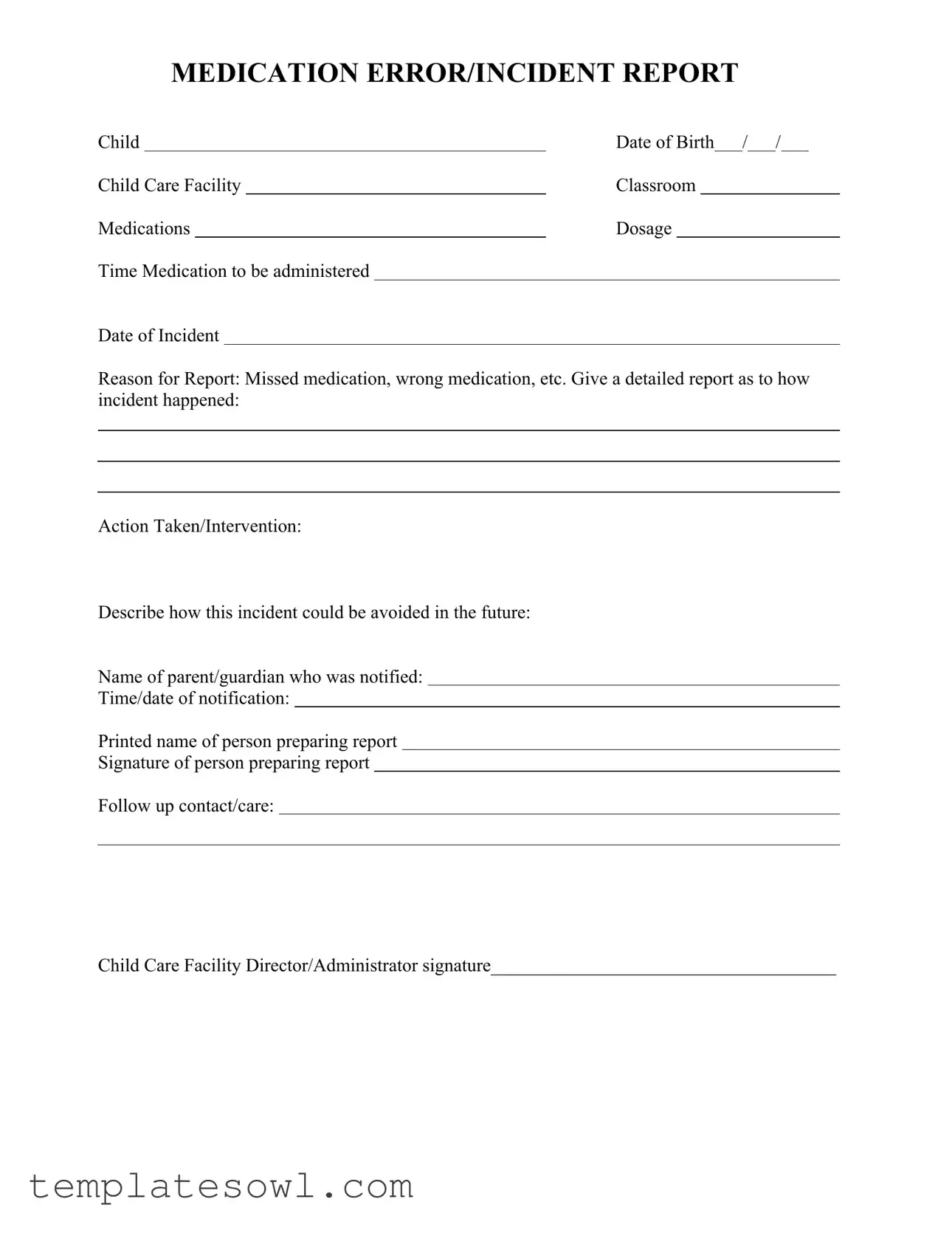
The Medication Incident Report form serves as an essential tool in documenting medication errors or incidents involving children in care facilities. It collects critical information such as the child's date of birth, the specific facility, and the classroom where the incident occurred. Each report requires details about the medications involved, including dosage and the time the medication was supposed to be administered. The form prompts users to specify the date of the incident and the reason for the report, which may include missed medications or incorrect dosages. A comprehensive narrative explaining how the incident transpired is crucial for understanding the context. Additionally, users are encouraged to outline the actions taken in response to the incident and suggest preventive measures for the future. The form also includes sections for notifying the child's parent or guardian, along with the time and date of that notification. Finally, the report must be signed by the individual preparing it, as well as the child care facility's director or administrator, ensuring accountability and proper follow-up care. Through its structured approach, the Medication Incident Report form facilitates both immediate action and long-term safety improvements in medication administration practices.
Medication Incident Report Example
MEDICATION ERROR/INCIDENT REPORT
Child |
|
Date of Birth / |
/ |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child Care Facility |
|
Classroom |
|
|
|
|
|
||||||
Medications |
|
Dosage |
|
|
|
|
|
||||||
Time Medication to be administered |
|
|
|
|
|
|
|
|
|
|
|||
Date of Incident
Reason for Report: Missed medication, wrong medication, etc. Give a detailed report as to how incident happened:
Action Taken/Intervention:
Describe how this incident could be avoided in the future:
Name of parent/guardian who was notified:
Time/date of notification:
Printed name of person preparing report
Signature of person preparing report
Follow up contact/care:
Child Care Facility Director/Administrator signature_____________________________________
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Medication Incident Report form is designed to document errors or incidents related to medication administration in childcare facilities. |
| Essential Information | It captures critical details, including the child's name, date of birth, facility, medications involved, dosage, and time of administration. |
| Incident Reporting | Reasons for the report include missed medication, wrong medication, or other medication-related issues. |
| Detailed Account | The form requires a thorough account of the incident, aiming to understand exactly how it occurred. |
| Preventative Measures | It prompts the reporter to suggest how similar incidents could be avoided in the future, enhancing safety protocols. |
| Parental Notification | The form includes a section to document which parent or guardian was notified about the incident, ensuring transparency. |
| Legal Compliance | In some states, specific laws govern the reporting of medication errors in childcare settings. These may include state health and safety regulations or administrative codes. |
Guidelines on Utilizing Medication Incident Report
When a medication incident occurs, timely and accurate reporting is essential. Filling out the Medication Incident Report form provides a thorough record of the event and helps prevent future occurrences. Here’s how to complete the form effectively.
- Begin by entering the child's full name.
- Fill in the child's date of birth in the specified format.
- Indicate the child care facility's name where the incident took place.
- Specify the classroom that the child belongs to.
- List all medications that were involved in the incident.
- Write down the dosages of the medications that were meant to be administered.
- Record the time that the medication was supposed to be given.
- Provide the name of the medication that was to be administered.
- Document the date when the incident occurred.
- Select the reason for the report, such as "missed medication" or "wrong medication."
- Give a detailed account of how the incident happened. Be specific about what led to the error.
- Describe the actions taken immediately following the incident and any interventions performed.
- Offer suggestions on how to avoid similar incidents in the future.
- Write the name of the parent or guardian who was notified about the incident.
- Note the time and date when the parent or guardian was informed.
- Print the name of the person who is preparing the report.
- Ensure the person preparing the report signs their name.
- Include any follow-up contact or care details if applicable.
- Lastly, obtain the signature of the Child Care Facility Director or Administrator.
What You Should Know About This Form
What is the purpose of the Medication Incident Report form?
The Medication Incident Report form is designed to document any incidents related to medication administration within a childcare facility. This could include missed medications, wrong doses, or any other errors that may occur. By systematically reporting these incidents, facilities can identify patterns, implement corrective actions, and improve overall medication safety.
Who should fill out the Medication Incident Report?
The report should be filled out by the staff member who discovers or is involved in the medication incident. It is crucial that the person preparing the report has firsthand knowledge of the incident to ensure the details are accurate and complete.
What information is required on the form?
The form requires specific information such as the child’s name and date of birth, the details of the medication (including dosage, time, and the medication to be administered), and the date of the incident. Additionally, the person filling out the report should provide a detailed account of how the incident occurred, what actions were taken in response, and suggestions for preventing future incidents.
How can incidents be prevented in the future?
To avoid future incidents, it is helpful to analyze the circumstances surrounding the error. Reported suggestions often include improving staff training on medication administration, implementing double-check procedures, and enhancing communication among staff and parents regarding medication schedules. Documenting these recommendations in the report assists in developing an action plan.
What should be done after a report is submitted?
After the report is submitted, the childcare facility director or administrator should review it for completeness and accuracy. They may conduct a follow-up discussion with the staff member involved and ensure that the suggested actions for prevention are put into effect. Follow-up care for the child affected may also be necessary, depending on the nature of the incident.
How is the parent or guardian informed of the incident?
The report requires details on the parent or guardian who was notified about the incident, including the date and time of notification. It is essential that communication with families is prompt and thorough, providing them with the necessary information about the incident and any actions taken to ensure the child's well-being.
Is the report confidential?
Yes, the Medication Incident Report is considered confidential. It contains sensitive information regarding a child's medication and health. Access to the report should be restricted to authorized personnel within the childcare facility, and parents or guardians should only receive information pertinent to the incident involving their child.
Common mistakes
Filling out a Medication Incident Report form correctly is crucial for documenting errors and ensuring the safety of children. One common mistake people make is providing incomplete information. This can include missing vital details like the child's date of birth, specific medications involved, or the exact dosage. Incomplete reports can lead to misunderstandings or insufficient responses to incidents.
Another frequent oversight occurs when the person does not clearly define the reason for the report. Indicating whether it was a missed medication, wrong medication, or a different incident is essential for proper assessment and follow-up. Failing to do this can result in a lack of clarity about the nature of the incident.
People often neglect to provide a detailed description of how the incident occurred. This section is crucial for understanding the series of events that led to the error. It's not enough to state that a mistake happened; one must explain the conditions surrounding the event to prevent future occurrences.
Omitting the section on action taken or intervention is another common error. Not detailing what measures were taken after the incident can hinder the ability of the facility to improve processes. It’s vital to record immediate actions to ensure all involved parties understand the response initiated.
Participants frequently overlook how to prevent similar incidents in the future. This section should contain thoughtful analysis and recommendations based on what went wrong. By foreseeing potential pitfalls and suggesting solutions, the report can contribute significantly to enhancing safety protocols.
The report must also include who notified the parent or guardian and the time/date of that notification. Some individuals may forget to document this, which can lead to confusion regarding communication and follow-up with families after an incident.
Finally, not collecting the necessary signatures can invalidate the report. It is essential to include the printed name and signature of the person preparing the report. Additionally, a signature from the Child Care Facility Director or Administrator is crucial for confirming that the incident has been reviewed at a higher level.
Documents used along the form
When addressing medication incidents in child care settings, several important forms and documents complement the Medication Incident Report. Each document plays a crucial role in ensuring accurate reporting, accountability, and future prevention strategies. Below is a list detailing these additional forms.
- Medication Administration Record (MAR): This document tracks the administration of medications given to a child, including dosage and time. It serves as a day-to-day log, ensuring medications are given as prescribed.
- Incident Report Form: Used for documenting any type of incident, this form provides a comprehensive overview of events that occurred, including the context and individuals involved. It is crucial for maintaining a safe environment.
- Parental Notification Form: This form is designed to communicate with parents or guardians regarding medication incidents. It informs them about what happened, the child’s condition, and any necessary follow-up actions.
- Follow-Up Care Plan: Following an incident, this document outlines any additional care or observations required for the child. It ensures that any medical or operational changes are clearly communicated and implemented.
- Staff Training Acknowledgment Form: This document confirms that staff members have received training related to medication administration and safety protocols. It plays a role in minimizing future incidents.
- Child Health History Form: Important for understanding a child’s health background, this form includes information about allergies, prior medications, and any medical conditions. It assists in making informed decisions about medication management.
- Emergency Action Plan: This document outlines specific steps to take in response to medication errors or reactions. It can include contacts, procedures, and necessary equipment to ensure swift action is taken.
- Quality Assurance Review Form: Used to assess the incident and its handling, this form evaluates processes and identifies areas for improvement in medication management and overall care protocols.
- Medication Supply Log: This log tracks all medications received and dispensed, ensuring that records are up to date and available for audits or reviews.
Utilizing these forms effectively enhances the safety and quality of care provided in child care facilities. Each document contributes to a thorough understanding of medication-related incidents, promoting transparency and accountability while seeking to improve standard practices.
Similar forms
The Medication Incident Report form is crucial for tracking medication errors in child care settings. It shares similarities with several other documents that also focus on reporting incidents or ensuring safety. Here are six documents that relate closely to the Medication Incident Report:
- Accident Report Form: This form captures details about any accidents that occur within a facility. Like the Medication Incident Report, it requires an account of what happened, actions taken, and recommendations for future prevention.
- Incident Report Form: Used for documenting a variety of incidents beyond medication errors, this form often parallels the Medication Incident Report by including specifics about the time, place, and nature of the incident.
- Child Abuse Reporting Form: This form is essential for documenting suspected child abuse. Similar to the Medication Incident Report, it requires a detailed narrative of the incident, including who was notified and steps taken after the report.
- Health and Safety Checklist: This document reviews safety protocols within a facility. Like the Medication Incident Report, it aims to identify potential risks and recommends strategies to enhance safety and prevent future incidents.
- Medical Emergency Report: When a medical emergency arises, this report details the circumstances, actions taken, and outcomes. The focus on thorough documentation mirrors the approach taken in the Medication Incident Report.
- Parent Notification Form: This form is used to inform parents about incidents involving their children. The emphasis on communication and timely notification relates closely to the requirements in the Medication Incident Report.
Each of these documents plays a pivotal role in maintaining safety and accountability in child care environments. Their structure and purpose reinforce the importance of clear communication and precise reporting.
Dos and Don'ts
When completing a Medication Incident Report form, attention to detail is crucial. Below is a list of dos and don'ts that can ensure the form is filled out correctly.
- Do provide accurate information about the child, including their full name and date of birth.
- Do specify the medications involved, including dosage and administration time.
- Do clearly indicate the reason for the report, such as missed or incorrect medication.
- Do give a thorough account of the incident, detailing how it occurred.
- Do include any actions taken or interventions that were made following the incident.
- Don’t skip the section on how the incident could be avoided in the future.
- Don’t forget to document the name of the parent or guardian who was notified.
- Don’t leave out the time and date of the notification, as this can be important.
- Don’t submit the report without the signatures of both the preparer and the facility director or administrator.
Misconceptions
- Misconception 1: Medication Incident Reports are only for serious errors.
Many individuals believe that these reports should only be filed for grave mistakes, such as administering the wrong medication or overdosing. However, all incidents, irrespective of their severity, should be documented. This helps identify patterns and areas for improvement.
- Misconception 2: Only healthcare professionals should complete the report.
While healthcare professionals are often involved, anyone working in a child care facility can and should fill out a Medication Incident Report if they witness or become aware of an incident. This encourages a team approach to safety.
- Misconception 3: Reports are not important for routine medication errors.
Some believe that minor mistakes do not require reports. This is inaccurate. Each report offers valuable insights into medication management and can help prevent repeated errors in the future.
- Misconception 4: Completing the report is time-consuming and burdensome.
Although it may first appear to be an additional task, the form is structured for efficiency. Once familiar with it, completing the report can be quick and straightforward, ultimately helping to enhance overall safety protocols.
- Misconception 5: The information on the report is not confidential.
Confidentiality should always be maintained. The details contained within a Medication Incident Report are sensitive, and sharing them outside of designated personnel compromises the privacy of those involved.
Key takeaways
Filling out and utilizing the Medication Incident Report form is essential for ensuring the safety and well-being of children within care facilities. Here are some key takeaways:
- Complete Details: Ensure that every section of the form is filled out thoroughly, including the child’s name, date of birth, and all medication details. Missing information can lead to misunderstandings and unresolved incidents.
- Specific Reasons: Clearly state the reason for the report. Whether it’s a missed medication or the administration of the wrong dosage, precise descriptions help clarify what happened.
- Descriptive Account: Include a detailed narrative of how the incident occurred. This reflection not only aids in understanding the circumstances but also contributes to improving practices and preventing future errors.
- Communication Is Key: Document the name of the parent or guardian notified about the incident, along with the date and time of this communication. Keeping caregivers informed fosters trust and transparency.
Browse Other Templates
Creating an Order Form - Encourage tracking of personal connections made during discussions that could aid in sales.
Punchline Bridge to Algebra 2001 Marcy Mathworks Answer Key - This section also stresses the relevance of algebra in everyday situations and problem-solving.