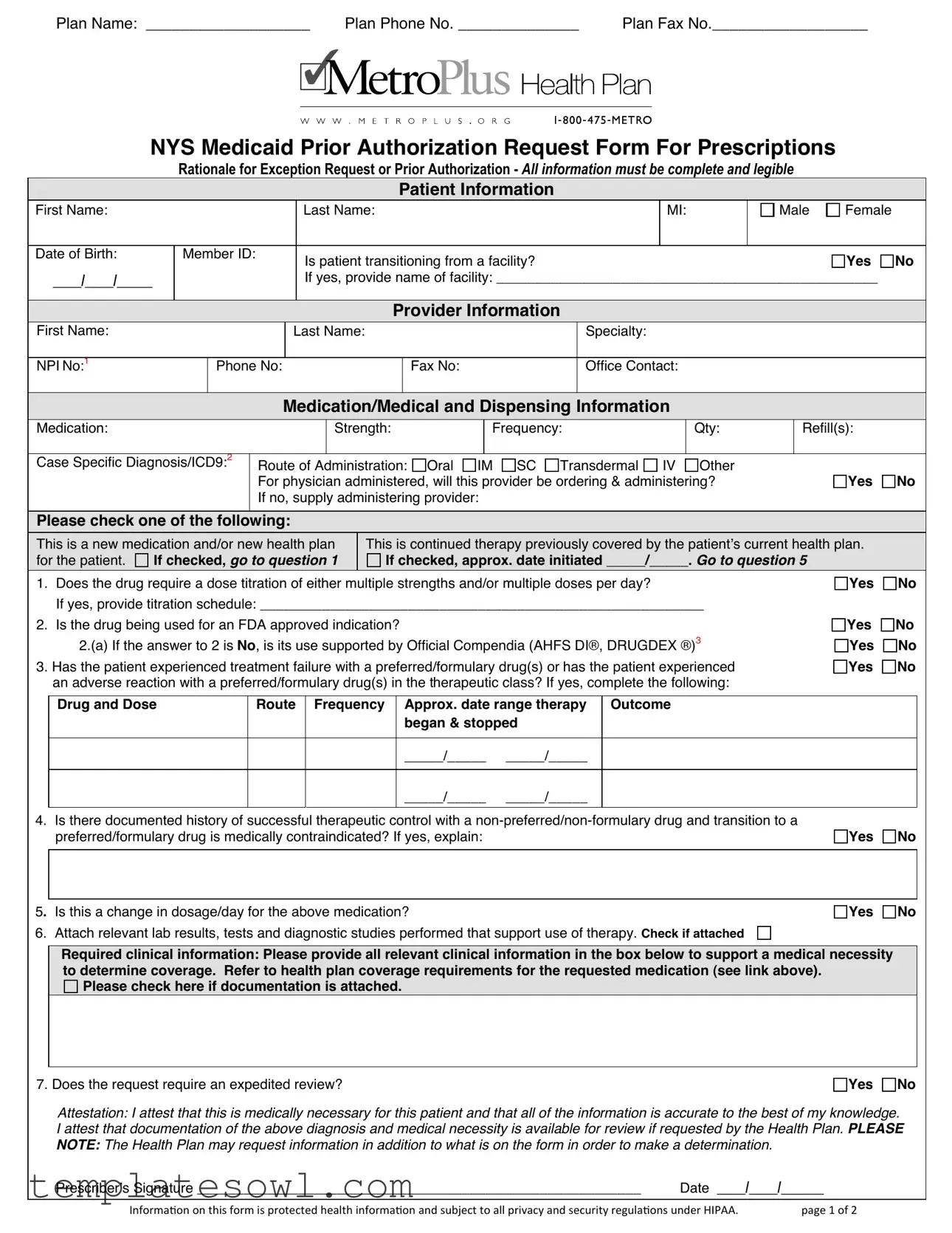
Fill Out Your Metroplus Health Plan Form
The Metroplus Health Plan form is an essential document for healthcare providers seeking prior authorization for medications prescribed to their patients. This comprehensive form gathers crucial information from both the patient and provider, ensuring that the patient's specific medical needs are clearly communicated. Key sections include patient details—such as name, date of birth, and member ID—along with the provider's information like specialty and contact details. It also requests details about the medication, including dosage and frequency, as well as the case-specific diagnosis. Importantly, the form assesses whether the medication is new or a continuation of therapy, which affects the approval process. Additional questions help establish medical necessity, such as prior treatment paths and any adverse reactions to formulary drugs. Relevant lab results and supporting documents play a critical role in this process. The attestation at the end ensures that the prescriber is confirming the accuracy of the submitted information. Understanding how to fill out this form accurately can streamline the approval process and impact patient care positively.
Metroplus Health Plan Example
Plan Name: ___________________ |
Plan Phone No. ______________ |
Plan Fax No.__________________ |
NYS Medicaid Prior Authorization Request Form For Prescriptions
Rationale for Exception Request or Prior Authorization - All information must be complete and legible
Patient Information
First Name: |
|
|
|
|
|
Last Name: |
|
|
|
MI: |
Male |
Female |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of Birth: |
Member ID: |
|
|
Is patient transitioning from a facility? |
|
|
|
|
|
Yes |
No |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
____/____/_____ |
|
|
|
|
|
If yes, provide name of facility: _________________________________________________ |
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Provider Information |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
First Name: |
|
|
|
|
Last Name: |
|
|
Specialty: |
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
NPI No:1 |
|
Phone No: |
|
Fax No: |
Office Contact: |
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
Medication/Medical and Dispensing Information |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Medication: |
|
|
|
|
|
|
Strength: |
|
Frequency: |
|
|
Qty: |
|
Refill(s): |
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
Case Specific Diagnosis/ICD9:2 |
Route of |
Administration: |
Oral IM SC Transdermal IV Other |
|
|
|
|
|
||||||||||
|
|
|
|
|
For physician administered, will this provider be ordering & administering? |
|
|
Yes |
No |
||||||||||
|
|
|
|
|
If no, supply administering provider: |
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Please check one of the following:
This is a new medication and/or new health plan for the patient. 
 If checked, go to question 1
If checked, go to question 1
This is continued therapy previously covered by the patient’s current health plan.
If checked, approx. date initiated _____/_____. Go to question 5
1.Does the drug require a dose titration of either multiple strengths and/or multiple doses per day?
If yes, provide titration schedule: _________________________________________________________
2.Is the drug being used for an FDA approved indication?
2.(a) If the answer to 2 is No, is its use supported by Official Compendia (AHFS DI®, DRUGDEX ®)3
3.Has the patient experienced treatment failure with a preferred/formulary drug(s) or has the patient experienced an adverse reaction with a preferred/formulary drug(s) in the therapeutic class? If yes, complete the following:
Yes
Yes
Yes
Yes
No
No No
No
Drug and Dose
Route Frequency Approx. date range therapy began & stopped
Outcome
_____/_____ _____/_____
_____/_____ _____/_____
4.Is there documented history of successful therapeutic control with a
Yes 
 No
No
5. Is this a change in dosage/day for the above medication?
6. Attach relevant lab results, tests and diagnostic studies performed that support use of therapy. Check if attached
Yes 
 No
No
Required clinical information: Please provide all relevant clinical information in the box below to support a medical necessity to determine coverage. Refer to health plan coverage requirements for the requested medication (see link above).
Please check here if documentation is attached.
7. Does the request require an expedited review?
Yes 
 No
No
Attestation: I attest that this is medically necessary for this patient and that all of the information is accurate to the best of my knowledge. I attest that documentation of the above diagnosis and medical necessity is available for review if requested by the Health Plan. PLEASE NOTE: The Health Plan may request information in addition to what is on the form in order to make a determination.
Prescriber’s Signature _________________________________________________________ |
Date ____/____/______ |
|
|
|
|
Informaion on this form is protected health informaion and subject to all privacy and security regulaions under HIPAA. |
page 1 of 2 |
|

Instructional Information for Prior Authorization
Upon our review of all required information, you will be contacted by the health plan.
When providing required clinical information, the following elements should be considered within the rationale to support your medical necessity request:
OHeight/Weight
OCompound ingredients
OSpecific dosage form consideration
ODrug or Other Related Allergies
Please consider providing the following information as applicable & when available:
OHealthcare Common Procedure Coding System (HCPCS) 4
OTransition of Care (contact, phone number, length of stay)
OPatient information (address, phone number)
OProvider information (address, direct electronic contact information,
This form must be signed by the prescriber but can also be completed by the prescriber or his/her authorized agent. The completed fax form and any supporting documents must be faxed to the proper health plan.
Helpful Definitions
1NPI: A national provider identifier (NPI) is a unique
2
3AHFS Drug Information® (AHFS DI®) provides
4The HCPCS is divided into two principal subsystems, referred to as level I and level II of the HCPCS:
OLevel I of the HCPCS is comprised of CPT (Current Procedural Terminology), a numeric coding system maintained by the American Medical Association (AMA). The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals.
OLevel II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Because Medicare and other insurers cover a variety of services, supplies, and equipment that are not identified by CPT codes, the level II HCPCS codes were established for submitting claims for these items. http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html
PAGE 2
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | This form is used to request prior authorization for medications under the NYS Medicaid program. |
| Patient Transition | The form includes a question regarding whether the patient is transitioning from a facility, which is an important consideration for continuity of care. |
| Provider Responsibility | The prescriber must attest that the information provided is accurate and that documentation supporting medical necessity is available if requested. |
| Federal Compliance | All patient information on this form is protected under HIPAA regulations, ensuring privacy and security of health data. |
Guidelines on Utilizing Metroplus Health Plan
Completing the Metroplus Health Plan form requires careful attention to detail. Each section must be filled out clearly, providing accurate information about the patient and the prescribed treatment. Ensuring that all necessary documentation accompanies the form is crucial for a smooth approval process. Below are the steps to guide you through filling out the form:
- Start with the plan information at the top. Fill in the Plan Name, Plan Phone No., and Plan Fax No..
- Provide patient information by entering the First Name, Last Name, MI, Date of Birth, and Member ID.
- Indicate if the patient is transitioning from a facility by checking Yes or No. If yes, specify the name of the facility.
- Fill out the provider's details including the First Name, Last Name, Specialty, NPI No., Phone No., Fax No., and Office Contact.
- Enter medication details, including Medication, Strength, Frequency, Qty, and Refill(s).
- Add the Case Specific Diagnosis/ICD9 and Route of Administration, selecting from options such as Oral, IM, SC, and others.
- If applicable, indicate whether this provider will be ordering and administering the medication.
- Check the appropriate box to indicate if it is a new medication or continued therapy and, if needed, provide the date initiated.
- Answer questions 1 through 7 regarding the medication’s dosage, FDA indications, and past treatment responses.
- Attach any relevant lab results, tests, or diagnostic studies that support the request for therapy.
- Provide all required clinical information in the designated space to justify the medical necessity for the treatment.
- Indicate if the request requires an expedited review by checking Yes or No.
- Finally, ensure the form is signed and dated by the prescriber.
Upon completion of the form, review for clarity and accuracy. Ensure all necessary supporting documents are included. The completed form must be faxed to the appropriate health plan to initiate the authorization process.
What You Should Know About This Form
1. What is the purpose of the Metroplus Health Plan form?
The Metroplus Health Plan form is designed to request prior authorization for medications and medical therapies. It ensures that the necessary information is provided to determine whether a medication is covered under the health plan.
2. How do I complete the patient information section?
In the patient information section, you will need to fill out the patient's first and last name, middle initial, gender, date of birth, and member ID. If the patient is transitioning from a facility, don’t forget to include the name of that facility.
3. What should I include under provider information?
Fill out the first and last name of the provider, their specialty, NPI number, phone number, fax number, and the office contact person’s name. This helps streamline communication regarding the authorization request.
4. What types of medication information are required?
You need to provide the medication name, strength, frequency, quantity, and number of refills requested. Additionally, indicate the case-specific diagnosis and the route of administration.
5. What if the medication has been previously covered?
If this is a continuation of therapy that has been covered by another health plan, provide the approximate date it started. You will then proceed to answer follow-up questions related to the medication’s necessity and effectiveness.
6. What types of supporting information are needed?
Support your medical necessity request with relevant clinical information, lab results, and any diagnostic studies. Complete information helps the health plan make informed decisions about coverage.
7. When is it appropriate to check the expedited review option?
Select the expedited review option if the patient’s situation requires quicker processing. This is particularly crucial when delays might affect their health or treatment outcome.
8. Is prior authorization required for all medications?
Not all medications require prior authorization. However, many high-cost or specialty medications do. Always check your specific plan requirements for further details.
9. What is the significance of the prescriber’s signature?
The prescriber’s signature is important because it attests to the accuracy of the information provided and confirms that the medication is medically necessary for the patient. This ensures accountability in the prescribing process.
10. How can I submit the form once it’s completed?
Once all the information is filled out, fax the form along with any supporting documents to the designated health plan fax number. Make sure to double-check that all required fields are completed to avoid processing delays.
Common mistakes
Filling out the Metroplus Health Plan form can be a complex task and it is crucial to complete it accurately. One common mistake is leaving sections blank. Every field in the form is important for processing the request effectively. Complete all areas, even if the information seems insignificant. Leaving any section empty might lead to delays or outright denial of the request.
Another frequent error occurs in the patient’s date of birth. A simple transposition of numbers can change the timeline of the patient’s medical history. Always double-check that this crucial piece of information is correctly entered. It is also advisable to ensure that the member ID matches the identification provided by the health plan.
Individuals often forget to provide specific details regarding medications. Failing to include the strength, dosage, and frequency can lead to confusion. Make sure to fill out the medication, strength, quantity, refill information, and the route of administration accurately. This ensures clarity in what is being requested from the health plan.
Another common issue involves the case-specific diagnosis section. Missing or incomplete diagnosis codes can hinder the approval process. The form requires the relevant ICD-9 codes to justify the need for the medication. Verify that these codes are up-to-date and correctly input to avoid delays.
People sometimes neglect to explain the rationale for exceptions in adequate detail. This can leave the request vulnerable to scrutiny. It is essential to provide a clear explanation of why the medication is necessary, particularly if it is not a routinely prescribed option within the formulary. Attach all supporting documentation to reinforce the case.
When listing any prior medications, individuals often omit past treatment failures or adverse reactions. Failure to acknowledge these details can weaken the entire request. It is essential to document any previous treatments that were ineffective or resulted in negative side effects.
Furthermore, some individuals overlook the requirement for signatures. All prescribers must sign the form, confirming that the information is accurate. Omitting the signature can effectively invalidate the form and lead to further complications.
Lastly, many people do not read the instructions carefully. Ignoring the guidelines can lead to incomplete submissions or missing documentation that might be necessary for an expedited review. Take time to familiarize yourself with all the requirements outlined for the prior authorization process and ensure all instructions are followed closely.
Documents used along the form
When filing a request with Metroplus Health Plan, various additional forms and documents may also be required to ensure a comprehensive review. These documents provide necessary support for the request, help clarify patient needs, and facilitate a smoother approval process.
- Insurance Information Form: This document collects necessary details about the patient’s insurance coverage, including policy numbers and contact information for the insurance company.
- Patient Medical History Form: This form outlines the patient’s medical background, including previous treatments, diagnoses, and any chronic conditions that may be relevant to the current request.
- Medication List: A detailed list of all current and past medications the patient has taken. This helps to identify possible interactions and the patient's treatment history.
- Physician's Notes: These notes from the prescribing physician detail the rationale for the prescribed medication, including observations concerning the patient’s health and treatment outcomes.
- Lab Results: Any relevant laboratory test results should be included. These documents substantiate the need for specific medications or treatments requested.
- Diagnostic Imaging Reports: If applicable, these reports provide visual evidence (like X-rays or MRIs) that support the medical necessity of the requested treatment.
- Medication Prior Authorization Guidelines: This document outlines specific criteria set by the health plan for medications, ensuring that the request meets all necessary coverage requirements.
- Specialist Consultation Reports: Reports from consultations with specialists can provide additional insight into the patient's condition and treatment needs, reinforcing the request for authorization.
- Expedited Review Request Form: If the situation is urgent, this form requests a faster review process to avoid delays in patient care.
Including these documents can strengthen the request and provide the necessary context for the evaluation process. Ensuring completeness and clarity in your submission can aid in obtaining timely approvals for the patient's needed treatment.
Similar forms
- NYS Medicaid Prior Authorization Request Form for Prescriptions: This document is also focused on obtaining prior authorizations for medication and treatment, requiring similar patient and provider information as well as a rationale for medical necessity. Both emphasize the need for complete and accurate data to ensure coverage.
- Insurance Claim Form: Like the Metroplus Health Plan form, an insurance claim form collects pertinent patient and provider details. It also specifies the services rendered, often requiring documentation to justify the expenses incurred, mirroring the need for comprehensive documentation seen in the prior authorization context.
- Patient History Form: This document gathers detailed patient background information, including medical history and current medications. It parallels the Metroplus form's focus on patient specifics, making it easier for providers to understand the patient's health status when seeking medication approval.
- Medication Reconciliation Form: This form seeks to ensure that all current medications are accounted for, similar to how the Metroplus form lists current medications and treatment history. It plays a crucial role in preventing medication interactions and ensuring continuity of care.
- Referral Request Form: A referral request form requires patient demographics and details about the reason for the referral. It aligns with the Metroplus form's aim to facilitate patient care by providing essential information to the new provider or specialist.
- Clinical Documentation for Prior Authorization: This document focuses on outlining clinical rationale for specific treatment requests, akin to how the Metroplus form requests supportive clinical information to verify medical necessity in obtaining coverage for prescribed therapies.
- Facility Discharge Summary: Documenting the details of patient care during a facility stay, this summary must provide thorough patient information. Similar to the Metroplus form, it helps in ensuring continuity of care, particularly when a patient transitions from a facility to home or another care setting.
Dos and Don'ts
When filling out the Metroplus Health Plan form, follow these guidelines to ensure your submission is accurate and complete.
- DO complete all sections of the form to avoid delays in processing.
- DO provide clear and legible handwriting or use a typed format.
- DO attach all relevant laboratory results and documentation that support the medical necessity.
- DO verify that the prescriber has signed the form before submission.
- DON'T leave any required fields blank, as this can result in requests for more information.
- DON'T submit the form without reviewing it for completeness and accuracy.
By adhering to these tips, you can help ensure that the review process goes smoothly.
Misconceptions
There are several misconceptions regarding the Metroplus Health Plan form. Understanding these can help streamline the process of obtaining prior authorization. Below are some common misunderstandings and clarifications about the form:
- Only doctors can fill out the form: While the form must be signed by the prescriber, it can also be completed by an authorized agent. This flexibility can ease the administrative burden.
- All requested information is optional: Each section of the form is necessary to ensure a comprehensive review. Incomplete forms may delay processing.
- The form can be submitted without supporting documents: Relevant supporting documents are critical for substantiating the medical necessity request.
- Once submitted, no further information is needed: The health plan may contact the provider for additional information during the review process.
- All prior authorizations are handled the same way: The specifics of each request can vary, impacting the required supporting documentation and approval timelines.
- Medications are approved automatically if all boxes are checked: Approval is based on medical necessity and adherence to coverage requirements, not just the completion of the form.
- There's no need to attach lab results: Supporting clinical information, including lab results, can support the use of the requested medication and is often required.
- Expedited reviews are available for any request: Only specific situations qualify for expedited reviews, and not all requests will meet the criteria.
- Privacy regulations do not apply when submitting the form: All information provided on the form is protected under HIPAA and must be handled with care to ensure patient confidentiality.
Clearing these misconceptions can enhance the experience of both providers and patients when seeking necessary medications and treatment under the Metroplus Health Plan.
Key takeaways
When navigating the Metroplus Health Plan form, several important aspects deserve attention to ensure a smooth submission process. Here are key takeaways:
- Complete and Clear Information: All sections of the form must be filled out completely and legibly. Incomplete entries can lead to delays in processing.
- Patient Details: Accurate patient information is crucial. Be sure to provide the patient's full name, member ID, and date of birth, along with any details about facility transitions if applicable.
- Provider Information: Include the provider's name, specialty, and contact details. This not only legitimizes the request but also facilitates communication with the health plan.
- Medications and Diagnosis: Clearly specify the medication, its strength, frequency, and the case-specific diagnosis. This section helps illustrate the medical necessity of the treatment.
- Support Documentation: Attach any relevant lab results, tests, and records that support your request. Strong evidence enhances the chances of approval.
- Signature and Attestation: The form must be signed by the prescribing provider, who also needs to attest to the accuracy of the information provided. This formal commitment underscores the necessity of the request.
By keeping these takeaways in mind, healthcare providers can navigate the authorization process more effectively, ultimately benefiting patient care.
Browse Other Templates
Lost Savings Bonds - Consult with the Bureau of the Fiscal Service for clarifications related to your unique situation.
Free Printable Child Care Receipt Template - It's important for parents to verify all information is correct before filing the receipt.