Fill Out Your Msp Form
The Medicare Secondary Payer (MSP) form is a crucial tool for healthcare providers seeking to navigate the complexities of claims related to Medicare payments. Designed to address various situations, this form facilitates requests for adjustments or cancellations of previous claims rather than submitting new ones. It serves as a means to clarify payment responsibilities when multiple insurers are involved, ensuring that Medicare pays only after the primary insurance has processed the claim. For the provider or organization filling it out, the MSP form requires comprehensive details, including the patient’s Medicare number, claim amounts, and insurance information to streamline the resolution process. It is essential that all required documentation, such as the primary payer's Explanation of Benefits (EOB), accompanies the form to prevent delays. Additionally, it's important to note what not to include: a refund check or a UB Claim Form. Providers must also indicate the reason for the request accurately, as any ambiguity might hinder timely processing. Overall, understanding the nuances of the MSP form can significantly ease the complexities surrounding Medicare claims management.
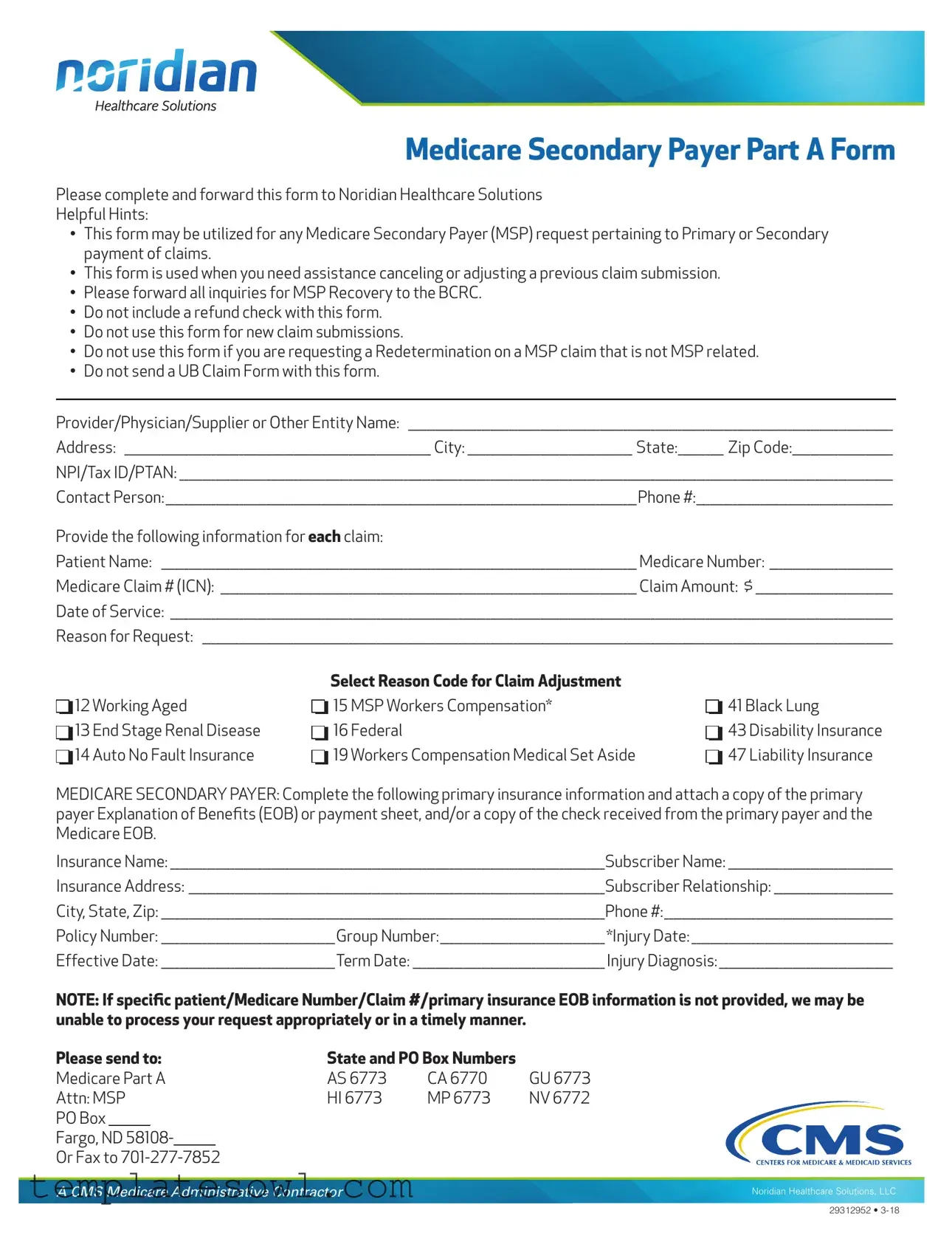
Msp Example
nor;d1an
HealthcareSolutions
Medicare Secondary Payer Part A Form
Please complete and forward this form to Noridian Healthcare Solutions
Helpful Hints:
•This form may be utilized for any Medicare Secondary Payer (MSP) request pertaining to Primary or Secondary payment of claims.
•This form is used when you need assistance canceling or adjusting a previous claim submission.
•Please forward all inquiries for MSP Recovery to the BCRC.
•Do not include a refund check with this form.
•Do not use this form for new claim submissions.
•Do not use this form if you are requesting a Redetermination on a MSP claim that is not MSP related.
•Do not send a UB Claim Form with this form.
Provider/Physician/Supplier or Other Entity Name: __________________________________________________________________________________________________________
Address: ___________________________________________________________________ City: ____________________________________ State:__________ Zip Code:______________________
NPI/Tax ID/PTAN: ____________________________________________________________________________________________________________________________________________________________
Contact Person:_______________________________________________________________________________________________________Phone #:___________________________________________
Provide the following information for each claim:
Patient Name: ________________________________________________________________________________________________________ Medicare Number: ___________________________
Medicare Claim # (ICN): ___________________________________________________________________________________________ Claim Amount: $ ______________________________
Date of Service: ______________________________________________________________________________________________________________________________________________________________
Reason for Request: _______________________________________________________________________________________________________________________________________________________
D
 D
D
 D
D

12 Working Aged
13 End Stage Renal Disease
14 Auto No Fault Insurance
D
 D
D
 D
D

Select Reason Code for Claim Adjustment
15 MSP Workers Compensation*
16 Federal
19 Workers Compensation Medical Set Aside
D
 D
D
 D
D

41 Black Lung
43 Disability Insurance
47 Liability Insurance
MEDICARE SECONDARY PAYER: Complete the following primary insurance information and attach a copy of the primary payer Explanation of Benefts (EOB) or payment sheet, and/or a copy of the check received from the primary payer and the Medicare EOB.
Insurance Name: _______________________________________________________________________________________________Subscriber Name: ____________________________________
Insurance Address: ___________________________________________________________________________________________Subscriber Relationship: __________________________
City, State, Zip: _________________________________________________________________________________________________Phone #:__________________________________________________
Policy Number: ______________________________________Group Number:____________________________________ *Injury Date: ____________________________________________
Effective Date: ______________________________________Term Date: __________________________________________ Injury Diagnosis: ______________________________________
NOTE: If specifc patient/Medicare Number/Claim #/primary insurance EOB information is not provided, we may be unable to process your request appropriately or in a timely manner.
Please send to: |
State and PO Box Numbers |
|
|||
Medicare Part A |
AS 6773 |
CA 6770 |
GU 6773 |
||
Attn: MSP |
HI 6773 |
MP 6773 |
NV 6772 |
||
PO Box |
|
|
|
|
|
Fargo, ND 58108-
Or Fax to
A CMS Medicare Administrative Contractor
Noridian Healthcare Solutions, LLC
29312952 •
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | This form is used for any Medicare Secondary Payer (MSP) requests related to claim payment adjustments or cancellations. |
| Who to Contact | Inquiries for MSP Recovery should be directed to the Benefits Coordination & Recovery Center (BCRC). |
| Prohibited Actions | Do not include refund checks or use this form for new claim submissions. |
| Not for Redetermination | This form should not be used for requesting a Redetermination on MSP claims that are not MSP related. |
| Required Attachments | Attach primary payer Explanation of Benefits (EOB) or payment sheet, as well as the Medicare EOB. |
| Claims Submission Location | Send the completed form to Noridian Healthcare Solutions at the designated address or fax number. |
| Claim Information Required | Mandatory details include patient name, Medicare number, claim number, and reasons for the request. |
| State-Specific Regulations | This form complies with the governing laws of the respective states including Medicare guidelines. |
| Important Note | If specific patient/claim information is not provided, processing may be delayed or incomplete. |
Guidelines on Utilizing Msp
Completing the MSP form is a crucial step in seeking assistance with Medicare claims. By providing accurate information, you can facilitate the processing of your request. Below are the steps to fill out the form correctly.
- Begin by entering your **Name** as the Provider, Physician, Supplier, or Other Entity.
- Fill in your **Address, City, State,** and **Zip Code**.
- Provide your **NPI/Tax ID/PTAN** for identification purposes.
- Identify a **Contact Person** within your organization and provide their **Phone Number**.
- For each claim, write the **Patient Name** and their **Medicare Number**.
- Include the **Medicare Claim Number (ICN)**, the **Claim Amount**, and the **Date of Service** for the claims being adjusted or canceled.
- In the **Reason for Request** section, clearly describe the reason for your request.
- Select the appropriate **Reason Code for Claim Adjustment** from the provided list.
- Complete the primary insurance information. Include the **Insurance Name**, **Subscriber Name**, and their **Address**.
- Fill in the **Subscriber Relationship** to the patient and the associated **City, State, Zip** code for the primary insurance.
- Provide the **Phone Number, Policy Number,** and **Group Number** for the primary insurance.
- Document the **Injury Date**, **Effective Date**, and **Term Date**, if applicable.
- Lastly, indicate the **Injury Diagnosis**, ensuring all necessary information is complete.
After filling out each section, be sure to attach any required documents, such as primary payer Explanation of Benefits (EOB) or payment sheets, to ensure your request is processed smoothly. Once complete, you can send the form to the appropriate address provided or fax it to the specified number.
What You Should Know About This Form
What is the purpose of the MSP form?
The Medicare Secondary Payer (MSP) form is designed to assist in the management of Medicare claims when there is a primary payer involved. This form can be used for requests related to the payment of claims, adjustments to previous submissions, and can facilitate the cancellation of prior claims. It is important to submit this form correctly to ensure timely processing.
Who should complete and submit the MSP form?
The MSP form should be completed by healthcare providers, physicians, suppliers, or entities involved in the billing and claims process. It is crucial that all required information is furnished to avoid delays in the handling of claims.
What information is required when completing the MSP form?
When filling out the MSP form, you will need to provide detailed information including the provider's name, contact details, and the specifics of the claim in question. This includes the patient’s name, Medicare number, claim number, date of service, and the reason for the request. Details of the primary insurance payer must also be included, along with necessary documentation like the Explanation of Benefits (EOB).
Can this form be used to submit new claims?
No, the MSP form is not intended for new claim submissions. It is specifically meant to address adjustments or inquiries regarding existing claims where another insurer is involved. Using this form for new claims will not yield the desired results.
What should I do if I want to request a Redetermination?
If you are seeking a Redetermination that is not related to an MSP claim, you should not use the MSP form. Instead, please follow the appropriate procedures for requesting a Redetermination specific to the type of claim you are dealing with. Ensure you are compliant with all respective guidelines.
What is the importance of providing the primary insurance information?
Providing the primary insurance information is crucial for the MSP process. If this information is not included, or if it is incomplete, it can prevent the request from being processed appropriately or in a timely manner. This can lead to delays in claims payment and potential financial repercussions for providers and patients alike.
Is it necessary to attach any documentation with the MSP form?
Yes, documentation is essential. When submitting the MSP form, you must include a copy of the primary payer’s Explanation of Benefits (EOB) or payment details. Additionally, a copy of the check received from the primary payer and the related Medicare EOB should also be attached to ensure proper processing of your request.
Can I include a refund check with the MSP form?
No, it is not permissible to include a refund check with the MSP form. Such actions can complicate the processing of claims and may result in confusion. Ensure that only the required documentation and information is submitted with the form.
How and where should I submit the MSP form?
The completed MSP form can be submitted via mail to Noridian Healthcare Solutions at the designated PO Box provided in the instructions. Alternatively, it can be sent via fax to the specified fax number. Choose the method that best suits your needs, while ensuring all required attachments are included.
Common mistakes
Filling out the MSP form can be a straightforward process if done correctly. However, there are common mistakes that people often make, which can lead to delays or complications. One frequent error is failing to provide complete information. All fields must be filled out accurately, including patient names, Medicare numbers, and claim amounts. Incomplete submissions may result in the form being sent back, which prolongs the resolution of your issue.
Another mistake is using the form for the wrong purpose. It is essential to remember that this form should not be used for new claim submissions or for requesting a redetermination of claims unrelated to MSP. Each request should be connected to the specific needs outlined for the form to ensure proper processing. Misuse can lead to confusion and further delays.
Many people also neglect to include the necessary documentation. When filling out the MSP form, it’s crucial to attach copies of the primary payer's Explanation of Benefits (EOB) or payment sheets, along with any applicable checks received. Not providing these documents can hinder the evaluation of your claim and could result in incomplete processing.
Lastly, not checking for accuracy before submission can lead to significant setbacks. Small errors in numbers or names can cause processing issues or result in the claim being rejected entirely. Always double-check the information you’ve provided to ensure everything is correct. Taking the time to verify details can save you time and effort down the road.
Documents used along the form
The Medicare Secondary Payer (MSP) form is commonly used for various administrative processes related to Medicare claims. To help streamline these processes, several other forms and documents are frequently needed. Below is a list of those documents, each with a brief description.
- Primary Insurance EOB: The Explanation of Benefits (EOB) from the primary insurer provides details on what has been covered and what is owed, essential for processing claims accurately.
- UB Claim Form: This form is used for hospital claims and provides detailed billing information to both Medicare and secondary payers. However, it should not be sent with the MSP form.
- Redetermination Request Form: Used to contest Medicare's initial claim decision, this form allows providers to request a review of the claim for issues related to payment amounts or service coverage.
- Medicare Part A Claim Form: A specific form for submitting inpatient hospital claims to Medicare, particularly for services covered under Part A.
- Coordination of Benefits (COB) Questionnaire: This document gathers information about all insurance coverages the patient holds. This is critical for determining the order of payment among various insurers.
- Liability Insurance Claim Form: If the claim involves a liability incident, this form details the specifics of the incident and outlines the insurance responsible for covering costs.
- Workers Compensation Form: Used to handle claims that arise from work-related injuries, this form helps to delineate the primary insurance payer's role in coverage.
- Medical Set Aside (MSA) Arrangement Documentation: This document outlines the strategy for funding future medical expenses in Workers' Compensation cases and is crucial for ensuring compliance with Medicare guidelines.
- Request for Evidence of Coverage: Used to obtain proof of coverage details from other insurance providers, this document is significant for verifying eligibility and benefits.
- Provider Reassignment of Benefits Form: This form is necessary when a provider wishes to direct payment to themselves rather than the patient for services rendered under Medicare.
Incorporating these forms appropriately can streamline the claims process and ensure that all necessary information is readily available. Proper documentation increases the likelihood of prompt and accurate processing of Medicare and related claims.
Similar forms
-
CMS-1500 Form: This is a standard form used by healthcare providers to bill for outpatient services. Like the MSP form, it requires detailed patient and insurance information, and it is essential for claim processing.
-
UB-04 Form: A uniform billing form used for hospital services, resembling the MSP form in its purpose of submitting claims to Medicare and other insurance providers. It captures comprehensive information on diagnoses, treatments, and patient details.
-
Medicare Claim Form (CMS-1450): This form serves to bill Medicare for services rendered by hospitals, specifically acute care. Similar to the MSP form, it demands information concerning patients, providers, and services.
-
Medicare Secondary Payer Recovery (MSPRC) Request: This form is utilized when requesting information related to claims adjustments or payments in situations similar to those described in the MSP form. It addresses Medicare's right of recovery for payments made when another payer should have paid first.
-
Reopening Request Form: This document is used when seeking to change a decision made on a Medicare claim. Much like the MSP form, it requires detailed information about the claim and the reasons for the request.
-
Request for Redetermination Form: This form is used to formally appeal an adverse claim decision. Similar in function to the MSP form, it necessitates a clear explanation of why the redetermination is being requested.
-
Medigap Insurance Claim Form: This is used by patients who have supplemental Medicare insurance to cover gaps in Medicare coverage. It shares the MSP form's emphasis on clear patient and provider information, ensuring accurate claim processing.
-
Patient Authorization Form: This document grants permission for healthcare providers to share patient information with insurance companies for billing and claims. Like the MSP form, it serves to ensure that all parties have clear authorization to process claims effectively.
Dos and Don'ts
When filling out the MSP form, follow these guidelines for a smooth process. Here are eight do's and don'ts:
- Do provide accurate personal information, including your name and contact details.
- Do include all necessary details for each claim, such as Medicare numbers and claim amounts.
- Do attach required documentation like the primary payer's Explanation of Benefits (EOB).
- Do double-check your entries to avoid mistakes that could delay processing.
- Don't include a refund check with the form.
- Don't submit this form for new claim submissions.
- Don't use this form if you need a redetermination on a non-MSP related claim.
- Don't send a UB Claim Form along with this MSP form.
By following these simple guidelines, you can ensure a more efficient and effective submission process.
Misconceptions
Misconceptions can often lead to confusion, especially about important forms like the Medicare Secondary Payer (MSP) form. Below are some common misunderstandings regarding this document, along with clarifications.
- MSP Form Is for New Claims: Many believe the MSP form can be used to submit new claims. In reality, it is specifically designed for requests related to adjusting or canceling previous claim submissions.
- Refund Checks Can Be Included: Some individuals think they can attach a refund check to the MSP form. However, this is not allowed and could delay processing.
- It's Only for Primary Insurance Issues: There is a misconception that the MSP form is solely for primary insurance issues. It can actually be used for Medicare Secondary Payer requests, regardless of whether the primary payer is involved.
- All Claims Need an EOB: While it's important to include an Explanation of Benefits (EOB) from the primary payer, many assume this is required for every claim submission. If specific patient or claim information is missing, your request may not be processed promptly.
- The Form Can Be Used for Redeterminations: A common confusion arises when people think the MSP form is suitable for redeterminations on unrelated claims. This form is not appropriate in such cases.
- Claims Can Be Faxed Without Following Up: Some users believe that simply faxing the MSP form guarantees processing. In practice, it's advisable to follow up to ensure everything was received correctly.
- Insurance Information Is Optional: Another misconception is that providing insurance details is optional. In fact, filling out accurate primary insurance information is crucial for effective processing of your request.
- All Types of Insurance Can Be Listed: People often think they can list any type of insurance on the form. The MSP form is limited to specific transactions, such as workers' compensation or liability insurance, which must be clearly identified.
Understanding these misconceptions can help ensure a smoother process when dealing with the MSP form. Always refer to the instructions provided with the form for the most accurate guidance.
Key takeaways
Filling out and using the MSP form correctly is crucial for effective communication with Noridian Healthcare Solutions. Here are key takeaways to ensure smooth processing:
- This form is applicable for any Medicare Secondary Payer (MSP) request, whether it's for primary or secondary payment of claims.
- It can be used to cancel or adjust a previously submitted claim.
- All inquiries regarding MSP Recovery should be directed to the BCRC.
- Do not attach a refund check when submitting the form.
- This form is not intended for new claim submissions.
- Avoid using this form for Redetermination requests on MSP claims that are unrelated to MSP.
- Do not send a UB Claim Form along with the MSP form.
- Ensure accurate patient and claim information is provided to avoid processing delays.
- Always attach the necessary documentation, such as the primary payer's Explanation of Benefits (EOB) or payment sheet.
Browse Other Templates
Welfare Documents - Household dynamics such as marital status and family members' ages can influence program eligibility.
Coworx Staffing Login - Contact CoWorx Staffing for assistance with timesheet completion.