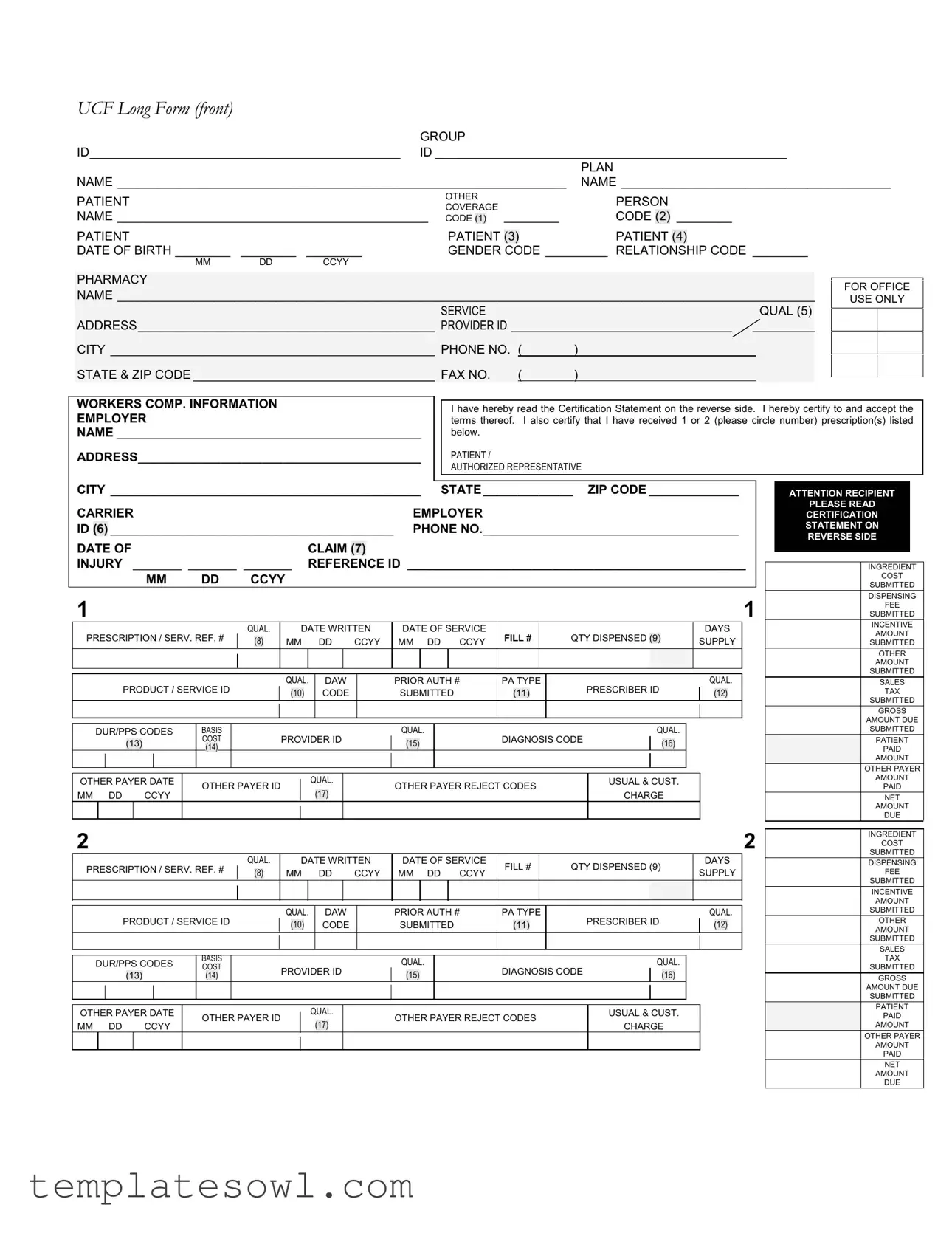
Fill Out Your Ncpdp Billing Form
The NCPDP Billing Form plays a crucial role in the healthcare industry, primarily addressing the needs of pharmacies, healthcare providers, and insurance carriers. To begin with, the form is designed to capture pertinent patient information such as name, date of birth, and insurance details, including group and identification numbers. Each section prompts for specific data that includes plan names and relationships to the patient, ensuring that eligibility for benefits can be accurately assessed. Furthermore, the form encompasses comprehensive fields to document prescription details. This includes the prescription number, service date, quantity dispensed, and diagnosis codes, which are essential for processing claims and ensuring compliance with various healthcare regulations. Additionally, it provides space for both ingredient costs and dispensing fees, enabling pharmacies to detail all components of the transaction. Workers’ compensation claims are also addressed, with dedicated fields to report related information. Upon filling out the form, patients or authorized representatives must sign a certification statement, asserting that all provided information is correct and complete. Overall, the NCPDP Billing Form facilitates a streamlined process for medication reimbursement and effective communication among all parties involved in the healthcare provision and insurance landscape.
Ncpdp Billing Example
UCF Long Form (front)
|
|
|
GROUP |
|
|
|
|
|
|
|
|||
ID_____________________________________________ |
ID ___________________________________________________ |
||||||||||||
|
|
|
|
|
|
|
|
|
PLAN |
||||
NAME _________________________________________________________________ |
NAME _______________________________________ |
||||||||||||
PATIENT |
|
|
|
OTHER |
|
|
PERSON |
|
|
|
|
||
|
|
|
COVERAGE |
|
|
|
|
|
|
||||
NAME _____________________________________________ |
CODE |
|
|
________ |
CODE |
(2) |
________ |
||||||
(1) |
|||||||||||||
PATIENT |
|
|
|
PATIENT |
|
|
PATIENT |
|
|
||||
|
|
|
(3) |
(4) |
|||||||||
DATE OF BIRTH ________ |
________ |
________ |
|
GENDER |
CODE _________ RELATIONSHIP CODE ________ |
||||||||
MM |
DD |
CCYY |
|
|
|
|
|
|
|
|
|
|
|
PHARMACY
NAME _____________________________________________________________________________________________________
SERVICE |
|
|
QUAL (5) |
ADDRESS___________________________________________ PROVIDER ID ________________________________ _________ |
|||
CITY _______________________________________________ PHONE NO. ( |
) |
|
|
STATE & ZIP CODE ___________________________________ FAX NO. |
( |
) |
|
FOR OFFICE
USE ONLY
WORKERS COMP. INFORMATION
EMPLOYER
NAME ____________________________________________
ADDRESS_________________________________________
I have hereby read the Certification Statement on the reverse side. I hereby certify to and accept the terms thereof. I also certify that I have received 1 or 2 (please circle number) prescription(s) listed below.
PATIENT /
AUTHORIZED REPRESENTATIVE
CITY _____________________________________________ STATE _____________ ZIP CODE _____________ |
|||||||
CARRIER |
|
|
|
|
EMPLOYER |
||
ID |
(6) |
_________________________________________ PHONE NO._____________________________________ |
|||||
DATE OF |
|
|
CLAIM |
|
|
||
|
|
(7) |
|||||
INJURY _______ _______ _______ |
REFERENCE ID _________________________________________________ |
||||||
|
|
MM |
DD |
CCYY |
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
||||
PRESCRIPTION / SERV. REF. # |
|
QUAL. |
|
|
DATE WRITTEN |
DATE OF SERVICE |
FILL # |
|
QTY DISPENSED |
|
|
|
|
|
DAYS |
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(9) |
|
|
|
SUPPLY |
|
||||||||||||||||||||
(8) |
MM |
|
DD |
CCYY |
MM DD CCYY |
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
PRODUCT / SERVICE ID |
|
|
|
|
QUAL. |
|
DAW |
|
|
PRIOR AUTH # |
PA TYPE |
|
PRESCRIBER ID |
|
QUAL. |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
(10) |
|
|
CODE |
|
|
SUBMITTED |
|
(11) |
|
|
|
|
|
(12) |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
DUR/PPS CODES |
BASIS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
||||||||||||||
|
|
|
|
(13) |
|
|
|
|
COST |
|
|
|
|
|
PROVIDER ID |
|
|
|
(15) |
|
|
|
DIAGNOSIS CODE |
|
|
(16) |
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
(14) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
OTHER PAYER DATE |
|
OTHER PAYER ID |
|
|
|
|
QUAL. |
|
|
|
OTHER PAYER REJECT CODES |
|
USUAL & CUST. |
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
MM DD |
|
|
|
CCYY |
|
|
|
|
|
|
(17) |
|
|
|
|
|
CHARGE |
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|||||||
PRESCRIPTION / SERV. REF. # |
|
QUAL. |
|
|
DATE WRITTEN |
DATE OF SERVICE |
FILL # |
|
QTY DISPENSED (9) |
|
|
|
|
DAYS |
|
|||||||||||||||||||||||||||||||
|
|
(8) |
|
MM |
|
DD |
CCYY |
MM DD CCYY |
|
|
|
|
SUPPLY |
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
PRODUCT / SERVICE ID |
|
|
|
|
QUAL. |
|
DAW |
|
|
PRIOR AUTH # |
PA TYPE |
PRESCRIBER ID |
|
|
|
|
QUAL. |
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
(10) |
|
|
CODE |
|
|
SUBMITTED |
|
(11) |
|
|
|
|
|
|
(12) |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DUR/PPS CODES |
BASIS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
||||||||||||||
COST |
|
|
|
|
PROVIDER ID |
|
|
|
DIAGNOSIS CODE |
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
(13) |
|
|
|
|
(14) |
|
|
|
|
|
|
|
|
(15) |
|
|
|
|
|
(16) |
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
OTHER PAYER DATE |
|
OTHER PAYER ID |
|
|
|
|
QUAL. |
|
|
|
OTHER PAYER REJECT CODES |
|
USUAL & CUST. |
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
MM DD |
|
|
|
CCYY |
|
|
|
|
|
|
(17) |
|
|
|
|
|
CHARGE |
|
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ATTENTION RECIPIENT
PLEASE READ
CERTIFICATION
STATEMENT ON
REVERSE SIDE
INGREDIENT
COST
SUBMITTED
DISPENSING
FEE
SUBMITTED
INCENTIVE
AMOUNT
SUBMITTED
OTHER
AMOUNT
SUBMITTED
SALES
TAX
SUBMITTED
GROSS
AMOUNT DUE
SUBMITTED
PATIENT
PAID
AMOUNT
OTHER PAYER
AMOUNT
PAID
NET
AMOUNT
DUE
INGREDIENT
COST
SUBMITTED
DISPENSING
FEE
SUBMITTED
INCENTIVE
AMOUNT
SUBMITTED
OTHER
AMOUNT
SUBMITTED
SALES
TAX
SUBMITTED
GROSS
AMOUNT DUE
SUBMITTED
PATIENT
PAID
AMOUNT
OTHER PAYER
AMOUNT
PAID
NET
AMOUNT
DUE
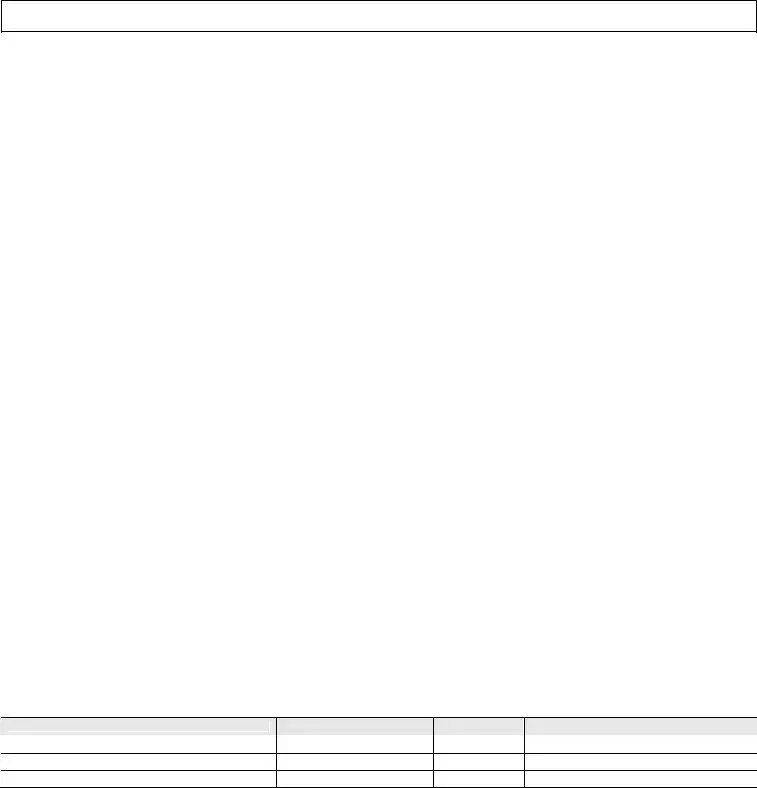
UCF Long Form (back)
IMPORTANT I certify that the patient information entered on the front side of this form is correct, that the patient named is eligible for the benefits and that I have received the medication described. If this claim is for a workers compensation injury, the appropriate section on the front side has been completed. I hereby assign the provider pharmacy any payment due pursuant to this transaction and authorize payment directly to the provider pharmacy. I also authorize release of all information pertaining to this claim to the plan administrator, underwriter, sponsor, policyholder and the employer.
PLEASE SIGN CERTIFICATION ON FRONT SIDE FOR PRESCRIPTION(S) RECEIVED
INSTRUCTIONS
1.Fill in all applicable areas on the front of this form.
2.Enter COMPOUND RX in the Product Service ID area(s) and list each ingredient, name, NDC, quantity, and cost in the area below. Please use a separate claim form for each compound prescription.
3.Worker’s Comp. Information is conditional. It should be completed only for a Workers Comp. Claim.
4.Report diagnosis code and qualifier related to prescription (limit 1 per prescription).
5.Limit 1 set of DUR/PPS codes per claim.
DEFINITIONS / VALUES
1. OTHER COVERAGE CODE
0=Not Specified |
1=No other coverage identified |
2=Other coverage |
3=Other coverage |
4=Other coverage |
5=Managed care plan denial |
6=Other coverage |
7=Other coverage |
8=Claim is billing for a copay |
2.PERSON CODE: Code assigned to a specific person within a family.
3.PATIENT GENDER CODE
0=Not Specified |
1=Male |
4. PATIENT RELATIONSHIP CODE |
|
0=Not Specified |
1=Cardholder |
3=Child |
4=Other |
5. SERVICE PROVIDER ID QUALIFIER |
|
Blank=Not Specified |
01=National Provider Identifier (NPI) |
03=Blue Shield |
04=Medicare |
06=UPIN |
07=NCPDP Provider ID |
09=Champus |
10=Health Industry Number (HIN) |
12=Drug Enforcement Administration (DEA) |
13=State Issued |
99=Other |
|
6.CARRIER ID: Carrier code assigned in Worker’s Compensation Program.
7.CLAIM/REFERENCE ID: Identifies the claim number assigned by Worker’s Compensation Program.
8.PRESCRIPTION/SERVICE REFERENCE # QUALIFIER
Blank=Not Specified |
1=Rx billing |
9.QUANTITY DISPENSED: Quantity dispensed expressed in metric decimal units (shaded areas for decimal values).
10.PRODUCT/SERVICE ID QUALIFIER: Code qualifying the value in Product/Service ID
00=Not Specified
03=National Drug Code (NDC)
06=Drug Use Review/Professional Pharm. Service (DUR/PPS) 09=HCFA Common Procedural Coding System (HCPCS) 12=International Article Numbering System (EAN)
1=Prior authorization 4=Exemption from copay
7=Aid to Families with Dependent Children (AFDC)
2=Female
2=Spouse
02=Blue Cross 05=Medicaid 08=State License 11=Federal Tax ID 14=Plan Specific
2=Service billing
01=Universal Product Code (UPC) 04=Universal Product Number (UPN) 07=Common Procedure Terminology (CPT4) 10=Pharmacy Practice Activity Classification (PPAC) 13=Drug Identification Number (DIN)
2=Medical Certification 5=Exemption from Rx limits
12.PRESCRIBER ID QUALIFIER: Use service provider ID values.
13.DUR/PROFESSIONAL SERVICE CODES: Reason for Service, Professional Service Code, and Result of Service. For values refer to current NCPDP data dictionary.
A=Reason for Service |
B=Professional Service Code |
C=Result of Service |
14. BASIS OF COST DETERMINATION |
|
|
Blank=Not Specified |
00=Not Specified |
01=AWP (Average Wholesale Price) |
02=Local Wholesaler |
03=Direct |
04=EAC (Estimated Acquisition Cost) |
05=Acquisition |
06=MAC (Maximum Allowable Cost) |
07=Usual & Customary |
09=Other |
|
|
15. PROVIDER ID QUALIFIER |
|
|
Blank=Not Specified |
01=Drug Enforcement Administration (DEA) |
02=State License |
03=Social Security Number (SSN) |
04=Name |
05=National Provider Identifier (NPI) |
06=Health Industry Number (HIN) |
07=State Issued |
99=Other |
16. DIAGNOSIS CODE QUALIFIER
Blank=Not Specified |
00=Not Specified |
02=International Classification of Diseases (ICD10) |
03=National Criteria Care Institute (NDCC) |
05=Common Dental Term (CDT) |
|
99=Other |
|
01=International Classification of Diseases (ICD9)
04=Systemized Nomenclature of Human and Veterinary Medicine (SNOMED) 07=American Psychiatric Association Diagnostic Statistical Manual of Mental Disorders (DSM IV)
17. OTHER PAYER ID QUALIFIER
Blank=Not Specified |
01=National Payer ID |
02=Health Industry Number (HIN) |
03=Bank Information Number (BIN) |
04=National Association of Insurance Commissioners (NAIC) |
09=Coupon |
99=Other |
|
|
COMPOUND PRESCRIPTIONS – LIMIT 1 COMPOUND PRESCRIPTION PER CLAIM FORM.
Name
NDC
Quantity
Cost
Form Characteristics
| Fact Name | Details |
|---|---|
| Group Identification | The NCPDP billing form requires a GROUP ID, which helps identify the patient's health plan. |
| Patient Information | Patient details, including name, date of birth, and gender, must be accurately filled out on the form. |
| Provider Identification | A PROVIDER ID is necessary to ensure the pharmacy can be identified and reimbursed for services rendered. |
| Workers' Compensation | If the claim is related to workers' compensation, specific sections of the form must be completed appropriately. |
| Prescription Details | You must include all relevant prescription information, such as the dates and quantities dispensed. |
| Diagnosis Code | A diagnosis code should be reported for prescriptions; only one code is allowed per prescription. |
| Cost Charges | The form includes sections to detail ingredient costs, dispensing fees, and other related charges. |
| State Governing Laws | Each state may have specific regulations governing pharmacy billing practices, such as Medi-Cal in California or Medicaid in Florida. |
| Certification | The person filling out the form must sign a certification statement affirming the accuracy of the information provided. |
Guidelines on Utilizing Ncpdp Billing
Completing the NCPDP Billing form requires careful attention to detail. It will help ensure the billing process goes as smoothly as possible. Follow these steps to accurately fill out the form.
- Begin by filling in the information in the top section: GROUP ID, ID, and PLAN NAME.
- Next, enter the NAME of the patient and other relevant coverage details.
- Provide the DATE OF BIRTH in the format MM/DD/YYYY and select the GENDER CODE and RELATIONSHIP CODE.
- In the PHARMACY NAME field, write the name of the pharmacy, and fill out the ADDRESS, CITY, STATE & ZIP CODE, and PHONE NO..
- Complete the WORKERS COMP. INFORMATION section if applicable. Enter the EMPLOYER NAME and ADDRESS.
- Read and certify acceptance of the Certification Statement.
- Indicate the DATE OF CLAIM (INJURY) and any REFERENCE ID.
- Input the prescription/service details for each prescription including PRESCRIPTION/SERV. REF. #, DATE WRITTEN, DATE OF SERVICE, QUANTITY DISPENSED, and DAYS SUPPLY.
- Complete the PRODUCT/SERVICE ID, DAW, PRIOR AUTH #, PRESCRIBER ID, and any other required fields.
- For each prescription, do not forget to fill out the DIAGNOSIS CODE, OTHER PAYER DETAILS, and billing amounts as needed.
- In the bottom section, summarize all the submitted costs for INGREDIENT COST, DISPENSING FEE, INCREMENTAL AMOUNTS, and SALES TAX.
- Lastly, carefully review all entries to ensure everything is accurate and complete before submitting.
What You Should Know About This Form
What is the NCPDP Billing Form used for?
The NCPDP Billing Form is primarily used for submitting claims for prescription drugs to insurance providers or payer organizations. It captures essential information about the patient, pharmacy, and billing specifics to facilitate the processing of claims related to pharmacy services and medications.
How do I fill out the Group and ID fields?
In these fields, you need to enter the group identification number provided by the patient’s insurance plan and the patient's individual ID number. This information ensures that the claim is processed under the correct insurance policy.
What details are required for the patient's information?
Complete the patient's name, date of birth, gender code, and relationship to the cardholder. This detail is crucial for verifying eligibility and for accurate processing of the claim.
How should I document prescriptions?
You need to list each prescription along with its corresponding details such as date written, date of service, quantity dispensed, and diagnosis code. Make sure to use a separate claim form for each compound prescription.
What is the importance of the Certification Statement?
This statement, located on the reverse side of the form, confirms that the information provided is accurate and that the patient is eligible for the benefits. Signing it allows you to authorize the release of information necessary for the claim processing.
Can I bill for multiple services on one claim form?
The form allows up to two sets of details for prescriptions/services. However, for compound prescriptions, use one form per prescription to provide a clear account of ingredients and their respective details.
What should I do if there is other insurance coverage?
If other insurance coverage exists, indicate it by selecting the appropriate coverage code. This informs the payer about any additional coverage that may apply to the claim, affecting payment responsibility accordingly.
Where should I provide Workers Compensation information?
Complete the Workers Compensation section only if the claim is related to a work-related injury. Make sure to provide all necessary employer details and the claim/reference ID assigned by the Workers Compensation program.
How do I fill in diagnosis and DUR/PPS codes?
Only one diagnosis code and one set of DUR/PPS codes are permitted per prescription. Accurately report these codes to ensure compliance and proper processing of the claim.
What should I do if a field doesn't apply to my claim?
If a field does not apply, it can be left blank unless otherwise specified. Ensure that all required fields, such as patient information and prescription details, are filled out correctly to avoid delays in processing.
Common mistakes
Filling out the NCPDP Billing Form accurately is essential for smooth processing and reimbursement. However, many common mistakes can lead to delays or denials of claims. Recognizing and avoiding these mistakes can help ensure that the billing process runs as efficiently as possible.
One of the most frequent errors occurs in the GROUP ID and PLAN NAME sections. Individuals often leave these fields blank or provide incorrect information. This can severely impact the eligibility verification, causing the claim to be denied. Make sure to double-check these details against the patient’s insurance card.
Another mistake involves the PATIENT DATE OF BIRTH entry. Incorrect dates can lead to confusion regarding the patient’s age and coverage eligibility. This is especially problematic when determining benefits linked to age-specific conditions or treatments.
Gaps in the PATIENT GENDER CODE and RELATIONSHIP CODE fields are also common. Omitting these codes can result in additional scrutiny from insurance companies. It is advisable to include all necessary codes as they directly relate to the claim’s assessment.
Many people neglect to complete the WORKERS COMP. INFORMATION section when applicable. If the claim is being submitted for a worker's compensation case, the relevant employer's information must be included. Failure to provide this information can lead to significant processing delays.
The DIAGNOSIS CODE section tends to be another area where errors occur. Reportedly, some claims include invalid or missing diagnosis codes. Always use the appropriate codes that align with the treatment provided, as insurers are stringent about these requirements.
Incorrectly completing the PRODUCT / SERVICE ID field is also quite common. Submitting the wrong code for a medication or service may lead to denials. When providing compound prescriptions, list the individual ingredients correctly along with their respective NDC numbers; using a separate claim form for each compound is necessary.
Lastly, neglecting to sign the certification statement on the front side of the form can invalidate the submission. This certification serves as an affirmation of the details provided and acceptance of the terms outlined. A missing signature could result in denial of the claim for failure to comply with submission requirements.
In summary, attention to detail helps in preventing errors on the NCPDP Billing Form. Accurate completion can save time, reduce frustration, and ensure that claims are processed without unnecessary delays. Always review and confirm every entry before submitting to maximize the chances of successful reimbursement.
Documents used along the form
The NCPDP Billing form is essential for submitting claims for prescription medication reimbursement. However, several other documents often accompany this form. Each of these documents serves a specific purpose and plays a crucial role in ensuring the claim process runs smoothly.
- Prior Authorization Request Form: This document is required when a medication needs approval from an insurance provider before it can be prescribed. It demonstrates that the medication is necessary and covered under the patient's plan.
- Medicaid Claim Form: Used specifically for Medicaid claims, this form captures essential details about the patient, provider, and services rendered. It ensures that Medicaid pays its fair share for eligible medical expenses.
- Worker’s Compensation Claim Form: If a medication is related to a workplace injury, this form must be filled out to ensure that the claim is processed under Worker’s Compensation. It documents injuries and medical expenses connected to work-related incidents.
- Drug Utilization Review (DUR) Form: This document helps assess the appropriateness and medical necessity of prescribed medications. It provides a checklist of potential issues, ensuring patient safety and compliance.
- Patient Medical History Form: This form collects information about the patient's past medical issues, medications, and allergies. It is vital for understanding the patient's health background and making informed prescribing decisions.
These accompanying forms and documents help streamline the billing process, clarify patient needs, and ensure that claims are handled efficiently. Together with the NCPDP Billing form, they are essential tools in managing medication reimbursement and patient care effectively.
Similar forms
The NCPDP Billing Form is essential for processing pharmacy claims. It shares similarities with various other forms used in the healthcare billing process. Here are four documents that are comparable to the NCPDP Billing Form:
- HCFA 1500 Form: This form is predominantly used for submitting claims for medical services provided by healthcare professionals. Like the NCPDP Billing Form, it requires detailed patient and provider information, tracking of services provided, and has specific fields for diagnoses, procedures, and charges associated with claims.
- CMS-1450 (UB-04) Form: Utilized by hospitals and other facilities for billing services, the UB-04 Form also collects comprehensive data about patient demographics and services rendered. Similar to the NCPDP form, it requires itemized billing and associated diagnosis codes to validate claims for reimbursement.
- Prescription Drug Claim Form: This document is specifically tailored for prescription drug claims submitted by patients or pharmacists directly to insurance companies. Like the NCPDP form, it includes sections for patient identification, prescription details, and pricing information to ensure appropriate reimbursement is processed.
- Workers' Compensation Claim Form: Used for claims relating to workplace injuries, this form shares a focus on capturing the necessary documentation for healthcare services provided due to a work-related incident. It parallels the NCPDP Billing Form by requiring accurate patient details, treatment information, and considerations for applicable payer codes.
Dos and Don'ts
When filling out the NCPDP Billing Form, consider the following guidelines to ensure accurate processing.
- Do: Fill in all required fields completely and accurately.
- Do: Use a separate claim form for each compound prescription.
- Do: Certify the patient information is correct and the patient is eligible for benefits.
- Do: Report only one diagnosis code per prescription.
- Don't: Submit incomplete forms; missing information can delay processing.
- Don't: Use the same claim form for multiple compound prescriptions.
- Don't: Forget to sign the certification section on the front side of the form.
- Don't: Provide incorrect prescription details, as this can lead to claims being denied.
Misconceptions
Understanding the NCPDP Billing Form is essential for ensuring accurate claims processing. However, several misconceptions can lead to errors in submission. Here are six common misunderstandings:
- Only the Pharmacy Uses the Form: Many believe that the NCPDP Billing Form is exclusive to pharmacies. In reality, healthcare providers also use it to submit claims for medication reimbursements.
- Claims Can Be Submitted Without Complete Information: Some think that missing details won’t affect their claims. However, incomplete information often leads to delays or denials of payment.
- All Codes Are Optional: While some fields may not require entry, key codes must be filled out to ensure proper processing. Each code serves a specific purpose and can affect the claim's outcome.
- Only One Claim Per Form: There’s a misconception that multiple claims cannot be submitted on a single form. In fact, the NCPDP form allows for multiple prescriptions or services to be recorded as long as it's done accurately.
- Pharmacy Audits Aren’t Related: Some believe that pharmacy audits have nothing to do with billing. In truth, how a claim is filed can influence audit outcomes, making accuracy and completeness crucial.
- The Certification Statement Is Optional: The significance of the certification statement is often underestimated. Signing it is mandatory, and it confirms that all information on the form is accurate and complete.
By addressing these misconceptions, healthcare teams can facilitate smoother claims processing and improve reimbursement outcomes.
Key takeaways
Filling out the NCPDP Billing form can seem daunting at first, but understanding its key components can make the process smoother. Here are some important takeaways:
- The form requires specific patient information. Double-check all entries for accuracy.
- Fill in the Group ID, ID number, and the plan name clearly.
- Specify the patient's date of birth and select the correct gender code.
- Record the pharmacy name and address neatly.
- Workers’ compensation information is optional and should only be filled out when applicable.
- Ensure to complete the certification statement on the front when signing.
- For compound prescriptions, list the product/service ID and detail each ingredient separately.
- Include the diagnosis code related to the prescription for proper processing.
- Each claim should include a maximum of one set of DUR/PPS codes.
- Make sure you understand the meaning of each qualifier code, as this can affect claim approval.
Using the NCPDP Billing form necessitates thorough attention to detail. This helps ensure that the claim will be processed correctly and efficiently. Familiarize yourself with all required fields to avoid errors.
Browse Other Templates
Dmv Accident Report Form - The DMV uses SR1 data to analyze traffic incidents and enforce safety regulations.
Freight Dispatch Document,Transport Order Bill,Shipping Instruction Form,Cargo Transfer Receipt,Delivery Acknowledgment Document,Lading Agreement Form,Freight Movement Bill,Consignment Shipping Paper,Logistics Transport Bill,Goods Shipment Authorizat - Shipping weight must be indicated in pounds for accurate billing.
What Does Eddm Stand for - Understanding delivery types is crucial for proper routing of mailpieces.