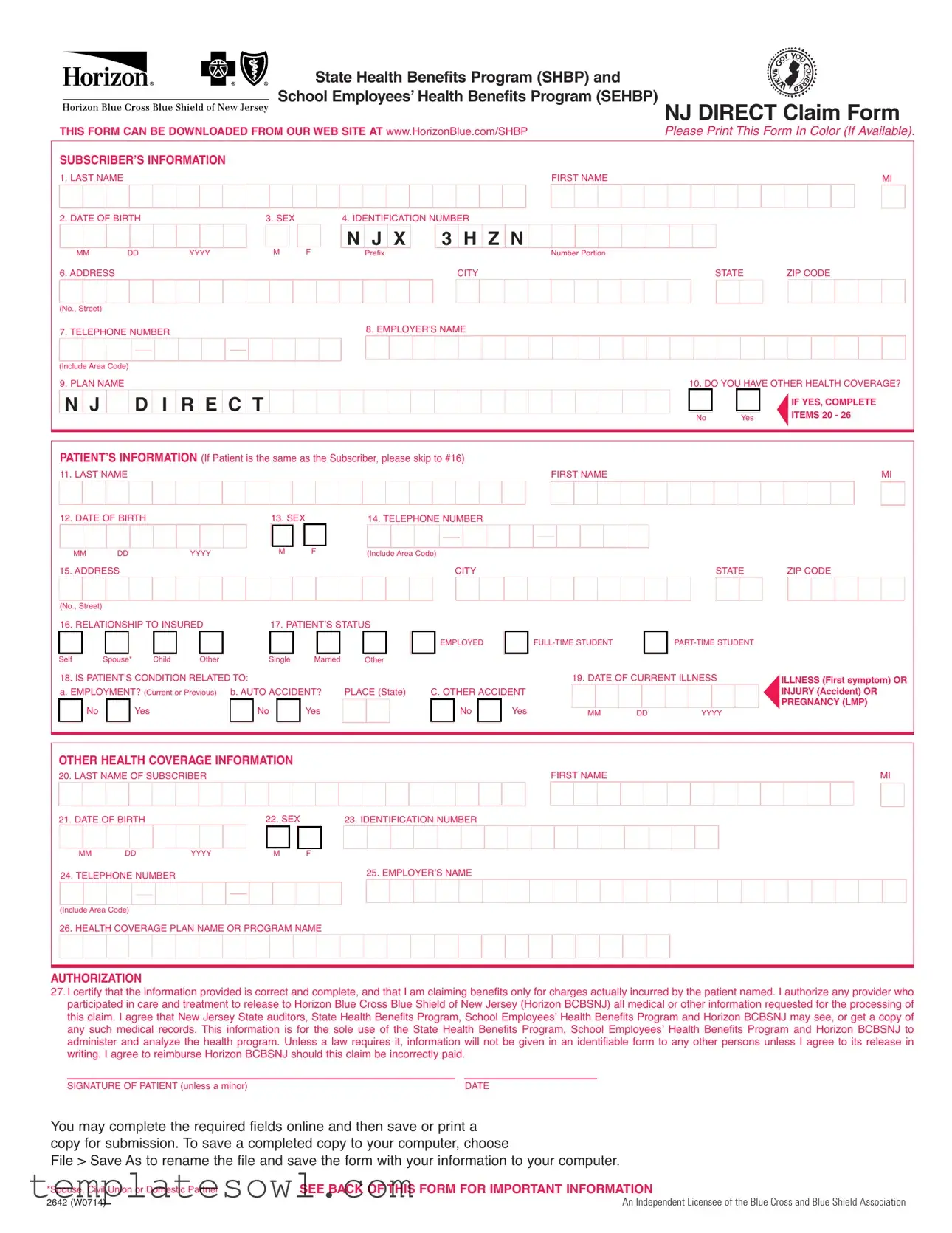
Fill Out Your Nj Direct Claim Form
The NJ Direct Claim form is an essential document for members of the State Health Benefits Program (SHBP) and the School Employees’ Health Benefits Program (SEHBP). This form allows subscribers to request reimbursement for eligible health care expenses. Key sections require personal details about the subscriber, like their name, ID number, and health coverage plan. If the patient is different from the subscriber, additional information must be provided, including the patient's relationship to the insured and any other health coverage they may have. It’s important to note whether the patient’s condition relates to employment or an accident. To process the reimbursement, itemized bills must accompany the claim, clearly detailing the services rendered and any associated charges. This ensures completeness and accuracy, as incomplete submissions may be returned. For individuals who are also covered by Medicare or other insurance plans, pertinent information must be included to coordinate benefits. Once filled out, the claim form can be easily submitted online or by mail to the appropriate Horizon Blue Cross Blue Shield office. Adhering to these guidelines will facilitate a smoother claims process and help ensure timely reimbursements.
Nj Direct Claim Example
State Health Benefits Program (SHBP) and
School Employees’ Health Benefits Program(SEHBP)
THIS FORM CAN BE DOWNLOADED FROM OUR WEB SITE AT www.HorizonBlue.com/SHBP |
NJ DIRECT Claim Form |
Please Print This Form In Color (If Available). |
SUBSCRIBER’S INFORMATION |
|
|
|
|
|
FIRST NAME |
|
MI |
|||
1. LAST NAME |
|
|
|
|
|
|
|
|
|
||
2. DATE OF BIRTH |
|
|
3. SEX |
|
4. IDENTIFICATION NUMBER |
|
|
|
|
||
MM |
DD |
|
YYYY |
M |
F |
N J X |
3 H Z |
N |
Number Portion |
|
|
|
Prefix |
CITY |
|
STATE |
ZIP CODE |
||||||
6. ADDRESS |
|
|
|
|
|
|
|
|
|||
(No., Street) |
|
|
|
|
|
8. EMPLOYER’S NAME |
|
|
|
|
|
7. TELEPHONE NUMBER |
|
|
|
|
|
|
|
||||
(Include Area Code) |
|
|
|
|
|
|
|
10. DO YOU HAVE OTHER HEALTH COVERAGE? |
|||
9. PLAN NAME |
|
|
R E C T |
|
|
|
|
|
|||
N J |
D |
I |
|
|
|
|
|
No |
Yes |
IF YES, COMPLETE |
|
|
|
|
|
|
ITEMS 20 - 26 |
||||||
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
||
PATIENT’S INFORMATION (If Patient is the same as the Subscriber, please skip to #16) |
FIRST NAME |
MI |
||
11. LAST NAME |
|
|
||
12. DATE OF BIRTH |
13. SEX |
14. TELEPHONE NUMBER |
|
|
MM |
DD |
YYYY |
M |
F |
(Include Area Code) |
CITY |
STATE |
15. ADDRESS |
|
|
|
|
|||
ZIP CODE
(No., Street)
16. RELATIONSHIP TO INSURED
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EMPLOYED |
|
||
|
Self |
|
|
Spouse* |
|
|
Child |
|
Other |
|
|
|
Single |
|
|
Married |
|
|
Other |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
18. IS PATIENT’S CONDITION RELATED TO: |
|
|
|
|
PLACE (State) |
|
C. OTHER ACCIDENT |
||||||||||||||||||||
|
a. EMPLOYMENT? (Current or Previous) |
|
b. AUTO ACCIDENT? |
|
||||||||||||||||||||||||
|
|
No |
|
|
|
Yes |
|
|
|
|
No |
|
|
Yes |
|
|
|
|
|
|
|
No |
|
Yes |
||||
|
||
|
||
|
|
|
19.DATE OF CURRENT ILLNESS
MM DD 
 YYYY
YYYY
ILLNESS (First symptom) OR INJURY (Accident) OR PREGNANCY (LMP)
OTHER HEALTH COVERAGE INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIRST NAME |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MI |
|||||||||||||||||||||||
20. LAST NAME OF SUBSCRIBER |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
21. DATE OF BIRTH |
|
|
|
|
22. SEX |
|
|
|
|
23. IDENTIFICATION NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
|
MM |
|
DD |
|
YYYY |
|
|
M |
|
|
|
F |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
25. EMPLOYER’S NAME |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
24. TELEPHONE NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
(Include Area Code)
26. HEALTH COVERAGE PLAN NAME OR PROGRAM NAME
27AUTHORIZATION.I certify that the information provided is correct and complete, and that I am claiming benefits only for charges actually incurred by the patient named. I authorize any provider who participated in care and treatment to release to Horizon Blue Cross Blue Shield of New Jersey (Horizon BCBSNJ) all medical or other information requested for the processing of this claim. I agree that New Jersey State auditors, State Health Benefits Program, School Employees’ Health Benefits Program and Horizon BCBSNJ may see, or get a copy of any such medical records. This information is for the sole use of the State Health Benefits Program, School Employees’ Health Benefits Program and Horizon BCBSNJ to administer and analyze the health program. Unless a law requires it, information will not be given in an identifiable form to any other persons unless I agree to its release in writing. I agree to reimburse Horizon BCBSNJ should this claim be incorrectly paid.
SIGNATURE OF PATIENT (unless a minor)DATE
You may complete the required fields online and then save or print a copy for submission. To save a completed copy to your computer, choose
File > Save As to rename the file and save the form with your information to your computer.
*Spouse, Civil Union or Domestic Partner |
SEE BACK OF THIS FORM FOR IMPORTANT INFORMATION |
2642 (W0714) |
An Independent Licensee of the Blue Cross and Blue Shield Association |
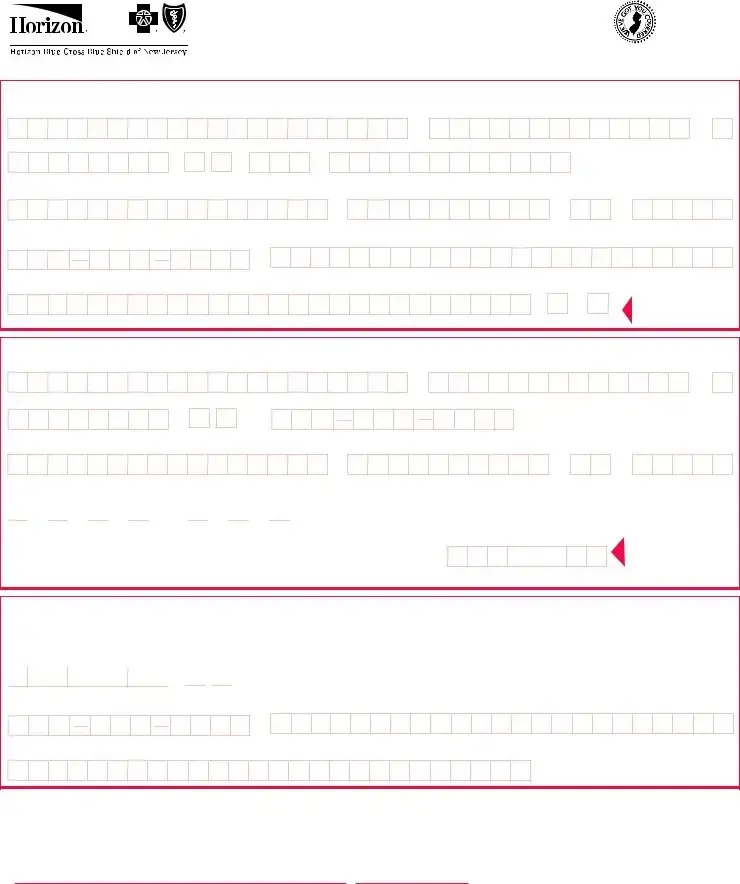
PLEASE READ THIS IMPORTANT INFORMATION
WHEN YOU ARE SUBMITTING EXPENSES FOR MORE THAN ONE FAMILY MEMBER, PLEASE USE A SEPARATE CLAIM FORM FOR EACH PERSON. ITEMIZED BILLS FOR COVERED SERVICES OR SUPPLIES MUST BE ATTACHED TO THIS FORM AND INCLUDE THE FOLLOWING:
Check that each itemized bill is legible and contains ALL of the following information:
☑ NAME & ADDRESS of person or institution rendering the service or supplying the item
☑ PATIENT’S FULL NAME
☑ TYPE of service rendered/produced or item supplied ☑ DATE each service rendered or item supplied
☑ AMOUNT charged for each service rendered or item supplied ☑ DIAGNOSIS of ailment
Cash register receipts, cancelled checks, money order receipts, personal itemizations, and bills only noting a "balance due" are not acceptable.
COORDINATION OF BENEFITS?
If you or your covered dependent(s) are covered by another health insurance program, please provide the information requested in the Other Health Coverage Section. Example: Spouse covered by another insurance company or other Horizon Blue Cross Blue Shield of New Jersey coverage.
When submitting charges for services or supplies that have been partially paid or declined by other group health coverage, attach a copy of the Notice of Payment or Explanation of Benefits from the other health care insurer along with itemized bill(s).
MEDICARE?
If PATIENTis eligible for Medicare Benefits, be sure you include the Explanation of Medicare Benefits (EOMB) that was sent to patient explaining the charges paid or not paid by Medicare.
To process a claim for your NJ DIRECT secondary coverage, we need a copy of the EOMB. This EOMB should have been sent to you when Medicare processed your claim. If your EOMB has more than one page, send us copies of all pages. Please write your NJ DIRECT identification number clearly on the first page.
CLAIM FORM MAY BE RETURNED TO YOU IF THIS ADDITIONAL INFORMATION IS NOT SUPPLIED
HELPFUL HINTS
When you are submitting expenses for more than one family member, please use a separate claim form for each person. It is suggested that you make copies for your own use before you submit the original bills.
Durable medical equipment? (Wheel chair, crutches, braces, oxygen, etc.) Your doctor’s certification must be submitted indicating the expected length of time the equipment will be in use. If renting, please have your medical equipment supplier also indicate the purchase price of the equipment on the bill. Foreign Claim? Bills for services incurred outside of the U.S. must include an English translation and the exchange rate at the time of services.
If you have any questions about how to submit your Claims, please call the Customer Service #
WHERE TO SUBMIT YOUR CLAIM FORMS
Please mail completed claim form for:
MEDICALHorizonCLAIMSBlue CrossTO:Blue Shield of New Jersey
P.O. Box 820
Newark, NJ
MENTALHorizonHEALTH/SUBSTANCEABUSEBlue Cross Blue Shield of NewCLAIMSJersey TO:
Horizon Behavioral Health
P.O. Box 10191
Newark, NJ
ANY PERSON WHO KNOWINGLY FILESFRAUDA STATEMENTWARNINGOF CLAIM CONTAINING ANY FALSE OR
MISLEADING INFORMATION IS SUBJECT TO CRIMINAL AND CIVIL PENALTIES
TO REPORT SUSPECTED FRAUD CALL
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The NJ Direct Claim form is used to submit medical expenses for reimbursement under the New Jersey State Health Benefits Program (SHBP) and School Employees’ Health Benefits Program (SEHBP). |
| Submission Requirements | Complete the form by providing essential information, including identification numbers, dates of service, and itemized bills. Submissions lacking required details may be returned. |
| Governing Laws | The form is governed by the New Jersey Administrative Code (NJAC) and regulations set forth by the SHBP and SEHBP. |
| Additional Coverage | If you have other health coverage, you must provide that information on the form to ensure accurate processing of claims. |
| Submission Address | Completed forms should be mailed to Horizon Blue Cross Blue Shield of New Jersey at P.O. Box 820, Newark, NJ 07101-0820 for medical claims. |
Guidelines on Utilizing Nj Direct Claim
Filling out the NJ Direct Claim form is crucial for processing your healthcare claims effectively. It is important to provide accurate and complete information to avoid delays. Follow these steps to ensure that your claim is submitted properly.
- Download the NJ Direct Claim form from the Horizon Blue Cross Blue Shield of New Jersey website.
- Print the form in color if possible.
- Fill in the subscriber’s information, including:
- First name
- Middle initial
- Last name
- Date of birth (MM/DD/YYYY)
- Sex (M/F)
- Identification number
- Address (No., street, city, state, ZIP code)
- Employer’s name
- Telephone number (include area code)
- Plan name
- Indicate if you have other health coverage by checking 'Yes' or 'No'. If 'Yes', complete items 20-26.
- Provide patient’s information, if different from the subscriber, including:
- First name
- Middle initial
- Last name
- Date of birth (MM/DD/YYYY)
- Sex (M/F)
- Telephone number (include area code)
- Address (No., street, city, state, ZIP code)
- Relationship to the insured (self, spouse, child, other)
- Indicate the patient’s status related to health conditions or accidents. Check 'Yes' or 'No' for each relevant section regarding employment, auto accidents, and the date of current illness or injury.
- Complete the additional health coverage information, including:
- First name and middle initial of the subscriber
- Last name
- Date of birth (MM/DD/YYYY)
- Sex (M/F)
- Identification number
- Employer’s name
- Telephone number (include area code)
- Health coverage plan name or program name
- Read the authorization section carefully, then sign and date your name as the patient unless a minor.
- Include itemized bills for covered services as an attachment. Ensure each bill contains necessary details such as
- Name and address of the provider
- Patient’s full name
- Type of service or item supplied
- Date of each service/item
- Amount charged
- Diagnosis of ailment
- Double-check that all fields are filled in correctly and legibly.
- Mail the completed form along with the attached bills to the appropriate address:
- For medical claims: Horizon Blue Cross Blue Shield of New Jersey, P.O. Box 820, Newark, NJ 07101-0820
- For mental health/substance abuse claims: Horizon Behavioral Health, P.O. Box 10191, Newark, NJ 07101-3189
What You Should Know About This Form
What is the NJ Direct Claim Form?
The NJ Direct Claim Form is a document used to submit health care claims under the State Health Benefits Program (SHBP) and the School Employees’ Health Benefits Program (SEHBP). It collects information about the subscriber and the patient, including details about medical services received, for the purpose of processing claims and determining benefits.
How do I download the NJ Direct Claim Form?
You can download the NJ Direct Claim Form from the Horizon Blue Cross Blue Shield of New Jersey website at www.HorizonBlue.com/SHBP. Ensure to print the form in color if possible, as it aids in processing.
What information is required on the form?
The NJ Direct Claim Form requires various details, including the subscriber's full name, date of birth, identification number, employer's name, and the patient's information. Additionally, it requires specifics about the medical claim, including the type of service rendered, the date of service, and diagnosis of the ailment involved, among other things.
What should I do if I have other health coverage?
If you or the patient have other health coverage, you need to complete the sections related to other health coverage on the form. This includes providing the subscriber name, date of birth, and details of the health coverage plan. Attach any relevant documentation if the claim was partially paid or denied by the other insurer.
What types of bills must be attached to the claim form?
It is crucial to attach itemized bills for covered services or supplies. These bills must clearly show the name and address of the service provider, the patient’s full name, the type of service, the date of service, the amount charged, and the diagnosis. Cash register receipts or bills showing only a "balance due" are not acceptable.
How should claims for durable medical equipment be submitted?
For claims involving durable medical equipment, such as wheelchairs or oxygen, you must include a physician's certification indicating the expected duration of use. If the equipment is rented, the medical supplier should also state the purchase price on the bill.
What if the claim is related to a foreign service?
For services rendered outside of the U.S., you need to provide the itemized bill along with an English translation and the exchange rate at the time the service was received. This ensures that the claim can be processed accurately.
Where do I submit the completed claim form?
There are separate mailing addresses for different types of claims. Medical claims should be mailed to Horizon Blue Cross Blue Shield of New Jersey at P.O. Box 820, Newark, NJ 07101-0820. Mental health or substance abuse claims should be sent to Horizon Behavioral Health at P.O. Box 10191, Newark, NJ 07101-3189.
What should I do if my claim is returned?
If your claim is returned, ensure to check that all required information is complete and legible. Missing or incomplete information is a common reason for claim returns. Review the form thoroughly before resubmitting it along with any necessary documentation.
How can I get assistance with the claim form?
If you have questions about completing the form or submitting claims, you can contact Customer Service at 1-800-414-SHBP (7427) for guidance and support. They can provide helpful direction and clarify any uncertainties you may have.
Common mistakes
Filling out the NJ Direct Claim form can sometimes feel overwhelming, leading to mistakes that could delay your claim processing. One of the most common errors is forgetting to provide complete patient information. This includes details such as the patient’s full name, date of birth, and address. When information is incomplete, claims can be returned, causing frustration and delays in receiving benefits.
Another frequent mistake involves skipping the section about other health coverage. If you have additional health insurance, you must indicate this on the form. Leaving this section blank can lead to misunderstandings about your coverage, ultimately affecting the processing of your claim. It’s essential to include all necessary details regarding other health plans to ensure everything is clear.
A third common error is not attaching the required itemized bills. Each bill must be legible and include crucial information like the name of the service provider, the type of service rendered, and the amount charged. Failing to include this information can lead to claim rejection. It’s important to ensure that the bills are formatted correctly and contain all necessary details.
People often overlook the importance of signing the form. Missing a signature can lead to automatic rejection of the claim, regardless of how well the rest of the form is completed. Always double-check that you’ve signed and dated the form before submitting it to avoid this simple but critical mistake.
Lastly, submitting the form without making a copy for your records is a mistake many make. If any issues arise or questions occur regarding your claim, having a copy can expedite the resolution process. Documenting all correspondence with the insurance provider is essential, not just for organization but also for peace of mind.
Documents used along the form
When filing a claim using the NJ Direct Claim form, there are several other documents that you might need to submit to support your claim. Each of these documents serves a specific purpose in the claims process. Here’s a brief overview of the most common forms and documents often used alongside the NJ Direct Claim form:
- Itemized Bills: These are detailed statements from healthcare providers that list the services rendered, dates of service, and the respective charges. It's essential for these bills to clearly indicate the patient's name and the type of service provided.
- Other Coverage Information: If you or your dependents have additional health insurance, you must provide information about those plans. This includes details such as the subscriber’s name and the plan’s benefits, which helps coordinate benefits between insurers.
- Explanation of Benefits (EOMB): If the patient is covered by Medicare, the EOMB needs to be included. It outlines what Medicare has paid or declined, ensuring that the NJ Direct claim can process any remaining balances.
- Provider's Certification: For claims involving durable medical equipment (DME), a note from the healthcare provider is required. This certification should confirm the necessity of the equipment and the estimated duration of its use.
Each document complements the NJ Direct Claim form, ensuring a smooth processing experience. Be sure to gather all necessary documentation before submission to avoid delays in the claims process.
Similar forms
The NJ Direct Claim Form serves as an important tool for claiming health benefits. It shares similarities with several other documents also designed to facilitate claims and request benefits. Below is a list of documents that are similar to the NJ Direct Claim Form, along with a brief explanation of how they are alike.
- Health Insurance Claim Form (CMS-1500): Like the NJ Direct Claim Form, the CMS-1500 is used to submit health care claims for reimbursement. It requires patient and provider information, along with details of services provided.
- Superbill: This document is a detailed invoice that healthcare providers give to patients for their services. It includes similar information regarding services rendered and can be used to file insurance claims, just like the NJ Direct Claim Form.
- Explanation of Benefits (EOB): While the EOB is generally provided after a claim is processed, it shares the same purpose of detailing what services were covered. Understanding the EOB can help patients know how to properly fill out the NJ Direct Claim Form.
- Medicare Claim Form (CMS-1490S): This form is specifically for Medicare beneficiaries seeking reimbursement for medical expenses. It mirrors the NJ Direct Claim Form in that it collects patient information and details of the healthcare services provided.
- Coordination of Benefits (COB) Form: Used when a patient has multiple insurance coverages, the COB form ensures that all insurers involved are aware of each other. It works hand-in-hand with the NJ Direct Claim Form to ensure proper reimbursement.
- Personal Injury Protection (PIP) Claim Form: In the case of an automobile accident, this form helps individuals file a claim for medical expenses resulting from an injury. It similarly gathers essential information about patients and the medical services required.
- Supplemental Health Claim Form: This form is often used for additional coverage such as gap insurance. It serves a similar purpose to the NJ Direct Claim Form in terms of collecting necessary patient and service information for processing claims.
Dos and Don'ts
When filling out the NJ Direct Claim form, there are some important dos and don'ts to keep in mind. Your accuracy and attention to detail can make the claims process smoother and quicker.
- Do print the form clearly and in color if possible. Clear visibility improves processing.
- Do provide complete and accurate patient and subscriber information. Every field matters.
- Do attach itemized bills for covered services, ensuring they meet the specified requirements.
- Do check for legibility of all receipts and documents submitted with the claim.
- Don't submit cash register receipts or documents that only show a "balance due." They are not acceptable.
- Don't forget to sign the form. Your signature certifies the information is correct.
- Don't include multiple family members on one form. Use a separate claim form for each member.
- Don't ignore additional documentation requests for Medicare claims or other health coverage. Complete information speeds up processing.
Misconceptions
- Misconception 1: The NJ Direct Claim form can be completed casually without precise information.
- Misconception 2: Submission of a claim is a one-step process.
- Misconception 3: All types of receipts are accepted.
- Misconception 4: The NJ Direct claim form does not require additional documentation for Medicare recipients.
Many people believe that minor errors or lacking details won’t affect their claim submission. However, inaccurate or incomplete information can lead to delays or even rejection of the claim. Ensuring accuracy is paramount when filling out the form.
Some assume that filling out the form is the only step needed. In reality, you must also attach itemized bills that meet specific criteria. Claims may be returned if required documents are missing, leading to frustration.
A common misunderstanding is that any type of receipt can be attached to support a claim. Only itemized bills that provide detailed information about services rendered will be accepted. Generic receipts or those indicating only a balance due will not suffice.
Individuals enrolled in Medicare often think that they can submit a claim without additional paperwork. However, it's crucial to include the Explanation of Medicare Benefits (EOMB) to process the claim accurately under NJ Direct secondary coverage.
Key takeaways
Filling out the NJ Direct Claim form accurately ensures that claims are processed without unnecessary delays. Here are some key takeaways to keep in mind:
- Make sure to fill out the form in color, if possible, to maintain clarity.
- Provide detailed subscriber information, including full name, date of birth, and identification number.
- If the patient is different from the subscriber, complete the patient information section to avoid confusion.
- Clearly indicate any other health coverage that the patient may have by answering the relevant questions.
- Attach itemized bills for services or supplies, making sure they are legible and include necessary details such as service type and charges.
- If there are multiple family members submitting claims, use a separate claim form for each individual.
- Keep copies of all documents for your personal records before submitting the originals.
- When claiming durable medical equipment, submit a doctor’s certification stating the expected usage duration.
- Submit completed forms to the designated addresses for medical and mental health claims as specified in the instructions.
By following these guidelines, claim submissions can be streamlined, reducing the likelihood of errors and ensuring that you receive your benefits promptly. Should questions arise during the process, contacting customer service is recommended for further assistance.
Browse Other Templates
Insurance Business Plans - Introducing customer loyalty programs can foster deeper connections with clients.
Mn New Hire Form - The form requires the employee’s Social Security Number for proper identification.
What Is Board Resolution - This document facilitates cooperation among officers in achieving the company’s transactional goals.