Fill Out Your Ohio Bwc Writable C 9 Form
The Ohio BWC Writable C-9 form is a vital document for those navigating the complexities of medical service reimbursement and recommendations for additional conditions related to industrial injuries or occupational diseases. It serves multiple purposes, making it an essential tool for both injured workers and healthcare providers. This form must be properly completed to ensure that requests for medical services are processed efficiently and without delay. Key sections include details about the injured worker, the medical services requested, and any additional conditions being recommended. It's crucial to include all necessary information, such as CPT codes and supporting medical documentation, as any omissions can slow down the processing time. Depending on the type of employer—self-insuring or state-fund—the completed form has different submission paths to follow. Accurate details about the treating physician and the services rendered are mandatory as well, leading to a quicker resolution of the request. Ultimately, the C-9 streamlines the reimbursement process and clarifies any conditions linked to an injury, making it indispensable for ensuring the injured worker receives the care they need.
Ohio Bwc Writable C 9 Example
Completing the Request for Medical Service
Reimbursement or Recommendation for Additional
Conditions for Industrial Injury or Occupational Disease
Instructions
•Please print or type this report.
•If injured worker is employed by a
•If injured worker is employed by a
•To determine the appropriate MCO, ask the injured worker or employer to visit BWC’s Web site at ohiobwc.com, or call BWC at
•Use this form if this is a request for services even if services are being provided under the
•Complete all applicable sections of the form to avoid possible delays in processing this request.
•You can obtain additional copies of this form on ohiobwc.com or by calling BWC at
Section I – Injured worker
1Enter the injured worker’s name, BWC claim number, the date the injured worker was injured or contracted an occupational disease.
Section II – Requested services
2Treating diagnosis for this request to include body part/levels.
3Indicate the beginning and ending date of the requested service. Indicate the last exam or treatment date.
4List the requested services and CPT codes, including frequency and duration. Attach copies of current medical reports necessary to support request. Include any referrals, therapy, medications, diagnostic testing, expected outcomes of medical interventions, results of treatment and ofice notes that contain subjective and objective indings and
*Failure to add CPT codes may delay processing.
5Provide the
Section III – Additional conditions
6Complete if you are recommending additional conditions to the claim. Provide a narrative diagnosis. Supporting medical documentation is required for all conditions listed. Include any referrals, therapy, medications, diagnostic testing, expected outcomes of medical interventions, results of treatment and ofice notes that contain subjective and objective indings and
• BWC will notify all parties and the MCO of the decision.
7This refers to the establishment of a relationship between the injury or occupational disease and the industrial accident or exposure. An explanation is required when answering yes or no.
Section IV – Physician/provider information
8Identify the provider who will render the requested services and the address where he or she will provide the services (required). Travel reimbursement may not be authorized when the service provided is available within 45 miles round trip from the injured worker’s residence.
9Print, type or stamp requesting physician/provider name and address.
10Physician/provider signature, individual BWC provider number and date of this report are mandatory.
Section V –
•If completed by
•If the
•Claim inactive (further investigation required)
•An MCO can only use the disclaimer box on the
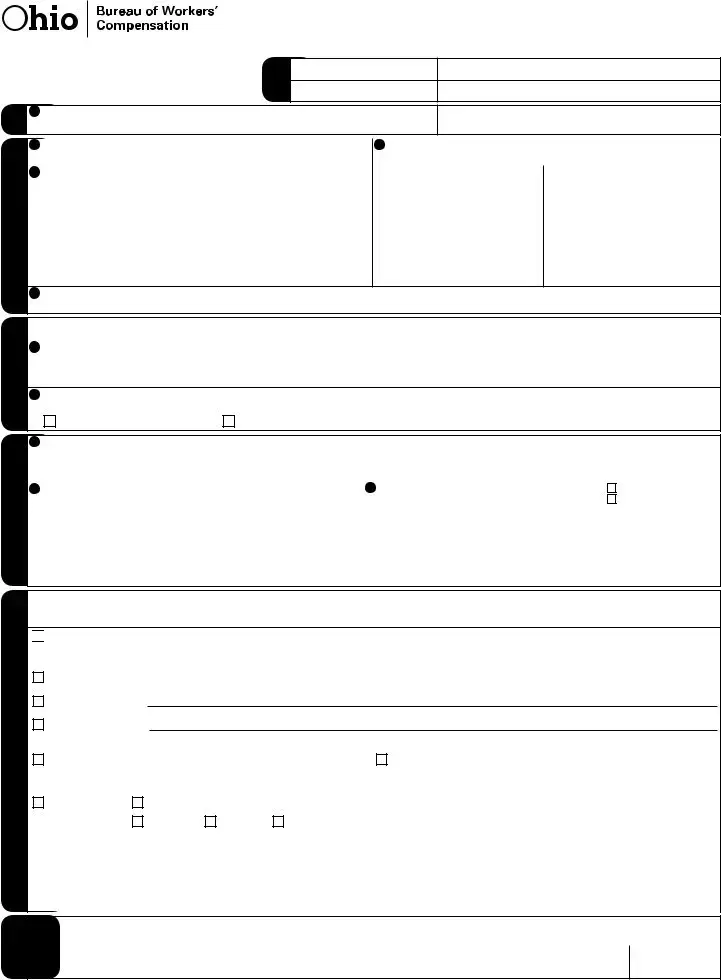
Request for Medical Service Reimbursement or Recommendation for Additional Conditions for Industrial Injury or Occupational Disease
• Instructions for completing the
IW |
1 Injured worker name |
|
|
|
|
Fax note
To
From
|
Phone number |
|
|
Phone number |
|
Fax number |
|
Claim number |
|
Date of injury |
|
|
|
||
|
|
||
|
|
/ |
/ |
II. Requested services |
|
III. Additional conditions |
|
Physician/provider |
information |
IV. |
|
V.
2 |
Treating diagnosis for this request to include body part/levels. |
3 Date service begins |
Date service ends |
Date of last exam or treatment |
|||
|
|
/ |
/ |
/ |
/ |
/ |
/ |
4 |
Requested services with CPT/HCPCS codes (required) |
|
Frequency |
|
|
Duration |
|
1. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. |
|
|
|
|
|
|
|
5Provide the
If you are recommending additional conditions to the claim, supporting documentation is required. You may not use the C9 to request
additional conditions for claims of
6Provide diagnosis (narrative description only), and location and site for conditions you are requesting.
7In your opinion, based on the history from the injured worker, your clinical evaluation and expertise, is the diagnosis or condition causally related, either directly or proximately, to the alleged industrial accident or exposure?
|
Yes, please attach explanation. |
|
No, please attach explanation. |
8Identify the provider who will render the requested services and the address where he or she will provide the services (required).Travel reimbursement may not be authorized when the service provided is available within 45 miles round trip from the injured worker’s residence.
9 |
Requesting physician/provider name and address (please print, type, or |
10 Physician/provider/authorized signature (required) |
POR |
|
stamp) |
|
Not POR — but treating |
|
|
|
physician/provider |
|
|
Individual BWC provider number (required) |
Date (M/D/Y) (required) |
|
|
|
|
I certify the above information is correct to the best of my knowledge. I am aware that any person who knowingly makes a false statement, misrepresentation, concealment of fact or any other act of fraud to obtain payment as provided by BWC or who knowingly accepts payment to which that person is not entitled, is subject to felony criminal prosecution and may, under appropriate criminal provisions, be punished by a ine, imprisonment, or both.
Managed care organization (MCO) — If this page is not faxed or mailed back to the submitting physician/provider within three business days of receipt or within ive business days of receipt of information requested on the

 Approved with disclaimer — This medical payment authorization is based upon a claim or additional condition that BWC/IC is considering as of the date of the MCO’s signature. If the claim or additional condition is ultimately disallowed, BWC may not cover the services/supplies to which this medical payment authorization applies.These services/supplies may be the responsibility of the injured worker (for MCO use only).
Approved with disclaimer — This medical payment authorization is based upon a claim or additional condition that BWC/IC is considering as of the date of the MCO’s signature. If the claim or additional condition is ultimately disallowed, BWC may not cover the services/supplies to which this medical payment authorization applies.These services/supplies may be the responsibility of the injured worker (for MCO use only).
Approved |
Date service begins _____ /_____ /_____ |
Date service ends _____ /_____ /_____ |
Amended approval:
Denied explanation:
You may ile disputes to the decision in writing with supporting documentation to the MCO.
Pending: The documentation requested must be submitted to |
Claim inactive: MCO cannot make a decision on this request, |
||||||||
the MCO case manager within 10 business days to allow for a |
further investigation required. BWC will issue a decision in writing |
||||||||
treatment decision. Failure to respond may result in denial. |
within 28 days. |
|
|
|
|
||||
Withdrawn |
Dismissed |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BWC claim status: |
Allowed |
Denied |
Pending |
|
|
|
|
|
|
MCO |
|
MCO name and signature (print, type or stamp and sign) |
|
|
|||||
(please print, type or stamp) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MCO number |
Telephone number |
Date |
|
|
|
|
|
|
|
|
|
( ) |
/ |
/ |
|
employer |
|||||
authorization for treatment shall be deemed granted, per Ohio Administrative Code |
/ |
/ |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date |
|
|
|
|
|
|
|
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of Form | This form is used to request reimbursement for medical services or to recommend additional conditions associated with an industrial injury or occupational disease. |
| Submission Guidelines | If the injured worker is employed by a self-insuring employer, the form must be mailed or faxed to the employer. For those employed by a state-fund employer, the form should be sent to the appropriate managed care organization (MCO). |
| Additional Conditions | Supporting medical documentation is required when recommending additional conditions. It’s important to note that this form cannot be used for self-insuring employers. |
| Governing Laws | The use and processes surrounding the C-9 form are governed by the Ohio Administrative Code, specifically OAC 4123-19-03 (K)(5). |
Guidelines on Utilizing Ohio Bwc Writable C 9
Follow these steps to complete the Ohio BWC Writable C-9 form. Ensure that all required information is accurate to avoid delays in processing the request. The form must be submitted to the appropriate entity based on the employment status of the injured worker.
- Enter the injured worker’s name, BWC claim number, and the date of the injury or occupational disease.
- In Section II, provide the treating diagnosis, including specific body parts or levels affected.
- Indicate the beginning and ending dates of the requested services as well as the date of the last exam or treatment.
- List the requested services along with their CPT codes, frequency, and duration. Include copies of current medical reports, referrals, therapy, medications, diagnostic testing, expected outcomes, treatment results, and office notes.
- Provide the two-digit facility site of service code as required by the Centers for Medicare and Medicaid Services (CMS), if applicable.
- If additional conditions are being recommended, complete Section III by providing a narrative diagnosis and attaching supporting documentation for all conditions listed.
- Answer whether the diagnosis or condition is related to the industrial accident or exposure. Provide an explanation for either answer.
- In Section IV, identify the provider who will render the services and include their address.
- Print or type the requesting physician/provider's name and address, and ensure the provider's signature, individual BWC provider number, and date are included.
- For self-insuring employers, follow the instructions provided in Section V regarding decision-making and response times.
Once the form is completed, it should be sent to the appropriate entity based on the employment status of the injured worker. Be sure to retain copies of all submitted documents for your records.
What You Should Know About This Form
What is the purpose of the Ohio BWC Writable C-9 form?
The Ohio BWC Writable C-9 form is used to request medical service reimbursement or to recommend additional conditions for workers with industrial injuries or occupational diseases. It gathers necessary information to ensure that the injured worker receives the appropriate medical care and that costs are covered by either a self-insuring employer or a state-fund employer through a managed care organization (MCO).
Who should complete and submit the C-9 form?
The injured worker's physician or provider should complete the C-9 form. Depending on the employer's insurance type, the completed form should then be mailed or faxed to either the self-insuring employer or the appropriate managed care organization (MCO) if the employer is state-funded.
What information is required on the C-9 form?
When completing the C-9 form, you must provide several key pieces of information. This includes the injured worker's name, BWC claim number, dates relevant to the injury or disease, requested medical services, related diagnoses, and supporting medical documentation. It is essential to fill in all applicable sections to avoid delays in processing the request.
Are there specific instructions for providing supporting medical documentation?
Yes, you should include copies of current medical reports that support the request for services. This includes any referrals, therapies, medications, diagnostic testing, and expected outcomes. Proper documentation is crucial, as any omissions can lead to delays.
What should be done if the injured worker is employed by a self-insuring employer?
If the injured worker is employed by a self-insuring employer, the C-9 form should be completed and sent directly to that employer. It is important to follow their specific submission procedures to ensure timely processing of the request.
What happens if the C-9 form is not processed within the specified time frame?
If the C-9 form is not returned to the submitting physician or provider within three business days (for self-insuring employers) or five business days (for state-fund claims), BWC will automatically grant authorization for the requested services, barring any retroactive requests. This process aims to streamline care for the injured worker.
Can additional conditions be requested on the C-9 form?
Yes, additional conditions can be requested, but only for claims that are managed by state-fund employers. When doing so, a narrative diagnosis and supporting medical documentation are required. However, the C-9 form cannot be used for requesting additional conditions for claims managed by self-insuring employers.
Common mistakes
Common mistakes can occur when filling out the Ohio BWC Writable C-9 form, which can lead to delays in processing requests. One prevalent error is failing to complete all applicable sections of the form. Skipping required information can result in longer processing times as additional follow-ups may be needed.
Another mistake is not attaching the necessary medical documentation. Comprehensive support for the request is essential, including reports, referrals, and relevant medical histories. Omitting these can delay approval or even lead to denial of the request entirely.
Many people also forget to use the correct CPT codes when listing requested services. This omission can significantly slow down the review process, as the coding is crucial for proper identification of the services needed.
Incorrectly identifying the appropriate managed care organization (MCO) poses another issue. It is important to confirm the correct MCO before mailing or faxing the form. Errors here could lead to the form being sent to the wrong entity, further delaying necessary responses.
Additionally, not providing a clear narrative diagnosis when recommending additional conditions can create complications. Clear explanations are essential to establish the relationship between the injury and the conditions being claimed.
Some individuals also forget to sign the form or miss including the date, which are mandatory requirements. A missing signature or date can result in the form being returned or rejected by the BWC.
Another common error is incorrect or incomplete information about the physician or provider. Failing to identify the provider’s name and address accurately can lead to confusion and processing issues, impacting the eventual approval of services.
Poor legibility is also a common problem. Handwritten forms should be clear and easy to read, as any confusion can lead to mistakes in data entry at the processing end.
Lack of attention to deadlines can further complicate matters. If the form is not returned to the submitting physician or provider within the established timeframe, the authorization for services may be automatically granted, which could lead to complications later.
Finally, misunderstanding the requirements for travel reimbursement can lead to incorrect assumptions about eligibility. It is important to thoroughly understand the criteria for reimbursement, as travel outside the specified mileage may not be covered.
Documents used along the form
The Ohio BWC Writable C-9 form is vital for facilitating requests for medical service reimbursement related to work injuries or occupational diseases. However, several other forms and documents complement the C-9 and are often necessary for a comprehensive approach to managing claims. Below are five essential documents commonly used in conjunction with the C-9 form.
- BWC C-84: Request for Temporary Total Compensation - This form is used by the injured worker to apply for temporary total compensation benefits. It details the period of time the worker is unable to perform their job duties due to injury and documents the medical information supporting this claim.
- BWC C-3: Injury Report - Also known as the "First Report of Injury," this form is completed by the employer to officially report an injury that occurred at work. It includes basic information about the employee, the nature of the injury, and the circumstances surrounding the incident.
- BWC C-9-A: Request for Additional Information - When the Managed Care Organization requires more details regarding a service request, they use the C-9-A form. This form prompts providers to furnish additional documentation to support ongoing treatments or services recommended for the injured worker.
- BWC C-1: Employee's Report of Injury - This form is completed by the injured employee to provide the BWC with a narrative of the injury. It captures the worker’s firsthand account, helping to establish the context and details of the injury for processing the claim.
- BWC C-157: Review of Medical Services - This form allows a injured worker or their medical provider to request a review of services already rendered. It is essential for addressing any disputes regarding the medical treatments provided and their associated costs.
Understanding these forms can significantly enhance the efficiency of processing a worker's compensation claim. Not only do they create a comprehensive record, but they also ensure that all parties involved have the necessary information to make informed decisions regarding the injured worker’s benefits and care. Familiarity with these documents is crucial for anyone involved in the workers' compensation process in Ohio.
Similar forms
The Ohio BWC Writable C-9 form plays a vital role in the process of requesting medical services reimbursement or recommending additional conditions related to industrial injuries or occupational diseases. There are several other documents that serve similar purposes in this context. Here are four such forms and how they relate to the C-9:
- Ohio BWC C-1 Form: This form is used to report an injury or occupational disease. Like the C-9, it collects essential information about the injured worker, the incident, and related medical conditions. However, the C-1 focuses primarily on the initial reporting rather than requests for medical services.
- Ohio BWC C-3 Form: This form is utilized when a claim is filed, providing a more comprehensive narrative about the injury. Similar to the C-9, it seeks to establish a connection between the injury and employment, but the C-3 is specifically geared toward initiating the claim rather than requesting reimbursement for services.
- Ohio BWC C-9A Form: This document acts as a request for additional medical information or clarification regarding a C-9 submission. Both forms address medical service requests and require supporting documentation, yet the C-9A serves a supplementary purpose focused on enhancing clarity for existing claims.
- Ohio BWC C-161 Form: This form also pertains to medical service requests, much like the C-9. While the C-9 is used for requests related to specific services, the C-161 was designed to address findings from medical examinations. They both require detailed medical documentation but are applied in slightly different circumstances depending on the nature of the request.
Dos and Don'ts
When filling out the Ohio BWC Writable C-9 form, specific best practices will aid in ensuring a smooth submission process. Below are guidelines that outline what to do and what to avoid.
- Do print or type the form clearly to ensure legibility.
- Do verify that you send the form to the correct recipient, based on whether the employer is self-insuring or a state-fund employer.
- Do include all relevant medical documentation and CPT codes to support the request.
- Do provide accurate information regarding the injured worker, including the claim number and details of the injury.
- Do complete all sections of the form to minimize processing delays.
- Don't forget to include the facility site of service code, if applicable.
- Don't submit the form without confirming that all required signatures and provider information are included.
- Don't request additional conditions for claims involving self-insuring employers using this form.
- Don't ignore the guidelines provided for responding to a claim status of "inactive" or "pending."
- Don't leave blank sections that could lead to processing delays; fill in all applicable information.
Following these guidelines can enhance the efficiency and accuracy of the reimbursement or recommendation process for medical services related to industrial injuries or occupational diseases.
Misconceptions
1. The C-9 form is only for state-fund employers. Many believe that this form is solely for state-fund employers. In fact, it is used by both self-insuring employers and state-fund employers, though self-insuring employers have specific guidelines.
2. You don’t need to provide any supporting documentation. Some individuals feel that filling out the form is sufficient. However, it’s essential to attach all necessary medical documentation to avoid delays in processing.
3. CPT codes are optional. A common misconception is that CPT codes can be left out. This is incorrect; including them is crucial. Failing to include these codes can lead to significant processing delays.
4. The C-9 can be used to request additional conditions for self-insuring claims. This is false. The C-9 form cannot be used to request additional conditions for cases involving self-insuring employers. There are separate processes for those claims.
5. All services are automatically authorized. Many may think that submitting the C-9 guarantees authorization for treatment. That's not true. Authorization depends on the claim status and the documentation provided.
6. Travel reimbursement is always available for medical services. Some believe they can always receive travel reimbursement for medical appointments. Reimbursement is not authorized if the service is available within 45 miles round trip of the injured worker’s residence.
7. An MCO can deny a C-9 request at any time. Although MCOs have the authority to deny requests, they cannot do so arbitrarily. They must provide valid reasons, and decisions must follow the established timelines and conditions for the claims.
Key takeaways
The Ohio BWC Writable C-9 form is essential for either requesting medical service reimbursement or for recommending additional conditions related to an industrial injury or occupational disease. Proper completion of the form is crucial to ensure accurate processing of requests.
When filling out the form, clear and legible information must be provided. This includes the injured worker’s name, claim number, and detailed information about requested services, such as CPT codes and necessary medical reports. Inadequate information may lead to delays in service approval.
If the injured worker is employed by a self-insuring employer, the form should be submitted directly to that employer. Conversely, if the employer is state-fund, the completed form must be sent to the appropriate managed care organization (MCO), which can be identified through the BWC website or by phone.
Timely submission is critical. The MCO or self-insuring employer must respond to the C-9 request within a specified timeframe to avoid automatic grant of authorization for treatment, subject to BWC policies. Any failure to adhere to these timelines can significantly affect the injured worker's access to necessary medical services.
Browse Other Templates
Mechanic Lien Nc - This form must be completed for any vehicle left unclaimed for at least 10 days.
How Much Does It Cost to Transfer a Title in Pa - Applicants must certify that the provided information is accurate and truthful.