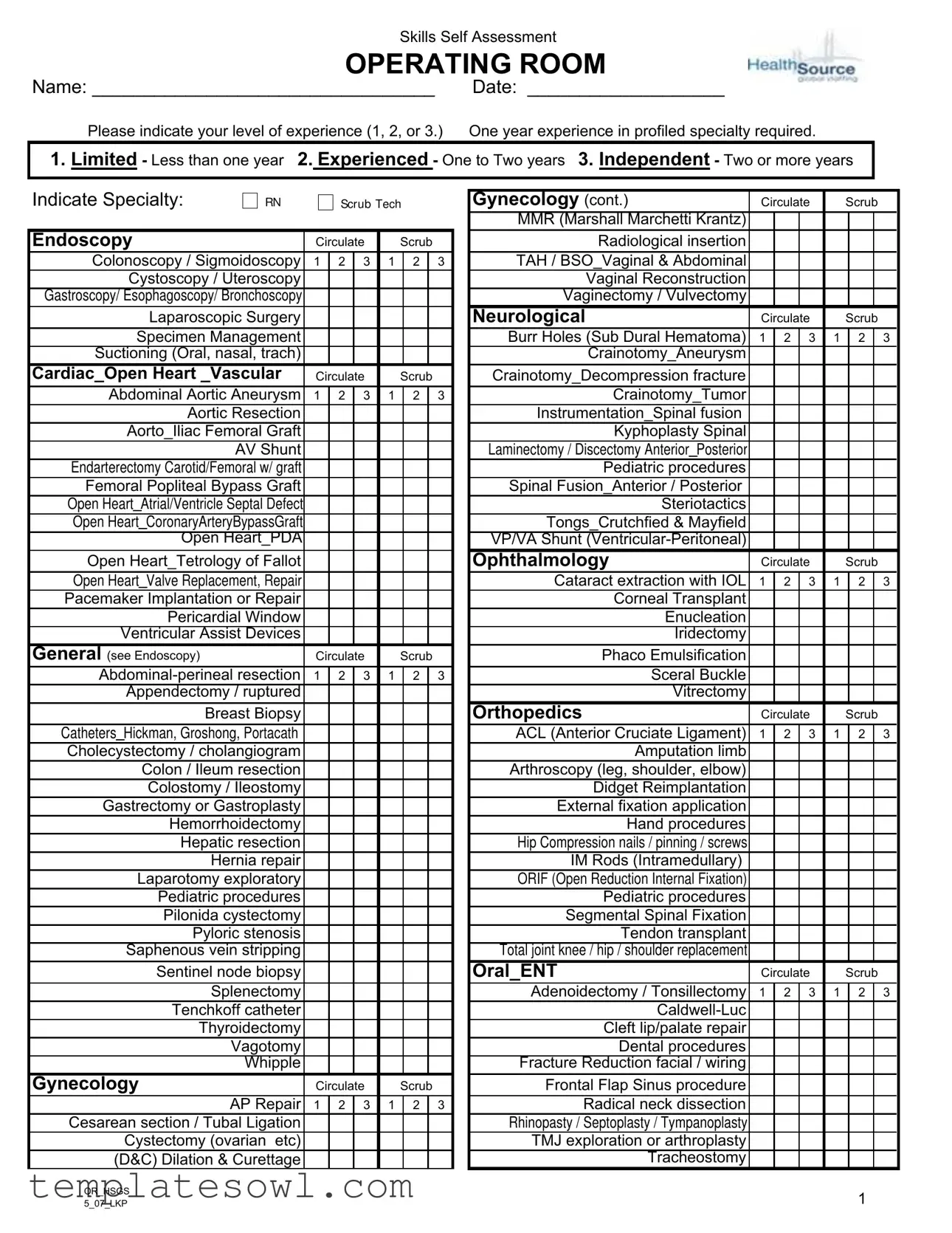
Fill Out Your Operating Room Competency Checklist Form
The Operating Room Competency Checklist form serves as a vital tool for healthcare professionals, particularly those working in surgical settings. This comprehensive document allows individuals to self-assess their skills and experience relevant to various surgical specialties and procedures. It delineates numerous categories, including RN scrub, endoscopy, cardiovascular, and orthopedics, among others, ensuring that all critical areas are covered. Practitioners indicate their experience level—ranging from limited to independent—across a vast array of procedures from simple appendectomies to complex cardiac surgeries. In addition to procedure-specific skills, the checklist also addresses essential equipment usage and care, emphasizing familiarity with various surgical instruments and devices, thus ensuring that team members are well-prepared for their roles. Furthermore, certifications relevant to operating room operations are highlighted, ensuring a standard of competency among personnel. The completion of this checklist not only aids in individual skill assessment but also fosters a culture of accountability and continuous improvement within the operating room environment.
Operating Room Competency Checklist Example
Skills Self Assessment
OPERATING ROOM
Name: _________________________________ |
Date: ___________________ |
Please indicate your level of experience (1, 2, or 3.) |
One year experience in profiled specialty required. |
1. Limited - Less than one year 2. Experienced - One to Two years 3. Independent - Two or more years
Indicate Specialty: |
RN |
|
SCRUB TECH |
|
|||||
|
|
|
|
|
|
|
|
|
|
Endoscopy |
|
Circulate |
|
Scrub |
|
||||
Colonoscopy / Sigmoidoscopy |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
|
Cystoscopy / Uteroscopy |
|
|
|
|
|
|
|
|
|
Gastroscopy/ Esophagoscopy/ Bronchoscopy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Laparoscopic Surgery |
|
|
|
|
|
|
|
|
|
Specimen Management |
|
|
|
|
|
|
|
|
|
Suctioning (Oral, nasal, trach) |
|
|
|
|
|
|
|
|
|
Cardiac_Open Heart _Vascular |
Circulate |
|
Scrub |
|
|||||
|
|
|
|
|
|
|
|
||
Abdominal Aortic Aneurysm |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
|
|
Aortic Resection |
|
|
|
|
|
|
|
|
Aorto_Iliac Femoral Graft |
|
|
|
|
|
|
|
|
|
|
AV Shunt |
|
|
|
|
|
|
|
|
Endarterectomy Carotid/Femoral w/ graft |
|
|
|
|
|
|
|
|
|
Femoral Popliteal Bypass Graft |
|
|
|
|
|
|
|
|
|
Open Heart_Atrial/Ventricle Septal Defect |
|
|
|
|
|
|
|
|
|
Open Heart_CoronaryArteryBypassGraft |
|
|
|
|
|
|
|
|
|
Open Heart_PDA |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Open Heart_Tetrology of Fallot |
|
|
|
|
|
|
|
|
|
Open Heart_Valve Replacement, Repair |
|
|
|
|
|
|
|
|
|
Pacemaker Implantation or Repair |
|
|
|
|
|
|
|
|
|
Pericardial Window |
|
|
|
|
|
|
|
|
|
Ventricular Assist Devices |
|
|
|
|
|
|
|
|
|
General (see Endoscopy) |
Circulate |
|
Scrub |
|
|||||
1 |
2 |
3 |
1 |
|
2 |
|
3 |
||
Appendectomy / ruptured |
|
|
|
|
|
|
|
|
|
|
Breast Biopsy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Catheters_Hickman, Groshong, Portacath |
|
|
|
|
|
|
|
|
|
Cholecystectomy / cholangiogram |
|
|
|
|
|
|
|
|
|
Colon / Ileum resection |
|
|
|
|
|
|
|
|
|
Colostomy / Ileostomy |
|
|
|
|
|
|
|
|
|
Gastrectomy or Gastroplasty |
|
|
|
|
|
|
|
|
|
Hemorrhoidectomy |
|
|
|
|
|
|
|
|
|
Hepatic resection |
|
|
|
|
|
|
|
|
|
|
Hernia repair |
|
|
|
|
|
|
|
|
Laparotomy exploratory |
|
|
|
|
|
|
|
|
|
Pediatric procedures |
|
|
|
|
|
|
|
|
|
Pilonida cystectomy |
|
|
|
|
|
|
|
|
|
|
Pyloric stenosis |
|
|
|
|
|
|
|
|
Saphenous vein stripping |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sentinel node biopsy |
|
|
|
|
|
|
|
|
|
|
Splenectomy |
|
|
|
|
|
|
|
|
Tenchkoff catheter |
|
|
|
|
|
|
|
|
|
|
Thyroidectomy |
|
|
|
|
|
|
|
|
|
Vagotomy |
|
|
|
|
|
|
|
|
|
Whipple |
|
|
|
|
|
|
|
|
Gynecology |
|
Circulate |
|
Scrub |
|
||||
|
AP Repair |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Cesarean section / Tubal Ligation |
|
|
|
|
|
|
|
|
|
Cystectomy (ovarian etc) |
|
|
|
|
|
|
|
|
|
(D&C) Dilation & Curettage |
|
|
|
|
|
|
|
|
|
Gynecology (cont.) |
Circulate |
|
Scrub |
|
||||
|
|
|
|
|
|
|
|
|
MMR (Marshall Marchetti Krantz) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Radiological insertion |
|
|
|
|
|
|
|
|
TAH / BSO_Vaginal & Abdominal |
|
|
|
|
|
|
|
|
Vaginal Reconstruction |
|
|
|
|
|
|
|
|
Vaginectomy / Vulvectomy |
|
|
|
|
|
|
|
|
Neurological |
Circulate |
|
Scrub |
|
||||
Burr Holes (Sub Dural Hematoma) |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Crainotomy_Aneurysm |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Crainotomy_Decompression fracture |
|
|
|
|
|
|
|
|
Crainotomy_Tumor |
|
|
|
|
|
|
|
|
Instrumentation_Spinal fusion |
|
|
|
|
|
|
|
|
Kyphoplasty Spinal |
|
|
|
|
|
|
|
|
Laminectomy / Discectomy Anterior_Posterior |
|
|
|
|
|
|
|
|
Pediatric procedures |
|
|
|
|
|
|
|
|
Spinal Fusion_Anterior / Posterior |
|
|
|
|
|
|
|
|
Steriotactics |
|
|
|
|
|
|
|
|
Tongs_Crutchfied & Mayfield |
|
|
|
|
|
|
|
|
VP/VA Shunt |
|
|
|
|
|
|
|
|
Ophthalmology |
Circulate |
|
Scrub |
|
||||
Cataract extraction with IOL |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Corneal Transplant |
|
|
|
|
|
|
|
|
Enucleation |
|
|
|
|
|
|
|
|
Iridectomy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Phaco Emulsification |
|
|
|
|
|
|
|
|
Sceral Buckle |
|
|
|
|
|
|
|
|
Vitrectomy |
|
|
|
|
|
|
|
|
Orthopedics |
Circulate |
|
Scrub |
|
||||
ACL (Anterior Cruciate Ligament) |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Amputation limb |
|
|
|
|
|
|
|
|
Arthroscopy (leg, shoulder, elbow) |
|
|
|
|
|
|
|
|
Didget Reimplantation |
|
|
|
|
|
|
|
|
External fixation application |
|
|
|
|
|
|
|
|
Hand procedures |
|
|
|
|
|
|
|
|
Hip Compression nails / pinning / screws |
|
|
|
|
|
|
|
|
IM Rods (Intramedullary) |
|
|
|
|
|
|
|
|
ORIF (Open Reduction Internal Fixation) |
|
|
|
|
|
|
|
|
Pediatric procedures |
|
|
|
|
|
|
|
|
Segmental Spinal Fixation |
|
|
|
|
|
|
|
|
Tendon transplant |
|
|
|
|
|
|
|
|
Total joint knee / hip / shoulder replacement |
|
|
|
|
|
|
|
|
Oral_ENT |
Circulate |
|
Scrub |
|
||||
Adenoidectomy / Tonsillectomy |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
|
|
|
|
|
|
|
|
|
Cleft lip/palate repair |
|
|
|
|
|
|
|
|
Dental procedures |
|
|
|
|
|
|
|
|
Fracture Reduction facial / wiring |
|
|
|
|
|
|
|
|
Frontal Flap Sinus procedure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Radical neck dissection |
|
|
|
|
|
|
|
|
Rhinopasty / Septoplasty / Tympanoplasty |
|
|
|
|
|
|
|
|
TMJ exploration or arthroplasty |
|
|
|
|
|
|
|
|
Tracheostomy |
|
|
|
|
|
|
|
|
OR_HSGS |
1 |
5_07_LKP |

Skills Self Assessment
OPERATING ROOM
Plastics |
Circulate |
|
Scrub |
|
||||
Abdominoplasty |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Blepharoplasty |
|
|
|
|
|
|
|
|
Face Lift |
|
|
|
|
|
|
|
|
Flaps_Free / Rotational |
|
|
|
|
|
|
|
|
Liposuction |
|
|
|
|
|
|
|
|
Mammoplasty_Augmentation |
|
|
|
|
|
|
|
|
Mammoplasty_Reduction |
|
|
|
|
|
|
|
|
Mammoplasty_TRAM flap / Reconstruction |
|
|
|
|
|
|
|
|
Radical Mastectomy |
|
|
|
|
|
|
|
|
Split Thickness Skin Graft |
|
|
|
|
|
|
|
|
Thoracic |
Circulate |
|
Scrub |
|
||||
Chest Tube/Drains |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Mediastinoscopy |
|
|
|
|
|
|
|
|
Pneumonectomy_Lobectomy |
|
|
|
|
|
|
|
|
Rib Resection |
|
|
|
|
|
|
|
|
Thoracotomy |
|
|
|
|
|
|
|
|
Thrombectomy_Embolectomy |
|
|
|
|
|
|
|
|
VATS (Video Assisted Thoracoscopy) |
|
|
|
|
|
|
|
|
Transplant_Procurment |
Circulate |
|
Scrub |
|
||||
Bone / Marrow |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Corneal |
|
|
|
|
|
|
|
|
Heart_Lung |
|
|
|
|
|
|
|
|
Kidney |
|
|
|
|
|
|
|
|
Liver |
|
|
|
|
|
|
|
|
Pancreas |
|
|
|
|
|
|
|
|
Trauma |
Circulate |
|
Scrub |
|
||||
Burns |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Gunshot Stab Wounds_Abdomen |
|
|
|
|
|
|
|
|
Gunshot Stab Wounds_Chest |
|
|
|
|
|
|
|
|
Gunshot Stab Wounds_Head |
|
|
|
|
|
|
|
|
MVA with Multiple injuries |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Traumatic Amputations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Urological (see Endoscopy) |
Circulate |
|
Scrub |
|
||||
|
|
|
|
|
|
|
|
|
Bladder Suspension |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
|
|
|
|
|
|
|
|
|
Cysto Retrograde |
|
|
|
|
|
|
|
|
Hypospadias repair |
|
|
|
|
|
|
|
|
Implant_Prosthesis insertion/removal |
|
|
|
|
|
|
|
|
Lithotripsy |
|
|
|
|
|
|
|
|
Nephrectomy |
|
|
|
|
|
|
|
|
Radical Node Dissection |
|
|
|
|
|
|
|
|
Radical Prostatectomy |
|
|
|
|
|
|
|
|
Radium Seed Implants |
|
|
|
|
|
|
|
|
Stent placement |
|
|
|
|
|
|
|
|
TURP |
|
|
|
|
|
|
|
|
Vasectomy |
|
|
|
|
|
|
|
|
I attest the information submitted is true and accurate to the best of my knowledge.
Name (print) ____________________________________________
EQUIPMENT (Use and Care of) |
Circulate |
|
Scrub |
|
||||
Argon Coagulator |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
Autoclave - Flash |
|
|
|
|
|
|
|
|
Cell Saver |
|
|
|
|
|
|
|
|
Cidex Soak |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CUSA |
|
|
|
|
|
|
|
|
Dermatome (Brown, Zimmer, Padgett) |
|
|
|
|
|
|
|
|
Drill assembly / usage (cordless & air/gas) |
|
|
|
|
|
|
|
|
Drills_Codman Cranitome |
|
|
|
|
|
|
|
|
Drills_Midas Rex |
|
|
|
|
|
|
|
|
Drills_Neurotome |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Drills_Surgairtome |
|
|
|
|
|
|
|
|
Electrical surgical unit & grounding pads |
|
|
|
|
|
|
|
|
Endoscopic equipment (camera, video, etc) |
|
|
|
|
|
|
|
|
Endoscopic Fiber optic luminator |
|
|
|
|
|
|
|
|
Harmonic Scaple |
|
|
|
|
|
|
|
|
Hypo/Hyperthermia Unit |
|
|
|
|
|
|
|
|
Intestinal Stapling |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Microscope |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nitrous Oxide |
|
|
|
|
|
|
|
|
Pneumatic tourniquet |
|
|
|
|
|
|
|
|
Robotics |
|
|
|
|
|
|
|
|
Seris unit |
|
|
|
|
|
|
|
|
Sterad machine |
|
|
|
|
|
|
|
|
Table_OR, Fracture, Jackson |
|
|
|
|
|
|
|
|
TPS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ultrasonic cleaner |
|
|
|
|
|
|
|
|
Vac Pack (Bean Bag) |
|
|
|
|
|
|
|
|
Vacuum Curettage |
|
|
|
|
|
|
|
|
Washer Sanitizer |
|
|
|
|
|
|
|
|
Wilson Frame |
|
|
|
|
|
|
|
|
OTHER |
Circulate |
|
Scrub |
|
||||
|
|
|
|
|
|
|
|
|
Blood / Blood Products Administration |
1 |
2 |
3 |
1 |
|
2 |
|
3 |
|
|
|
|
|
|
|
|
|
Catheter Care/Insertion |
|
|
|
|
|
|
|
|
Conscious Sedation |
|
|
|
|
|
|
|
|
Diseases Infectious/Communicable |
|
|
|
|
|
|
|
|
Hemodynamic Monitoring |
|
|
|
|
|
|
|
|
IV Care/Therapy |
|
|
|
|
|
|
|
|
Lab Obtain / Interpret |
|
|
|
|
|
|
|
|
Latex Allergy Guidelines/Procedure |
|
|
|
|
|
|
|
|
O2 Saturations / Oxygen Therapy |
|
|
|
|
|
|
|
|
Pain Assess / Manage |
|
|
|
|
|
|
|
|
Restraints |
|
|
|
|
|
|
|
|
System Assessment |
|
|
|
|
|
|
|
|
Teaching Pt/Others |
|
|
|
|
|
|
|
|
Wound / Dressing Care |
|
|
|
|
|
|
|
|
CERTIFICATIONS |
Expires RN |
Expires ST |
||||||
Certified Scrub Tech |
|
|
|
|
|
|
|
|
CNOR Certification |
|
|
|
|
|
|
|
|
Laser Certification |
|
|
|
|
|
|
|
|
Signature:______________________________ |
Date: ________________________________ |
OR_HSGS |
2 |
5_07_LKP |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Checklist | The Operating Room Competency Checklist is designed to assess the skills and experience levels of healthcare professionals working in the operating room. |
| Self-Assessment Levels | Participants indicate their skill level on a scale of 1 (Limited) to 3 (Independent), which reflects their years of relevant experience. |
| Specialties Covered | The checklist covers various specialties, including RN scrub tech, endoscopy, orthopedics, and urology, among others. |
| Equipment Utilization | It includes sections for self-assessment on equipment use and care, like argon coagulators, electrosurgical units, and robotics. |
| Signature and Attestation | Participants must attest that the information provided is true and accurate by signing the form. |
| Certification Requirements | The checklist asks participants to note any relevant certifications, such as RN or specialty certifications. |
| Infection Control Knowledge | It emphasizes knowledge of infectious diseases and proper protocols for infection control within the operating room setting. |
| State-Specific Governing Laws | In some states, specific laws govern the use of competency checklists in clinical settings. For instance, California’s Business and Professions Code Section 2725 mandates ongoing education for licensed nurses. |
| Documentation of Experience | Participants must document their experience level for a variety of procedures to ensure competency oversight. |
| Training and Education | Training programs often use this checklist as part of their curriculum to meet accreditation standards. |
Guidelines on Utilizing Operating Room Competency Checklist
When preparing to fill out the Operating Room Competency Checklist form, it's essential to gather all relevant information about your experience and specialties. Completing this form accurately is crucial, as it helps assess your competencies in the operating room. Follow the steps below to ensure you fill out the form correctly.
- Start by writing your name in the designated space at the top of the form.
- Enter the date on which you are filling out the form.
- Next, assess your experience level in the specified specialties. Choose from the options: 1 for limited experience (less than one year), 2 for experienced (one to two years), or 3 for independent (two or more years).
- Indicate your specialty by marking the appropriate box. Options include RN, Scrub Tech, and various surgical specialties listed.
- In the sections under each specialty, choose your experience level (1, 2, or 3) for the specific skills listed. Make sure to complete all relevant rows.
- Review the section on equipment use and care. Again, circle your level of experience (1, 2, or 3) for each type of equipment listed.
- In the 'Other' section, assess your competencies and circle the appropriate level (1, 2, or 3) for each area mentioned.
- Lastly, verify your certifications. Record expiration dates for your RN and Scrub Tech certifications, as well as any other relevant certifications.
- Finally, sign and date the form to attest that all the information provided is true and accurate.
What You Should Know About This Form
What is the purpose of the Operating Room Competency Checklist form?
The Operating Room Competency Checklist form is designed to assess and document an individual's skills and experience in various operating room procedures and equipment usage. It helps ensure that healthcare staff have the necessary competencies to perform their roles safely and effectively. By completing this form, personnel can self-evaluate their expertise in specific surgical specialties, guiding management in making informed decisions about training, assignments, and professional development.
How should I indicate my level of experience on the checklist?
The form provides a three-level scale for indicating experience: 1 for Limited (less than one year), 2 for Experienced (one to two years), and 3 for Independent (two or more years). Each procedure listed on the form has corresponding columns for you to mark your level of experience. Be sure to assess your skills accurately to reflect your true abilities.
Is there a requirement for experience in a profiled specialty before completing the checklist?
Yes, the form specifies that at least one year of experience in the chosen specialty is required for completion. Individuals who have less than one year of experience should select a rating of 1 (Limited) for their competencies. This requirement ensures that the assessment is meaningful and accurately reflects the individual’s proficiency for each procedure listed.
What should I do if I find a discrepancy in my skills once the checklist is submitted?
If a discrepancy in skills is identified after submitting the checklist, it is advisable to discuss these concerns with a supervisor or manager. They can guide remedial training opportunities or reassessments as needed. Continuous communication about skills and competencies is vital to maintain safety and effectiveness in the operating room environment.
Common mistakes
When completing the Operating Room Competency Checklist form, many individuals make common mistakes that can lead to inaccuracies in their self-assessment. One significant error is failing to provide their name and date. Without this basic information, the form lacks the essential identifiers needed for tracking competency over time.
Another frequent mistake is misinterpreting the experience levels. The form categorizes skills into three levels: Limited, Experienced, and Independent. Some individuals either overestimate their experience or choose a lower rating out of modesty. This discrepancy can affect future assignments and professional development opportunities.
People often overlook the specialty section which requires specific indications for either RN or Scrub Tech roles. Failing to check the appropriate boxes means that the assessment cannot accurately reflect specialized skills in the Operating Room. This could result in the misallocation of responsibilities that do not match a person's actual capabilities.
Many individuals mistakenly skip certain procedures or skills listed on the form. For instance, if a person has experience in laparoscopic surgery but does not indicate it, they may miss showcasing their relevant expertise. Each unchecked skill could be a missed opportunity for recognition of their experience.
Moreover, some may fill out the form too quickly without taking the time to reflect on their experiences. Rushing through the checklist can lead to omissions or errors. A careful assessment of one's skills is crucial for an accurate representation of capabilities.
In some cases, individuals fail to sign and date the form at the bottom. Without a signature, the form may be considered incomplete or invalid. This action not only validates the information presented but also confirms accountability.
People sometimes neglect to include updates on certifications in the designated section. This omission can misrepresent an individual’s qualifications, as many roles in the Operating Room require current certifications. Keeping these details up to date is vital for maintaining compliance with hospital standards.
Lastly, many individuals do not seek assistance or clarification when needed. If there are uncertainties about how to assess oneself accurately, reaching out for guidance from supervisors or colleagues can help prevent misinterpretation of one’s skills. Collaboration fosters a more accurate and comprehensive assessment, benefiting everyone involved.
Documents used along the form
In the healthcare setting, especially within the operating room, numerous forms and documents work together to ensure smooth operations and patient safety. One of these crucial documents is the Operating Room Competency Checklist form, which assesses the skills and responsibilities of medical staff. In addition to this checklist, there are several other forms that play a vital role in the overall competency and compliance of healthcare practitioners. Understanding these documents can enhance the team's effectiveness and foster an environment of trust and care.
- Skills Assessment Documentation: This form captures a healthcare professional's self-assessment of their skills in various procedures specific to their specialty. It provides insight into their confidence and areas needing improvement.
- Continuing Education Records: Documentation of ongoing training and educational achievements ensures that staff members maintain up-to-date knowledge on the latest techniques and protocols in their field.
- Credential Verification Forms: This form verifies that a healthcare worker's licenses and certifications are current. It serves as a safeguard for patients, assuring them of the expertise and qualifications of the medical team.
- Incident Report Forms: Should any unforeseen situations occur during patient care, this form helps document the details. Reporting such incidents is essential for quality improvement and preventing future occurrences.
- Compliance Checklists: This document outlines essential policies and regulations that need to be adhered to within the operating room. It ensures that best practices are followed, promoting patient safety and institutional accountability.
Collectively, these forms contribute to the comprehensive operation of the operating room. When properly utilized, they enhance communication, support continuous education, and ultimately focus on providing exceptional patient care. Each individual document has its role in creating a cohesive and informed healthcare team.
Similar forms
- Skills Competency Checklist: Similar to the Operating Room Competency Checklist, this form evaluates the proficiency of healthcare professionals in specific skills relevant to their roles. Both documents focus on self-assessment and allow staff to rate their experience levels, ensuring a comprehensive understanding of individual capabilities.
- Clinical Skills Assessment Form: This document is utilized to assess clinicians' practical skills during hands-on procedures and tasks. Like the Operating Room Competency Checklist, it categorizes skills into different areas and requires the individual to assess their experience. Both forms emphasize the importance of ongoing evaluation in clinical settings.
- Application for Clinical Privileges: This application is crucial for healthcare providers seeking to practice specific procedures within a facility. It requires a detailed account of experience, much like the Operating Room Competency Checklist necessitates self-assessment of procedural familiarity, underlying the importance of competency for patient safety.
- Continuing Education Tracking Form: This document records completed training and education efforts of healthcare providers. It shares a common goal with the Operating Room Competency Checklist in ensuring that healthcare professionals maintain and enhance their skills through ongoing education and self-evaluation.
- Performance Evaluation Form: Used during staff performance reviews, this form assesses overall job performance, including technical skills. It bears similarities to the Operating Room Competency Checklist in that both documents require reflection on competence and progression over time, thereby promoting personal and professional development.
Dos and Don'ts
Filling out the Operating Room Competency Checklist form is important for accurately assessing skills. Here are some guidelines on what to do and what to avoid when completing this form:
- Do print clearly when entering your name and date.
- Do take your time to accurately assess your experience level for each specialty.
- Do circle the correct numbers (1, 2, or 3) for your level of experience.
- Do ensure all required fields are complete before submitting the form.
- Don't skip any sections that apply to your experience.
- Don't guess your experience level; be honest about your skills.
- Don't use any abbreviations that might not be understood.
- Don't forget to sign and date the form before submission.
Misconceptions
- Misconception 1: The checklist is only for nurses.
- Misconception 2: The checklist only assesses technical skills.
- Misconception 3: Completing the checklist guarantees competency.
- Misconception 4: You only need to complete the checklist once.
- Misconception 5: The checklist is not necessary for experienced professionals.
- Misconception 6: The form is too complicated to be useful.
- Misconception 7: All competencies are weighted equally.
- Misconception 8: The checklist is only for new hires.
- Misconception 9: The checklist is a punitive tool.
Many believe the Operating Room Competency Checklist is designed solely for registered nurses. In reality, it is applicable to various roles, including scrub techs and other surgical team members.
People often think the checklist focuses only on technical skills related to surgical procedures. It actually covers a broad range of competencies, including patient care, equipment handling, and teamwork skills.
Some assume that filling out the checklist means an individual is fully competent. The checklist serves as a self-assessment tool, but actual competency is determined through ongoing training and evaluations by supervisors.
Many think that the checklist is a one-time requirement. In contrast, it should be regularly updated to reflect changes in skills, experience, or certification.
Some experienced individuals may feel the checklist is unnecessary. However, it is essential for all team members, as it promotes self-reflection and identifies areas for continued growth.
A common belief is that the form's structure makes it hard to navigate. Actually, it provides a clear and organized method to evaluate competencies across various specialties and procedures.
Many think each skill on the checklist carries the same importance. In practice, some competencies are more critical depending on the specific role and surgical environment, impacting patient safety and care.
There is a misconception that the checklist applies only to newly hired staff. In truth, it is useful for all staff members, as it helps maintain high standards of care throughout their careers.
Some view the checklist as a way to penalize staff for deficiencies. However, its primary purpose is to foster learning and improvement, ensuring that all team members can provide safe and effective patient care.
Key takeaways
Completing the Operating Room Competency Checklist form is a vital step in ensuring effective and safe surgical practice. Below are key takeaways to consider when filling out and using this form:
- Self-Assessment is Crucial: Accurately assess your own skills by evaluating your experience level in various specialties. This reflection helps identify areas for growth and improvement.
- Level of Experience: Clearly indicate your level of experience as Limited, Experienced, or Independent. This classification helps supervisors understand where you might need additional support or training.
- Specialty Focus: Specify your specialty and the corresponding skills. Use the checklist to confirm your competency in specific surgical procedures relevant to your role.
- Honesty is Key: Provide truthful information about your experience. The accuracy of this form ensures that patient safety is prioritized and that you are assigned appropriate responsibilities.
- Signature Requirement: Your signature affirms that the information provided is true and accurate. This commitment reflects your professionalism and integrity in the workplace.
- Continuous Learning: Use the checklist not just as a reflection of current skills, but as a tool for planning future training and development opportunities.
- Communication with Supervisors: Engage in conversations with your supervisors or training coordinators after submitting the checklist. Sharing your self-assessment can lead to targeted training sessions designed for your needs.
Filling out this form thoughtfully contributes to a safer operating room environment, ensuring that all staff members are well-prepared and competent in their roles.
Browse Other Templates
If You Win the Lottery Can You Remain Anonymous in California - Contact the Lottery if you have questions about the claims process.
California Sales Tax Exemption - Providing a purchase order or invoice can enhance clarity.
Pa Registration Lookup - Changes or corrections to the lienholder’s name must be accompanied by appropriate documentation.