Fill Out Your Optumrx Prior Authorization Form
The OptumRx Prior Authorization form serves an essential role in managing medication requests between healthcare providers and OptumRx. This form streamlines the process by integrating with CoverMyMeds, which allows for real-time determinations on prior authorization requests, ultimately saving time for both patients and providers. The form requires various pieces of information, including member details like name, date of birth, and insurance ID, as well as provider specifics such as name, NPI number, and contact information. Medication details are critical as well; providers must specify the medication name, its strength and dosage form, and whether the request is for a brand name or a continuation of therapy. Additionally, clinical information is necessary to support the request, including the patient's diagnosis, medications previously attempted, and any related lab results. For patients aged 65 and older, special considerations regarding high-risk medications must also be acknowledged by the prescribing provider. The form also addresses quantity limit requests, allowing for justifications when higher amounts are needed, and emphasizes the importance of submitting all required information to avoid potential denials. This comprehensive form not only facilitates timely access to necessary medications but also ensures compliance with applicable privacy laws, specifically regarding protected health information.
Optumrx Prior Authorization Example
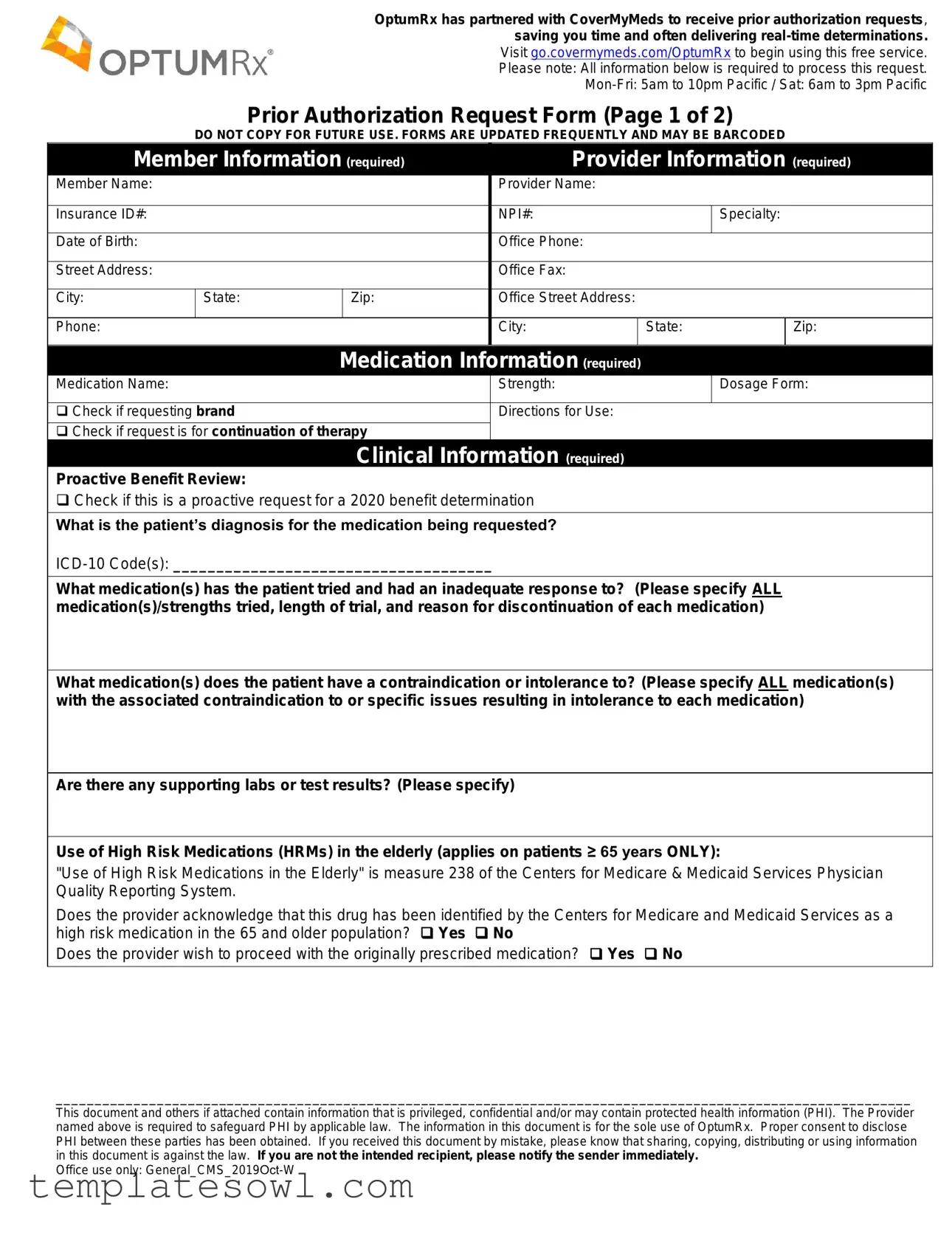
OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering
Visit go.covermymeds.com/OptumRx to begin using this free service.
Please note: All information below is required to process this request.
Prior Authorization Request Form (Page 1 of 2)
DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED
|
Member Information (required) |
|
|
Provider Information (required) |
|
|||||||
|
|
|
|
|||||||||
|
Member Name: |
|
|
|
|
|
Provider Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Insurance ID#: |
|
|
|
|
|
NPI#: |
|
Specialty: |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of Birth: |
|
|
|
|
|
Office Phone: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address: |
|
|
|
|
|
Office Fax: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
State: |
|
Zip: |
|
Office Street Address: |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Phone: |
|
|
|
|
|
City: |
|
State: |
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
Medication Information (required) |
|
|
|
|
|||||
|
Medication Name: |
|
|
|
|
|
Strength: |
|
Dosage Form: |
|||
|
|
|
|
|
|
|
|
|
|
|
||
|
Check if requesting brand |
|
|
|
|
Directions for Use: |
|
|
|
|
||
|
Check if request is for continuation of therapy |
|
|
|
|
|
|
|
||||
|
|
|
|
Clinical Information (required) |
|
|
|
|
||||
|
Proactive Benefit Review: |
|
|
|
|
|
|
|
|
|
|
|
|
Check if this is a proactive request for a 2020 benefit determination |
|
|
|
|
|||||||
|
What is the patient’s diagnosis for the medication being requested? |
|
|
|
|
|||||||
What medication(s) has the patient tried and had an inadequate response to? (Please specify ALL medication(s)/strengths tried, length of trial, and reason for discontinuation of each medication)
What medication(s) does the patient have a contraindication or intolerance to? (Please specify ALL medication(s) with the associated contraindication to or specific issues resulting in intolerance to each medication)
Are there any supporting labs or test results? (Please specify)
Use of High Risk Medications (HRMs) in the elderly (applies on patients ≥ 65 years ONLY):
"Use of High Risk Medications in the Elderly" is measure 238 of the Centers for Medicare & Medicaid Services Physician Quality Reporting System.
Does the provider acknowledge that this drug has been identified by the Centers for Medicare and Medicaid Services as a high risk medication in the 65 and older population? Yes No
Does the provider wish to proceed with the originally prescribed medication? Yes No
______________________________________________________________________________________________________________
This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). The Provider named above is required to safeguard PHI by applicable law. The information in this document is for the sole use of OptumRx. Proper consent to disclose PHI between these parties has been obtained. If you received this document by mistake, please know that sharing, copying, distributing or using information in this document is against the law. If you are not the intended recipient, please notify the sender immediately.
Office use only:
Prior Authorization Request Form (Page 2 of 2)
DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED
Quantity limit requests:
What is the quantity requested per DAY? ______
What is the reason for exceeding the plan limitations?
Titration or
Patient is on a
Requested strength/dose is not commercially available
There is a medically necessary justification why the patient cannot use a higher commercially available strength to achieve the same dosage and remain within the same dosing frequency. Please specify: _______________________________
Patient requires a greater quantity for the treatment of a larger surface area [Topical applications only]
Other: ______________________________________________________________________________________
Note: If the patient exceeds the maximum FDA approved dosing of 4 grams of acetaminophen per day because he/she needs extra medication due to reasons such as going on a vacation, replacement for a stolen medication, provider changed to another medication that has acetaminophen, or provider changed the dosing of the medication that resulted in acetaminophen exceeding 4 grams per day, please have the patient’s pharmacy contact the OptumRx Pharmacy Helpdesk at (800) 788- 7871 at the time they are filling the prescription for a
Are there any other comments, diagnoses, symptoms, medications tried or failed, and/or any other information the physician feels is important to this review?
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Please note: This request may be denied unless all required information is received.
If the patient is not able to meet the above standard prior authorization requirements, please call
This form may be used for
______________________________________________________________________________________________________________
This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). The Provider named above is required to safeguard PHI by applicable law. The information in this document is for the sole use of OptumRx. Proper consent to disclose PHI between these parties has been obtained. If you received this document by mistake, please know that sharing, copying, distributing or using information in this document is against the law. If you are not the intended recipient, please notify the sender immediately.
Office use only:
Form Characteristics
| Fact Name | Detail |
|---|---|
| Partnership with CoverMyMeds | OptumRx has collaborated with CoverMyMeds to streamline prior authorization requests, often providing real-time determinations. |
| Service Availability | The prior authorization request service is available Monday to Friday from 5am to 10pm Pacific and Saturday from 6am to 3pm Pacific. |
| Required Information | All information on the form is mandatory for processing the prior authorization request. |
| Form Updates | This form is frequently updated. Copies of older versions are not valid. |
| Medication Strength and Form | Providers must specify the medication's name, strength, dosage form, and whether the request is for a brand-name medication or for continuation of therapy. |
| Clinical Information Required | The form asks for details about the patient's diagnosis, previous medications tried, and any contraindications or intolerances to medications. |
| Approval for High Risk Medications | For patients aged 65 and older, providers must acknowledge if the medication is considered high risk by the Centers for Medicare & Medicaid Services. |
| Quantity Limit Justifications | Existing criteria for quantity limit requests must be supported by valid justifications, such as titration or medically necessary reasons. |
| Denial Risk Notice | The request may be denied if all required information is not provided; follow-up contact numbers are available for assistance. |
Guidelines on Utilizing Optumrx Prior Authorization
Filling out the OptumRx Prior Authorization form accurately is essential to ensure that the request is processed smoothly. Follow the steps below to complete the form effectively.
- Visit the CoverMyMeds website: Go to go.covermymeds.com/OptumRx to access the service.
- Enter member information: Fill in the member's name, insurance ID number, date of birth, and address details.
- Provide provider information: Enter the provider's name, NPI number, specialty, and office contact information.
- Gather medication information: Specify the medication name, strength, dosage form, and whether you're requesting a brand name.
- Fill out directions for use: State how the medication should be taken and whether this request is for continuing therapy.
- Detail clinical information: Include the patient’s diagnosis, ICD-10 code, and any medications previously tried along with reasons for discontinuation.
- Include contraindications: List any medications the patient cannot take or has had an intolerance to.
- Document supporting labs: Note any relevant lab or test results that support the request.
- Address high-risk medications: If the patient is 65 or older, indicate whether the provider acknowledges the prescription as a high-risk medication and if they wish to proceed.
- Complete quantity limit requests: Note the quantity requested per day and provide a reason for exceeding the plan limitations if applicable.
- Provide additional comments: Share any other relevant information, diagnoses or medications that may aid in the review.
- Submit the form: Send the completed form to the appropriate fax number, which is 1-844-403-1028, for non-urgent requests or call 1-800-711-4555 for urgent requests.
What You Should Know About This Form
What is the OptumRx Prior Authorization form used for?
The OptumRx Prior Authorization form is used to request the approval of certain medications that require prior authorization before they can be covered by insurance. By completing this form, healthcare providers can ensure that necessary medications are reviewed and approved in a timely manner, helping patients access their treatments without unnecessary delays.
Where can I submit the OptumRx Prior Authorization form?
You can submit the OptumRx Prior Authorization form through CoverMyMeds at go.covermymeds.com/OptumRx. This service allows for easier submissions and often provides real-time determinations. Alternatively, you can fax the completed form to 1-844-403-1028 for non-urgent requests.
What information is required on the form?
To process a request, all sections of the form must be completed. This includes member information, provider information, medication details, clinical information, and any additional comments relevant to the request. Complete and accurate information is essential for the request to be reviewed promptly.
What happens if the information provided is incomplete?
The request may be denied if all required information is not received. It is crucial to fill out each section thoroughly. Furthermore, if additional information is necessary, providers may be contacted for clarification to help expedite the review process.
Are there urgent requests for prior authorization?
Yes, there is a process for urgent or expedited requests. For urgent needs, you can call 1-800-711-4555. This ensures that critical medication needs are addressed quickly, which can be crucial for patient care.
What if I need assistance while filling out the form?
If you need help while filling out the OptumRx Prior Authorization form, you can reach out to the OptumRx Pharmacy Helpdesk at 1-800-788-7871. They can provide guidance, clarify requirements, and assist you in completing the form accurately to facilitate the approval process.
Common mistakes
Filling out the OptumRx Prior Authorization form is crucial for ensuring that patients receive the medications they need. However, mistakes can lead to delays or denials in authorization. One common error is omitting necessary information. Every section of the form requires specific details, including patient and provider information, medication specifics, and clinical details. Leaving sections blank or failing to provide complete answers can significantly slow the process.
Another frequent mistake is insufficient clinical justification. When describing a patient’s diagnosis or previous treatments, vague answers or lack of detail may occur. It's essential to include the exact medication names, strengths, lengths of trial, and reasons for discontinuation. This information provides the reviewer with insights that are vital for the decision-making process.
Not including the correct ICD-10 codes is also a common pitfall. These codes are critical for accurately identifying the patient's diagnosis. If the codes are missing or incorrect, it can directly impact the approval status. Make sure to verify that these codes are up-to-date and correctly matched to the diagnosis.
Another area where errors can arise is in the medication history. When listing the medications the patient has previously tried, it’s important to specify every medication, including all strengths used. Additionally, mentioning any contraindications or intolerances is necessary. Skipping this step or providing incomplete information might lead to a misunderstanding of the patient's needs by the reviewing party.
Some individuals forget to check the appropriate boxes indicating critical information, such as whether the request is for a continuation of therapy or if it's a proactive request. These checks help streamline the review process by highlighting essential facts about the authorization request. Missing this step can cause unnecessary confusion.
Another mistake involves misunderstanding quantity limits. When requesting medication quantities, if the requested amount exceeds the plan's limits, a valid reason must be provided. A lack of clarity regarding why a higher quantity is needed can lead to denials. In cases where a medically necessary justification is required, be sure to elaborate on the reasoning in detail.
Finally, overlooking the need for complete supporting documentation can hinder approval. If there are relevant lab results, test outcomes, or other pertinent information that could support the request, attaching those documents is essential. Omitting this information may result in the request being flagged for further review or declined outright.
Documents used along the form
The OptumRx Prior Authorization form is an essential document for healthcare providers when requesting coverage for certain medications. Along with this form, several other documents and forms are commonly used to facilitate this process. Each document serves a specific purpose in providing necessary information or supporting details to streamline the prior authorization request.
- Clinical Summary: A document outlining the patient’s medical history, diagnoses, and treatment plans relevant to the medication being requested. It offers a comprehensive view of the patient's health for the reviewer.
- Medication History Form: This form details the medications the patient has previously taken, including dosages and durations, to show previous treatments and their outcomes.
- Lab Results: Recent lab test results can demonstrate the need for the requested medication, especially if the patient has specific medical conditions that the medication addresses.
- Urgent Care Notes: Documentation from urgent care visits can provide insights into the patient’s acute conditions or worsening symptoms, supporting the need for immediate medication access.
- Insurance Benefit Verification: A document confirming the patient’s benefits and coverage options. This helps ensure that the requested medication is covered under the patient’s plan.
- Drug Interaction Check: A report showing potential drug interactions for the proposed medication, highlighting any safety concerns regarding current patient prescriptions.
- Prescribing Provider Statement: A letter from the prescribing healthcare provider justifying the need for the specific medication, including reasons for selecting it over alternatives.
- Patient Consent Form: A document indicating that the patient has authorized the healthcare provider to share their medical information necessary for the prior authorization process.
- Pharmacy Records: Documentation from the patient’s pharmacy that may include previous prescriptions and refill history relating to the medication in question.
- Discontinuation Notification: A notice explaining any discontinuation of prior medications, including reasons that may necessitate the new prescription being requested.
These documents work in tandem with the OptumRx Prior Authorization form to support a more efficient review process. Providing comprehensive and accurate information can lead to quicker determinations and ultimately enhance patient care.
Similar forms
- Medicare Prior Authorization Form: Similar to the OptumRx form, this document also requests detailed patient and provider information, medication details, and clinical justification, ensuring compliance with regulations and coverage guidelines before medication approval.
- Medicaid Prior Authorization Form: Like the OptumRx form, it requires comprehensive patient data, medication use history, and clinical rationale to approve prescriptions, often used for controlled substances or expensive therapies.
- Commercial Insurance Prior Authorization Form: This form closely resembles the OptumRx document by requiring specifics about patient treatments, previous therapy attempts, and supporting medical information to facilitate prompt insurance review.
- Drug Utilization Review (DUR) Form: Both documents collect patient medication history and physician notes to evaluate the appropriateness of prescribed medications and ensure safe practices in pharmacotherapy.
- Continuity of Care Document (CCD): This document provides similar patient history data and treatment details, focusing on maintaining seamless care between providers, somewhat paralleling the detailed clinical information in the OptumRx form.
- Clinical Trials Application Form: While different in purpose, this form requests detailed patient information and medical history, akin to the extensive data requirements found in the OptumRx Prior Authorization form to assess eligibility for the trial.
Dos and Don'ts
When filling out the OptumRx Prior Authorization form, consider the following:
- Provide complete and accurate patient information. Ensure all member details, including name and insurance ID, are correctly filled in.
- Include relevant medication details. Specify the medication name, strength, and dosage form clearly.
- Detail previous medications used. List all medications tried, the duration of trials, and why they were discontinued.
- Check for any high-risk medications. If applicable, indicate whether the medication has been recognized as high risk for patients 65 and older.
- Avoid missing required information. Double-check that all sections requiring input are completed to prevent delays.
- Do not submit outdated forms. Ensure you are using the most current version of the form, as they are frequently updated.
By following these guidelines, you can help ensure a smooth submission process for prior authorization requests.
Misconceptions
Here are some common misconceptions about the OptumRx Prior Authorization form:
- Misconception 1: The form is only for certain medications.
- Misconception 2: You can send the form later if you forget some information.
- Misconception 3: You must request a prior authorization for every prescription.
- Misconception 4: The process is always lengthy and complicated.
Many people think the Prior Authorization form applies to a select few drugs. In reality, it can be used for a wide range of medications that require pre-approval from insurance before being covered.
This belief can lead to delays. All required information must be included when submitting the request. If anything is missing, the request may be denied, and you'll have to start over.
Not all prescriptions require prior authorization. Patients may only need to fill out this form if their medication falls under specific conditions set by the insurance provider.
While some requests may take time, utilizing the partnership with CoverMyMeds can often result in quicker determinations. Many requests can even be resolved in real-time, making it much easier for both providers and patients.
Key takeaways
- Complete all sections of the OptumRx Prior Authorization form to ensure timely processing. Incomplete forms may result in delays or denials.
- Utilize the partnership with CoverMyMeds for a more efficient submission process. This service provides real-time determinations for prior authorization requests.
- Familiarize yourself with the required information, such as patient and provider details, medication specifics, and clinical data. Missing any required data can delay the process.
- Be mindful of the submission timeline. The form must be submitted during specified operational hours: Monday to Friday from 5 AM to 10 PM Pacific, and Saturday from 6 AM to 3 PM Pacific.
- For urgent situations, direct all inquiries to 1-800-711-4555. Non-urgent requests can be faxed to 1-844-403-1028.
Browse Other Templates
California Health Insurance Penalty Exemptions - This form helps ensure compliance with health insurance requirements.
Registered Retail Merchant Certificate - Assistance is available from DOR for businesses unfamiliar with requirements or processes related to the BT-1.