Fill Out Your Oregon 801 Form
The Oregon Workers' Compensation Claim Form 801 is an essential document that plays a pivotal role in the workers' compensation system in Oregon. Specifically designed to capture detailed information about workplace injuries or occupational diseases, the form must be completed by both employees and employers in a timely manner. Importantly, workers must file their claims within 90 days of the injury or within one year of discovering an occupational disease; failure to adhere to this deadline can lead to claim denial. For employers, there's a critical obligation to report any claims to their insurance company within five days of becoming aware of the incident. The form contains specific sections that require information regarding the worker's educational background, the nature and specifics of the injury, and prior injuries, along with detailed accident descriptions to aid in the claims process. There are also important guidelines for filling out the form, such as using a ballpoint pen for clarity and noting specific dates and details about the injury when it occurred. The significance of the 801 form extends beyond mere compliance; it is the worker’s gateway to receiving vital medical benefits and wage loss compensation, emphasizing the urgent need for accuracy and completeness in reporting claims. Additionally, workers are reminded of their rights and responsibilities, including the critical requirement to authorize the release of medical records to facilitate the claims process. Navigating the complexities of this form is not just a bureaucratic formality; it can greatly impact a worker's recovery and financial stability following an unexpected work-related incident.
Oregon 801 Example
OREGON
Workers' Compensation Division
Workers' Compensation Claim Form 801
Notice to worker: Failure to file a claim with your employer within 90 days of injury or within one year of learning you have
an occupational disease may result in claim denial. Please read about your rights and responsibilities on the back of this form. Notice to employer: Failure to report a claim to your insurance company within five days of knowledge of the claim may
result in untimely payment of
Guidelines for completing the 801
Use a ballpoint pen, press firmly, and write clearly, or use a typewriter. The numbered items
below correspond to those on the 801 and may help you complete the claim form.
Worker section
7.Enter the number of years of education you have completed (GED is 12.)
8.If you were hospitalized past midnight for treatment and lodging, check "Yes."
9.Provide the type of injury (example: cut leg, broken arm).
11. |
Identify the body part(s) injured (example: low back, leg - right, shoulder - left, etc.). |
13.Provide the actual date of accident, if an injury, or the date your condition first required medical attention,
if an occupational disease.
15.If "Yes," briefly describe the prior injury (example: car accident in 1995, work injury in 1996, etc.).
17.Describe the accident as completely as possible. This will help the insurance company handling your claim.
18.Read "Important information about your Social Security Number (SSN)," "Authorization to release medical
records," and "Caution against making false statements," on the back of the 801.
Employer section
20. A Business Identification Number (BIN) is assigned by the Oregon Department of Revenue and is printed on your Oregon Tax Coupons (OTCs).
22. FEIN is your Federal Employers Identification Number.
a client.
28.Examples: truck manufacturing, retail grocery, log hauling, etc.
29.Enter the payroll class code under which you report this worker's earnings to your workers' compensation insurer.
33.Report the earliest of the following:
•the date you first knew of a claim
•the date you first knew of an accident or disease that may result in a compensable injury that requires medical services or causes time loss, permanent disability, or death.
37.See
50.Examples: "Loading dock, north end" or "Client's office at 452 Monroe Street, Washington, D.C., 20210."
51.Examples: acetylene cutting torch, metal plate.
52.Example: "Cutting metal plate for flooring." (Indicate whether or not activity was part of normal job duties.)
53.Example: "Worker stepped back to inspect work and slipped on some scrap metal. As she fell, worker brushed against the hot metal."
56.Check "Yes" if the worker presented a Preferred Worker Eligibility Card to you at the time of hire or you received a "Notice of Premium Exemption" from the Workers' Compensation Division (and the injury occurred on or before the eligibility end date on the card or notice).
Si Ud. tiene preguntas relacionadas a este formulario, |
If you have questions about this form, call the |
comuníquese con la División de Compensación para |
Workers' Compensation Division, Benefits Section, |
Trabajadores, Sección de Beneficios, en Salem al número |
in Salem at (503) |
telefónico (503) |
or |
o (llamada gratis en Oregon) |
(800) |
|
801 |
|
WC 8468b |
OSHA Recordkeeping Guidelines
Recordable Cases
If you are subject to recordkeeping regulations, you are required to record information on OSHA Form 200 about: (1) every occupational fatality; (2) every nonfatal occupational illness; and (3) those nonfatal occupational injuries that involve one or more of the following: loss of consciousness, restriction of work or motion, transfer to another job, or medical treatment other than first aid (see guidelines below).
Nature of injury |
|
Medical treatment (recordable) |
First aid |
|
Cuts, lacerations, punctures, |
· |
Sutures (stitches) |
· Bandaging on any visit to doctor or nurse |
|
· Butterfly adhesive dressing(s) or steri strip(s) in |
· Application of antiseptic on first visit to |
|||
abrasions, splinters |
||||
|
lieu of sutures |
doctor or nurse |
||
|
· |
Treatment of infection |
· Application of ointments on first or |
|
|
· Application of antiseptic on second or |
subsequent visits to prevent drying or |
||
|
|
subsequent visit to a doctor or nurse |
cracking of skin |
|
|
· Removal of foreign bodies requiring skilled |
· Removal of foreign bodies from wound by |
||
|
|
services of physician due to depth of |
tweezers or other simple techniques |
|
|
|
embedment, size or shape of object(s), or |
· Removal of foreign bodies in the eye, not |
|
|
|
location of wound |
embedded, by irrigation |
|
|
· Removal of foreign bodies embedded in eye |
|
||
|
· Cutting away dead skin (surgical debridement) |
|
||
Fractures |
· Where |
· When |
||
· |
Application of a cast or other professional |
|||
negative for fracture |
||||
|
|
means of immobilizing the injured part is |
||
|
|
|
||
|
|
required |
|
|
Strains, sprains, dislocations |
· Application of a cast or other professional |
· Use of an elastic (Ace) bandage on a strain |
||
|
means of immobilizing injured part |
that is not otherwise recordable, on a first |
||
Any strain, sprain, or dislocation is recordable if |
|
|||
· |
Use of hot or cold compresses for treatment of |
visit to a doctor or nurse |
||
the worker's range of motion is affected in a |
|
strains, sprains, and dislocation on second or |
· Use of hot or cold compresses for |
|
manner that prevents the worker from doing |
|
subsequent visits to a doctor or nurse |
treatment of a strain on first visit to a |
|
regularly assigned duties, whether or not |
· |
Use of diathermy and whirlpool treatments on |
doctor or nurse |
|
medical treatment is rendered. |
|
second or subsequent visits to a doctor or nurse |
· Use of diathermy and whirlpool treatments |
|
|
· A series of chiropractic treatments |
on first visit to doctor or nurse |
||
|
|
|
· A single chiropractic treatment for minor |
|
|
|
|
injury or discomfort |
|
Thermal or chemical burns |
· Treatment of all second- and |
· Treatment by a doctor or nurse for a first- |
||
|
|
degree burn |
||
Any burn is recordable if the worker's range of |
|
|
||
|
|
|
||
motion is affected in a manner which prevents |
|
|
|
|
the worker from doing his or her regularly |
|
|
|
|
assigned duties, whether or not medical |
|
|
|
|
treatment is rendered. |
|
|
|
|
Bruises, contusions |
· Treatment of a bruise by draining collected |
· Soaking or application of cold compresses |
||
|
blood |
to a bruise, that is otherwise not |
||
Any bruise or contusion is recordable if the |
|
|||
· |
Soaking or application of cold compresses to a |
recordable, on first visit to a doctor or |
||
worker's range of motion is affected in a |
|
bruise on second or subsequent visits to a |
nurse |
|
manner that prevents the worker from doing |
|
doctor or nurse |
|
|
regularly assigned duties, whether or not |
|
|
|
|
medical treatment is rendered. |
|
|
|
|
Miscellaneous procedures |
|
|
|
|
Medical treatment is only one criteria for determining recordability. Any injury that required only
• Tetanus shots, either initial shots or boosters, are considered• All diagnosed occupational illnessesare recordable. preventive in nature and are not considered medical treatment.
• |
Hospitalization for observation, where no treatment is rendered other |
• |
All occupational fatalities are recordable. |
|
|
||
|
than first aid, is not considered medical treatment. However, most |
• |
A heart attack, if determined to be |
|
injuries requiring hospitalization will result in lost workdays and will be |
||
|
|
illness |
|
|
recordable for that reason. |
|
|
|
|
(col 7g and col 8 of log). |
|
|
|
|
|
• |
The observation of injuryby a doctor or nurse is not recordable. |
• |
Replacement of broken eyeglasses in itself is not recordable. |
|
|
•Giving worker prescriptions for drugs on second or subsequent visits constitutes medical treatment. Use of prescription medication, when a single dose is administered on the first visit for minor injury or discomfort, is not recordable. Recommending or giving nonprescription medicines is considered first aid.
OSHA recordkeeping questions may be referred to:
Department of Consumer & Business Services,
Information Management Division
350 Winter St. NE, Salem, OR
Phone: (503)
State of Oregon |
|
|
|
|
|
|
|
|
|
|
|
|
FEIN of claim administrator: |
|
||
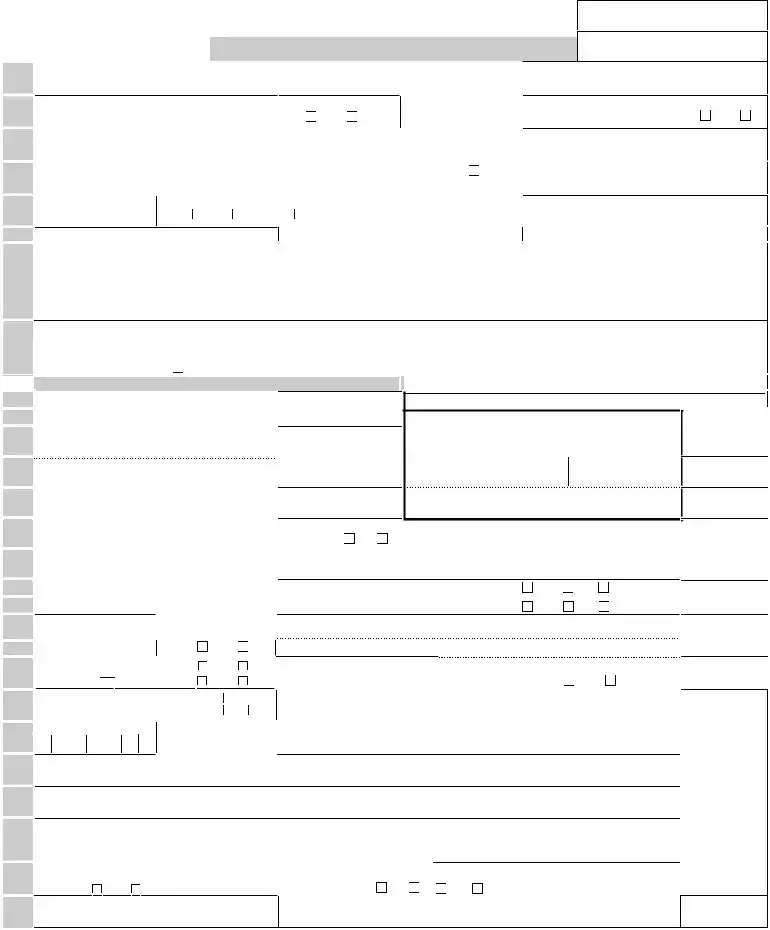
Workers' and Employer's |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Report of Occupational |
|
Complete all items — Failure to do so may delay beneftis |
Insurer claim number: |
|
|
|||||||||||
Injury or Disease |
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
back. |
1. Worker's legal name (first, m.i., last): |
|
2. |
Home phone: |
3. |
Date of birth: |
4. |
Social Security number (see back of form): |
|
|||||||
5. Worker's street, mailing, and |
|
6. |
Male |
Female |
7. |
Education - |
grade |
8. |
Hospitalized overnight as inpatient? |
|
||||||
|
|
|
||||||||||||||
on |
address: |
|
|
|
|
|
|
|
completed: (0 – 20) |
(If emergency room - only, mark "No") |
Yes |
No |
||||
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
9. |
Nature of injury/disease |
|
|
10. Name and city of hospital: |
|
|
|||||
information |
|
|
|
|
|
(strain, cut, bruise, etc.): |
|
|
||||||||
13. Date of injury/disease: |
14. Time of injury: |
|
15. Has body part been injured before? |
(If yes, explain) |
16. Full name, address, and phone of attending |
|
||||||||||
|
City |
|
State |
ZIP |
|
11. Body part(s) affected: |
|
|
Left |
12. Name and address of health insurance |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
Right |
provider: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
See |
|
|
: |
a.m. |
p.m. |
|
Yes |
No |
|
|
|
physician: |
|
|
|
|
17. Describe accident fully (please print): |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
WORKER |
Witness(es): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18. By my signature I am giving NOTICE OF CLAIM and authorizing medical providers and other custodians of claim records to release relevant |
|||||||||||||||
|
medical records. I certify that the above information is true to the best of my knowledge and belief (see paragraphs 3 and 4 on the back). By my |
|||||||||||||||
|
signature, I also authorize the use of my SSN as described in paragraph 2 on the back. (If you do not authorize the use of your SSN as described |
|||||||||||||||
|
in paragraph 2, check here |
.) |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Worker: Sign and give form to your employer for completion |
X |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EMPLOYER |
19. Employer's legal business name: |
|
20. Employer BIN: |
|
Worker signature |
|
|
|
Date |
|
||||||
|
|
|
|
|
|
|
|
Employer: Complete items |
Dept. use |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21. Employer's street and |
|
22. Employer FEIN: |
24. Client's legal business name: |
|
25. Client BIN: |
Emp no |
|
||||||||
|
|
|
|
|
||||||||||||
|
City |
State |
ZIP |
|
23. Insurer Policy #: |
26. Client's street and |
|
|
27. Client FEIN: |
Ins no |
|
|||||
|
|
|
|
|
|
|
|
|
address: |
|
|
|
|
|
|
|
|
28. Nature of business: |
|
|
|
29. Worker class code: |
City |
State |
|
ZIP |
Occ |
|
|||||
requirements. |
30. |
Worker's occupation (do not abbreviate): |
|
31. Is worker owner or |
32. |
Address of injury site if different from 21 or 26: |
|
Nature |
||||||||||
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
corp. officer? Yes No |
|
|
|
|
|
|
||
|
33. |
Date employer first knew of claim: |
|
34. |
If fatal, date of death |
City |
|
State |
ZIP |
|
|
Part |
||||||
|
35. |
Date of hire: |
|
36. State of hire: |
|
37. |
Injured on employer's or client's premises? |
|
Yes |
No |
Unknown |
Event |
||||||
recordkeeping |
|
|
|
|
|
|
|
|
|
38. |
Did injury occur during course of job? |
|
Yes |
No |
Unknown |
|
||
39. |
Date left work: |
40. |
Time left work: |
|
41 |
Date returned to regular work: |
|
|
|
|
Source |
|||||||
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
: |
|
a.m. |
p.m. |
42. |
Date returned to work with restrictions/light duty: |
|
|
|
|
||||
|
43. |
Working |
> |
from |
: |
|
a.m. |
p.m. |
44. No. of hours worked per |
45. If returned to work with restrictions, |
|
Assoc |
||||||
|
|
shift: |
to |
: |
|
a.m. |
p.m. |
shift: |
|
were full wages paid? |
Yes |
No |
object |
|||||
101 |
46. |
Wage and wage period: |
Hr. |
Day |
|
47. |
If wage varies or includes other earnings |
(tips, room and board, commission, etc.) give |
Insurer use |
|||||||||
|
$ |
|
|
per |
Wk. |
Mo. |
Yr. total weekly wage and explain |
: (Attach payroll records for last 52 weeks prior to date of injury) |
|
|||||||||
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
||||
Form |
48. Scheduled days off: |
49. |
No. of days |
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
worked per week: |
|
|
|
|
|
|
|
|
|
|
||
|
S |
S M T W T F |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
OSHA |
50. |
Department and location where event |
|
51. |
All equip., materials, or chemicals employee was using when event |
|
|
|||||||||||
occurred: |
|
|
|
|
|
|
|
occurred: |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
satisfies |
52. |
Specific activity the employee was engaged in when event occurred. |
(Indicate if activity was part of normal job duties): |
|
|
|||||||||||||
53. |
How injury or illness occurred; describe the sequence of events and include any objects or substances that directly injured the employee or |
|
||||||||||||||||
|
|
|||||||||||||||||
|
|
made the employee ill: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
form |
54. Was accident caused by person |
(other than |
55. Were other workers injur- |
|
56. Is worker "premium exempt" |
(a Preferred Worker)? |
||||
injured worker) or by failure of machinery or |
|
|||||||||
ed in the accident? |
Yes |
No |
|
|
|
|||||
product? |
Yes |
No |
|
Yes |
No (If "Yes," attach copy of eligibility card.) |
|||||
This |
57. Signature of employer representative: |
58. Print name, title and phone: |
|
|
59. Date: |
|||||
X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Attention: Fatalities must be reported to
local field office. Report fatalities or accidents by calling (503)
Original and copy to insurer within 5 days of notice of claim; |
copy to worker immediately as receipt of claim; copy to employer's file. |
WC 8468b
Notice to Worker
Important information about your Social Security Number (SSN)
1.You must provide your SSN. The Workers' Compensation Division (WCD) of the Department of Consumer and Business Services (DCBS) has authority to request your SSN under the Privacy Act of 1974, 5 USC & 552a (West 1977), Section 7(a)(2)(B). Authority under state law is provided in Oregon Revised Statute 656.265, and under Administrative Order WCB
2.Your voluntary authorization for the use of your SSN is also requested for use by various government agencies to carry out their statutory duties, including, but not limited to, planning, research, child support enforcement, employment assistance, benefit coordi- nation, child labor law enforcement, risk management, hazard identification, rate setting, and training programs. If you do not authorize this use, please check the box by your signature in Section 18 on the front of this form.
Authorization to release medical records
3.By signing this 801, you are giving "Notice of Claim" and authorizing medical providers and other custodians of claim record to release records related to the injury or disease claimed on this 801 under ORS Chapter 656 and OAR Chapter 436. Medical information relevant to the claim includes past history of the complaints or treatment of a condition similar to that presented in the claim or other conditions related to the same body part.
Caution against making false statements
4.Any person who knowingly makes any false statement or representation for the purpose of obtaining any benefit or payment is punishable, upon conviction, by imprisonment for a term of not more than one year, a fine of not more than $1,000, or both, under ORS 656.990(1).
This is your receipt, when signed by your employer, that you gave notice of a claim. Keep it as your record.
5.Your employer will submit the claim for you. You will receive written notice from your employer's insurer of any action taken on
your claim. If your employer is
Medical care
6.If your claim is accepted, the insurer or
You must tell your doctor or hospital on your first visit that your injury or illness is work related. The doctor must tell you if there are any limits to the medical services he or she may provide you under the Oregon workers' compensation system.
If you are enrolled in a managed care organization (MCO), your attending physician may be any medical service provider authorized by contract with the MCO. An MCO contracts with insurance companies to provide managed medical care to injured workers of employers covered by the insurance company. Check with the MCO to find out who can be your attending physician. If you are not enrolled in an MCO, your attending physician must be one of the following:
•A licensed medical doctor, a licensed doctor of osteopathy, or a licensed oral and maxillofacial surgeon
•A licensed chiropractor (only for 30 days from the date of the first chiropractic visit on the initial claim or for 12 chiropractic visits during the
Payments for time lost from work
7.In order for you to receive payments for time lost from work, your attending physician must notify the insurer or
If you are disabled for more than three calendar days, the insurer or
If you have questions about your claim that are not resolved by your employer or insurer, you may contact:
Workers' Compensation Division |
OR |
350 Winter Street NE, Room 27, Salem, OR
or
Ombudsman for Injured Workers
350 Winter Street NE, Salem, OR
(503)
UNIFORM INFORMATION SERVICES, INC. WC 8468b |

OREGON
Understanding workers' compensation claims
A guide for workers recently hurt on the job
Workers' Compensation Division
You have received this information because you are filing a workers' compensation injury claim (Form 801) with your employer. If you have additional questions, please do one or more of the following:
Contact your employer's workers' compensation insurer to find out what decisions have been made about your claim and what you need to do to get benefits.
Call the Ombudsman for Injured Workers for help understanding your rights and responsibilities, (503)
Call the Workers' Compensation Division (WCD) for general information about benefits,
(503)
Contact the insurer or the Workers' Compensation Division at the phone number above and ask for the brochure "What happens if I'm hurt on the job?." The insurer will send this automatically if you are disabled by your injury.
What do I do now?
Tell your doctor that you were hurt on the job. Your doctor will ask you to fill out a Form 827 - "First report of injury/disease." Your doctor will send the Form 827 to the insurer for you.
May I get treatment from any doctor?
Unless the insurer has enrolled you in a managed care organization (MCO), you may treat with any doctor who qualifies as an attending physician under Oregon law. Your doctor will tell you if there are any limits to the services he or she can provide.
What are my doctor's responsibilities?
Your doctor is in charge of your medical treatment. Only your doctor can authorize time off work, reduce work hours or duties, or release you to go back to work.
Will my employer's insurer pay my medical bills?
If your claim is accepted, the insurer will pay injury- related medical bills. Save your receipts for pre- scription medications, transportation, and other bills you pay for
If I can't work, will I receive payments from the insurer for lost wages?
Yes, if your doctor notifies the insurer that you cannot work or cannot do your regular work due to your injuries, you will receive temporary disability payments. However, Oregon law requires a
What can I do to make sure I receive benefits to which I am entitled?
•Find out the legal business name of your employer and the name of its workers' compensation insurer. If you have a problem getting this information, call the Workers' Compensation Division Employer Index, (503)
•Keep all medical appointments.
•Read and keep copies of all letters and forms you receive regarding your claim.
•Keep track of phone calls, including with whom you speak, subject matter, and dates.
•Observe all deadlines. Do not be late to submit information or to file appeals.
•Contact your employer immediately when your doctor releases you for work.
•Contact the insurer if you have questions.
WC 8468b
Form Characteristics
| Fact Name | Fact Description |
|---|---|
| Form Purpose | The Oregon 801 Form is used for reporting workers' compensation claims. |
| Governing Law | This form operates under Oregon Revised Statute (ORS) Chapter 656. |
| Claim Filing Deadline | Workers must file their claim within 90 days of injury or within one year of discovering an occupational disease. |
| Employer Responsibilities | Employers must report claims to their insurance company within five days to ensure timely payments. |
| Evidence Collection | Include all relevant details about the accident for better claim processing. |
| Use of SSN | Workers must provide their Social Security Number for claims processing and record-keeping. |
| Medical Treatment Coverage | If the claim is accepted, insurers cover medical expenses related to the injury. |
| Temporary Disability Payments | Payments for lost wages may start after a three-day waiting period, depending on medical notification. |
Guidelines on Utilizing Oregon 801
After collecting the necessary information about your injury, it's important to accurately complete the Oregon Form 801. This form will help set up your workers' compensation claim. Follow the steps below to ensure everything is filled out correctly.
- Start by using a ballpoint pen or a typewriter to fill out the form.
- In section 1, write your legal name, including your first name, middle initial, and last name.
- In section 2, enter your home phone number.
- For section 3, provide your date of birth.
- In section 4, include your Social Security number.
- Fill in your street and mailing address in section 5.
- For section 6, check either "Male" or "Female" as appropriate.
- Next, enter the number of years of your education in section 7 (consider GED as 12 years).
- If you were hospitalized overnight, mark "Yes" in section 8; otherwise, mark "No."
- In section 9, detail the nature of your injury, such as "cut" or "sprain."
- Identify the affected body parts in section 11, like "right leg" or "left shoulder."
- Provide the date of the accident or the first time you sought medical attention in section 13.
- If applicable, answer section 15 about any prior injuries and explain briefly.
- In section 17, describe the accident in complete detail to aid your claim.
- If you agree to have your medical records released, read the important information in section 18 and sign if you consent.
- Hand the completed form to your employer for the employer's section to be filled out.
It’s crucial to ensure all details are accurate and filled out completely to avoid delays. Once you submit the form to your employer, they will process it and send it to the workers' compensation insurer.
What You Should Know About This Form
What is Form 801 used for?
The Oregon Form 801 is a Workers’ Compensation Claim Form. It is required for reporting injuries or diseases that occur while performing work duties. This form meets record-keeping requirements set by OSHA and allows workers to notify their employer of an injury or occupational disease for potential benefits.
What happens if I don’t file my claim within the required timeframes?
If a worker fails to file a claim with their employer within 90 days of the injury or within one year of discovering an occupational disease, they risk having their claim denied. It is crucial to adhere to these timelines to ensure the eligibility for benefits.
What should I include when describing the accident on Form 801?
When describing the accident, provide detailed information about what happened. Include specifics such as the nature of the injury, the exact date the injury occurred, and a thorough account of the circumstances leading up to the incident. This information aids the insurance company in processing the claim efficiently.
What is the significance of the Social Security Number (SSN) on Form 801?
The Social Security Number is necessary for processing your claim. The Workers' Compensation Division is authorized to request your SSN under federal and state law. Your SSN helps with compliance, claims processing, and maintaining records. If you have concerns about its use, be sure to check the appropriate box on the form.
What medical treatments will be covered if my claim is accepted?
If your claim is approved, injury-related medical expenses will be covered. This includes costs for treatments, medications, transportation related to medical appointments, and other necessary expenses, provided you submit proper documentation and receipts. However, expenses will not be paid before claim acceptance.
Are there penalties if my employer fails to report my claim?
Yes, if an employer does not report a claim to their insurance company within five days of being informed of the claim, this may lead to delayed payments for time-loss benefits, and could result in penalties against the employer or their insurance company.
What information should I provide in the worker's section of Form 801?
In the worker's section, include your legal name, contact information, Social Security number, details about your injury, education completed, and any past injuries to the affected body part. Make sure to provide clear and accurate information as this will impact the processing of your claim.
How does the insurer determine wage loss benefits?
The insurer calculates wage loss benefits based on two-thirds of your gross weekly wage at the time of your injury, capped at a maximum equal to Oregon's average weekly wage. Specific rules apply for lower wages, ensuring you receive a minimum benefit if your earnings fall below a certain threshold.
Can I see any doctor for treatment of my injury?
Unless you are enrolled in a Managed Care Organization (MCO), you can select your own doctor, provided they meet the qualifications as an attending physician under Oregon law. Your healthcare provider will inform you about any limitations on services they can provide under the workers' compensation system.
What should I do if I have questions about my claim?
If you have questions regarding your claim that are not addressed by your employer or insurance insurer, you can contact the Workers' Compensation Division for assistance. You may also reach out to the Ombudsman for Injured Workers for help understanding your rights and responsibilities regarding your claim.
Common mistakes
Completing the Oregon Workers' Compensation Claim Form 801 can be a straightforward process, but mistakes can lead to delayed benefits or claim denials. One common mistake is failing to provide accurate personal information. This includes the worker's legal name, social security number, date of birth, and contact information. If any of this information is incorrect or incomplete, it could create barriers to processing the claim. Double-checking this section before submission is vital for ensuring that the claim is properly identified.
Another frequent error involves not detailing the nature of the injury or the incident leading to it. Not fully describing how the injury occurred can hinder the insurer's understanding and investigation of the claim. Use clear, simple language to outline the specific circumstances surrounding the accident. For instance, rather than just stating "cut," the description should include indicators like "while cutting metal, the worker inadvertently slipped and cut their arm." Such detailed accounts can significantly impact the evaluation of the claim.
A third mistake is neglecting to adhere to reporting timelines. The form requires that claims be filed within 90 days of the injury or within one year of discovering an occupational disease. Delaying the submission of the claim can lead to automatic denials, regardless of the validity of the injury. It is crucial to promptly initiate the process to avoid unnecessary setbacks.
Lastly, signatures and authorizations can be overlooked. The worker must sign the form to authorize the release of medical records and to affirm that all provided information is true. A missing signature can result in the cancellation of the claim processing. It's important to carefully review the entire form, ensuring all necessary signatories are in place before submission.
Documents used along the form
The Oregon 801 form is a vital component in the workers' compensation claim process. Alongside this form, various other documents are often required to ensure that claims are processed smoothly and completely. Below are four key documents that are commonly used with the Oregon 801 form.
- Workers' Compensation Claim Form 827: This form serves as the first report of injury or disease completed by the employee's healthcare provider. It is essential as it provides detailed medical information about the employee's condition, injury, or illness related to the workplace incident. Additionally, this form notifies the insurer of the need for treatment and plays a critical role in the initial claim submission.
- Transitional Duty Agreement: This document outlines temporary job duties that an injured worker can perform while recovering from their injury. It helps facilitate the worker's return to the workplace in a reduced capacity. Employers and employees typically customize this agreement to fit the individual's specific restrictions and the employer's needs.
- Third Party Liability Form: This form must be completed if the injury was caused by someone other than the employer. It allows the injured employee to pursue compensation from a third party—such as another driver in a vehicle accident—while still retaining their right to workers' compensation benefits. This form is crucial for ensuring that the claim is comprehensive and addresses all potential sources of compensation.
- Employment Verification Form: When claims are made, it is often necessary to verify the employee’s job status and income at the time of injury. This document helps establish the worker's wages, hours, and employment status, which are essential for calculating any benefits owed. Employers typically complete this form, ensuring accurate information is submitted to the insurer.
These documents, when combined with the Oregon 801 form, help create a comprehensive application for workers' compensation. Ensuring that all necessary paperwork is correctly completed and submitted can significantly impact the efficiency of the claims process and the delivery of benefits to the injured worker.
Similar forms
- OSHA Form 200: This form is used to record workplace injuries and illnesses. Like the Oregon Form 801, it requires details about the incident, helping employers maintain accurate records for health and safety compliance.
- Workers' Compensation Claim Form 827: Similar to Form 801, this document notifies the insurer of a work-related injury. It gathers essential details from the worker, like specifics of the injury and medical treatment, to initiate the claims process.
- Employer's Report of Occupational Injury or Disease: This form is completed by employers to inform the insurance company of an employee’s work-related injury. Like Form 801, it requires timely reporting to ensure benefits are processed efficiently.
- First Report of Injury (FROI): This report enables the documentation of an employee’s injury shortly after it occurs. Like Form 801, it is critical for initiating claims and gathering the necessary information to process benefits.
- Uniform Injury Report: This report serves as a standard document for reporting work injuries or conditions, similar to Form 801 in its purpose to ensure compliance with reporting requirements.
- Medical Authorization Form: This document allows healthcare providers to share injury-related information, paralleling Form 801’s requirement for consent to release medical records for the claims process.
- Notice of Denial of Claim: When a worker's claim is denied, this notice explains the reasons, similar to how Form 801 outlines the importance of proper filing for claim acceptance.
- Return to Work Form: After a worker is treated for an injury, this form confirms their ability to return. This is similar to the information required in Form 801 regarding the worker's condition and restrictions.
- Job Hazard Analysis (JHA): This tool outlines potential workplace hazards and safety measures. While not a claim form like 801, it aligns with Oregon’s commitment to worker safety, much like the reporting framework established in Form 801.
- Injury Tracking Log: This log is used by employers to monitor workplace injuries. It includes data similar to what is collected in Form 801, serving as a helpful tool for compliance and safety analysis.
Dos and Don'ts
- Do use a ballpoint pen to fill out the form and ensure your writing is clear.
- Do provide accurate information, particularly regarding dates, injuries, and prior medical conditions.
- Do submit the form within the required timeframe to avoid denial of your claim.
- Do sign the form to authorize the release of your medical records related to your claim.
- Don't leave any required fields blank; incomplete forms may delay processing.
- Don't make false statements or misrepresent information, as this can lead to legal consequences.
- Don't forget to check that the employer has completed their sections before submission.
- Don't rely solely on your employer to submit the claim; ensure you retain a copy for your records.
Misconceptions
- Misconception 1: The Oregon 801 form is only necessary for severe injuries.
- Misconception 2: Workers have unlimited time to file this form after an injury.
- Misconception 3: Employers handle the submission of the form without worker involvement.
- Misconception 4: The information provided in the form is not crucial for processing claims.
- Misconception 5: Filing an Oregon 801 form guarantees automatic acceptance of a claim.
This form is required for all workers' compensation claims, not limited to serious injuries. Even minor incidents can lead to compensation needs, so filing the 801 form is essential regardless of the injury's severity.
In reality, workers must submit the claim within 90 days of the injury or within one year if it's an occupational disease. Failing to do so might result in claim denial.
While employers are responsible for submitting the claim to the insurance company, workers must first complete their portion of the form accurately. The worker's signature is crucial to initiate the process.
Accurate and detailed responses are vital. The clarity of information regarding the injury, prior injuries, and accident descriptions influences the likelihood of the claim being accepted. Insurance companies rely on this information to make informed decisions.
Submitting the form does not guarantee acceptance. After submission, the insurer has 90 days to accept or deny the claim based on available evidence and regulations. Workers should remain proactive and follow up on their claims.
Key takeaways
Understanding the Oregon Workers' Compensation Claim Form 801 is essential for both workers and employers in the event of an injury or occupational disease. Here are key takeaways to keep in mind:
- Form 801 must be filed within 90 days of an injury or one year from learning about an occupational disease.
- Using a ballpoint pen or typewriter is recommended; clarity is crucial for processing.
- Provide comprehensive injury details, including the nature of the injury and body parts affected. This information aids in claim evaluation.
- For employers, failure to report claims within five days can delay worker benefits and result in penalties.
- If the injured worker cannot complete the form, the employer should still submit it on their behalf.
- Include a detailed description of the accident, as it will facilitate the claims process for the insurance company.
- Both parties should maintain records of all communications related to the claim for reference.
- Upon filing, workers will receive written notice of the claim's status from the insurer, which is essential for tracking benefit approvals.
Browse Other Templates
Superbill for Family Practice - The Superbill incorporates a variety of common procedures, allowing for versatile application across specialties.
Beneficiary Update Request,Beneficiary Designation Modification,Beneficiary Assignment Change,Beneficiary Information Update,Beneficiary Selection Form,Beneficiary Nomination Document,Beneficiary Revision Form,Beneficiary Declaration Form,Beneficiary - Retain a copy of your submitted beneficiary change form for future reference.