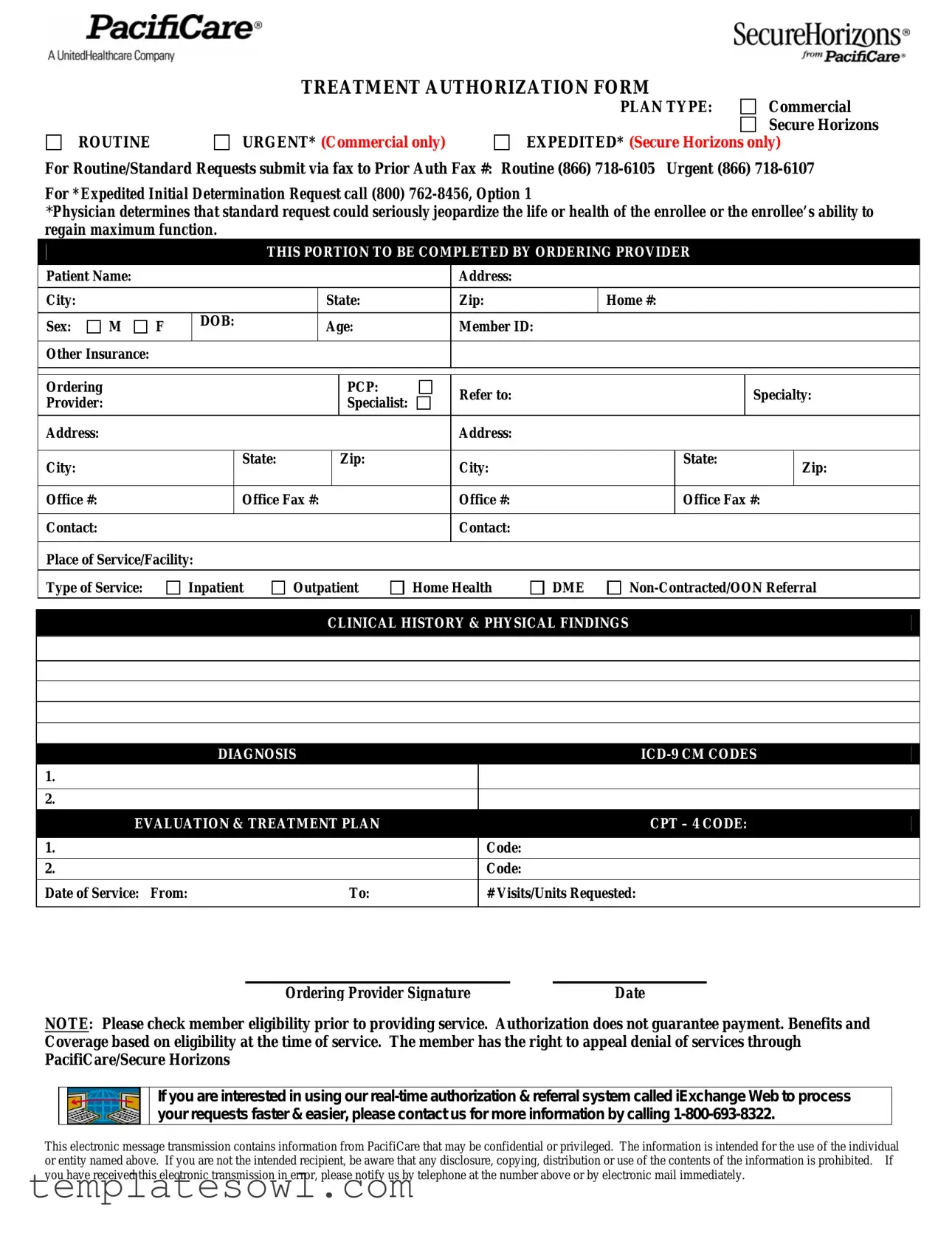
Fill Out Your Pacificare Form
The Pacificare Treatment Authorization Form serves as a vital tool for healthcare providers seeking approval for patient services under specific insurance plans, including Commercial and Secure Horizons. With designated sections for essential patient information, the form requires details such as the patient's name, address, date of birth, and member ID. Additionally, providers must specify the type of plan and treatment being requested, whether it be routine or urgent. The form also addresses the need for expedited authorization in cases where a standard request could jeopardize the patient's health. This streamlined process ensures efficient communication between healthcare providers and insurance companies, facilitating timely treatment for patients. Moreover, the form outlines the necessary clinical history, diagnoses, and treatment plans, alongside corresponding codes, making it easier to document and review requests. It’s important to highlight that while the form initiates the authorization process, it does not guarantee payment, emphasizing the need for providers to verify member eligibility before proceeding with services. Should a request be denied, members have the right to appeal through PacifiCare/Secure Horizons, reinforcing the importance of maintaining patient rights throughout the treatment process.
Pacificare Example
TREATMENT AUTHORIZATION FORM
ROUTINE
URGENT* (Commercial only)
PLAN TYPE: |
Commercial |
|
Secure Horizons |
EXPEDITED* (Secure Horizons only)
For Routine/Standard Requests submit via fax to Prior Auth Fax #: Routine (866)
For *Expedited Initial Determination Request call (800)
*Physician determines that standard request could seriously jeopardize the life or health of the enrollee or the enrollee’s ability to regain maximum function.
THIS PORTION TO BE COMPLETED BY ORDERING PROVIDER
|
Patient Name: |
|
|
|
|
|
|
|
|
|
Address: |
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
State: |
|
Zip: |
|
Home #: |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sex: |
M |
F |
|
DOB: |
|
Age: |
|
Member ID: |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other Insurance: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ordering |
|
|
|
|
|
|
|
|
PCP: |
|
Refer to: |
|
|
|
Specialty: |
||
|
Provider: |
|
|
|
|
|
|
|
|
Specialist: |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Address: |
|
|
|
|
|
|
|
|
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
State: |
|
|
|
Zip: |
|
City: |
|
|
State: |
Zip: |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Office #: |
|
|
|
|
Office Fax #: |
|
Office #: |
|
|
Office Fax #: |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Contact: |
|
|
|
|
|
|
|
|
|
|
Contact: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Place of Service/Facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Type of Service: |
|
Inpatient |
Outpatient |
Home Health |
DME |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
CLINICAL HISTORY & PHYSICAL FINDINGS |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
DIAGNOSIS |
|
|
|
|
|
||||||||
1. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EVALUATION & TREATMENT PLAN |
|
|
|
|
CPT – 4 CODE: |
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1. |
|
|
|
|
|
|
|
|
|
|
|
Code: |
|
|
|
|
|
|
2. |
|
|
|
|
|
|
|
|
|
|
|
Code: |
|
|
|
|
|
|
|
Date of Service: |
From: |
|
|
|
|
|
|
To: |
|
|
# Visits/Units Requested: |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Ordering Provider Signature |
|
Date |
NOTE: Please check member eligibility prior to providing service. Authorization does not guarantee payment. Benefits and Coverage based on eligibility at the time of service. The member has the right to appeal denial of services through PacifiCare/Secure Horizons
If you are interested in using our
This electronic message transmission contains information from PacifiCare that may be confidential or privileged. The information is intended for the use of the individual or entity named above. If you are not the intended recipient, be aware that any disclosure, copying, distribution or use of the contents of the information is prohibited. If you have received this electronic transmission in error, please notify us by telephone at the number above or by electronic mail immediately.
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | The Pacificare Treatment Authorization Form is used to request approval for various healthcare services and treatments, ensuring that providers can secure necessary authorizations for patient care. |
| Submission Methods | Routine requests can be submitted via fax, while urgent requests require a different fax number, and expedited requests must be initiated through a phone call. |
| Governing Laws | This form and its procedures are subject to state-specific healthcare regulations, including but not limited to the Affordable Care Act and state insurance laws. |
| Provider Responsibilities | Ordering providers must complete specific sections of the form, including patient information and treatment details, to ensure proper authorization processing. |
| Member Rights | Patients have the right to appeal any denial of services, ensuring their interests are represented in the authorization process. |
| Confidentiality Notice | The communication surrounding this form contains confidential information, emphasizing the importance of privacy when handling patient data. |
Guidelines on Utilizing Pacificare
Completing the Pacificare Treatment Authorization Form correctly is essential for timely processing of requests for medical services. Follow the steps below to ensure all required information is accurately filled out.
- Begin by selecting the type of plan. Choose either Commercial or Secure Horizons.
- Indicate the request type: Routine, Urgent, or Expedited.
- Prepare to submit the request. For Routine/Standard Requests, fax it to the appropriate number:
- Routine: (866) 718-6105
- Urgent: (866) 718-6107
- If submitting an Expedited Initial Determination Request, call (800) 762-8456 and choose Option 1.
- Fill out the patient information section. Include:
- Patient Name
- Address
- City
- State
- Zip Code
- Home Phone Number
- Sex (Male or Female)
- Date of Birth
- Age
- Member ID
- Other Insurance Information
- Complete the Ordering Provider section. Include:
- Ordering PCP
- Referring Provider
- Specialty
- Provider Address
- City
- State
- Zip Code
- Office Phone Number
- Office Fax Number
- Provide the contact person's name.
- Specify the place of service or facility, and the type of service requested.
- Document clinical history and physical findings, including the diagnosis and the appropriate ICD-9 CM codes.
- Outline the evaluation and treatment plan. Include:
- CPT Codes
- Start and End Dates of Service
- Number of Visits/Units Requested
- Sign and date the form in the appropriate section.
- Check member eligibility before proceeding with services. Remember, authorization does not guarantee payment.
What You Should Know About This Form
What is the purpose of the Pacificare Treatment Authorization Form?
The Pacificare Treatment Authorization Form is designed to facilitate the approval process for medical services that require pre-authorization. It helps ensure that the needed treatment aligns with the patient’s insurance plan and meets the necessary medical requirements. Both routine and urgent requests can be submitted using this form, streamlining patient care and provider communication.
How should I submit a routine authorization request?
For routine requests, you should fill out the Pacificare Treatment Authorization Form completely and submit it via fax to the appropriate Prior Auth Fax number. For commercial plans, use (866) 718-6105. Ensuring that all required fields are completed will help expedite the review process.
What should I do if my request is urgent?
If you have an urgent request, you must determine that a standard request could jeopardize the member's health or ability to function. In such cases, you can fax your completed form to (866) 718-6107 for urgent requests. Alternatively, you can reach out directly by calling (800) 762-8456, Option 1, for an expedited initial determination. This approach prioritizes immediate care needs.
What information is required to be filled out by the ordering provider?
The ordering provider needs to complete various fields on the form, including patient details, diagnosis, and treatment plans. Essential information includes the patient’s name, address, member ID, and contact information for the primary care provider and specialist. Additionally, the ordering provider must indicate the type of service, such as inpatient or outpatient, and provide the relevant diagnosis and CPT codes.
Does submitting the authorization guarantee payment for services?
Submitting the Treatment Authorization Form does not guarantee payment for services rendered. Payment is contingent on member eligibility and benefits at the time of service. It is advisable to check the member’s eligibility prior to providing any services to avoid any misunderstanding regarding coverage.
How can I appeal if a service is denied?
If a service is denied, the member has the right to appeal the decision through PacifiCare/Secure Horizons. It is important to follow the specific appeal process outlined in the denial notification. Be sure to gather all necessary documentation and submit your appeal within the specified timeframe to ensure it is considered.
Common mistakes
When completing the Pacificare form, individuals occasionally make several common mistakes that can lead to delays or complications in the authorization process. One frequent error is improperly filling out the section for patient information. Ensuring that every detail is correct, particularly the Patient Name, DOB (Date of Birth), and Member ID, is essential. Mistakes or omissions in these areas might cause confusion, resulting in a rejection of the request.
Another critical misstep is related to the diagnosis and treatment codes. The form requires both ICD-9 CM Codes and CPT-4 Codes. If these codes are inaccurately assigned, the services may not only be denied but could also delay care for the patient. It’s beneficial to double-check that the codes reflect the actual medical diagnosis and proposed treatment accurately.
Completing the section regarding the ordering provider can also be problematic. Many people overlook providing complete contact information, such as the Office Fax # and Contact person. Incomplete or incorrect details can hinder effective communication, which is important for timely approvals.
Lastly, miscalculating the # Visits/Units Requested could lead to issues. If this number doesn't align with clinical necessity or fails to reflect the treatment plan adequately, it may result in a denial of the request. Reviewing the treatment needs before submitting the form can ensure that this section accurately represents what is being sought, thus minimizing potential complications.
Documents used along the form
When working with the Pacificare Treatment Authorization Form, several other documents often accompany it to ensure a smooth processing experience. These forms help provide additional context and support for the authorization request, safeguarding both the patient and the healthcare provider. Here are a few key documents that you might encounter.
- Member Eligibility Verification Form: This document confirms the patient's eligibility for insurance coverage at the time of the service. It ensures that the patient is active in the plan and eligible for specific treatments or services.
- Clinical Summary Report: A clinical summary report details the patient’s medical history, diagnosis, and treatment plans. This report assists insurers in understanding the necessity of the requested services, ensuring a thorough review process.
- Referral Form: A referral form is used when a primary care physician directs a patient to a specialist. This form often includes information about the referral reason and the specialist's details, streamlining the process for authorization from the insurance provider.
- Appeal Request Form: In cases where authorization is denied, the appeal request form allows the provider to formally contest the denial. This document should include all relevant details and provide a compelling argument as to why the treatment is necessary.
Understanding these accompanying documents is crucial for a streamlined authorization process. Each plays a vital role in easing communication between healthcare providers and insurers, ultimately benefiting the patient. Properly preparing and submitting these forms can make a significant difference in timely access to necessary treatments.
Similar forms
- Treatment Authorization Request (TAR): Similar to the Pacificare form, a TAR documents requests for procedures or services that require prior approval from an insurance provider. It includes patient details, physician information, and descriptions of the requested services.
- Prior Authorization Form: This form is used to obtain approval before providing certain medical services. Like the Pacificare form, it collects information about the patient, diagnosis, treatment plan, and the health care providers involved.
- Referral Form: A referral form is needed when a primary care physician directs a patient to a specialist. It shares similarities with the Pacificare form by requiring patient information, provider details, and the reason for the referral.
- Informed Consent Form: Although primarily focused on patient understanding, an informed consent form contains details about procedures similar to those in the Pacificare form, including diagnosis and treatment methods, ensuring patients are aware of what to expect.
- Clinical Assessment Form: This document gathers clinical data regarding a patient’s condition. It parallels the Pacificare form in terms of collecting diagnosis and treatment plans, helping in requesting necessary authorizations.
- Insurance Verification Form: This form confirms a patient’s coverage status before services are rendered. Its purpose resembles the Pacificare form as both necessitate eligibility checks prior to treatment.
- Patient Medical History Form: This form collects comprehensive health information from patients. While its emphasis is different, both forms contain critical patient data that facilitates a proper assessment of care needs.
- Medicare Referral Form: Similar in structure, this form is specifically used for Medicare patients when referrals are needed for specialty care. It outlines pertinent information about the patient, the specialist, and the services requested.
- Authorization for Release of Medical Information: This form is used to obtain consent from patients to share their medical information with other healthcare providers. The consent process is vital, as having necessary information is crucial for effective treatment, akin to the details found in the Pacificare form.
- Case Management Referral Form: Used by case managers to document a patient’s specific needs, this form is similar because it gathers extensive information about the patient’s situation, ensuring that the appropriate care is coordinated.
Each of these documents shares a focus on patient care, requiring detailed information that health care providers need for effective treatment decisions and authorization requests.
Dos and Don'ts
When filling out the Pacificare form, here are four important actions to take and avoid. Follow these tips carefully to ensure a smooth process.
- Do double-check the patient's information. Ensure that the name, date of birth, and member ID are correct.
- Do provide complete details about the treatment plan. Include necessary ICD-9 codes and CPT codes.
- Do verify member eligibility before providing services. This can prevent issues with payment later.
- Do keep a copy of the completed form for your records. This can be useful for future reference.
- Don't leave any sections blank. Each part of the form needs to be filled out for processing.
- Don't assume that authorization guarantees payment. Always check the benefits and coverage at the time of service.
- Don't use incorrect or outdated codes. Using accurate ICD-9 and CPT codes is critical for approval.
- Don't forget to include your signature and the date. Missing this can delay the authorization process.
Misconceptions
Here are some common misconceptions about the Pacificare form, along with clarifications for each:
- Misconception 1: The Pacificare form is only for urgent cases.
- Misconception 2: Submitting the form guarantees payment for services.
- Misconception 3: Only primary care physicians can complete the form.
- Misconception 4: The patient doesn’t need to know about this form.
- Misconception 5: The form is only for inpatient services.
- Misconception 6: There are no specific instructions for urgent requests.
- Misconception 7: There’s no need to verify member eligibility.
- Misconception 8: The process is always slow and cumbersome.
This form can be used for both routine and urgent requests. Depending on the situation, proper documentation is necessary to determine the urgency.
Authorization from Pacificare does not guarantee payment. Coverage depends on the member's eligibility at the time services are provided.
The form should be completed by the ordering provider, which can include specialists and other healthcare providers.
Patients should be informed that the form is being submitted on their behalf. Communication ensures better understanding and coordination of care.
The Pacificare form accommodates various types of services, including outpatient, home health, and durable medical equipment (DME).
Urgent requests must be submitted via fax to the designated urgent line. An additional call may also be required for expedited requests.
It is crucial to check member eligibility prior to providing any services. This step helps avoid potential issues with coverage.
Using the iExchange Web system can streamline the authorization and referral process, making it faster and easier.
Key takeaways
Understanding how to effectively fill out and utilize the Pacificare form can streamline the authorization process for medical treatments. Here are eight essential takeaways:
- Plan Type Selection: Choose the correct plan type at the top of the form, as it affects how your request is processed.
- Urgent Requests: For urgent requests, ensure you submit them via fax using the number designated for urgent inquiries.
- Expedited Requests: If a request qualifies as expedited, call the appropriate number for immediate assistance rather than faxing it.
- Completing the Provider Information: Accurate completion of the ordering provider’s details is crucial for maintaining a clear line of communication.
- Member Eligibility: Always check the patient's eligibility before providing service. Authorization does not guarantee payment.
- Clinical History Sections: Provide detailed clinical history and diagnosis codes accurately as they inform the medical necessity of the request.
- Electronic System Access: Consider using the iExchange Web system for a streamlined authorization and referral process.
- Right to Appeal: Inform members that they have the right to appeal if their services are denied, ensuring they are aware of their options.
Browse Other Templates
Heroin - State how long you have been living together.
El Super Application - We look forward to the opportunity to learn more about you.