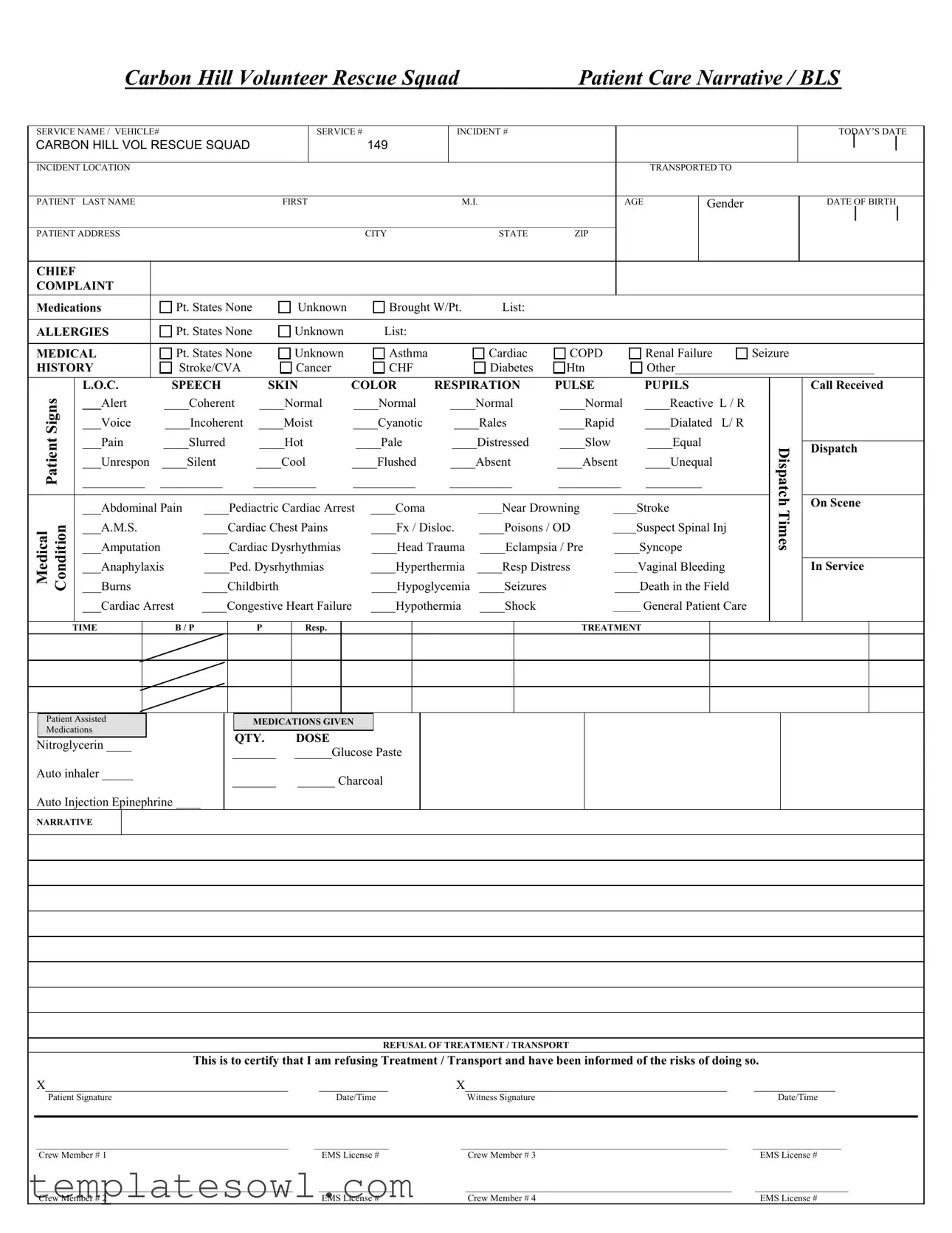
Fill Out Your Patient Care Report Form
The Patient Care Report (PCR) form is an essential document utilized by emergency medical services to document patient interactions and care provided during medical incidents. This form captures critical details such as the patient's personal information, including name, age, gender, and date of birth, which is vital for identifying the individual receiving care. The chief complaint section identifies the primary medical issue reported by the patient or observed by medical personnel. To ensure continuity of care, the form records relevant medical history, including allergies and pre-existing conditions, facilitating informed decision-making by healthcare providers. Additionally, it encompasses a comprehensive assessment of the patient's current condition, detailing vital signs, level of consciousness, and physical observations. Treatment administered, including medications given and interventions performed, is meticulously documented to maintain a clear record of the care provided. Furthermore, the PCR includes a section on refusal of treatment or transport, ensuring that patients have the opportunity to acknowledge their decisions regarding care. This report not only serves as a vital communication tool among medical teams but also provides legally binding documentation of the services rendered during emergency response situations.
Patient Care Report Example
|
|
|
Carbon Hill Volunteer Rescue Squad |
|
Patient Care Narrative / BLS |
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
SERVICE NAME / VEHICLE# |
|
|
|
SERVICE # |
|
INCIDENT # |
|
|
|
|
|
|
|
|
|
TODAY’S DATE |
||||||||
CARBON HILL VOL RESCUE SQUAD |
|
|
|
149 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INCIDENT LOCATION |
|
|
|
|
|
|
|
|
|
|
|
|
TRANSPORTED TO |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
PATIENT |
LAST NAME |
|
|
FIRST |
|
|
|
M.I. |
|
|
AGE |
|
Gender |
|
|
|
|
DATE OF BIRTH |
||||||
______________________________________________________________________________________________________________________________ |
|
|
|
|
|
|
|
|
|
|||||||||||||||
PATIENT ADDRESS |
|
|
|
|
|
CITY |
|
|
STATE |
ZIP |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CHIEF |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMPLAINT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Medications |
|
Pt. States None |
Unknown |
|
Brought W/Pt. |
List: |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
ALLERGIES |
|
Pt. States None |
Unknown |
|
List: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
MEDICAL |
|
Pt. States None |
Unknown |
|
Asthma |
|
|
Cardiac |
COPD |
|
|
Renal Failure |
Seizure |
|
|
|
||||||||
HISTORY |
|
Stroke/CVA |
Cancer |
|
CHF |
|
|
Diabetes |
Htn |
|
|
Other________________________________ |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
Signs |
|
L.O.C. |
SPEECH |
SKIN |
COLOR |
RESPIRATION |
PULSE |
|
|
PUPILS |
|
|
|
|
Call Received |
|||||||||
|
___Alert |
____Coherent |
____Normal |
____Normal |
|
____Normal |
____Normal |
____Reactive L / R |
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
___Voice |
____Incoherent |
____Moist |
____Cyanotic |
|
____Rales |
____Rapid |
____Dialated L/ R |
|
|
|
|
|
|
|||||||||
Patient |
|
___Pain |
____Slurred |
____Hot |
|
____Pale |
|
____Distressed |
____Slow |
|
|
____Equal |
|
|
Dispatch |
|
On Scene |
|||||||
|
|
|
|
|
|
|
|
|
|
Dispatch |
||||||||||||||
|
|
___Unrespon |
____Silent |
____Cool |
____Flushed |
|
____Absent |
____Absent |
____Unequal |
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
__________ __________ |
__________ |
__________ |
__________ |
__________ |
_________ |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
___Abdominal Pain |
____Pediactric Cardiac Arrest |
____Coma |
|
|
_____Near Drowning |
_____Stroke |
|
|
Times |
|
|
|
||||||||||
Medical Condition |
|
___A.M.S. |
|
____Cardiac Chest Pains |
|
____Fx / Disloc. |
____Poisons / OD |
_____Suspect Spinal Inj |
|
|
|
|
|
|||||||||||
|
___Burns |
|
____Childbirth |
|
____Hypoglycemia |
____Seizures |
|
____Death in the Field |
|
|
|
|
|
|||||||||||
|
|
___Amputation |
|
____Cardiac Dysrhythmias |
|
____Head Trauma |
____Eclampsia / Pre |
____Syncope |
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
___Anaphylaxis |
____Ped. Dysrhythmias |
|
____Hyperthermia |
____Resp Distress |
_____Vaginal Bleeding |
|
|
|
|
In Service |
||||||||||||
|
|
___Cardiac Arrest |
____Congestive Heart Failure |
____Hypothermia |
____Shock |
|
______ General Patient Care |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TIME
B / P
P
Resp.
TREATMENT
Patient Assisted
Medications
Nitroglycerin ____
Auto inhaler _____
Auto Injection Epinephrine ____
MEDICATIONS GIVEN
QTY. |
DOSE |
_______ |
______Glucose Paste |
_______ |
______ Charcoal |
NARRATIVE
REFUSAL OF TREATMENT / TRANSPORT
This is to certify that I am refusing Treatment / Transport and have been informed of the risks of doing so.
X_______________________________________ |
___________ |
X__________________________________________ |
_____________ |
Patient Signature |
Date/Time |
Witness Signature |
Date/Time |
|
|
|
|
______________________________________________________ |
________________ |
_________________________________________________________ |
___________________ |
Crew Member # 1 |
EMS License # |
Crew Member # 3 |
EMS License # |
_______________________________________________________ |
________________ |
_________________________________________________________ |
____________________ |
Crew Member # 2 |
EMS License # |
Crew Member # 4 |
EMS License # |
Form Characteristics
| Fact Title | Description |
|---|---|
| Form Purpose | The Patient Care Report (PCR) is essential for documenting patient information and the care provided during medical emergencies. It provides a comprehensive record of treatment and interactions with the patient. |
| Patient Information | The form collects various patient details, including name, age, gender, date of birth, and address. This information is critical for ensuring appropriate care and for future medical references. |
| Chief Complaint | Under the "Chief Complaint" section, the form records the patient's primary medical issue upon arrival. This can guide medical personnel in prioritizing treatment effectively. |
| Medication Documentation | The PCR includes sections for documenting medications administered and those brought by the patient. Accurate medication records are vital in preventing drug interactions or adverse effects. |
| Governing Law | In some states, forms like the PCR are mandated under specific health care regulations to ensure compliance and patient safety. For example, in California, the governing law includes the California Health and Safety Code, Section 1797.220, which outlines requirements for ambulance services. |
Guidelines on Utilizing Patient Care Report
Completing the Patient Care Report form is an essential step in documenting the care provided to patients during an emergency medical service incident. Properly filling out this form ensures that all relevant patient information is accurately recorded for future reference and helps maintain continuity of care.
- Start by indicating the service name at the top of the form. Write “Carbon Hill Volunteer Rescue Squad” in the designated space.
- Next, fill in the vehicle number, service number, and incident number in their respective boxes.
- Enter today’s date in the given space.
- Provide the incident location where the patient was found.
- Document where the patient was transported to.
- Write the patient’s last name, first name, and middle initial in the appropriate fields.
- Indicate the age and gender of the patient.
- Fill in the date of birth using the format specified on the form.
- Complete the patient’s address, including the city, state, and ZIP code.
- Identify the chief complaint using the options provided and provide additional context if necessary.
- Detail the patient’s medications and allergies as needed.
- Record the medical history by selecting from the listed conditions or writing in specifics if applicable.
- Assess the patient’s signs such as level of consciousness, speech, skin color, respiration, pulse, and pupils, marking each accordingly.
- Note the dispatch times for call received, on scene, and when dispatched.
- Document the patient’s general condition and specific medical conditions present, checking all that apply.
- Fill in the vital signs section, noting blood pressure, respiration, and temperature.
- Outline the treatment provided, indicating medications given and dosages.
- If applicable, the patient may refuse treatment or transport; ensure to document signatures and dates in this section.
- Finally, have all crew members sign and include their EMS license numbers in the provided spaces.
What You Should Know About This Form
What is the purpose of the Patient Care Report form?
The Patient Care Report (PCR) form is used to document the details of patient care during emergency medical services (EMS) responses. It serves several important functions. First, it captures patient information, medical history, and treatment provided. Second, it ensures that all relevant data is collected for continuous care and helps with legal documentation. Lastly, the PCR assists in quality assurance and helps improve future medical responses by providing a record for analysis and training.
Who is required to complete the Patient Care Report form?
All EMS personnel involved in the care of a patient must complete the PCR. This includes paramedics, EMTs, and any other crew members who delivered care or were part of the incident response. Each provider is responsible for accurately filling out their section and signing the report to confirm authenticity. This ensures accountability and provides a comprehensive history of the patient’s treatment.
What information should be included in the Patient Care Report?
The PCR must include detailed patient information such as name, age, gender, and address. It should outline the chief complaint and any relevant medical history, allergies, or medications. Vital signs, treatment administered, and the patient’s condition at various times during the incident must also be documented. Any refusals for treatment or transport must be clearly noted, alongside signatures from the patient and witness, if applicable.
How is the Patient Care Report used after an emergency call?
After an emergency call, the PCR is filed for record-keeping and can be reviewed by medical directors and quality assurance personnel. It is crucial for ongoing patient care, as it transfers vital medical information to hospitals or other facilities. Furthermore, the report may be used in compliance audits and to assist in training and improving EMS protocols. Secure storage and access to PCRs ensure that patient confidentiality is maintained while supporting continuous improvement in emergency care.
Common mistakes
Filling out the Patient Care Report form is essential for ensuring the best possible care for a patient. However, common mistakes can lead to complications in documentation. One major error often seen is incomplete patient information. Fields such as patient last name, first name, and date of birth should not be skipped. Missing these details can create confusion later, affecting continuity of care.
Another frequent mistake is not accurately documenting the chief complaint. This section is crucial as it guides the medical team in determining the necessary treatment. Failing to describe the patient's condition clearly or selecting "Unknown" without further details can hinder effective care. It's important to provide as much information as possible.
People also tend to overlook the medical history section. This part should contain significant past medical issues such as diabetes or asthma that could impact the current situation. Neglecting to list these can lead to inappropriate treatment decisions. Always double-check that this section is filled out completely.
In the section regarding vital signs, mistakes happen when measurements are either not taken or incorrectly recorded. For example, documenting a heart rate as "normal" when the patient is in distress can be misleading. Vital signs should reflect the most accurate readings to ensure proper assessment and response from the medical team.
Lastly, the narrative section often receives inadequate attention. This part allows crew members to explain the situation thoroughly. Vague or overly brief descriptions can leave out valuable context for subsequent medical teams. A clear, detailed narrative assists in understanding the patient’s experience and the pre-hospital care provided.
Documents used along the form
The Patient Care Report (PCR) form is crucial for documenting patient information and the care provided. However, several other forms and documents complement it to ensure comprehensive patient care and compliance with regulations. Below is a list of such documents.
- Run Sheet: This document outlines essential details about the emergency response call, including the time of dispatch, arrival, and transport. It serves as a timeline of events for the incident and helps in evaluating the efficiency of the response.
- Patient Release Form: Used when a patient refuses treatment or transport. This form confirms that the patient understands the risks associated with refusing care and provides legal protection for the emergency responders.
- Informed Consent Form: This document is signed by the patient or their representative, indicating that they understand the procedures and potential risks involved in their care. It ensures that consent is obtained before any treatment is administered.
- Medication Administration Record (MAR): This form is used to document any medications administered to the patient during the call. It includes details such as dosage, time given, and any reactions observed, which are critical for ongoing patient care.
These documents, when used alongside the Patient Care Report, help create a comprehensive view of the patient's situation and the care provided. Proper documentation supports quality care and accountability in emergency medical services.
Similar forms
- Emergency Medical Services (EMS) Report: Similar to the Patient Care Report, the EMS report documents patient care provided during transport. It includes information such as incident details, patient demographics, and treatment rendered. Both reports emphasize clear chronological documentation for continuity of care.
- Patient Transfer Document: This document is used when transferring a patient from one facility to another. Like the Patient Care Report, it provides detailed information about the patient's condition, treatment received, and any pertinent medical history to ensure safe and effective care during transfer.
- Medical History Form: This form gathers comprehensive medical history from patients. It shares similarities with the Patient Care Report in that it collects vital information on allergies, medications, and past medical conditions to inform healthcare providers about the patient's background.
- Consent for Treatment Form: Both the Patient Care Report and consent forms serve to document patient agreement to care, though the consent form explicitly addresses the patient's rights and the risks of treatments. They both aim to protect both patient and provider by ensuring informed consent.
- Discharge Summary: This document summarizes a patient’s care and treatment prior to discharge. It parallels the Patient Care Report in terms of documenting key medical events and interventions, ensuring that follow-up care is well-informed for continued recovery.
- Nursing Assessment Form: A nursing assessment form records a nurse’s assessment of a patient's condition and care needs. Like the Patient Care Report, it captures vital signs, physical exams, and subjective complaints, aiding in care planning.
- Incident Report: Used in both medical and non-medical contexts to record any unusual incidents. This report shares some elements with the Patient Care Report by detailing the circumstances of an incident and any actions taken, providing a comprehensive overview of what occurred.
- Medication Administration Record (MAR): This record tracks all medications administered to a patient. Similar to the Patient Care Report, it documents dosage, timing, and the route of administration, ensuring accuracy and accountability in patient care.
- Advance Directive Form: This document outlines a patient's preferences for medical treatment in situations where they cannot make their own decisions. While it serves a different purpose, it shares the goal of capturing vital patient information to guide healthcare decisions, much like the Patient Care Report.
- Emergency Contact Information Form: This form includes important contact information for family members or guardians in the event of an emergency. Like the Patient Care Report, it emphasizes the need for quick access to critical information to facilitate patient care during emergencies.
Dos and Don'ts
When filling out the Patient Care Report form, it's crucial to present information clearly and accurately. Here is a list of things you should and shouldn't do:
- Do write legibly and clearly, ensuring that anyone reading the report can understand your notes.
- Do include all relevant patient information, such as name, age, and medical history.
- Do document the exact times of significant events during the care provided.
- Do use objective language and avoid assumptions about the patient’s condition.
- Don't leave any sections blank. If information is unavailable, indicate it clearly (e.g., “unknown”).
- Don't alter or erase any information once it has been entered. Corrections should be made properly.
Misconceptions
There are several misconceptions about the Patient Care Report (PCR) form. Understanding these can help ensure that the documentation process is clear and effective.
- The PCR form is optional. Many believe that completing the PCR is not necessary. In reality, it is crucial for documenting patient care and ensuring compliance with regulations.
- Only doctors need to fill out the PCR form. Some think that only medical professionals should complete the form. However, it is the responsibility of all EMS personnel involved in patient care to document their actions.
- The PCR form is only for serious incidents. People might assume that the PCR is only needed for life-threatening situations. In fact, it should be completed for all patient interactions, regardless of severity.
- The PCR is the same as a hospital discharge report. There is a belief that these two forms serve the same purpose. They differ in function; the PCR is used for initial patient care documentation, while discharge reports are for hospital summaries.
- Corrections can be made freely. Some think they can easily change information on the PCR after it’s filled out. However, corrections must follow specific protocols to maintain accuracy and integrity.
- Completing the PCR does not involve patient consent. There may be a misconception that consent is not necessary for documentation. In truth, obtaining patient consent is an important ethical responsibility.
- The PCR form does not need to be shared with other healthcare providers. Some assume this documentation is only for EMS records. On the contrary, sharing the PCR with hospitals and other providers is essential for continual patient care.
- Handwritten notes are sufficient. People might think that scribbling down notes is enough. While notes are helpful, they should be formally documented on the PCR for clarity and consistency.
- The PCR form is merely a legal requirement. There is a common belief that the form only exists to meet legal standards. In reality, it is also a valuable tool for improving patient care and outcomes.
Key takeaways
When completing the Patient Care Report (PCR) form, attention to detail is crucial. Here are key takeaways to ensure that the report is filled out correctly and effectively utilized.
- Understand the Purpose: The Patient Care Report is a vital document that captures essential information about the patient's condition and the care provided during an emergency response.
- Accurate Patient Information: Always double-check to ensure the patient's name, age, gender, and other identifying information are correct.
- Chief Complaint: Clearly document the chief complaint using the patient's own words when possible. This helps to provide clarity on the reason for the visit.
- Medical History: Be thorough when recording the patient's medical history. Include relevant conditions, medications, and allergies that may affect treatment.
- Vital Signs: Record all vital signs, including blood pressure, pulse, respiration rate, and temperature. These metrics are critical for ongoing care decisions.
- Treatment Documentation: Clearly describe any treatments administered, including medications, dosages, and patient responses. This information is vital for continuity of care.
- Refusal of Treatment: If a patient refuses treatment or transport, document this carefully. Include signatures from both the patient and a witness to confirm understanding of the risks.
- Brief But Detailed Narrative: The narrative section should summarize the events and interventions that took place. Use clear, concise language to convey key points without unnecessary detail.
Filing out the PCR form correctly not only ensures accuracy in patient records but also enhances communication among healthcare providers during patient transfers and follow-ups.
Browse Other Templates
Owcp-1168 - Electronic submission is encouraged to expedite the enrollment process.
Dr 0024 - For any clarifications, refer to the accompanying instructions for guidance on the form.
Vehicle Condition Assessment Form,Transport Evaluation Sheet,Auto Transport Inspection Report,Vehicle Condition Report,Transportation Inspection Document,Car Transport Assessment Sheet,Pre-Transport Vehicle Checklist,Transport Vehicle Evaluation Form - Clarifies vehicle delivery timelines and expectations.