Fill Out Your Perinatal Sbar Form
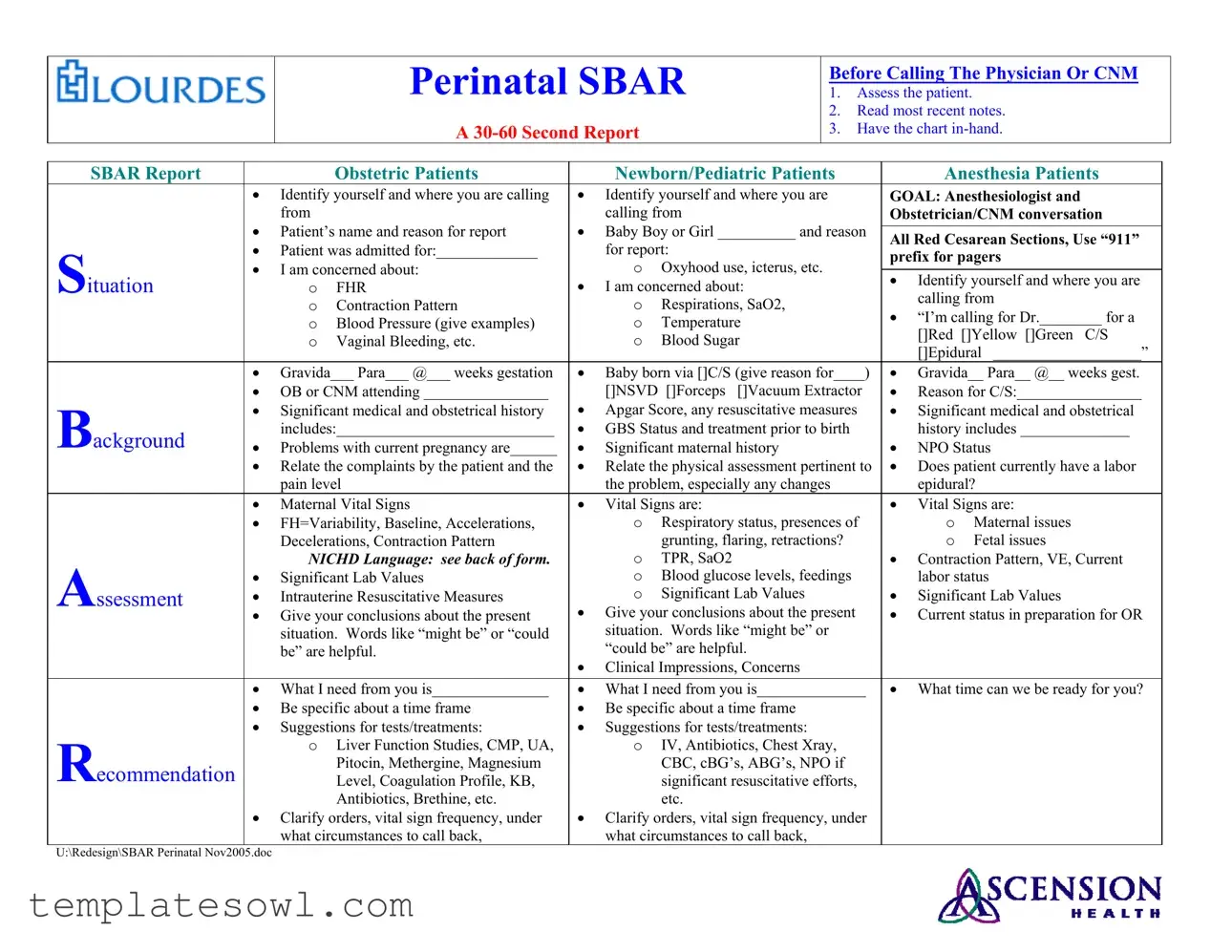
The Perinatal SBAR form plays a crucial role in the healthcare communication process, particularly in maternal and neonatal care. Designed to streamline conversations between healthcare providers, it ensures that essential information is relayed swiftly and accurately, which can be vital in urgent situations. This structured communication tool consists of four key sections: Situation, Background, Assessment, and Recommendation, each aimed at enhancing understanding and facilitating better decision-making. Before contacting a physician or Certified Nurse Midwife (CNM), caregivers must thoroughly assess the patient, review the latest medical notes, and prepare to deliver a concise 30- to 60-second report. This report begins with a clear identification of oneself and the location, immediately followed by crucial details about the patient and their current condition. Whether dealing with obstetric patients, newborns, or pediatric cases, the SBAR form prompts the caregiver to highlight pertinent issues like vital signs, contraction patterns, or any emerging concerns. The clarity provided by this structured approach helps to mitigate the risk of miscommunication, allowing for timely interventions and better patient outcomes. In addition to presenting vital information, the form encourages providers to communicate their needs and expectations directly, fostering collaboration and accountability throughout the care process.
Perinatal Sbar Example
|
|
|
Perinatal SBAR |
|
Before Calling The Physician Or CNM |
|||||||
|
|
|
|
1. Assess the patient. |
|
|
||||||
|
|
|
|
|
|
|
|
2. Read most recent notes. |
||||
|
|
|
A |
|
|
3. Have the chart |
||||||
|
|
|
|
|
|
|
|
|
||||
SBAR Report |
|
|
Obstetric Patients |
|
Newborn/Pediatric Patients |
|
Anesthesia Patients |
|
||||
|
• |
Identify yourself and where you are calling |
• |
Identify yourself and where you are |
GOAL: Anesthesiologist and |
|
||||||
|
• |
from |
|
• |
calling from |
|
|
Obstetrician/CNM conversation |
|
|||
|
Patient’s name and reason for report |
Baby Boy or Girl __________ and reason |
|
|
|
|
||||||
|
All Red Cesarean Sections, Use “911” |
|
||||||||||
|
• Patient was admitted for:_____________ |
|
for report: |
|
|
|
||||||
Situation |
|
|
|
prefix for pagers |
|
|||||||
• I am concerned about: |
|
O Oxyhood use, icterus, etc. |
|
|||||||||
|
|
|
|
|
||||||||
• |
• Identify yourself and where you are |
|
||||||||||
|
O |
FHR |
I am concerned about: |
|
||||||||
|
|
calling from |
|
|||||||||
|
|
|
|
|
|
|
||||||
|
|
O |
Contraction Pattern |
|
O |
Respirations, SaO2, |
• “I’m calling for Dr.________ for a |
|
||||
|
|
O Blood Pressure (give examples) |
|
O |
Temperature |
|
||||||
|
|
|
|
[]Red []Yellow []Green C/S |
|
|||||||
|
|
O |
Vaginal Bleeding, etc. |
|
O |
Blood Sugar |
|
|
||||
|
|
|
|
[]Epidural ___________________” |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
||
|
• |
Gravida___ Para___ @___ weeks gestation |
• |
Baby born via []C/S (give reason for____) |
• Gravida__ Para__ @__ weeks gest. |
|
||||||
|
• OB or CNM attending ________________ |
• |
[]NSVD []Forceps |
[]Vacuum Extractor |
• |
Reason for C/S:________________ |
|
|||||
Background |
• |
Significant medical and obstetrical history |
Apgar Score, any resuscitative measures |
• Significant medical and obstetrical |
|
|||||||
|
includes:____________________________ |
• |
GBS Status and treatment prior to birth |
|
history includes ______________ |
|
||||||
• |
Problems with current pregnancy are______ |
• |
Significant maternal history |
• |
NPO Status |
|
||||||
|
• |
Relate the complaints by the patient and the |
• |
Relate the physical assessment pertinent to |
• Does patient currently have a labor |
|
||||||
|
|
pain level |
|
the problem, especially any changes |
|
epidural? |
|
|||||
|
• |
Maternal Vital Signs |
• |
Vital Signs are: |
|
|
• |
Vital Signs are: |
|
|||
|
• |
FH=Variability, Baseline, Accelerations, |
|
O Respiratory status, presences of |
|
O |
Maternal issues |
|
||||
|
|
Decelerations, Contraction Pattern |
|
|
grunting, flaring, retractions? |
|
O |
Fetal issues |
|
|||
|
• |
NICHD Language: see back of form. |
|
O |
TPR, SaO2 |
|
|
• Contraction Pattern, VE, Current |
|
|||
Assessment |
Significant Lab Values |
|
O Blood glucose levels, feedings |
• |
labor status |
|
||||||
• |
Intrauterine Resuscitative Measures |
• |
O |
Significant Lab Values |
Significant Lab Values |
|
||||||
• |
Give your conclusions about the present |
Give your conclusions about the present |
• Current status in preparation for OR |
|
||||||||
|
|
|||||||||||
|
|
situation. Words like “might be” or “could |
|
situation. Words like “might be” or |
|
|
|
|
||||
|
|
be” are helpful. |
• |
“could be” are helpful. |
|
|
|
|
||||
|
|
|
|
Clinical Impressions, Concerns |
|
|
|
|
||||
|
|
|
|
|
|
|
||||||
|
• |
What I need from you is_______________ |
• |
What I need from you is______________ |
• What time can we be ready for you? |
|
||||||
|
• |
Be specific about a time frame |
• |
Be specific about a time frame |
|
|
|
|
||||
|
• |
Suggestions for tests/treatments: |
• |
Suggestions for tests/treatments: |
|
|
|
|
||||
Recommendation |
|
O Liver Function Studies, CMP, UA, |
|
O IV, Antibiotics, Chest Xray, |
|
|
|
|
||||
|
|
Pitocin, Methergine, Magnesium |
|
|
CBC, cBG’s, ABG’s, NPO if |
|
|
|
|
|||
|
|
Level, Coagulation Profile, KB, |
|
|
significant resuscitative efforts, |
|
|
|
|
|||
|
|
|
Antibiotics, Brethine, etc. |
|
|
etc. |
|
|
|
|
|
|
|
• |
Clarify orders, vital sign frequency, under |
• |
Clarify orders, vital sign frequency, under |
|
|
|
|
||||
|
|
what circumstances to call back, |
|
what circumstances to call back, |
|
|
|
|
||||
U:\Redesign\SBAR Perinatal Nov2005.doc
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Perinatal SBAR form is used to communicate critical patient information effectively before contacting healthcare providers. |
| Format | This form follows the SBAR (Situation, Background, Assessment, Recommendation) communication method to deliver concise reports. |
| Required Information | Essential patient data includes identification, patient history, vital signs, clinical impressions, and specific concerns. |
| State-Specific Laws | Depending on the state, healthcare providers must adhere to local regulations governing patient information sharing and reporting. |
| Goal Audience | The intended recipients of reports are obstetricians, Certified Nurse Midwives (CNM), and anesthesiologists who require timely updates. |
| Clear Communication | The form emphasizes clarity, urging users to avoid ambiguous language, especially when discussing patient conditions and needs. |
Guidelines on Utilizing Perinatal Sbar
Completing the Perinatal SBAR form is a crucial process that requires your attention to detail and clarity. This form helps facilitate effective communication regarding the patient's condition, issues, and required actions. The next steps will guide you through filling out the form thoroughly and accurately, ensuring that the necessary information is conveyed efficiently.
- Start by assessing the patient and gathering relevant information.
- Read the most recent notes related to the patient.
- Prepare for a concise report, ensuring you have the chart in-hand.
- Identify yourself and your location clearly at the beginning of the report.
- State the patient’s name and the reason for the report.
- Specify if the patient is being reported as OB, Newborn, Pediatric, or Anesthesia.
- Provide details regarding the patient's admission, significant medical history, and relevant obstetrical history.
- List any current concerns with the patient, such as vital signs, labor pain level, or any other pertinent symptoms.
- Summarize significant lab values related to the patient’s condition.
- Clearly state your clinical impressions, concerns, and what you need from the recipient of the report.
- Ask for a specific time frame for response or readiness.
- Make any suggestions for tests or treatments that may be necessary.
- Clarify any orders that need to be followed and the conditions under which to follow up.
What You Should Know About This Form
What is the purpose of the Perinatal SBAR form?
The Perinatal SBAR (Situation, Background, Assessment, Recommendation) form is designed to facilitate clear and concise communication among healthcare providers regarding obstetric patients, newborns, and pediatric patients. By organizing information into a structured format, it helps caregivers convey critical updates to physicians or certified nurse midwives efficiently, ensuring that everyone involved is on the same page regarding a patient's condition and needs.
When should the Perinatal SBAR form be used?
This form should be utilized before calling a physician or certified nurse midwife. It serves as a preparation tool to guide healthcare professionals in reporting significant details about their patients. Whenever there are changes in a patient's status or concerning observations, the SBAR format helps ensure that important information is communicated swiftly and accurately.
What key components are included in the SBAR format?
The SBAR format comprises four main sections: Situation, Background, Assessment, and Recommendation. The Situation outlines the patient's current condition or reason for the call. Background provides relevant medical history and information that led to the current situation. Assessment presents the healthcare provider's evaluation, including vital signs and observations. Finally, the Recommendation section suggests what actions should be taken and any pertinent follow-up required.
How does the SBAR format improve communication in a stressful setting?
In high-pressure situations, clear communication is crucial. The SBAR format encourages a systematic approach to conveying information, reducing the likelihood of misunderstandings. Its structured layout allows healthcare providers to communicate efficiently, ensuring essential details are relayed without unnecessary chaos or confusion. This enhances patient safety and promotes timely interventions.
What type of patients does the Perinatal SBAR cover?
The Perinatal SBAR form is comprehensive and can be used for various patients, including obstetric patients, newborns, and pediatric patients. By addressing the unique needs and conditions of these distinct groups, the SBAR format promotes tailored communication specific to each patient's situation, ultimately ensuring better care and outcomes.
How can the use of the Perinatal SBAR form lead to better outcomes for patients?
Utilizing the Perinatal SBAR form can lead to improved patient outcomes by fostering effective communication among healthcare providers. When crucial information is shared promptly and accurately, it allows for quicker interventions and appropriate decision-making. This streamlining of communication not only enhances patient safety but also supports a collaborative healthcare environment where all team members are informed, aligned, and ready to provide the best care possible.
Common mistakes
Filling out the Perinatal SBAR form correctly is crucial for ensuring effective communication among healthcare providers. However, several common mistakes often occur during this process. Addressing these errors can significantly improve patient care.
One frequent mistake is failing to review the most recent notes before making a report. Without this context, important information about the patient’s condition may be missed. This oversight can lead to miscommunication and could compromise patient safety. Always check the latest notes to provide a comprehensive and accurate situation assessment.
Another error involves inadequate identification of the patient and the reporter. When calling, it’s vital to clearly state your name, role, and location. Omitting these details can confuse the receiving physician or nurse-midwife about who is providing information and the context of the call. Clear identification fosters trust and ensures that there's no misunderstanding about the source of the information being relayed.
In addition, many individuals neglect to include essential vital sign data in their report. The absence of critical metrics such as blood pressure, contraction patterns, or fetal heart rate can hinder the receiving provider’s understanding of the patient’s current status. Comprehensive data enhances decision-making and facilitates timely interventions. Always verify that all necessary vital signs are included.
Finally, some people may express their concerns using vague language such as “might be” or “could be.” While it’s important to be cautious, these phrases can introduce uncertainty. Clear, decisive language helps convey urgency and seriousness. Make specific requests, articulating exactly what is needed from the physician, to ensure effective communication and prompt action.
Documents used along the form
The Perinatal SBAR form is a crucial tool in the healthcare setting, especially for those working with pregnant patients and newborns. However, it often works alongside several other forms and documents that provide key information and help ensure quality care. Below is a list of documents that complement the Perinatal SBAR form, each with a brief description.
- Patient Admission Form: This document captures essential details about the patient upon entering the healthcare facility, including medical history, allergies, and contact information.
- Vital Signs Record: A continuous log of a patient's vital signs—such as heart rate, blood pressure, and temperature—that aids in monitoring changes throughout their care.
- Labor and Delivery Record: This comprehensive chart details the patient’s labor progress, including contractions and interventions, providing a complete account of the delivery.
- Neonatal Assessment Form: Used to evaluate a newborn’s health immediately after birth, it includes aspects like Apgar scores, physical assessment results, and feeding needs.
- Medication Administration Record: A critical document that tracks medications given to the patient, including dosages and times, helping to prevent errors and ensure proper treatment.
- Consent Forms: These forms ensure that patients understand and agree to various treatments and procedures, thereby protecting their rights and allowing them to make informed choices.
- Transfer Forms: When a patient needs to be moved within the hospital or to another facility, these forms provide essential information about the patient's status and care needs.
- Postpartum Assessment Form: This document tracks the health and recovery of the patient after delivery, including monitoring for complications and ensuring proper postpartum care.
- Patient Discharge Summary: At the conclusion of care, this summary provides a comprehensive review of the patient's condition upon discharge, follow-up plans, and any new prescriptions.
Using these forms in conjunction with the Perinatal SBAR can greatly enhance communication and care coordination, ultimately leading to better outcomes for both mothers and their newborns. These documents serve as the backbone of patient care, ensuring all relevant information is shared and understood among the healthcare team.
Similar forms
- SBAR Communication Tool: The SBAR (Situation, Background, Assessment, Recommendation) communication tool is a widely adopted system in healthcare settings. Like the Perinatal SBAR form, it provides a structured method for relaying important information. Each section serves to clarify the situation at hand, background context, assessments made, and recommendations for next steps.
- Patient Handoff Report: A patient handoff report is similar in that it facilitates communication between healthcare providers during transition of care. Both documents emphasize critical information transfer, ensuring continuity of care while detailing patient status, concerns, and necessary interventions.
- Clinical Assessment Form: A clinical assessment form gathers patient data to evaluate health status. This document mirrors the Perinatal SBAR form in that both emphasize the importance of thorough patient assessment and documentation of vital signs, medical history, and presenting problems to inform future care decisions.
- Discharge Summary: A discharge summary is prepared when a patient is released from care. It shares similarities with the Perinatal SBAR form in summarizing the patient's condition and treatment while outlining any follow-up care required. Both forms aim to ensure that all pertinent information is communicated effectively to prevent any gaps in patient care.
Dos and Don'ts
Here are 7 things you should and shouldn't do when filling out the Perinatal SBAR form:
- Do: Assess the patient thoroughly before making the call.
- Do: Review the most recent notes to gather relevant information.
- Do: Have the patient’s chart readily available during the call.
- Do: Clearly identify yourself and your location at the start of the conversation.
- Don't: Use vague phrases, such as “might be” or “could be.” Be direct in your communication.
- Don't: Omit significant medical or obstetrical history from the report.
- Don't: Neglect to specify the time frame for any necessary follow-up or interventions.
Misconceptions
When discussing the Perinatal SBAR form, several misconceptions can cloud understanding and its effective use. Here are six common misunderstandings along with clarifications that can help whittle away confusion.
- The SBAR form is only for physicians. Many believe that only doctors should use the SBAR format. In reality, the SBAR is a communication tool that can be employed by all healthcare professionals involved in perinatal care, including nurses, midwives, and any staff interacting with patients during this critical time.
- You can skip the assessment. Some may think that a thorough assessment is unnecessary before using the SBAR. However, assessing the patient and reviewing recent notes is crucial. This ensures that the information shared is accurate and relevant, helping everyone involved make informed decisions.
- It’s just a formality and doesn't impact care. There's a misconception that the SBAR form is merely a routine step that lacks significance. On the contrary, effective communication through SBAR can significantly enhance patient outcomes and ensure that the right interventions occur quickly.
- The SBAR format is rigid and unchangeable. Many think the SBAR form cannot be adapted to varying situations. Although it follows a structured framework, healthcare providers can tailor the format to fit the unique narrative of each case as long as the essential components are present.
- I can provide vague information. Some individuals may believe that being vague in their reports is acceptable. In reality, clarity is essential. Detailed and specific descriptions enable better assessment and quicker responses, ultimately enhancing patient safety.
- Only urgent situations require SBAR communication. There is a belief that the SBAR is only necessary during emergencies. While it is critical in urgent situations, it can also be beneficial in routine exchanges of information regarding a patient's plan of care, ensuring everyone is on the same page at all times.
Understanding these misconceptions can help improve the utilization of the Perinatal SBAR form, facilitating better communication among healthcare providers and ultimately enhancing patient care.
Key takeaways
Filling out and using the Perinatal SBAR form effectively can enhance communication and patient care. Here are some key takeaways:
- Assess the patient first. Before contacting the physician or CNM, ensure you have thoroughly assessed the patient's condition.
- Read recent notes. Familiarize yourself with the patient’s medical history and recent remarks to provide an informed report.
- Keep the patient’s chart readily available. This will help you pull any necessary information quickly during the call.
- Conciseness is crucial. Aim for a 30-60 second report summarizing all essential information effectively.
- Clearly introduce yourself. Always state who you are, where you are calling from, and your role.
- Use a structured approach. Follow the SBAR format: Situation, Background, Assessment, Recommendation ensures you convey all necessary points.
- Stay specific in your communication. When mentioning concerns, detail exact symptoms or issues so the physician or CNM can understand the urgency.
- Be prepared with questions and suggestions. Know what you need from the physician and suggest possible tests or treatments as necessary.
Browse Other Templates
Difference Between Provider Enrollment and Credentialing - All fields in the Provider Information form are mandatory.
What Is a Permissible Withdrawal From 401k - The detailed instructions at the end of the form serve as a guide to submitting a complete request smoothly.
How to Hook Up Directv - This process ensures a smooth installation experience overall.