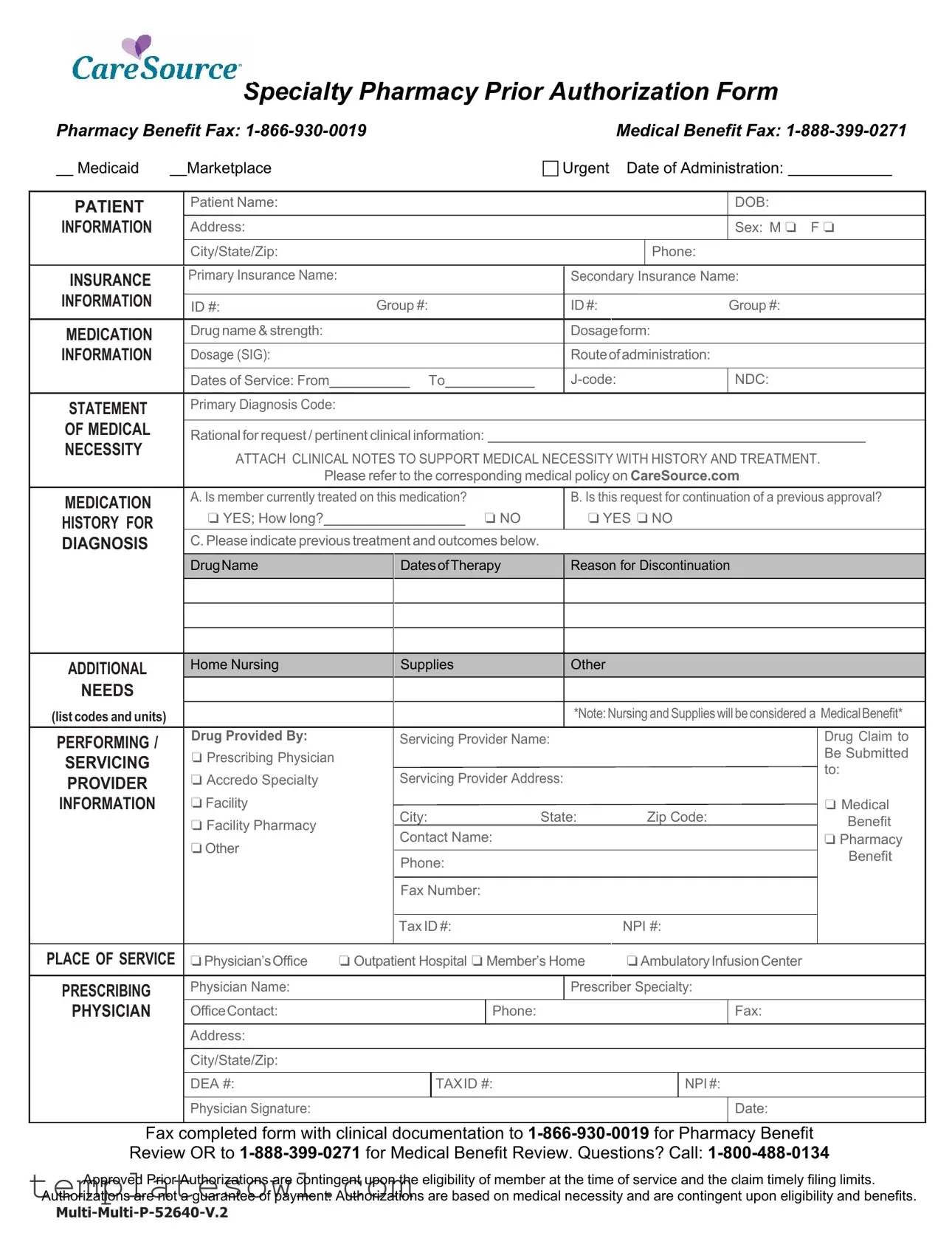
Fill Out Your Pharmacy Prior Authorization Form
The Pharmacy Prior Authorization form is a crucial tool within the healthcare system, designed to streamline medication requests and ensure patients receive the necessary treatments without unnecessary delays. Provided by CareSource, this form serves multiple purposes, encompassing both pharmacy benefits for Medicaid and marketplace medical benefits. When filling out this form, a healthcare provider must include detailed patient information, which involves the patient's name, date of birth, and insurance details, both primary and secondary. It also requires specific medication information, such as the drug name, dosage, and route of administration, along with critical dates and diagnosis codes. Furthermore, the form emphasizes the need for a robust statement of medical necessity, accompanied by clinical notes that outline the patient's medication history and previous treatment outcomes. Additional sections designate spaces for prescribing physician information and for the facility or provider handling the medication service. Notably, any approval granted through this prior authorization is subject to the member's eligibility and is not a guarantee of payment, highlighting the importance of medical necessity and adherence to filing limits. Understanding this form empowers both healthcare providers and patients to navigate the complexities of medication access more effectively.
Pharmacy Prior Authorization Example
Specialty Pharmacy Prior Authorization Form
|
Pharmacy Benefit Fax: |
|
Medical Benefit Fax: |
|||||||||||||||||||||||
|
|
Medicaid |
|
Marketplace |
|
|
|
|
|
|
|
|
Urgent |
Date of Administration: |
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
PATIENT |
Patient Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
DOB: |
|
|
|
|
|||||
|
INFORMATION |
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Sex: M ❏ |
F ❏ |
||||||||
|
|
|
|
|
City/State/Zip: |
|
|
|
|
|
|
|
|
|
|
|
Phone: |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
INSURANCE |
Primary Insurance Name: |
|
|
|
|
|
|
|
|
|
Secondary Insurance Name: |
|
|
|
|
||||||||||
|
INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
ID #: |
Group #: |
|
ID #: |
|
|
|
Group #: |
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
MEDICATION |
Drug name & strength: |
|
|
|
|
|
|
|
|
|
Dosageform: |
|
|
|
|
||||||||||
|
INFORMATION |
|
Dosage (SIG): |
|
|
|
|
|
|
|
|
|
Routeof administration: |
|
|
|
|
|||||||||
|
|
|
|
|
Dates of Service: From |
|
|
|
To |
|
|
|
|
NDC: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
STATEMENT |
Primary Diagnosis Code: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
OF MEDICAL |
|
Rational for request / pertinent clinical information: |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
NECESSITY |
ATTACH CLINICAL NOTES TO SUPPORT MEDICAL NECESSITY WITH HISTORY AND TREATMENT. |
||||||||||||||||||||||||
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
Please refer to the corresponding medical policy on CareSource.com |
|
|
|
|
||||||||||||||||
|
MEDICATION |
A. Is member currently treated on this medication? |
|
B. Is this request for continuation of a previous approval? |
||||||||||||||||||||||
|
HISTORY FOR |
|
❏ YES; How long? |
|
|
|
|
|
|
❏ NO |
|
❏ YES ❏ NO |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
DIAGNOSIS |
C. Please indicate previous treatment and outcomes below. |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
DrugName |
|
DatesofTherapy |
|
Reason for Discontinuation |
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
ADDITIONAL |
|
Home Nursing |
|
Supplies |
|
Other |
|
|
|
|
|
|
|
|
|
||||||||||
|
|
NEEDS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(list codes and units) |
|
|
|
|
|
|
|
|
|
|
|
|
*Note: Nursing and Supplies will be considered a MedicalBenefit* |
|||||||||||||
|
PERFORMING / |
Drug Provided By: |
|
Servicing Provider Name: |
|
|
|
|
|
|
Drug Claim to |
|||||||||||||||
|
SERVICING |
❏ Prescribing Physician |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Be Submitted |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
to: |
|||||||||
|
PROVIDER |
❏ Accredo Specialty |
|
Servicing Provider Address: |
|
|
|
|
|
|
❏ Medical |
|||||||||||||||
|
INFORMATION |
❏ Facility |
|
City: |
State: |
|
Zip Code: |
|
||||||||||||||||||
|
|
|
|
|
❏ Facility Pharmacy |
|
|
|
Benefit |
|||||||||||||||||
|
|
|
|
|
|
Contact Name: |
|
|
|
|
|
|
|
|
❏ Pharmacy |
|||||||||||
|
|
|
|
|
❏Other |
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Benefit |
|||||
|
|
|
|
|
|
Phone: |
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
Fax Number: |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
Tax ID #: |
|
|
NPI #: |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
PLACE OF SERVICE |
❏Physician’sOffice |
❏ Outpatient Hospital ❏ Member’s Home |
❏Ambulatory Infusion Center |
|
|
|
|
|||||||||||||||||||
|
PRESCRIBING |
Physician Name: |
|
|
|
|
|
|
|
|
|
Prescriber Specialty: |
|
|
|
|
||||||||||
|
PHYSICIAN |
|
OfficeContact: |
|
|
|
|
|
|
Phone: |
|
|
|
|
|
Fax: |
|
|
|
|
||||||
|
|
|
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
City/State/Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
DEA #: |
|
|
|
TAXID #: |
|
|
|
|
NPI #: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
Physician Signature: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: |
|
|
|
|
|||
Fax completed form with clinical documentation to
Approved Prior Authorizations are contingent upon the eligibility of member at the time of service and the claim timely filing limits.
Authorizations are not a guarantee of payment. Authorizations are based on medical necessity and are contingent upon eligibility and benefits.
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of the Form | The Pharmacy Prior Authorization form is used to obtain approval for specific medications, ensuring they are medically necessary before they are covered by insurance. This process helps control costs and ensures appropriate treatment for patients. |
| Patient Information Section | Essential patient details such as name, date of birth, address, and insurance information are required. Completing this section ensures that the request can be processed without delays due to missing information. |
| Supporting Documentation | Clinical notes supporting the medical necessity of the medication must be attached. This includes a history of previous treatments and outcomes to provide a comprehensive view of the patient's condition. |
| Submission Instructions | Completed forms should be faxed to the designated numbers for either Pharmacy Benefit Review or Medical Benefit Review. This differentiation is crucial for the timely processing of requests. |
| State-Specific Regulations | The use of the prior authorization form may be governed by specific state laws, which can vary significantly. In many states, such requirements are codified under Medicaid regulations or pharmacy benefit management laws. |
Guidelines on Utilizing Pharmacy Prior Authorization
Completing the Pharmacy Prior Authorization form is essential for ensuring that your medication is approved in a timely manner. By following the steps outlined below, you can accurately fill in the required information, helping to streamline the approval process for necessary treatment.
- Begin with the PATIENT INFORMATION section. Fill in the patient's name, date of birth, address, city, state, zip code, phone number, and sex.
- Next, provide details in the INSURANCE INFORMATION section. Include the primary and secondary insurance names, along with the corresponding ID and group numbers.
- In the MEDICATION INFORMATION section, write the drug name and strength. Specify the dosage form, dosage (SIG), and route of administration. List the dates of service, along with the primary diagnosis code, J-code, and NDC number.
- Articulate the STATEMENT OF MEDICAL NECESSITY. Include a rationale for the request, along with pertinent clinical information. Remember to attach clinical notes that support the medical necessity regarding the history and treatment of the patient.
- Indicate whether the member is currently treated with the medication. If yes, specify how long. If no, proceed to the next question about previous treatments and their outcomes.
- Confirm if this request is for the continuation of a previous approval. Note the reason for discontinuation if applicable. You may also list any ADDITIONAL NEEDS by including necessary codes and units.
- In the PERFORMING / SERVICING PROVIDER INFORMATION section, indicate the name and address of the servicing provider. Specify whether the drug is provided by a home nursing service, prescribing physician, specialty facility, or pharmacy.
- Designate the DRUG CLAIM TO BE SUBMITTED TO section by filling out the appropriate contact information and city.
- In the PLACE OF SERVICE section, mark the location where the service will be provided, such as the physician’s office, outpatient hospital, member’s home, or ambulatory infusion center.
- Next, complete the PRESCRIBING PHYSICIAN information with the physician’s name, specialty, office contact, address, phone, fax numbers, and DEA, Tax ID, and NPI numbers.
- Finally, ensure the physician sign and date the form, confirming their acknowledgment of the provided information.
- Fax the completed form along with any clinical documentation to the correct number: 1-866-930-0019 for Pharmacy Benefit Review or 1-888-399-0271 for Medical Benefit Review.
By carefully adhering to these steps, you create a comprehensive and thorough submission, improving the likelihood of a swift and successful approval for the medication required. Pay attention to each detail, as incomplete information may delay the process significantly.
What You Should Know About This Form
What is a Pharmacy Prior Authorization form?
The Pharmacy Prior Authorization form is a document that healthcare providers fill out to request approval for certain medications before the insurance company will cover the costs. This process helps ensure that the medication is medically necessary for the patient’s treatment plan and that it meets the insurer’s guidelines.
When is a Pharmacy Prior Authorization needed?
A Pharmacy Prior Authorization is typically needed when a specific medication is not covered under a patient's insurance policy, or when the medication requires additional approval due to its high cost or potential risks. The insurance provider will specify which medications require this form.
What information is required on the form?
The form asks for detailed patient information, medication details, and a statement of medical necessity. This includes the patient’s name, date of birth, insurance information, the name and dosage of the medication, the diagnosis code, and a rationale for why the medication is needed.
How does the approval process work?
After the healthcare provider submits the completed form with all necessary documentation, the insurance company will review it. This review will determine if the medication is medically necessary and if it complies with their policies. The provider will receive a response indicating whether the request has been approved or denied.
What should be included in the Statement of Medical Necessity?
The Statement of Medical Necessity should explain why the medication is essential for the patient’s treatment. It should include the patient’s medical history, previous treatments, their outcomes, and any relevant clinical notes that support the need for this specific medication.
What happens if a prior authorization request is denied?
If the prior authorization request is denied, the patient's healthcare provider will be notified. The provider can appeal the decision by submitting additional information or documentation that may support the need for the medication. It is important for the patient to communicate with their provider about any next steps.
Can patients submit the Pharmacy Prior Authorization form directly?
Typically, patients should not submit the Pharmacy Prior Authorization form directly. The form needs to be filled out by a healthcare provider who has a full understanding of the patient’s medical history and treatment needs. Patients should work closely with their provider to ensure the request is submitted correctly.
How long does it take to receive a decision?
The timeframe for receiving a decision can vary. Generally, patients can expect to hear back from the insurance company within a few business days after the form is submitted. However, in urgent situations, the process may be expedited. If additional information is needed, this may delay the decision.
Common mistakes
Filling out a Pharmacy Prior Authorization form can be a straightforward process, but several common mistakes can lead to delays or denials. One common mistake occurs when the patient's information is not completely filled out. Missing details like the patient's date of birth, address, or contact information can cause confusion and slow down the review process.
Another issue arises with the insurance information. Sometimes, people forget to include details about their primary and secondary insurance plans. It's crucial to provide accurate ID numbers and group numbers. If this information is incorrect or missing, the claim may not be processed correctly.
A third mistake involves the medication information section. Some individuals may not specify the drug name, strength, or dosage form properly. Additionally, failing to provide a complete dosage instruction can lead to uncertainties about how the medication will be administered.
In the section requesting medical necessity, it's common to see vague statements. Applicants often leave out critical information about previous treatments and outcomes. Providing thorough details about prior therapies can significantly impact the approval process.
Another frequent error occurs when individuals overlook the supporting documentation. It is essential to attach clinical notes that back up the claim of medical necessity. Without these documents, the request may be deemed insufficient.
People also sometimes do not check whether the member is currently being treated with the medication. Clearly indicating if this request is for continuation or a new approval is vital. This information helps provide context to the reviewer.
Lastly, some applicants may forget to sign the form or include the prescriber’s details. Missing signatures or inaccurate provider information can lead to automatic rejections. Ensure that all required sections are filled completely and accurately.
Documents used along the form
The Pharmacy Prior Authorization form is an essential document utilized in the approval process for medication coverage by insurance providers. Several other forms and documents typically accompany this form to provide comprehensive information regarding the patient's treatment plan. Here are some of the additional documents that may be required:
- Clinical Notes: These notes provide detailed information from the healthcare provider regarding the patient's medical history and treatment response. They help support the medical necessity of the requested medication.
- Medication History Form: This document outlines the patient's previous and current medications. It highlights any existing allergies or adverse reactions, which can be crucial for safe prescribing.
- Diagnosis Documentation: Medical records demonstrating the patient's diagnoses, including relevant lab results or imaging tests, are usually necessary to justify the requested medication.
- Insurance Verification Form: This form confirms the patient's insurance coverage details, including policy numbers and coverage limits, which may affect the authorization process.
- Continuity of Care Form: If the request is for a continuation of a previously approved medication, this document outlines the treatment history, including prior approval details and reasons for ongoing treatment.
- Prescription Drug Claim Form: This form is submitted to request reimbursement for the cost of the medication. It includes specific details about the medication, the provider, and the patient.
- Provider Credentialing Form: This document verifies the qualifications of the prescribing physician. It includes information such as the prescriber's certifications and affiliations with medical boards.
Each of these documents plays a critical role in ensuring that the Pharmacy Prior Authorization process is thorough and efficient. Collecting all necessary documentation helps healthcare providers ensure that patients receive timely access to their prescribed medications.
Similar forms
Insurance Prior Authorization Form: Similar to the Pharmacy Prior Authorization form, the Insurance Prior Authorization form requests approval from an insurance provider before receiving specific medical services. It requires patient details, a description of the service, and justification for the request based on medical necessity.
Medication Request Form: This document is used to request a medication that requires special approval before filling. Like the Pharmacy Prior Authorization form, it includes patient information, medication specifics, and reasons for the request, emphasizing the need for the medication in the patient's treatment.
Durable Medical Equipment (DME) Prior Authorization Form: This form serves a similar purpose for requesting approval for specific medical equipment. Both documents require patient and provider information and a statement justifying the medical necessity of the requested equipment.
Specialist Referral Form: Used to obtain permission to see a specialist, this form collects relevant patient information and the reasons for the referral. Both forms necessitate thorough justifications, ensuring that the patient receives the appropriate level of care based on medical necessity.
Hospital Admission Authorization Form: This form requests approval for inpatient hospital services. It includes patient details, the reason for admission, and supporting medical information—similar to the pharmacy prior authorization that emphasizes medical necessity and justifies the request.
Dos and Don'ts
When filling out the Pharmacy Prior Authorization form, following some simple dos and don'ts can help ensure a smooth process. Here’s what to keep in mind:
- Do provide complete patient information. Include the patient's name, date of birth, address, and phone number.
- Don't leave out insurance details. Make sure to fill in both primary and secondary insurance information, including ID and group numbers.
- Do clearly indicate the medication being requested. Include the drug name, strength, dosage form, and dosage instructions.
- Don't forget about medical necessity. Attach clinical notes that support the need for the medication and any previous treatments.
- Do verify details about the prescribing physician. Ensure their name, contact information, and relevant credentials are accurately listed.
- Don't forget your signature. The prescriber must sign and date the form before submission to validate the request.
Misconceptions
Understanding the complexities surrounding pharmacy prior authorization is essential for both patients and healthcare providers. Misconceptions can lead to confusion and frustration. Here are some common misconceptions about the Pharmacy Prior Authorization form:
- 1. Prior authorization means my medication is denied. Many people believe that if a medication requires prior authorization, it will be automatically denied. In reality, prior authorization is a process that allows insurance companies to assess whether a medication is necessary before it is dispensed. It does not signify a denial but rather a safeguard to ensure appropriate use of medications.
- 2. The process is the same for all medications. Not all medications require prior authorization. The requirements vary depending on the insurance plan and the specific medication. Many common generic drugs may not require this extra step, while certain brand-name or specialty drugs typically do.
- 3. The forms are always filled out incorrectly. While mistakes can occur, many healthcare providers are experienced in completing prior authorization forms accurately. Additional information may be needed, but with clear communication, the likelihood of errors can be minimized.
- 4. The prior authorization process takes an unreasonable amount of time. Although it can sometimes feel lengthy, many requests are reviewed within a short period. If additional documentation is required or if there are unusual circumstances, the process may take longer. Generally, providers can assist in expediting urgent requests.
- 5. Prior authorization guarantees that my medication will be covered. Even with an approved prior authorization, coverage is not guaranteed. The authorization is contingent upon patient eligibility and benefit verification at the time of service. It’s crucial to understand that this process focuses on medical necessity and does not assure payment.
For patients navigating this process, being informed can help in interacting with healthcare providers and insurance representatives. Each step brings clarity to a system designed to facilitate patient care.
Key takeaways
The Pharmacy Prior Authorization form is a crucial document in the process of obtaining necessary medications. Here are eight key takeaways to consider when filling out and using this form:
- Patient Information: Ensure all patient details are complete and accurate. This includes the patient's name, date of birth, address, and contact information.
- Insurance Information: Double-check both primary and secondary insurance details, including the ID and group numbers, to avoid delays.
- Medication Details: Specify the drug name, strength, dosage form, and route of administration. This information is essential for processing the request.
- Medical Necessity: Attach detailed clinical notes that support the need for the medication. This documentation should outline history and previous treatment outcomes.
- Previous Treatments: Clearly indicate if the member is currently on this medication or if this is a request for continuation. Record past therapies and their results.
- Prescribing Physician: Provide complete information about the prescribing physician, including their specialty, contact details, and applicable identification numbers.
- Submission of the Form: Fax the completed form along with all necessary clinical documentation to the correct review line. The numbers are 1-866-930-0019 for Pharmacy Benefit Review or 1-888-399-0271 for Medical Benefit Review.
- Understand Limits: Approved prior authorizations depend on member eligibility at the time of service and adherence to claim filing limits. They do not guarantee payment.
Browse Other Templates
Who Has the Right to Change a Life Insurance Policy's Beneficiary - Your signature and date signify your acceptance and understanding of the changes being made.
Vanguard Ira Distribution Form - Use this form as part of your financial planning when ownership changes are necessary.
Answer to Complaint California - The response should include details about the defendant’s position regarding each allegation raised in the complaint.