Fill Out Your Physician Statement Form
The Physician Statement Form is a crucial document that serves multiple purposes in the context of health insurance claims. This form must be completed by both the primary insured individual and the examining physician. For the primary insured, it requires essential information such as their name, policy number, and insurance purchase date. The physician section gathers detailed patient data including the patient's name, date of birth, and a description of their medical condition. Additionally, the physician’s qualifications are recorded—this includes their specialty, contact information, and whether they are the patient’s primary care physician. The form also asks for information about the patient's diagnosis, the nature of the examination, the dates of prior office visits, and any recommendations regarding travel plans due to medical conditions. Furthermore, it requires certification from the physician, affirming that the provided details are true and accurate, ensuring that the insurance company has the necessary information to process claims efficiently. This form ultimately bridges the gap between healthcare providers and insurance companies, helping to facilitate the claims process for individuals who encounter unexpected health issues while traveling.
Physician Statement Example
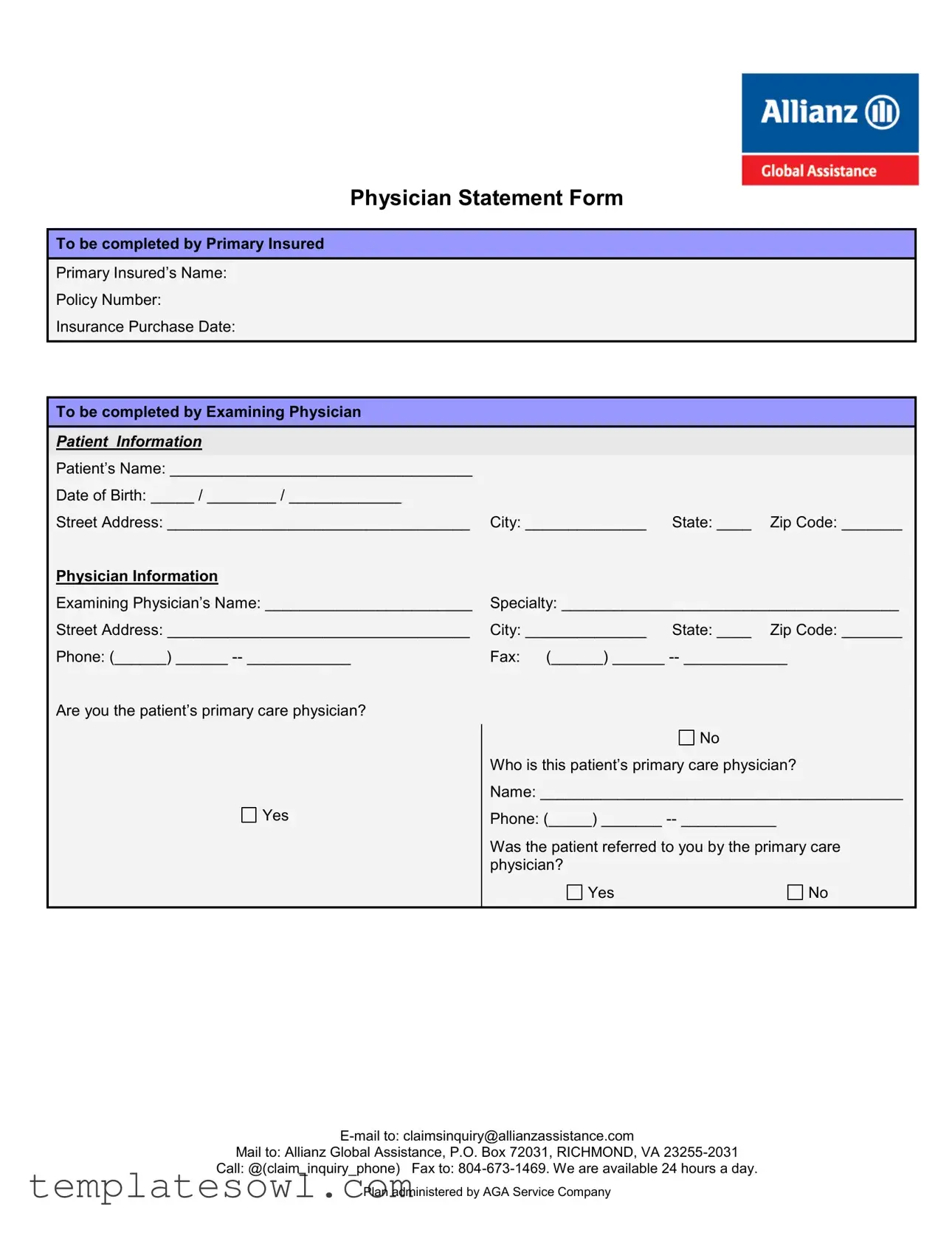
Physician Statement Form
To be completed by Primary Insured
Primary Insured’s Name:
Policy Number:
Insurance Purchase Date:
To be completed by Examining Physician
|
|
PATIENT INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient’s Name: ___________________________________ |
|
|
|
|
|
|
Date of Birth: _____ / ________ / _____________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address: ___________________________________ |
City: ______________ |
State: ____ |
Zip Code: _______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Physician Information |
|
|
|
|
|
|
Examining Physician’s Name: ________________________ |
Specialty: _______________________________________ |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address: ___________________________________ |
City: ______________ |
State: ____ |
Zip Code: _______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Phone: (______) ______ |
Fax: (______) ______ |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you the patient’s primary care physician? |
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
Who is this patient’s primary care physician? |
|||
|
|
|
Name: __________________________________________ |
|||
|
|
Yes |
Phone: (_____) _______ |
|||
|
|
|
|
|
|
|
|
|
|
Was the patient referred to you by the primary care |
|||
|
|
|
physician? |
|
|
|
|
|
|
Yes |
|
|
No |
|
|
|
|
|
|
|
Mail to: Allianz Global Assistance, P.O. Box 72031, RICHMOND, VA
Call: @(claim_inquiry_phone) Fax to:
Plan administered by AGA Service Company
Patient’s Diagnosis: |
|
|
Did you perform an actual examination? |
Yes |
No |
Date of the exam: ____ / _____ / _________
Please indicate the primary diagnosis for which you examined the patient:
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Date symptoms first appeared or accident occurred: ____ / _____ / _________ |
|
|
Is this condition a complication of an underlying condition? |
Yes (specify below) |
No |
__________________________________________________________________________________________________
Please list the dates of the patient’s office visits in the 120 days before the insurance purchase date, noted above. Circle the dates where you treated the patient for the above stated condition.
|
|
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
|
|
|
|
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
|
|
|
|
|
|
|
|
|
|
|
|
Did you advise the trip be cancelled or interrupted due to the patient’s medical condition? |
|
|
|
||
|
|
Yes Date: ___ / ___ / _________ |
|
No |
|
|
|
|
|
Please explain why you made this recommendation. |
Please explain why you did not make this recommendation. |
|
|
||
|
|
Provide details on the circumstances and medical diagnosis |
Provide details on the circumstances and medical diagnosis |
|
|
||
|
|
of the patient that you consider relevant to the insured’s |
of the patient that you consider relevant to the insured’s |
|
|
||
|
|
decision to cancel or interrupt their trip due to injury or |
decision to cancel or interrupt their trip due to injury or |
|
|
||
|
|
illness. |
|
illness. |
|
|
|
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
|
|
|
|
|
|
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
If the patient is the insured, on what date did he/she become medically unable to travel? |
___ / ___ / ________ |
|
|
||
|
|
|
|
|
|
|
|
By my signature and stamp below, I hereby certify that the above is true and correct
Physician Signature: _________________________________________________ Date ____/____/______
Physician Stamp:
Mail to: Allianz Global Assistance, P.O. Box 72031, RICHMOND, VA
Call: @(claim_inquiry_phone) Fax to:
Plan administered by AGA Service Company
Form Characteristics
| Fact Title | Details |
|---|---|
| Purpose | The Physician Statement Form is designed to collect relevant medical information about a patient, typically for insurance claims related to travel or health insurance. |
| Patient Information | It requires basic details about the patient, including their name, date of birth, and contact information to ensure accurate identification. |
| Physician Information | Physicians must provide their own details, such as name, specialty, and contact information, to verify their qualifications and authority in providing the medical evaluation. |
| Primary Care Physician | The form asks whether the examining physician is the patient's primary care physician and requires the name and contact information of the primary care physician if not. |
| Diagnosis Section | There's a section dedicated to the patient's diagnosis, including the primary diagnosis and relevant ICD-9 code, for clear medical documentation. |
| Office Visit Dates | Physicians must list patient office visit dates within 120 days prior to the insurance purchase date, assessing continuity of care and relevant treatment history. |
| Recommendation to Cancel | Physicians are required to indicate whether they advised the patient to cancel or interrupt their trip, providing reasoning for their recommendation. |
| Certification | The physician must sign and stamp the form, certifying that all provided information is accurate and true, which adds a layer of accountability. |
| Submission Details | The completed form can be submitted via email, fax, or postal mail to Allianz Global Assistance, ensuring multiple avenues for submission. |
| Governing Laws | The governing laws may vary by state; healthcare practitioners should familiarize themselves with local regulations involving patient privacy and insurance claims. |
Guidelines on Utilizing Physician Statement
Once you have gathered all necessary information, you are ready to fill out the Physician Statement form. This process requires attention to detail to ensure accuracy in documenting the patient’s condition and doctor's recommendations. Follow these steps for a smooth experience.
- Complete the top section: Fill in the Primary Insured’s Name, Policy Number, and Insurance Purchase Date.
- Provide patient information: Include the Patient’s Name, Date of Birth, Street Address, City, State, and Zip Code.
- Enter examining physician information: Write down the Examining Physician’s Name, Specialty, Street Address, City, State, Zip Code, Phone, and Fax.
- Identify the primary care physician: State whether you are the patient’s primary care physician. If not, include the primary care physician’s name and phone number.
- Clarify referral details: Indicate if the patient was referred by the primary care physician.
- Diagnose the patient: Provide the Patient’s Diagnosis, state if you performed an actual examination, and include the exam date.
- Record the primary diagnosis: Clearly write the primary diagnosis and its corresponding ICD-9 Code. Also, indicate when symptoms first appeared.
- Address underlying conditions: Specify if the condition is a complication of another condition.
- List office visits: Document the dates of the patient’s office visits in the 120 days prior to the insurance purchase date, circling the relevant ones.
- Advise on travel: State whether you recommended canceling or interrupting the patient’s trip, and provide the date if applicable.
- Explain your recommendation: Offer details on the medical circumstances that led to your recommendation or why you did not recommend a change in travel plans.
- Document medical inability: If the patient is the insured, indicate when they became medically unable to travel.
- Certify the information: Sign and date the form and apply your physician stamp where required.
Be sure to double-check your entries for accuracy. After completing the form, it can be submitted via email, fax, or regular mail to the designated address. Ensuring this is done promptly might be crucial for the patient’s claims process.
What You Should Know About This Form
What is the purpose of the Physician Statement Form?
The Physician Statement Form is designed to gather essential medical information about a patient from their examining physician. This information is crucial for processing insurance claims, particularly for evaluating whether a medical condition is valid for trip cancellation or interruption claims. By providing accurate details, the form helps ensure that claims are reviewed thoroughly and fairly.
Who should complete this form?
The form should be completed by the examining physician who has firsthand knowledge of the patient’s medical condition. The primary insured, the individual covered under the insurance policy, must also provide some initial information. Collaboration between both parties ensures that the form is filled out accurately and completely, reflecting the patient's current health status.
What information is required from the physician?
The physician must provide their name, specialty, and contact information, including phone and fax numbers. They will also document the patient's diagnosis and confirm whether they performed an actual examination. Additionally, the physician needs to indicate important dates, such as the date of the exam and when the symptoms first appeared. This comprehensive information assists in evaluating the patient's medical situation regarding the insurance claim.
How does the physician note their recommendation regarding trip cancellation?
If the physician recommends cancelling or interrupting a trip due to medical reasons, they must check "Yes" and provide the date of that recommendation. Furthermore, they should elaborate on the circumstances that led to this advice. If they do not recommend cancellation, they must explain their reasoning as well. This information is vital for the claims process and helps the insurance provider understand the medical perspective.
What are the implications of the physician’s signature on the form?
By signing the form, the physician certifies that all provided information is accurate and truthful. This signature holds significant weight, as it confirms that the examining physician has thoroughly assessed the patient and stands by their professional opinion regarding the treatment and travel ability of the patient. Inaccuracies or misunderstandings can lead to delays in processing claims.
What should be done if additional information is needed after the form is submitted?
If additional clarification or information is required after submission, the claims department may reach out to the physician or the insured. It is essential to respond promptly to any inquiries, as this can expedite the claims process. The insurance provider is available 24/7 via various contact methods, ensuring that support is accessible whenever needed.
Common mistakes
Filling out a Physician Statement form can be a critical process for ensuring that claims are processed smoothly and efficiently. However, many people make common mistakes that can lead to delays or complications. Understanding these pitfalls can help ensure that the form is completed accurately.
One frequent error occurs when the primary insured’s information is not clearly stated. It is essential to properly fill in the name and policy number of the primary insured at the beginning of the form. Missing or incorrect details can result in the claim not being attributed to the correct insurance policy, causing unnecessary confusion and delays in processing.
Another mistake involves failing to provide accurate patient information. This might include omitting the patient’s date of birth, street address, or other critical identifying information. Complete and accurate patient details are crucial. They not only demonstrate the legitimacy of the claim but also help the insurance company to process claims efficiently.
Many individuals overlook the significance of documenting office visit dates. This section requires a list of dates when the patient visited the physician in the 120 days before the insurance purchase date. Forgetting to provide this information can weaken the claim and lead to additional requests for information, which can slow down the processing time.
Inconsistent or vague responses can also create issues. For instance, when asked if the physician advised the patient to cancel or interrupt their trip due to medical conditions, clear affirmations or explanations are vital. A simple “Yes” or “No” without accompanying details can lead to questions from the insurance provider. Providing thorough explanations helps to clarify the physician’s recommendations and supports the claim.
Lastly, failing to sign and date the form appropriately can render it invalid. The physician’s signature is essential to verify that the information provided is accurate and truthful. Moreover, failing to use a physician stamp, if applicable, can lead to further verification processes, delaying claims processing.
By being aware of these common mistakes, physicians can help their patients navigate the requirements of the Physician Statement form more effectively. Clear, accurate, and complete submissions contribute to a more streamlined claims experience.
Documents used along the form
The Physician Statement form plays a crucial role in the claims process for travel or health insurance. It provides necessary medical information regarding the patient’s condition, often influencing insurance decisions. However, this document is typically used in conjunction with several other forms that help complete the claims process and provide context to the insurer. Below are four common documents that may be required alongside the Physician Statement form.
- Medical Records Release Form: This document authorizes the release of a patient's medical records to the insurance company. It ensures that the insurer has access to relevant health information and past medical history necessary for processing claims. Without this form, insurers may face challenges in verifying claims related to the patient’s medical history.
- Claim Form: The claim form serves as the official request for benefits from the insurance company. It includes details about the insured event, such as the date of travel, type of coverage, and specifics about the claim itself. This form usually requires detailed information that complements the insights provided in the Physician Statement form.
- Travel Insurance Policy Document: This document outlines the specific terms and conditions of the insurance coverage purchased by the insured. It details the extent of the coverage, including any exclusions or limitations. Reviewing this document alongside the Physician Statement is essential for understanding what the insurer is obligated to cover.
- Patient Authorization Form: This form grants permission for medical professionals to share the patient’s health information with the insurance provider. It is an important component in ensuring compliance with privacy regulations. With this authorization, claims processors can efficiently handle the necessary documentation for a smoother claims experience.
Collectively, these documents create a comprehensive case for insurance providers to evaluate patient claims accurately. Each one plays a pivotal role in ensuring that all relevant information is available to make informed decisions regarding coverage and benefits. If you are navigating this process, be sure to gather all necessary documentation to support your claim effectively.
Similar forms
- Medical Clearance Form: Like the Physician Statement, a Medical Clearance Form requires a physician to evaluate a patient's fitness for travel. Both documents include patient medical history and may indicate whether travel should be postponed due to health concerns.
- Patient Referral Form: This form documents referrals from one healthcare provider to another. Similar to the Physician Statement, it includes patient information and treatment details, establishing continuity of care while also specifying the patient's health status.
- Insurance Claim Form: This document is used to request reimbursement for medical expenses. Like the Physician Statement, it often necessitates detailed medical information and diagnosis to justify claims related to travel or health disruptions.
- Doctor’s Letter: A Doctor’s Letter explains a patient’s medical situation, much like a Physician Statement. Both convey vital health information that may affect decisions like trip cancellations or medical leave.
- Disability Certificate: This document certifies that a patient is unable to work due to health conditions. Similar to the Physician Statement, it provides thorough details regarding medical diagnoses and the implications for the patient’s daily activities.
- Injury Report: This form outlines the specifics of an injury, including diagnosis and treatment history. It aligns closely with the Physician Statement, detailing the medical evaluation and the need for travel coverage.
- Health Assessment Form: Used by healthcare facilities to evaluate a patient’s overall health, this form includes medical history and current conditions. Both forms aim to ensure the patient's well-being and travel safety.
- Patient History Form: This document collects comprehensive medical history before treatment. While the Physician Statement focuses on a specific condition, both forms facilitate the understanding of a patient’s health background.
- Travel Health Insurance Application: This form collects necessary information to assess eligibility for health insurance while traveling. Similar to the Physician Statement, it combines personal health details with the patient’s travel intentions and potential risks.
- Pre-Travel Risk Assessment Form: Used to evaluate travelers’ health risks, this form gathers specific information about medical conditions, much like the Physician Statement. Both aim to identify any potential health issues before traveling.
Dos and Don'ts
When filling out the Physician Statement form, attention to detail is essential. Understanding what to do and what to avoid can make a significant difference in the accuracy and effectiveness of your submission. Here are key considerations.
- Do ensure all patient information is complete and accurate. Check the spelling of names and the correctness of dates.
- Do clearly state the patient's primary diagnosis, including appropriate ICD-9 codes where applicable. This information is crucial for processing the claim efficiently.
- Do indicate whether you performed an actual examination, as this can affect the validity of the statement.
- Do note all relevant office visit dates, especially those related to the patient's condition leading up to the insurance purchase. Highlight any treatments administered on those dates.
- Do provide detailed explanations if you advise canceling or interrupting a trip due to medical conditions. This context assists in substantiating the recommendation.
- Don't leave any sections blank. Incomplete forms can cause delays in processing and approvals.
- Don't use vague language. Clearly articulate the medical conditions and circumstances to avoid misunderstandings.
- Don't forget to sign and stamp the form. An unsigned form may be considered invalid, regardless of the content provided.
- Don't provide unnecessary personal details about the patient that are not relevant to their medical condition or treatment.
- Don't submit the form without reviewing it. A final check can reveal mistakes or omissions that could hinder the claim process.
By following these guidelines, the process of completing the Physician Statement form can become much simpler and more effective, ultimately benefiting both the physician and the patient.
Misconceptions
The Physician Statement form is a crucial document in the insurance claim process, but many people hold misconceptions about its purpose and use. Understanding these misconceptions can help ensure that the form is completed correctly and efficiently.
- It is only needed for travel insurance claims. While the form is commonly used in travel insurance contexts, it can also be relevant for other types of insurance claims, such as health or life insurance, where medical conditions impact coverage.
- The patient must fill out the entire form. In fact, only the primary insured (the policyholder) is required to complete their section. The rest of the form should be filled out by the physician providing the medical evaluation.
- A physician's signature guarantees that a claim will be approved. Although a completed Physician Statement form is essential for processing a claim, it does not guarantee approval. Insurance companies evaluate claims based on various factors, including policy terms and the evidence provided.
- Only primary care physicians can complete the form. Any licensed physician qualified to assess the patient's condition can fill out the form, including specialists involved in the patient's care.
- The form must be filled out in person. Physicians can complete and submit the form electronically, making the process more convenient for both the provider and the patient.
- The information provided on the form is kept confidential. While medical information is subject to privacy laws, there are instances where information from the form may be shared with other parties involved in the insurance process. It is essential to understand the privacy implications.
- All insights from the physician are optional. Detailed explanations for recommended actions, such as travel cancellations, need to be included for the form to be effective. These insights are vital for the insurance company to assess the claim accurately.
Clarifying these misconceptions helps ensure that patients, physicians, and insurance providers navigate the claims process smoothly. Correctly completing the Physician Statement form contributes to an efficient claims experience and can significantly impact claim outcomes.
Key takeaways
When filling out and using the Physician Statement form, keep these important points in mind:
- Complete all sections: Ensure that both the primary insured and examining physician fill out their respective sections completely. Missing information could delay processing.
- Accuracy is crucial: All details provided, especially concerning patient diagnosis and treatment history, should be accurate and up-to-date to reflect the patient's medical condition accurately.
- Include dates of office visits: Clearly list all relevant office visit dates prior to the insurance purchase date. It’s important to circle any dates where the patient received treatment for their current condition.
- Document your recommendations: If you advise that a trip be canceled or interrupted due to the patient’s medical condition, provide a detailed explanation. This assists in clarifying the medical necessity of your recommendation.
- Submit by the correct method: Ensure the completed form is submitted via the specified methods—email, mail, or fax—to the correct Allianz Global Assistance address listed on the form.
Browse Other Templates
Cslb Preliminary Notice Form - Agree to comply with company rules and regulations upon hiring.
Tc-810 - Owners need to be cognizant of the expiration of the TC-810 validity as it relates to vehicle registration and inspections.
Mining Activity Operations Plan,National Forest Mining Proposal Form,USDA Forest Service Mining Plan,Mining Project Operation Document,FS 2800 Series Operations Plan,Forest Service Mining Activity Application,National Forest System Mining Operations - Details regarding potential impacts on surrounding environments are vital in the submitted form.