Fill Out Your Polst Form
The Physician Orders for Life-Sustaining Treatment (POLST) form is an essential tool designed to communicate a patient's medical preferences regarding life-sustaining treatments. It serves as a medical order that healthcare providers are required to follow, thus ensuring that a patient's wishes are respected, especially in emergency situations. The form, established by California law and effective from October 1, 2014, outlines specific treatment options based on a patient's health status and individual preferences. These options include cardiopulmonary resuscitation (CPR) directives and medical interventions, categorized as full treatment, selective treatment, or comfort-focused treatment. The POLST form is particularly beneficial for individuals with serious or chronic illnesses, as it addresses their desires regarding advanced medical interventions, including nutrition options. Importantly, while the POLST complements an Advance Directive, it is not a replacement. It must be signed by both a physician and either the patient or their legally recognized decisionmaker to be deemed valid. In instances where treatment preferences change or the patient's condition evolves, it is recommended that the POLST be reviewed to ensure continued alignment with the patient's wishes.
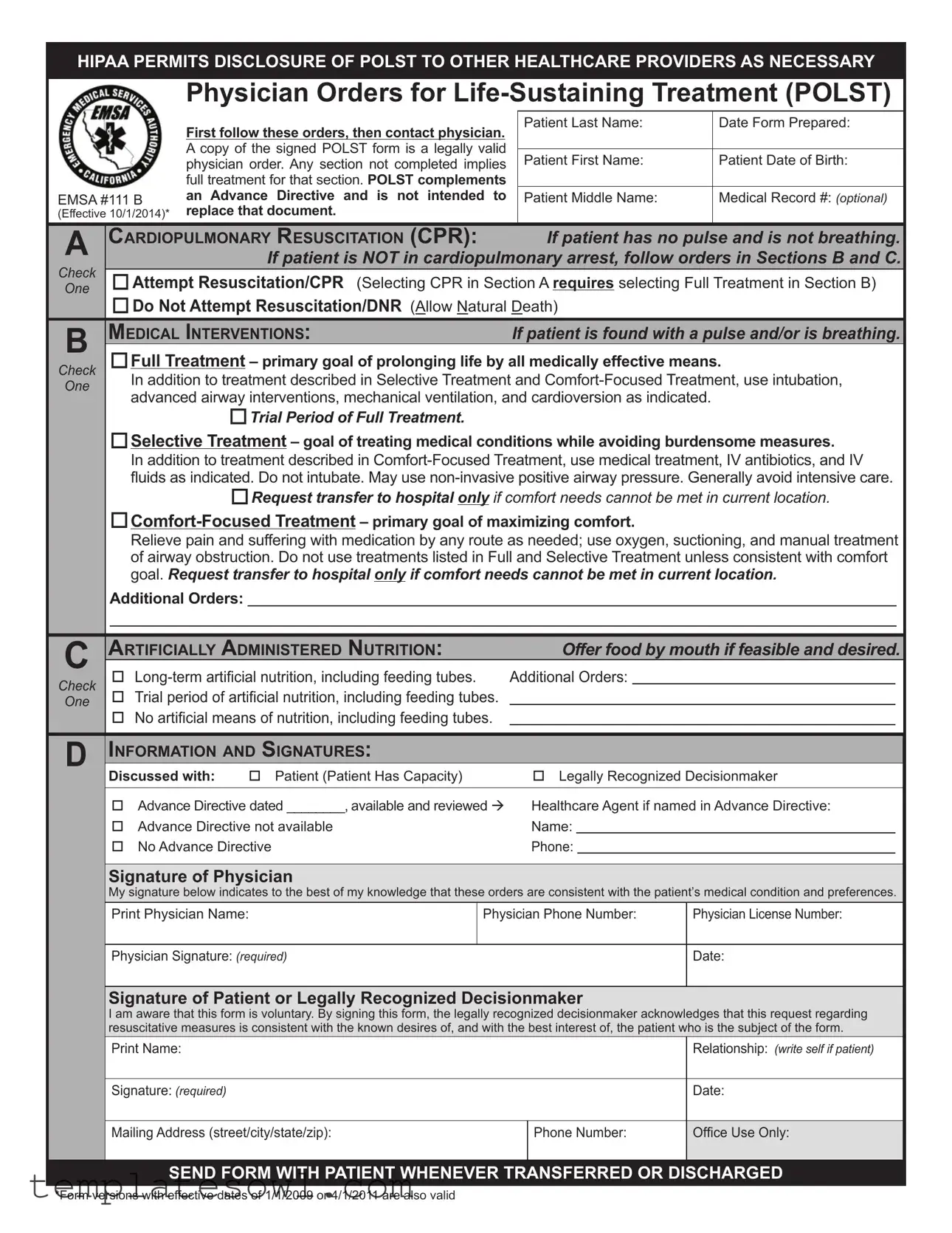
Polst Example
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTHCARE PROVIDERS AS NECESSARY
EMSA #111 B
(Effective 10/1/2014)*
Physician Orders for
First follow these orders, then contact physician. |
Patient Last Name: |
Date Form Prepared: |
|
|
|
||
A copy of the signed POLST form is a legally valid |
|
|
|
Patient First Name: |
Patient Date of Birth: |
||
physician order. Any section not completed implies |
|||
full treatment for that section. POLST complements |
|
|
|
an Advance Directive and is not intended to |
Patient Middle Name: |
Medical Record #: (optional) |
|
replace that document. |
|
|
|
|
|
|
A |
CARDIOPULMONARY RESUSCITATION (CPR): |
If patient has no pulse and is not breathing. |
|
||||
|
|
|
If patient is NOT in cardiopulmonary arrest, follow orders in Sections B and C. |
|
|||
CheckOne |
|
oAttempt Resuscitation/CPR (Selecting CPR in Section A requires selecting Full Treatment in Section B) |
|
||||
|
|
oDo Not Attempt Resuscitation/DNR (Allow Natural Death) |
|
||||
B |
|
MEDICAL INTERVENTIONS: |
If patient is found with a pulse and/or is breathing. |
|
|||
|
oFull Treatment – primary goal of prolonging life by all medically effective means. |
|
|||||
Check |
|
||||||
One |
In addition to treatment described in Selective Treatment and |
|
|||||
advanced airway interventions, mechanical ventilation, and cardioversion as indicated. |
|
||||||
|
|
|
|||||
|
|
oTrial Period of Full Treatment. |
|
|
|
|
|
|
|
oSelective Treatment – goal of treating medical conditions while avoiding burdensome measures. |
|
||||
|
|
In addition to treatment described in |
|
||||
|
|
luids as indicated. Do not intubate. May use |
|
||||
|
|
oRequest transfer to hospital only if comfort needs cannot be met in current location. |
|
||||
|
|
|
|||||
|
|
Relieve pain and suffering with medication by any route as needed; use oxygen, suctioning, and manual treatment |
|
||||
|
|
of airway obstruction. Do not use treatments listed in Full and Selective Treatment unless consistent with comfort |
|
||||
|
|
goal. Request transfer to hospital only if comfort needs cannot be met in current location. |
|
||||
|
|
Additional Orders: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C |
|
ARTIFICIALLY ADMINISTERED NUTRITION: |
Offer food by mouth if feasible and desired. |
|
|||
|
o |
Additional Orders: |
|
||||
CheckOne |
|
||||||
o Trial period of artiicial nutrition, including feeding tubes. |
|
|
|
|
|||
|
|
|
|
||||
oNo artiicial means of nutrition, including feeding tubes.
DINFORMATION AND SIGNATURES:
Discussed with: |
o Patient (Patient Has Capacity) |
o Legally Recognized Decisionmaker |
|||
|
|
|
|
||
o Advance Directive dated ________, available and reviewed à |
Healthcare Agent if named in Advance Directive: |
||||
o |
Advance Directive not available |
Name: |
|
|
|
o |
No Advance Directive |
Phone: |
|
|
|
Signature of Physician
My signature below indicates to the best of my knowledge that these orders are consistent with the patient’s medical condition and preferences.
Print Physician Name: |
Physician Phone Number: |
Physician License Number: |
|
|
|
Physician Signature: (required) |
|
Date: |
|
|
|
Signature of Patient or Legally Recognized Decisionmaker
I am aware that this form is voluntary. By signing this form, the legally recognized decisionmaker acknowledges that this request regarding resuscitative measures is consistent with the known desires of, and with the best interest of, the patient who is the subject of the form.
|
Print Name: |
|
Relationship: (write self if patient) |
|
|
|
|
|
Signature: (required) |
|
Date: |
|
|
|
|
|
Mailing Address (street/city/state/zip): |
Phone Number: |
Ofice Use Only: |
|
|
|
|
SEND FORM WITH PATIENT WHENEVER TRANSFERRED OR DISCHARGED
*Form versions with effective dates of 1/1/2009 or 4/1/2011 are also valid
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTHCARE PROVIDERS AS NECESSARY
Patient Information
Name (last, irst, middle):
Date of Birth:
Gender:
M F
Healthcare Provider Assisting with Form Preparation |
o N/A if POLST is completed by signing physician |
Name:
Title:
Phone Number:
Additional Contact |
o None |
Name:
Relationship to Patient:
Phone Number:
Directions for Healthcare Provider
Completing POLST
•Completing a POLST form is voluntary. California law requires that a POLST form be followed by healthcare providers, and provides immunity to those who comply in good faith. In the hospital setting, a patient will be assessed by a physician who will issue appropriate orders that are consistent with the patient’s preferences.
•POLST does not replace the Advance Directive. When available, review the Advance Directive and POLST form to ensure consistency, and update forms appropriately to resolve any conlicts.
•POLST must be completed by a healthcare provider based on patient preferences and medical indications.
•A legally recognized decisionmaker may include a
•A legally recognized decisionmaker may execute the POLST form only if the patient lacks capacity or has designated that the decisionmaker’s authority is effective immediately.
•POLST must be signed by a physician and the patient or decisionmaker to be valid. Verbal orders are acceptable with
•If a translated form is used with patient or decisionmaker, attach it to the signed English POLST form.
•Use of original form is strongly encouraged. Photocopies and FAXes of signed POLST forms are legal and valid. A copy should be retained in patient’s medical record, on Ultra Pink paper when possible.
Using POLST
•Any incomplete section of POLST implies full treatment for that section.
Section A:
•If found pulseless and not breathing, no deibrillator (including automated external deibrillators) or chest compressions should be used on a patient who has chosen “Do Not Attempt Resuscitation.”
Section B:
•When comfort cannot be achieved in the current setting, the patient, including someone with
•
•IV antibiotics and hydration generally are not
•Treatment of dehydration prolongs life. If a patient desires IV luids, indicate “Selective Treatment” or “Full Treatment.”
•Depending on local EMS protocol, “Additional Orders” written in Section B may not be implemented by EMS personnel.
Reviewing POLST
It is recommended that POLST be reviewed periodically. Review is recommended when:
•The patient is transferred from one care setting or care level to another, or
•There is a substantial change in the patient’s health status, or
•The patient’s treatment preferences change.
Modifying and Voiding POLST
•A patient with capacity can, at any time, request alternative treatment or revoke a POLST by any means that indicates intent to revoke. It is recommended that revocation be documented by drawing a line through Sections A through D, writing “VOID” in large letters, and signing and dating this line.
•A legally recognized decisionmaker may request to modify the orders, in collaboration with the physician, based on the known desires of the patient or, if unknown, the patient’s best interests.
This form is approved by the California Emergency Medical Services Authority in cooperation with the statewide POLST Task Force.
For more information or a copy of the form, visit www.caPOLST.org.
SEND FORM WITH PATIENT WHENEVER TRANSFERRED OR DISCHARGED
Form Characteristics
| Fact Name | Description |
|---|---|
| What is POLST? | The Physician Orders for Life-Sustaining Treatment (POLST) is a medical order designed to ensure that a patient's treatment preferences are honored in emergency situations and beyond. |
| How Does it Work? | The POLST form outlines specific medical interventions a patient wishes to receive or avoid. Healthcare providers are expected to follow these orders in accordance with California law. |
| Complementary Document | POLST works alongside Advance Directives but does not replace them. Both documents should be consistent and updated periodically. |
| Requirements for Validity | A POLST form must be signed by both a physician and the patient or their legally recognized decision-maker to be valid. Verbal orders can also be accepted with appropriate follow-up documentation. |
| Review and Update | Regularly reviewing the POLST form is essential, especially after significant changes in the patient's health status or care setting to ensure alignment with their current wishes. |
Guidelines on Utilizing Polst
When preparing to fill out the POLST (Physician Orders for Life-Sustaining Treatment) form, it's essential to gather the necessary information and understand the sections of the form. This document allows patients to convey their health care preferences, and it needs to be completed meticulously to ensure clarity in their medical care. The following steps will guide you through the process of filling out the POLST form.
- Start by filling in the Patient’s Last Name and First Name.
- Next, indicate the Patient Date of Birth and, if available, the Patient Middle Name.
- If applicable, include the Medical Record #.
- Move to Section A: Choose either Attempt Resuscitation/CPR or Do Not Attempt Resuscitation/DNR. Note that selecting CPR requires choosing full treatment in Section B.
- In Section B, select the appropriate medical interventions based on the patient’s wishes. Options include:
- Full Treatment
- Trial Period of Full Treatment
- Selective Treatment
- Comfort-Focused Treatment
- In Section C, address Artificially Administered Nutrition by choosing:
- Long-term artificial nutrition
- Trial period of artificial nutrition
- No artificial means of nutrition
- Proceed to the Information and Signatures section. Indicate who discussed the form with the patient, checking one option from:
- Patient (Patient Has Capacity)
- Legally Recognized Decisionmaker
- If there is an Advance Directive, include the date if available.
- Print the Physician’s Name, provide the Physician Phone Number and Physician License Number, and obtain the Physician Signature with the date.
- Obtain the Signature of the Patient or their Legally Recognized Decisionmaker. Include their printed name, relationship, signature, date, mailing address, and phone number.
- Finally, ensure the form is appropriately documented and retained as per the guidelines.
Following these steps carefully ensures that the POLST form reflects the patient’s wishes. Always remember to send a copy of the signed form with the patient whenever they are transferred or discharged to ensure continuity of care.
What You Should Know About This Form
What is a POLST form?
The Physician Orders for Life-Sustaining Treatment (POLST) form is a medical order that outlines a patient's preferences for treatment in emergency medical situations. It aids healthcare providers in making decisions aligned with a patient's wishes, especially when they are unable to communicate. The form must be signed by a physician and the patient or their legally recognized decision-maker to be valid.
How does the POLST work with an Advance Directive?
A POLST form complements, but does not replace, an Advance Directive. While an Advance Directive provides guidance for future healthcare decisions, POLST serves as a clear set of orders for immediate medical treatment based on current preferences. When both documents are available, it is important to ensure they are consistent with one another.
Who should complete the POLST form?
The POLST form is typically completed by a healthcare provider based on the patient's medical condition and preferences. Patients may also include their legally recognized decision-maker if they lack the capacity to make decisions themselves. This could be a spouse, a guardian, or someone familiar with the patient’s wishes.
What happens if a section of the POLST form is left incomplete?
If any section of the POLST form is left blank, it indicates that the patient desires full treatment in that area. For example, if the section regarding medical interventions is incomplete, healthcare providers will proceed with the full range of treatments available to prolong life.
Can a patient change their mind about their POLST preferences?
Yes, a patient who has decision-making capacity can change their preferences at any time. One effective method to revoke a POLST order is to draw a line through each section of the form, write “VOID” across it, and sign and date the document. This updated information should be communicated to healthcare providers promptly.
What should be done if the POLST form is not available during an emergency?
In the absence of a POLST form, doctors and emergency medical personnel will typically rely on the patient's medical history, their Advance Directive, or will make decisions based on what they believe to be in the patient's best interests. It is crucial to ensure that the POLST form, if available, accompanies the patient during transfers or discharges.
How can healthcare providers verify that the POLST form is current?
POLST forms should be reviewed periodically or whenever a patient experiences a significant change in their health status. They should also be reevaluated whenever a patient is transferred to a new care setting. Regular discussions about the patient's treatment preferences are essential in ensuring that the POLST is up to date.
Are copies of the POLST form valid?
Yes, photocopies and FAXed versions of signed POLST forms are legally valid. Whenever possible, however, it is recommended to retain the original document. A copy should always be included in the patient’s medical record to ensure continuity of care.
What is the importance of using the POLST form?
The POLST form plays a vital role in facilitating conversations about end-of-life care preferences. It allows patients to express their wishes clearly and ensures that healthcare providers are prepared to follow those preferences. With this level of documentation, unnecessary treatments can be avoided, and healthcare can be aligned with the patient's goals for comfort and care.
Common mistakes
When filling out the Physician Orders for Life-Sustaining Treatment (POLST) form, clarity and accuracy are crucial. Yet, many individuals make mistakes that can lead to unintended consequences for their healthcare. Understanding these common pitfalls can help you navigate the process more effectively.
One frequent error occurs when individuals assume that an incomplete section implies a specific directive. In fact, any section left blank on the POLST form implies full treatment. This misunderstanding can lead to situations where medical personnel may provide unexpected or unwanted interventions, leaving patients and their families distressed.
Another mistake involves disregarding the necessity for signatures. Both a physician and the patient—or their legally recognized decision-maker—must sign the form for it to be valid. Failing to obtain a signature could render the POLST ineffective, and healthcare providers may default to aggressive interventions, contrary to the patient’s wishes.
Some people overlook the importance of involving a legally recognized decision-maker, especially if the patient lacks capacity. Without proper consultation, the chosen surrogate may not fully understand the patient’s desires. This can result in decisions made that do not align with what the patient would want, complicating their care.
Additionally, individuals often neglect to keep their POLST form updated. As health conditions evolve or treatment preferences change, it’s vital to review and modify the POLST accordingly. A stagnant form may no longer reflect the patient’s current healthcare wishes, which could lead healthcare providers to make inappropriate decisions based on outdated information.
Finally, some individuals mistakenly assume that the POLST form replaces an Advance Directive. While the POLST complements an Advance Directive, it does not replace it. Both documents play different roles in guiding medical decisions. Ensuring consistency between the two forms can prevent conflicts and confusion among healthcare providers, promoting care that honors patient choices.
Documents used along the form
The Physician Orders for Life-Sustaining Treatment (POLST) form serves as a critical document in a patient’s healthcare planning, outlining the specific medical actions that should be taken during emergencies. However, it is important to recognize that the POLST is often utilized in conjunction with other important legal documents. Below are four such documents that complement the POLST in ensuring that a patient’s wishes regarding medical treatment are respected and followed.
- Advance Directive: This document provides clear instructions regarding a person's healthcare preferences in situations where they may not be able to communicate their wishes. It typically includes a living will, which outlines specific medical treatments a person does or does not want, and appoints a healthcare agent to make decisions on their behalf if they are incapacitated.
- Durable Power of Attorney for Healthcare: This form designates a trusted individual to make healthcare decisions on behalf of a patient if they become unable to do so. The appointed agent is empowered to follow the patient's wishes as expressed in the document, thus ensuring that their healthcare preferences are honored during critical times.
- Healthcare Proxy: Similar to the durable power of attorney, this document specifically names a person who can make medical decisions for someone else. The healthcare proxy acts as a representative during times when the patient is unable to communicate directly with healthcare providers, ensuring that their values and preferences guide medical choices.
- Do Not Resuscitate (DNR) Order: This is a specific medical order that indicates that a patient does not wish to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. While elements of this order may be encompassed within the POLST, having a separate DNR can provide additional clarity and immediate recognition of the patient’s wishes in emergencies.
Each of these forms plays an integral role in a comprehensive healthcare planning process. By utilizing them alongside the POLST, patients can ensure that their medical preferences are clearly articulated and respected, ultimately contributing to care that aligns with their values and wishes.
Similar forms
- Advance Directive: This document outlines a person's wishes regarding medical treatment in case they become incapacitated. Similar to a POLST form, it helps ensure that healthcare providers respect the patient's preferences. However, it is generally broader and can cover a wide range of decisions beyond end-of-life care.
- Health Care Proxy: A health care proxy allows someone to make medical decisions on behalf of another person who is unable to do so. Both documents aim to ensure a person’s preferences are honored, but while a POLST form provides specific medical orders, a health care proxy grants decision-making authority to an individual.
- DNR (Do Not Resuscitate) Order: A DNR order specifically instructs healthcare providers not to perform CPR in the event of cardiac arrest. Similar to the POLST, it communicates a patient’s wishes regarding resuscitation efforts but does not provide a comprehensive treatment plan.
- Living Will: A living will is a type of advance directive where a person outlines their wishes regarding medical treatment if they become terminally ill or cannot communicate effectively. Like a POLST form, it emphasizes a patient’s preferences but usually addresses more general scenarios rather than specific medical situations.
- Medical Power of Attorney: This document designates an individual to make medical decisions on someone’s behalf. It complements the POLST by providing a trusted person to advocate for medical care while the POLST specifies treatment preferences.
- Personal Health Record (PHR): A personal health record allows patients to maintain an ongoing record of their medical history and preferences. While the POLST provides actionable medical orders for providers, a PHR serves more as a resource for both patients and their healthcare teams.
- Care Plan: A care plan is a comprehensive document created by healthcare professionals that outlines a patient’s treatment strategies and objectives. While POLST provides specific medical orders based on patient goals, a care plan often includes broader strategies for managing overall health.
- Emergency Medical Services (EMS) Protocols: These protocols guide emergency responders in delivering care quickly and efficiently. Similar to the POLST, these protocols include specific instructions about treatment, but they reflect organizational procedures rather than a patient's individual wishes.
- Patient's Bill of Rights: This document educates individuals about their rights in healthcare settings, ensuring they receive proper care and respect. Both POLST and the Patient’s Bill of Rights center around empowering patients, although the POLST focuses specifically on treatment preferences.
- Medication Order: A medication order provides directives on a patient’s prescription regimen. While it ensures the correct medications are administered, similar to POLST, it does not encompass the broader context of treatment preferences or goals.
Dos and Don'ts
Filling out the POLST form is an important step in ensuring that medical preferences are clearly documented. Here is a guide on what to do and what to avoid in this process.
- Do ensure all patient information is accurate and complete, including names and dates of birth.
- Do discuss the patient's wishes thoroughly with them or their legally recognized decision-maker.
- Do review any existing Advance Directives to ensure consistency with the POLST form.
- Do get the form signed by both the physician and the patient or their decision-maker.
- Don't leave any sections incomplete, as this implies full treatment in those areas.
- Don't use verbal orders unless they will be followed by a written signature as per facility policy.
- Don't forget to keep a copy of the POLST form in the patient’s medical record, especially on Ultra Pink paper if available.
Misconceptions
- POLST is the same as an Advance Directive. This is incorrect. POLST complements an Advance Directive but does not replace it. Both serve different purposes in conveying a patient's wishes.
- POLST forms cannot be altered or revoked. This misconception is false. Patients with capacity can request changes or revoke a POLST at any time, marking the form clearly to indicate intent.
- Healthcare providers can ignore the POLST form. In truth, California law mandates that healthcare providers follow POLST orders. Ignoring them can lead to significant consequences for care.
- A verbal order for POLST is not valid. This is misleading. Verbal orders can be accepted, provided that a physician follows up with a signed confirmation according to facility policy.
- It’s unnecessary to review POLST forms. This is incorrect. POLST forms should be reviewed periodically, especially during transfers or changes in a patient's health status.
- Photocopies of POLST forms are not valid. This is a misconception. Although original forms are preferred, photocopies and faxes of signed POLST forms are legally valid and should be retained in the patient’s medical record.
- PATIENTS must always sign their own POLST forms. In cases where patients lack capacity, a legally recognized decisionmaker can sign on their behalf, provided they understand the patient’s preferences.
Key takeaways
Understanding the Physician Orders for Life-Sustaining Treatment (POLST) form is crucial for patients and their healthcare providers. Here are some key takeaways:
- POLST is a legal document: The POLST form serves as a legally valid physician order that outlines a patient’s preferences for medical treatment. It should include signatures from both a physician and the patient or a legally recognized decision-maker.
- Compliments Advance Directive: While POLST complements an Advance Directive, it does not replace it. Both documents should be reviewed and updated to ensure consistency and respect for the patient’s wishes.
- Incomplete sections imply full treatment: Any section of the POLST form that is not filled out implies that the patient is consenting to full treatment for that section.
- Regular reviews are recommended: It is advisable to periodically review the POLST form, particularly when the patient is transferred to a different care setting or when there is a significant change in the patient's health condition.
Browse Other Templates
Subpoena Form (pdf) - The AO 88B may also facilitate negotiations between parties regarding the scope of the requests.
Periodic Table Khan Academy - Identifying the trends requires careful analysis and promotes collaboration among students through discussion.
Va Form 28-1900 - The VA 28 form is crucial for veterans seeking financial assistance while pursuing vocational rehabilitation.