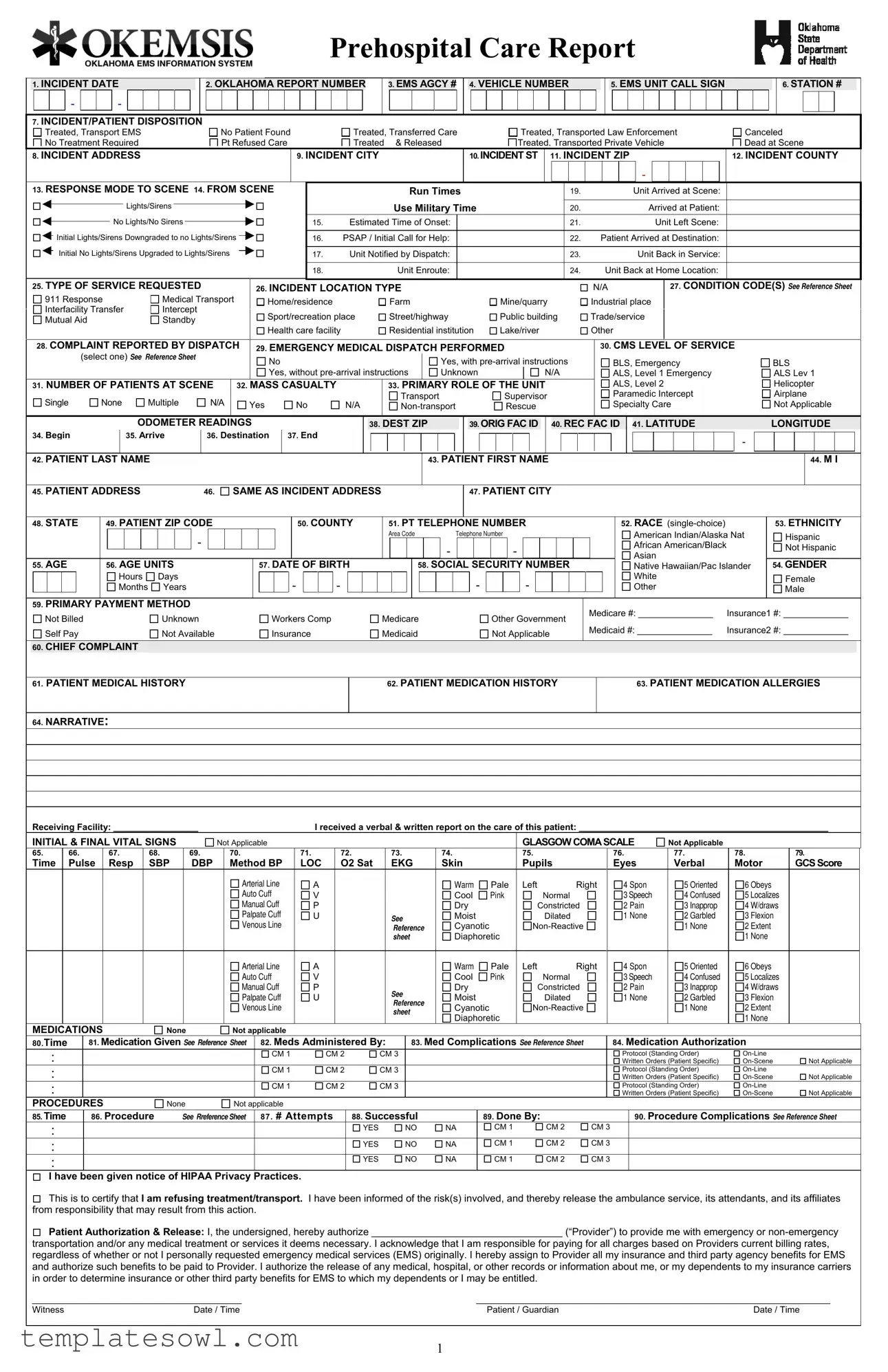
Fill Out Your Prehospital Care Report Form
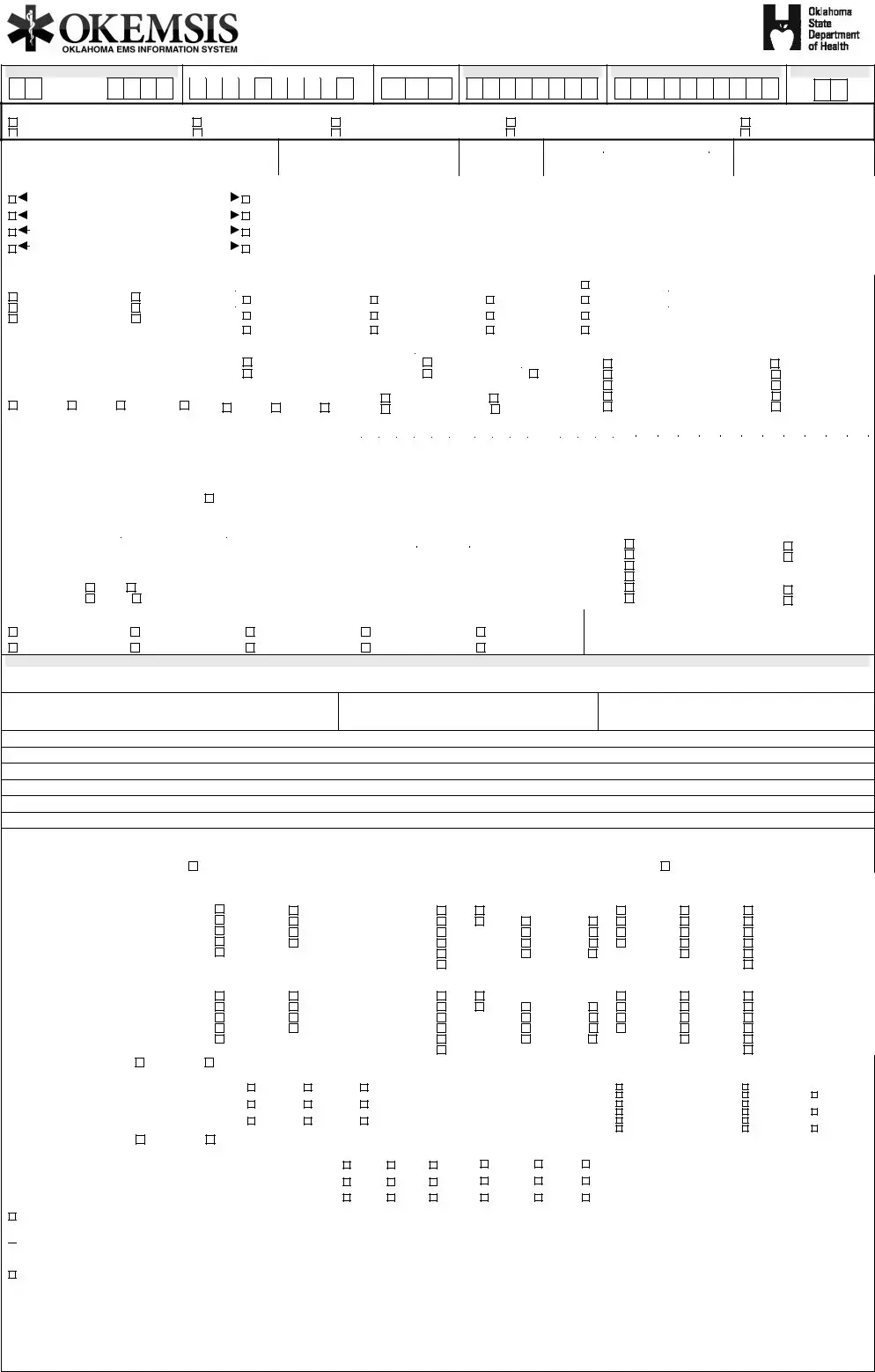
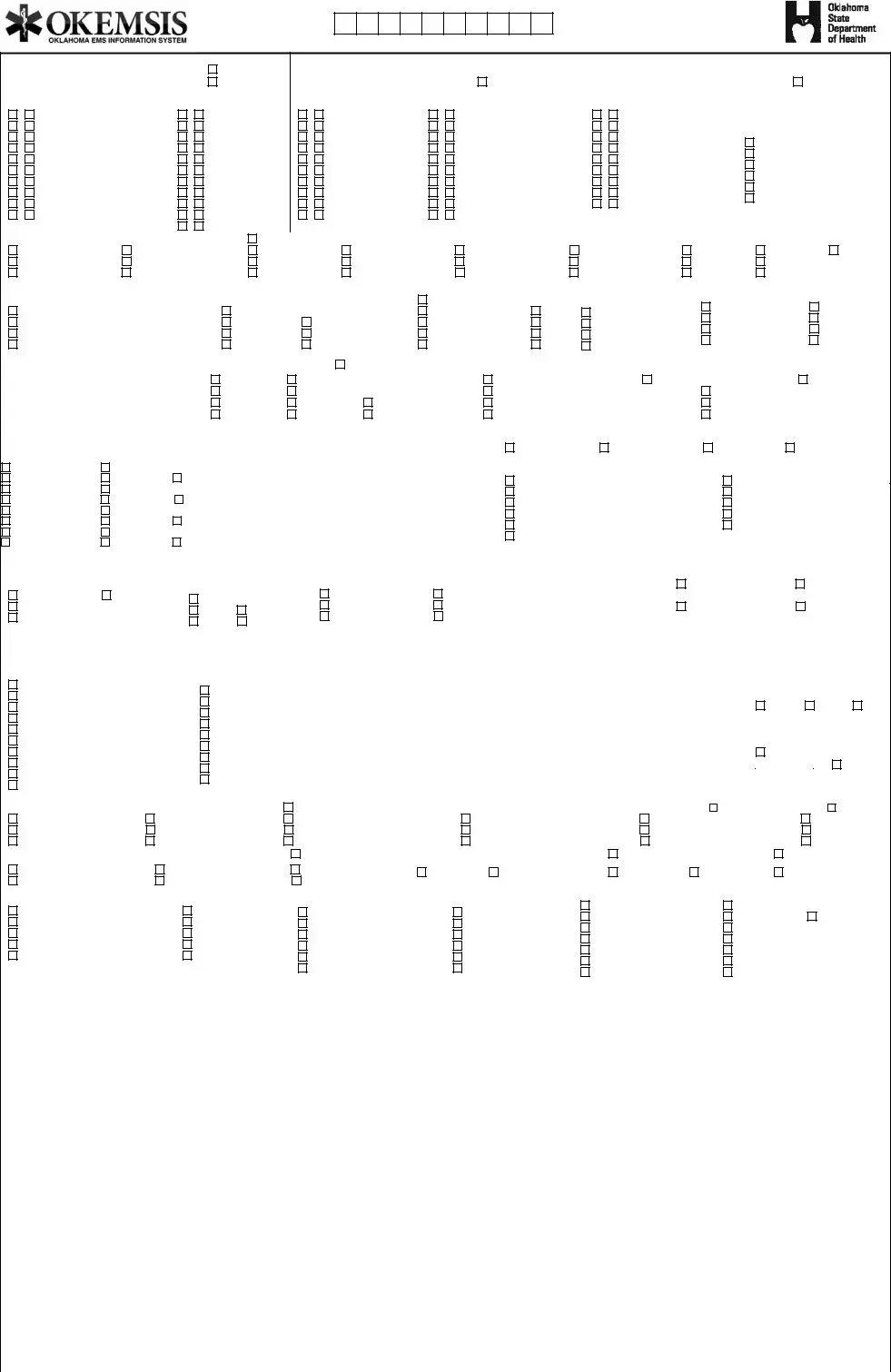
The Prehospital Care Report (PCR) form is a crucial document utilized by Emergency Medical Services (EMS) to capture essential data during emergency medical responses. This comprehensive form includes fields for key information like the incident date, report number, vehicle identification, and details about the EMS agency involved. The form helps track the disposition of the patient, whether they were treated and transported, refused care, or were pronounced dead at the scene. It collects critical incident details such as the location, response modes, and run times for better situational awareness. Furthermore, it documents patient demographics, medical history, and vital signs during the response, ensuring continuity of care once the patient reaches a medical facility. Additional sections address medications administered, procedures performed, and the crew members involved, fostering excellent accountability and organization within healthcare teams. By systematically gathering this information, the PCR form plays a vital role in maintaining high-quality emergency medical services and is instrumental for subsequent analysis and quality assurance in the field.
Prehospital Care Report Example
Prehospital Care Report
1.INCIDENT DATE
- |
|
|
- |
2.OKLAHOMA REPORT NUMBER
3.EMS AGCY #
4.VEHICLE NUMBER
5.EMS UNIT CALL SIGN
6.STATION #
7.INCIDENT/PATIENT DISPOSITION
Treated, Transport EMS
No Treatment Required
No Patient Found Pt Refused Care
Treated, Transferred Care Treated & Released
Treated, Transported Law Enforcement Treated, Transported Private Vehicle
Canceled Dead at Scene
8. INCIDENT ADDRESS |
9. INCIDENT CITY |
10. INCIDENT ST 11. INCIDENT ZIP |
12. INCIDENT COUNTY |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
13. RESPONSE MODE TO SCENE 14. FROM SCENE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Run Times |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
19. |
|
|
|
|
|
|
|
|
|
Unit Arrived at Scene: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Lights/Sirens |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Use Military Time |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20. |
|
|
|
|
|
|
|
|
|
|
Arrived at Patient: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
No Lights/No Sirens |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
15. |
|
|
Estimated Time of Onset: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21. |
|
|
|
|
|
|
|
|
|
|
|
Unit Left Scene: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
Initial Lights/Sirens Downgraded to no Lights/Sirens |
|
|
|
|
|
|
|
|
|
|
|
|
16. PSAP / Initial Call for Help: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
22. Patient Arrived at Destination: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unit Notified by Dispatch: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unit Back in Service: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
Initial No Lights/Sirens Upgraded to Lights/Sirens |
|
|
|
|
|
|
|
|
|
|
|
|
17. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
23. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18. |
|
|
|
|
|
|
|
|
|
Unit Enroute: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
24. |
|
|
|
Unit Back at Home Location: |
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
25. TYPE OF SERVICE REQUESTED |
|
|
|
|
|
|
|
|
|
26. INCIDENT LOCATION TYPE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
N/A |
|
|
|
|
|
|
27. CONDITION CODE(S) SEE REFERENCE SHEET |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
911 Response |
|
|
Medical Transport |
|
|
|
|
|
|
Home/residence |
|
|
|
|
|
|
|
Farm |
|
|
|
|
|
|
|
|
|
|
|
Mine/quarry |
|
|
|
|
Industrial place |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Interfacility Transfer |
|
|
Intercept |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Sport/recreation place |
|
Street/highway |
Public building |
|
|
|
|
Trade/service |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Mutual Aid |
|
|
Standby |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Health care facility |
|
Residential institution |
Lake/river |
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
28. COMPLAINT REPORTED BY DISPATCH |
|
29. EMERGENCY MEDICAL DISPATCH PERFORMED |
|
|
|
|
|
30. CMS LEVEL OF SERVICE |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
(select one) SEE REFERENCE SHEET |
|
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes, with |
|
|
|
|
|
|
|
BLS, Emergency |
|
BLS |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes, without |
|
|
|
Unknown |
|
|
|
|
|
|
|
|
N/A |
|
|
|
|
|
|
|
ALS, Level 1 Emergency |
|
ALS Lev 1 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
31. NUMBER OF PATIENTS AT SCENE |
|
32. MASS CASUALTY |
|
|
|
|
|
|
|
33. PRIMARY ROLE OF THE UNIT |
|
|
|
|
|
|
|
ALS, Level 2 |
|
Helicopter |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Transport |
|
Supervisor |
|
|
|
|
|
|
|
Paramedic Intercept |
|
|
Airplane |
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Single |
|
None |
|
Multiple |
|
N/A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Specialty Care |
|
Not Applicable |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
Yes |
|
|
No |
N/A |
|
|
|
Rescue |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
ODOMETER READINGS |
|
|
|
|
|
|
|
|
|
|
|
|
|
38. DEST ZIP |
|
|
|
|
|
|
39. ORIG FAC ID |
|
|
40. REC FAC ID |
|
|
41. LATITUDE |
|
LONGITUDE |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
34. Begin |
|
|
|
|
|
35. Arrive |
|
36. Destination |
37. End |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
42. PATIENT LAST NAME |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
43. PATIENT FIRST NAME |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
44. M I |
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
45. PATIENT ADDRESS |
|
|
|
|
|
|
46. SAME AS INCIDENT ADDRESS |
|
|
|
|
|
|
|
|
|
|
|
|
|
47. PATIENT CITY |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
48. STATE |
|
49. PATIENT ZIP CODE |
|
|
|
|
|
|
|
|
|
|
50. COUNTY |
|
51. PT TELEPHONE NUMBER |
|
|
|
|
|
|
|
|
|
|
52. RACE |
|
|
53. ETHNICITY |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Area Code |
|
|
|
Telephone Number |
|
|
|
|
|
|
|
|
|
|
|
|
American Indian/Alaska Nat |
|
|
Hispanic |
|||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
African American/Black |
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not Hispanic |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Asian |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
55. AGE |
|
56. AGE UNITS |
|
|
|
|
|
|
|
|
|
|
57. DATE OF BIRTH |
|
|
|
|
|
58. SOCIAL SECURITY NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
Native Hawaiian/Pac Islander |
|
54. GENDER |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
Hours |
Days |
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
White |
|
|
Female |
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
Months |
Years |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other |
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Male |
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
59.PRIMARY PAYMENT METHOD
Not Billed |
Unknown |
Self Pay |
Not Available |
Workers Comp
Insurance
Medicare
Medicaid
Other Government
Not Applicable
Medicare #: _______________ |
Insurance1 #: _____________ |
Medicaid #: _______________ |
Insurance2 #: _____________ |
60.CHIEF COMPLAINT
61.PATIENT MEDICAL HISTORY
62.PATIENT MEDICATION HISTORY
63.PATIENT MEDICATION ALLERGIES
64.NARRATIVE:
Receiving Facility: _________________I received a verbal & written report on the care of this patient: __________________________________________________
INITIAL & FINAL VITAL SIGNS |
|
Not Applicable |
|
|
|
|
|
|
|
|
|
|
GLASGOW COMASCALE |
Not Applicable |
|
|
|||||||||||||
65. |
|
66. |
|
|
67. |
68. |
69. |
|
70. |
|
71. |
72. |
|
|
73. |
|
74. |
|
|
75. |
|
|
|
76. |
|
77. |
78. |
79. |
|
Time |
|
Pulse |
|
Resp |
SBP |
DBP |
|
Method BP |
LOC |
O2 Sat |
|
|
EKG |
Skin |
|
Pupils |
|
|
Eyes |
Verbal |
Motor |
GCS Score |
|||||||
|
|
|
|
|
|
|
|
|
Arterial Line |
A |
|
|
|
|
|
|
Warm |
Pale |
Left |
Right |
|
4 Spon |
5 Oriented |
6 Obeys |
|
||||
|
|
|
|
|
|
|
|
|
Auto Cuff |
V |
|
|
|
|
|
|
Cool |
Pink |
|
Normal |
|
|
3 Speech |
4 Confused |
5 Localizes |
|
|||
|
|
|
|
|
|
|
|
|
Manual Cuff |
P |
|
|
|
|
|
|
Dry |
|
|
Constricted |
|
|
2 Pain |
3 Inapprop |
4 W/draws |
|
|||
|
|
|
|
|
|
|
|
|
Palpate Cuff |
U |
|
|
|
|
SEE |
Moist |
|
|
Dilated |
|
|
1 None |
2 Garbled |
3 Flexion |
|
||||
|
|
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
|
REFERENCE |
Cyanotic |
|
|
|
|
|
1 None |
2 Extent |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SHEET |
Diaphoretic |
|
|
|
|
|
|
|
1 None |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Arterial Line |
A |
|
|
|
|
|
|
Warm |
Pale |
Left |
Right |
|
4 Spon |
5 Oriented |
6 Obeys |
|
||||
|
|
|
|
|
|
|
|
|
Auto Cuff |
V |
|
|
|
|
|
|
Cool |
Pink |
|
Normal |
|
|
3 Speech |
4 Confused |
5 Localizes |
|
|||
|
|
|
|
|
|
|
|
|
Manual Cuff |
P |
|
|
|
|
SEE |
Dry |
|
|
Constricted |
|
|
2 Pain |
3 Inapprop |
4 W/draws |
|
||||
|
|
|
|
|
|
|
|
|
Palpate Cuff |
U |
|
|
|
|
Moist |
|
|
Dilated |
|
|
1 None |
2 Garbled |
3 Flexion |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
REFERENCE |
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
|
Cyanotic |
|
|
|
|
|
1 None |
2 Extent |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SHEET |
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diaphoretic |
|
|
|
|
|
|
|
1 None |
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
MEDICATIONS |
|
None |
|
Not applicable |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
80.Time |
|
81. Medication Given SEE REFERENCE SHEET |
82. Meds Administered By: |
|
83. Med Complications SEE REFERENCE SHEET |
|
|
84. Medication Authorization |
|
||||||||||||||||||||
: |
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not Applicable |
||||
: |
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not Applicable |
||||
: |
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not Applicable |
||||
PROCEDURES |
|
None |
|
Not applicable |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
85. Time |
|
86. Procedure |
SEE RREFERENCE SHEET |
87. # Attempts |
|
88. Successful |
|
89. Done By: |
|
|
|
90. Procedure Complications SEE REFERENCE SHEET |
|||||||||||||||||
: |
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|
|
|
NO |
NA |
|
CM 1 |
|
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
: |
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|
|
|
NO |
NA |
|
CM 1 |
|
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
: |
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|
|
|
NO |
NA |
|
CM 1 |
|
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I have been given notice of HIPAA Privacy Practices. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||

 This is to certify that I am refusing treatment/transport. I have been informed of the risk(s) involved, and thereby release the ambulance service, its attendants, and its affiliates from responsibility that may result from this action.
This is to certify that I am refusing treatment/transport. I have been informed of the risk(s) involved, and thereby release the ambulance service, its attendants, and its affiliates from responsibility that may result from this action.
Patient Authorization & Release: I, the undersigned, hereby authorize __________________________________ (“Provider”) to provide me with emergency or
transportation and/or any medical treatment or services it deems necessary. I acknowledge that I am responsible for paying for all charges based on Providers current billing rates, regardless of whether or not I personally requested emergency medical services (EMS) originally. I hereby assign to Provider all my insurance and third party agency benefits for EMS and authorize such benefits to be paid to Provider. I authorize the release of any medical, hospital, or other records or information about me, or my dependents to my insurance carriers in order to determine insurance or other third party benefits for EMS to which my dependents or I may be entitled.
__________________________________________ |
_______________________________________________________________________ |
||
Witness |
Date / Time |
Patient / Guardian |
Date / Time |
1
Prehospital Care Report Number:
SYMPTOMS 91. P=PRIMARY (pick one) |
Not applicable |
|
|
92. A =ASSOCIATED (multi) |
Not applicable |
P A |
P A |
|
|
Transport Only |
Fever |
|
None |
Malaise |
|
Bleeding |
Mass/Lesion |
|
Breathing |
Mental/Psych |
|
Changes in Responsiveness |
Nausea/Vomiting |
|
Choking |
Pain |
|
Death |
Palpitations |
|
Device/Equip Problem |
Rash/Itching |
|
Diarrhea |
Swelling |
|
Drainage/Discharge |
Weakness |
|
|
Wound |
PROVIDER IMPRESSION
93. P= PRIMARY (pick one)
P SP S
Abdominal pain
Airway obstruct
Allergic reaction
Altered LOC
Behavior/psych
Cardiac arrest
Cardiac arrhythmia
Chest pain
CHF COPD
Not applicable |
94. S=SECONDARY (pick one) |
Not applicable |
||
P |
S |
|
|
|
|
|
|||
Diabetic |
Respiratory arrest |
95. ALCOHOL/DRUG USE |
||
Electrocution |
Respiratory distress |
INDICATORS |
||
Hyperthermia |
Seizure |
|
Not applicable |
|
Hypothermia |
Sexual assault/rape |
|
||
|
None |
|||
Hypovolemia/shock |
Stings/venomous bites |
|
||
|
Smell of alcohol present |
|||
Inhalation injury/toxic gas |
Stroke/CVA |
|
||
|
Pt admits to alcohol use |
|||
Inhalation/smoke |
Syncope/fainting |
|
||
|
Pt admits to drug use |
|||
Obvious Death |
Traumatic injury |
|
||
|
Alcohol and/or drug |
|||
Poisoning/drug OD |
Vaginal hemorrhage |
|
||
paraphernalia at scene |
||||
Pregnancy/OB delivery |
|
|||
|
|
|
||
|
|
|
|
|
|
96. CHIEF COMPLAINT ANATOMIC LOCATION |
Not applicable |
|
97. CHIEF COMPLAINT ORGAN SYSTEM |
|
|
|
|
|
|
|
|
|
|
|
98. Incident |
|||||||||||||||||||||||||||||||
|
Abdomen |
|
Extremity Lower |
|
|
Genitalia |
|
|
|
|
|
Not applicable |
Endocrine/Metabolic |
Musculoskeletal |
|
|
|
Pulmonary |
|
|
Yes |
|
|
No |
|||||||||||||||||||||||
|
Back |
|
Extremity Upper |
|
|
Head |
|
|
|
|
|
Cardiovascular |
GI |
|
|
|
OB/GYN |
|
|
|
Renal |
|
|
Unknown |
|
|
|||||||||||||||||||||
|
Chest |
|
General/Global |
|
|
Neck |
|
|
|
|
|
CNS/Neuro |
Global |
|
|
|
Psych |
|
|
|
Skin |
|
|
Not applicable |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
99. CARDIAC ARREST |
|
|
|
100. RESUSCITATION (multi) |
|
|
101. TIME OF ARREST (mins) |
|
102. ARREST |
|
|
|
103. CAUSE OF ARREST |
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not applicable |
|
|
|
WITNESSED BY: |
|
Not applicable |
|
Drowning |
||||||||||||||||
|
Not applicable |
|
|
|
|
|
|
Not applicable |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not applicable |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unknown |
|
Respiratory |
|||||||||||||||||||
|
Yes, Prior to Arrival |
|
|
|
|
|
Defibrillation |
|
|
|
|
|
|
|
|
|
|
|
|
Lay Person |
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Presumed Cardiac |
|
Electrocution |
||||||||||||||||||||||||
|
Yes, After Arrival |
|
|
|
|
|
|
Ventilation |
|
|
|
|
|
|
|
|
|
|
|
|
Healthcare Provider |
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Trauma |
|
|
|
Other |
|||||||||||||||||||||||
|
No |
|
|
|
|
|
|
Chest Comp |
|
|
|
|
|
|
|
|
>20 |
|
|
|
Not Witnessed |
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
STEMI |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not applicable |
|
108. Stroke Scale |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
104. |
|
|
|
Yes |
|
|
|
No |
|
|
|
|
|
|
|
|
|
Not applicable |
|
|
Not available |
|
|
Not known |
||||||||||||||||||||||
105. |
Transmitted for interpretation: |
|
Yes |
|
|
|
No |
|
|
|
|
|
|
|
|
|
Cincinnati Stroke Scale Negative |
|
|
|
|
LA Stroke Scale Negative |
|||||||||||||||||||||||||
106. |
Interpreter (indicate all): |
|
|
|
Paramedic |
|
Physician |
Computer Program |
|
|
Cincinnati Stroke Scale |
|
|
LA Stroke Scale |
|||||||||||||||||||||||||||||||||
107. |
STEMI probable: |
|
|
|
|
Yes |
|
|
|
No |
|
Inconclusive |
|
|
Cincinnati Stroke Scale Positive |
|
|
|
|
LA Stroke Scale Positive |
|||||||||||||||||||||||||||
|
PRIOR AID RECEIVED PRIOR TO ARRIVAL OF UNIT See Reference Sheet |
|
|
|
|
|
|
|
111. OUTCOME OF PRIOR AID |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
109. PRIOR AID PERFORMED BY: |
|
|
110. PRIOR AID (Use PROCEDURES |
|
|
Improved |
|
|
Unchanged |
|
|
Worse |
|
|
Unknown |
|||||||||||||||||||||||||||||||
|
|
|
List and/or MEDICATIONS List) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
EMS Provider |
|
Other Health Care Provider |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
112. BARRIERS TO EFFECTIVE CARE |
|
|
|
|
||||||||||||||||||||||
|
Law Enforcement |
|
Lay Person |
|
Unknown |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not applicable |
|
|
|
|
|
|
|
Physically Impaired |
|
|
||||||||||||||
|
EMS Provider |
|
Other Health Care Provider |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Developmentally Impaired |
|
|
|
|
Physically Restrained |
|
|
|||||||||||||||||||
|
Law Enforcement |
|
Lay Person |
|
Unknown |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unattended/Unsupervised |
|
|
|
|
Speech Impaired |
|
|
||||||||||||||||||||
|
EMS Provider |
|
Other Health Care Provider |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hearing Impaired |
|
|
|
|
Unconscious |
|
|
|
|
|||||||||||||||||||
|
Law Enforcement |
|
Lay Person |
|
Unknown |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Language |
|
|
|
|
|
|
|
None |
|
|
|
|
|||||||||||||||
|
EMS Provider |
|
Other Health Care Provider |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unattended or unsupervised (including minors) |
|
|
|
|
|
|
||||||||||||||||||||||
|
Law Enforcement |
|
Lay Person |
|
Unknown |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
113. TRAUMA |
|
114. CAUSE |
|
115. MECHANISM OF |
|
|
|
116. HOSPITAL TEAM NOTIFIED |
|
117. TIME HOSPITAL |
|
118. Trauma Triage Level |
|
|
|
|
||||||||||||||||||||||||||||||
|
PRESENT |
|
OF INJURY |
|
INJURY |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TEAM NOTIFIED |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not applicable |
|
|
Priority 2 |
|||||||
|
Not applicable |
|
|
Not applicable |
Not applicable |
|
|
|
Not applicable |
|
|
|
Trauma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
Yes |
|
|
|
|
|
|
|
|
Yes |
|
|
|
|
Stroke |
|
|
|
|
|
|
|
|
|
Priority 1 |
|
|
Priority 3 |
|||||||||||||||||||
|
|
|
|
|
|
Blunt |
Penetrating |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
No |
|
|
|
|
|
|
|
No |
|
|
|
|
STEMI |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
Burn |
Not Known |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
_______________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
________________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
See Ref. Sheet |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
119. TRAUMA TRIAGE CRITERIA |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Intercept: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
124. TRAUMA REFERRAL |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CENTER (TreC) |
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Not applicable |
|
|
|
|
|
Flail chest |
|
|
|
|
|
|
|
|
|
|
120.TIME REQUESTED: |
|
|
121.TIME ARRIVED: |
|
|
NOTIFIED |
|
|
|||||||||||||||||||||
|
GCS <=13 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
Two or more proximal long bone fractures |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
GCS improving |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
No |
N/A |
||||||||||||||
|
|
|
|
|
|
Open or depressed skull fracture |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
Resp compromise resulting from trauma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
Unstable pelvis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
125.TreC |
|
|
126. TIME |
|||||||||||||
|
Hemodynamic compromise from trauma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
PTS <= 8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
Blunt trauma/no hemodynamic trauma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TRACKING#: |
TReC |
|||||||||||||
|
|
BSA >= 10% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
Penetrating injury to |
|
|
|
|
|
|
|
|
|
|
|
122.TIME OF CARE TRANSFER: |
|
|
123.REC AGENCY: |
|
|
N/A |
|
|
NOTIFIED: |
|||||||||||||||||||||||||
|
|
BSA < 10% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
Penetrating injuries to extremities |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
N/A |
|||||||||||
|
|
Other single system injury |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
Amputation proximal to wrist or ankle |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
Minor injuries |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
Paralysis resulting from trauma |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
127. VEHICULAR INJURY INDICATORS |
|
|
|
|
Not applicable |
|
|
|
|
128. USE OF SAFETY EQUIPMENT [multi] |
|
|
Not applicable |
|
|
None |
||||||||||||||||||||||||||||||
|
Dash Deformity |
|
|
Fire |
|
|
|
|
|
Space Intrusion >1 foot |
|
|
|
|
|
Child Restraint |
|
|
Lap Belt |
|
|
|
|
|
|
|
|
Protective Gear |
|||||||||||||||||||
|
DOA Same Vehicle |
|
Rollover/Roof Deformity |
Windshield Spider/Star |
|
|
|
|
|
Eye Protection |
|
|
Pers Flotation Device |
|
|
|
Shoulder Belt |
||||||||||||||||||||||||||||||
|
Ejection |
|
|
Side Post Deformity |
|
|
Steering Wheel Deformity |
|
Helmet Worn |
|
|
Protective Clothing |
|
|
|
Other (Airbag) |
|||||||||||||||||||||||||||||||
|
129. AIRBAG DEPLOYMENT |
|
|
|
|
|
|
|
|
|
Not applicable |
|
130. PATIENT POSITION |
|
|
Not applicable |
|
|
|
|
|
|
Unknown |
|
|
||||||||||||||||||||||
|
Airbag Deployed Front |
|
Airbag Deployed Other |
|
No Airbag Present |
|
|
|
Driver |
|
|
Left |
|
|
Middle |
|
|
|
Right |
|
Other |
|
|
||||||||||||||||||||||||
|
Airbag Deployed Side |
|
Airbag Not Deployed |
|
|
Unknown |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
131. TYPE OF DESTINATION |
|
|
|
|
|
|
|
132. REASON FOR CHOOSING DESTINATION |
|
133. ED DISPOSITION |
|
|
134. HOSPITAL DISPOSITION |
|||||||||||||||||||||||||||||||||
|
Home |
|
|
|
|
Hospital |
|
|
|
|
Closest |
|
|
|
|
|
|
|
|
|
|
|
|
|
Death |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discharge |
|
Not applicable |
||||||||||||||||||||||||
|
Medical Office/Clinic |
|
|
|
Morgue |
|
|
|
|
Diversion |
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Death |
|
|
|
|
|
|
|||||||||||||||||||||||
|
Nursing Home |
|
|
|
|
Other EMS (air) |
|
|
|
Family Choice |
|
|
|
|
|
Pt Choice |
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Not Applicable |
|
|
|
|
||||||||||||||||||||||||||
|
Other EMS (ground) |
|
|
|
Police/Jail |
|
|
|
|
Insurance |
|
|
|
|
|
|
Pt Physician’s Choice |
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Released |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
Other |
|
|
|
|
Not applicable |
|
|
|
Law Enforcement Choice |
Protocol |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Transferred |
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Specialty Resource Center |
Not applicable |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unknown |
|
|
|
|
Unknown |
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
135. TYPE OF DELAY(S) |
136. TYPE OF DELAY(S) |
|
137. TYPE OF DELAY(S) |
|
138. TYPE OF DELAY(S) |
|
|
139. TYPE OF DELAY(S) (select all) |
||||||||||||||||||||||||||||||||||||||
|
(select all) |
|
|
(select all) |
|
|
|
|
SCENE (select all) |
|
|
|
|
|
|
TRANSPORT (select all) |
|
|
RETURN |
|
|
|
|
|
|
||||||||||||||||||||||
|
DISPATCHER |
|
|
RESPONSE |
|
|
|
|
Not applicable |
|
|
|
|
|
|
|
Not applicable |
|
|
|
|
|
|
Not applicable |
|
|
|
|
|||||||||||||||||||
|
Not applicable |
|
|
|
Not applicable |
|
|
|
|
None |
|
|
|
|
|
|
|
|
|
None |
|
|
|
|
|
|
None |
|
|
|
|
|
|
||||||||||||||
|
None |
|
|
|
None |
|
|
|
|
|
|
Crowd |
|
|
|
|
|
|
|
|
|
Crowd |
|
|
|
|
|
|
Clean up |
|
|
|
|
|
|
||||||||||||
|
Caller Uncooperative |
|
|
Crowd |
|
|
|
|
|
|
Directions |
|
|
|
|
|
|
|
|
Directions |
|
|
|
|
|
|
Decontamination |
|
|
|
|
||||||||||||||||
|
High Call Volume |
|
|
|
Directions |
|
|
|
|
|
|
Distance |
|
|
|
|
|
|
|
|
Distance |
|
|
|
|
|
|
Documentation |
|
|
|
|
|||||||||||||||
|
Language Barrier |
|
|
|
Distance |
|
|
|
|
|
|
Diversion |
|
|
|
|
|
|
|
|
Diversion |
|
|
|
|
|
|
ED Overcrowding |
|
|
|
|
|||||||||||||||
|
Location (Inability to obtain) |
|
Diversion |
|
|
|
|
|
|
Extrication>20 Min |
|
|
|
|
|
|
|
HazMat |
|
|
|
|
|
|
Equipment Failure |
|
|
|
|
||||||||||||||||||
|
No Unit Available |
|
|
|
HazMat |
|
|
|
|
|
|
HazMat |
|
|
|
|
|
|
|
|
Safety Conditions |
|
|
|
Equipment Replenishment |
|
|
||||||||||||||||||||
|
Safety Conditions |
|
|
|
Safety Conditions |
|
|
|
|
Language Barrier |
|
|
|
|
|
|
|
Staff Delay |
|
|
|
|
|
|
Staff Delay |
|
|
|
|
|
|
||||||||||||||||
|
Technical Failure |
|
|
|
Staff Delay |
|
|
|
|
Safety Conditions |
|
|
|
|
|
|
|
Traffic |
|
|
|
|
|
|
Vehicle Failure |
|
|
|
|
||||||||||||||||||
|
Other |
|
|
|
Traffic |
|
|
|
|
|
|
Staff Delay |
|
|
|
|
|
|
|
Vehicle Crash |
|
|
|
|
|
|
Other |
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
Vehicle Crash |
|
|
|
|
Traffic |
|
|
|
|
|
|
|
|
|
Vehicle Failure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
Vehicle Failure |
|
|
|
|
Vehicle Crash |
|
|
|
|
|
|
|
Weather |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
Weather |
|
|
|
|
|
|
Vehicle Failure |
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
Weather |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
Enter CREW MEMBER Information for: |
140. CREW MEMBER ID NUMBER |
141. LEVEL OF SERVICE |
142. CREW MEMBER ROLE |
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
CREW MEMBER 1 ID NUMBER |
|
|
|
|
|
|
|
CREW MEMBER 2 ID NUMBER |
|
|
|
|
|
|
|
|
|
CREW MEMBER 3 ID NUMBER |
|
|
|
|
||||||||||||||||||||||||
____________________________________________________________ |
|
|
|
____________________________________________________________ |
|
|
|
____________________________________________________________ |
|
||||||||||||||||||||||||||||||||||||||
|
Crew Member1 Signature |
|
|
|
|
|
|
|
|
|
|
|
Crew Member2 Signature |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Crew Member3 Signature |
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
Ο B |
Ο I Ο P Ο EMR |
Ο Physician |
|
Ο Nurse Ο Student Ο Other |
|
|
Ο B Ο I |
Ο P |
Ο EMR |
Ο Physician Ο Nurse Ο Student Ο Other |
|
|
Ο B Ο I Ο P |
Ο EMR |
|
Ο Physician |
Ο Nurse Ο Student Ο Other |
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
CREW MEMBER 1 ROLE |
|
|
|
|
|
|
|
|
|
CREW MEMBER 2 ROLE |
|
|
|
|
|
|
|
|
|
CREW MEMBER 3 ROLE |
|
|
|
|
|
|
||||||||||||||||||||
|
Primary Patient Caregiver |
|
|
|
|
Driver |
|
|
|
Primary Patient Caregiver |
|
|
|
|
Driver |
|
|
Primary Patient Caregiver |
|
|
|
|
Driver |
||||||||||||||||||||||||
|
Secondary Patient Caregiver |
|
|
|
|
Other |
|
|
|
Secondary Patient Caregiver |
|
|
|
|
Other |
|
|
Secondary Patient Caregiver |
|
|
|
|
Other |
||||||||||||||||||||||||
|
Third Patient Caregiver |
|
|
|
|
|
|
|
|
|
|
Third Patient Caregiver |
|
|
|
|
|
|
|
|
|
Third Patient Caregiver |
|
|
|
|
|
|
|||||||||||||||||||
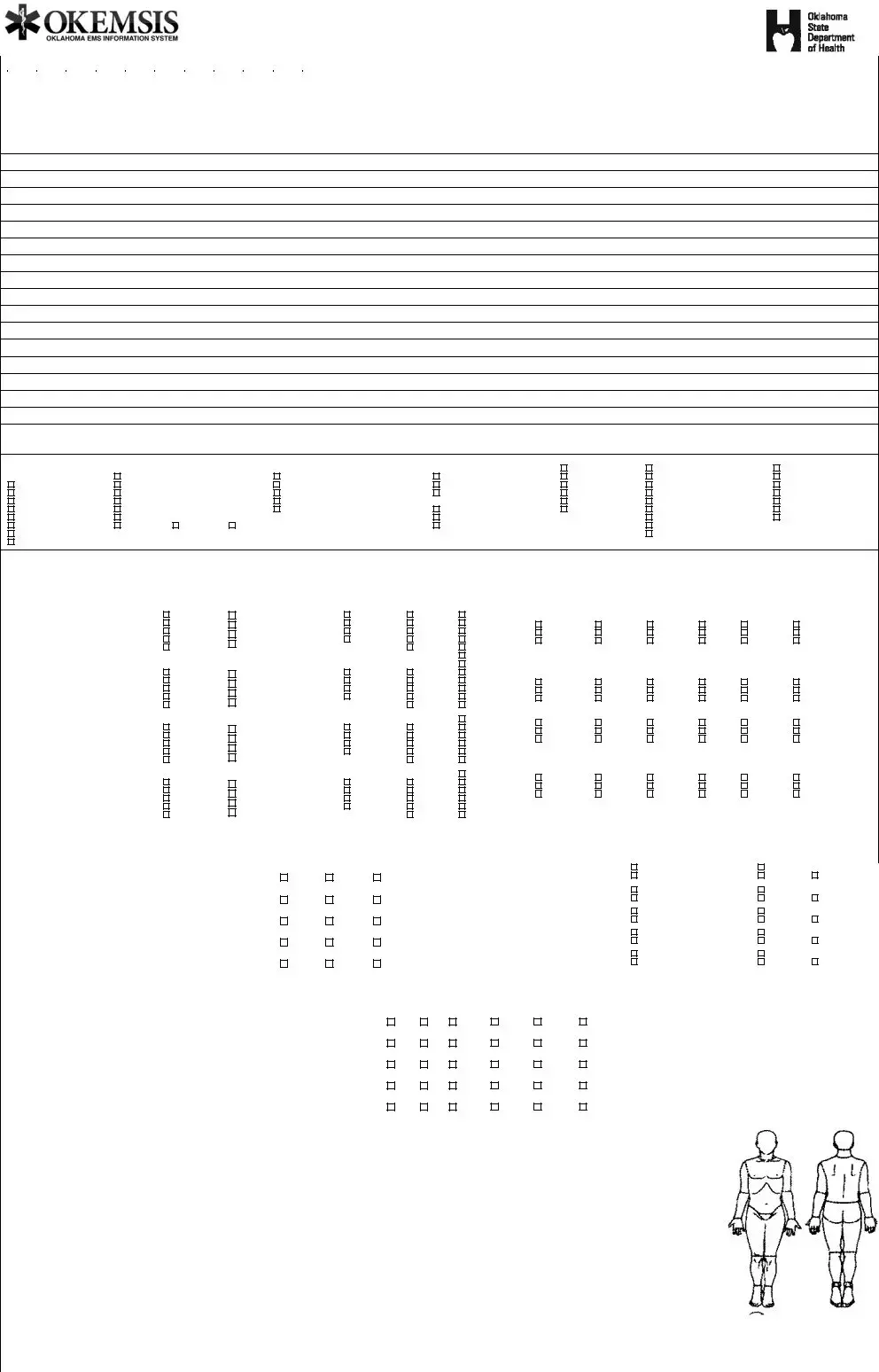
Prehospital Care Report
SUPPLEMENTAL PAGE
|
Oklahoma Report Number from 1st page: |
|
|
PATIENT LAST NAME from 1st page: |
|
|
INCIDENT DATE from 1st page: |
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional PATIENT MEDICAL HISTORY from 1st page: |
Additional PATIENT MEDICATION HISTORY from 1st page: |
Additional PATIENT ALLERGIES from 1st page: |
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional NARRATIVE from 1st page:
Report Given to: _____________________________________; Narrative page ___ of ___ pages
Necessity For Service |
|
|
|
Patient moved to |
Was patient |
Did patient require |
Patient placed in |
Upon arrival, Patient |
Was stretcher necessary? |
|
Stretcher via |
Incontinent |
IV |
Ambulating |
|
Found in: |
Unable to sit upright |
MI |
Total lift |
Combative |
Saline hep lock |
Geri Cardiac Chair |
|
Ambulating |
Unable to balance in sitting position |
Unset or poss fracture |
Draw sheet |
Confused/lethargic |
Drug therapy |
Recliner |
|
Geri Cardiac Chair |
Unconscious/shock |
Acute stroke |
Other _________ |
Dizzy |
Oxygen |
Wheelchair |
|
Recliner |
Req. physical restraints |
MVC |
Did patient |
Weak |
Intubation |
Bed |
|
Wheelchair |
Severe hemorrhage |
Other _________ |
Vomit |
Other _______ |
Ventilator |
Gurn/exam table |
|
Bed |
Bed Confined |
|
|
Complain of nausea |
|
EKG monitor |
Other _____ |
Gurney/exam table |
Fetal position |
Contractures |
Paralyzed |
Complain of pain |
|
Chemstrip |
|
Floor |
|
|
|
|
|
Other ______ |
|
Other _________ |
|
|
|
|
|
|
|
|
Additional VITAL SIGNS & Glasgow Coma Scale from 1st page: |
Glasgow Coma Scale |
|
|
|
|
Pediatric Trauma Score: |
Age 12 and under |
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
O2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
GCS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Time Pulse |
|
Resp |
SBP DBP |
Method BP |
LOC |
Sat |
|
|
EKG |
Eyes |
|
|
Verbal |
|
Motor |
|
Score |
Weight |
Airway |
CNS |
BP |
Wounds |
Skeletal 143. PT Score |
||||||||||||||||||||||||
|
|
|
|
|
|
|
Arterial Line |
|
A |
|
|
|
|
|
4 Spon |
|
5 Oriented |
|
6 Obeys |
|
|
|
|
Initial: |
|
Initial: |
|
Initial: |
|
Initial: |
|
Initial: |
|
Initial: |
|
Initial: |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
Auto Cuff |
|
V |
|
|
|
|
|
3 Speech |
|
4 Confuse |
|
5 Localizes |
|
|
|
>20:+2 |
|
Normal:+2 |
|
Awake:+2 |
|
>90:+2 |
|
|
|
None: +2 |
|
|
None:+2 |
|
|
|
|
||||||||
|
|
|
|
|
|
|
Manual Cuff |
|
|
|
|
|
|
2 Pain |
|
3 Inapprop |
|
4 W/draws |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
P |
|
|
|
|
|
|
|
|
|
|
|
Maint:+1 |
|
Obtund:+1 |
|
|
|
Minor: 1 |
|
|
Closed fx:+1 |
|
_____ |
|
||||||||||||||||
|
|
|
|
|
|
|
Palpate Cuff |
|
|
|
|
See Ref |
1 None |
|
2 Garbled |
|
3 Flexion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
U |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
Sheet |
|
|
|
1 None |
|
2 Extent |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 None |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6 Obeys |
|
|
|
|
Final: |
|
Final: |
|
Final: |
|
Final: |
|
Final: |
|
Final: |
|
|
|
|
|||||||
|
|
|
|
|
|
|
Arterial Line |
|
A |
|
|
|
|
|
4 Spon |
|
5 Oriented |
|
5 Localizes |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
Auto Cuff |
|
|
|
|
|
|
3 Speech |
|
4 Confuse |
|
4 W/draws |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
V |
|
|
|
|
|
|
|
|
|
|
>20:+2 |
|
Normal:+2 |
|
Awake:+2 |
|
>90:+2 |
|
|
|
None: +2 |
|
|
None:+2 |
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
Manual Cuff |
|
|
|
|
|
|
2 Pain |
|
3 Inapprop |
|
3 Flexion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
P |
|
|
|
|
|
|
|
|
|
|
|
|
Maint:+1 |
|
Obtund:+1 |
|
|
|
Minor: 1 |
|
|
Closed fx:+1 |
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
Palpate Cuff |
|
|
|
|
See Ref |
1 None |
|
2 Garbled |
|
2 Extent |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
U |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
Sheet |
|
|
|
1 None |
|
1 None |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6 Obeys |
|
|
|
|
>20:+2 |
|
Normal:+2 |
|
Awake:+2 |
|
>90:+2 |
|
|
|
None: +2 |
|
|
None:+2 |
|
|
|
|
||||
|
|
|
|
|
|
|
Arterial Line |
|
A |
|
|
|
|
|
4 Spon |
|
5 Oriented |
|
5 Localizes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Maint:+1 |
|
Obtund:+1 |
|
|
|
Minor: 1 |
|
|
Closed fx:+1 |
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
Auto Cuff |
|
|
|
|
|
|
3 Speech |
|
4 Confuse |
|
4 W/draws |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
V |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
Manual Cuff |
|
|
|
|
|
|
2 Pain |
|
3 Inapprop |
|
3 Flexion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
P |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
Palpate Cuff |
|
|
|
|
See Ref |
1 None |
|
2 Garbled |
|
2 Extent |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
U |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
Sheet |
|
|
|
1 None |
|
1 None |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6 Obeys |
|
|
|
|
>20:+2 |
|
Normal:+2 |
|
Awake:+2 |
|
>90:+2 |
|
|
|
None: +2 |
|
|
None:+2 |
|
|
|
|
||||
|
|
|
|
|
|
|
Arterial Line |
|
A |
|
|
|
|
|
4 Spon |
|
5 Oriented |
|
5 Localizes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Maint:+1 |
|
Obtund:+1 |
|
|
|
Minor: 1 |
|
|
Closed fx:+1 |
|
Final: |
||||||||||||||||||
|
|
|
|
|
|
|
Auto Cuff |
|
|
|
|
|
|
3 Speech |
|
4 Confuse |
|
4 W/draws |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
V |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
Manual Cuff |
|
|
|
|
|
|
2 Pain |
|
3 Inapprop |
|
3 Flexion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
P |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
Palpate Cuff |
|
|
|
|
See Ref |
1 None |
|
2 Garbled |
|
2 Extent |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_____ |
|
|||||||
|
|
|
|
|
|
|
|
U |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
Venous Line |
|
|
|
|
Sheet |
|
|
|
1 None |
|
1 None |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
MEDICATIONS |
Continued from 1st page |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Time |
|
Medication Given See Reference Sheet |
|
|
Medication Administered By: |
|
Reactions |
See Reference Sheet |
|
Medication Authorization |
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not applic |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not applic |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not applic |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not applic |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Protocol (Standing Order) |
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
CM 1 |
CM 2 |
CM 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Written Orders (Patient Specific) |
Not applic |
||||||||||||||||
|
PROCEDURES Continued from 1st page |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Time |
|
Procedure |
|
|
|
|
|
|
|
# Attempts |
|
Successful |
|
|
|
Done By: |
|
|
|
Complications |
|
|
See Reference. Sheet |
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|
NA |
|
|
|
CM 1 |
CM 2 |
|
CM3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|
NA |
|
|
|
CM 1 |
CM 2 |
|
CM3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|
NA |
|
|
|
CM 1 |
CM 2 |
|
CM3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|
NA |
|
|
|
CM 1 |
CM 2 |
|
CM3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
NO |
|
NA |
|
|
|
CM 1 |
CM 2 |
|
CM3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
CREW MEMBER 4 ID NUMBER |
|
|
|
CREW MEMBER 5 ID NUMBER |
|
|
|
|
|
CREW MEMBER 6 ID NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
_____________________________________________ |
|
|
____________________________________________ |
|
|
|
|
_____________________________________________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
Crew Member4 Signature |
|
|
|
|
|
|
Crew Member5 Signature |
|
|
|
|
|
|
|
Crew Member6 Signature |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
Ο B Ο I Ο P |
Ο EMR Ο Physician Ο Nurse O Student O Other |
|
Ο B |
Ο I Ο P Ο EMR Ο Physician Ο Nurse O Student O Other |
|
Ο B |
Ο I |
Ο P Ο EMR Ο Physician Ο Nurse O Student O Other |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
CREW MEMBER 4 ROLE |
|
|
|
|
CREW MEMBER 5 ROLE |
|
|
|
|
|
|
|
CREW MEMBER 6 ROLE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
Primary Patient Caregiver |
Driver |
|
|
Primary Patient Caregiver |
|
|
Driver |
|
|
|
|
Primary Patient Caregiver |
|
Driver |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
Secondary Patient Caregiver |
Other |
|
|
Secondary Patient Caregiver |
Other |
|
|
|
|
Secondary Patient Caregiver |
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
Third Patient Caregiver |
|
|
|
|
|
Third Patient Caregiver |
|
|
|
|
|
|
|
|
|
|
Third Patient Caregiver |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Form Characteristics
| Fact Name | Description |
|---|---|
| Incident Date | The report begins with the incident date, crucial for documentation and legal purposes. |
| Oklahoma Report Number | This unique identifier helps in tracking and reference, governed by Oklahoma's EMS regulations. |
| EMS Agency Number | This is a mandatory field that identifies the emergency medical services unit responding to the incident. |
| Patient Disposition | Multiple options, such as “Treated and Transported” or “Patient Refused Care,” provide clarity on the outcome of the response. |
| Response Mode to Scene | Captures the urgency of the EMS response, influencing regulatory compliance under Oklahoma law. |
| Patient Medical History | This section collects vital information about known medical conditions, which is essential for effective care. |
| HIPAA Compliance | The form contains a notice regarding HIPAA Privacy Practices, ensuring patient confidentiality during treatment. |
Guidelines on Utilizing Prehospital Care Report
Filling out the Prehospital Care Report form accurately is crucial for proper documentation and continuity of care. Below are the steps required to complete this form efficiently.
- Incident Date: Enter the date of the incident.
- Oklahoma Report Number: Write the assigned report number.
- EMS Agency Number: Fill in the emergency medical services agency number.
- Vehicle Number: State the vehicle number involved in the call.
- EMS Unit Call Sign: Indicate the call sign for the EMS unit.
- Station Number: Enter the relevant station number.
- Incident/Patient Disposition: Select the appropriate patient outcome from the provided options.
- Incident Address: Fill in the specific location of the incident.
- Incident City: Enter the city where the incident took place.
- Incident State: Indicate the state of the incident.
- Incident Zip Code: Provide the zip code for the incident location.
- Incident County: Specify the county of the incident.
- Response Mode to Scene: Choose the response mode utilized.
- Estimated Time of Onset: Document the estimated time when the incident began.
- PSAP / Initial Call for Help: Include details of the Public Safety Answering Point call.
- Unit Arrived at Scene: Note the time using military format when the unit arrived at the scene.
- Arrived at Patient: Record the time the unit arrived at the patient with indication of lights/sirens used.
- Unit Left Scene: Indicate the time the unit departed the scene.
- Patient Arrived at Destination: Document the arrival time at the receiving facility.
- Unit Back in Service: Write the time the unit was available for the next call.
- Type of Service Requested: State the type of service provided.
- Incident Location Type: Select the applicable location type for the incident.
- Number of Patients at Scene: Specify how many patients were at the scene.
- Primary Role of the Unit: Indicate the main function of the unit during the incident.
- Patient Information: Fill in last name, first name, middle initial, address, and contact details.
- Patient Age: Specify the patient's age in appropriate units (e.g., years, months).
- Date of Birth: Enter the date of birth of the patient.
- Social Security Number: Provide the patient's Social Security number if applicable.
- Race and Ethnicity: Select the patient's race and indicate their ethnicity.
- Gender: Indicate the patient's gender.
- Primary Payment Method: Choose the payment method that applies.
- Chief Complaint: Describe the primary complaint of the patient.
- Patient Medical and Medication History: Enter the medical and medication details for the patient.
- Patient Medication Allergies: List any known allergies the patient has related to medication.
- Narrative: Provide a detailed narrative about the patient’s condition and treatment received.
- Vital Signs: Record the initial and final vital signs as well as the Glasgow Coma Scale score.
- Medications Given: Include details on medications administered to the patient.
- Procedures: State any procedures performed and their outcomes.
- Crew Member Details: Document the information of all crew members involved in the response.
- Barriers to Effective Care: Note any barriers experienced during the care of the patient.
- Outcome of Care: Indicate how the patient was transferred and what the final disposition was.
What You Should Know About This Form
What is the purpose of the Prehospital Care Report (PCR)?
The Prehospital Care Report serves as a crucial document that records the details of prehospital care provided to patients by emergency medical services. This report includes essential information such as the date of the incident, patient demographics, assessment findings, interventions performed, and disposition of the patient after treatment. By documenting these facts, the PCR helps ensure continuity of care and provides valuable data for future medical assessments and quality improvement initiatives.
What information is collected in the PCR?
The PCR collects a wide range of information including, but not limited to, the incident date, Oklahoma report number, EMS agency details, vehicle number, patient demographics, nature of the incident, chief complaint, medical history, and assessment findings. It also documents vital signs, medications administered, procedures performed, and the final disposition of the patient, such as whether they were treated and transported or refused care. This comprehensive approach facilitates thorough patient care and accurate record-keeping.
Who is responsible for completing the PCR?
Typically, the PCR is completed by the emergency medical personnel on the scene, such as paramedics and emergency medical technicians (EMTs). Each crew member involved in patient care contributes to the report based on their role and the care provided. It is important that the information captured is accurate and complete to reflect the interventions made and patient outcomes.
How does the PCR impact patient care?
The PCR directly impacts patient care by providing a clear account of the treatment administered and the patient's condition upon arrival at the hospital. Emergency departments rely on this report to understand the patient's medical background and the prehospital care they received. Accurate and detailed documentation can lead to better treatment decisions and improved health outcomes for patients.
What happens if the patient refuses care?
If a patient refuses care, this must be clearly documented in the PCR. The report will note that the patient was informed of the risks associated with their decision to refuse treatment. It is also essential to have the patient or their guardian sign a release form to acknowledge their decision. This documentation can protect both the healthcare provider and the patient by ensuring that informed consent was considered.
Are there specific codes used in the PCR, and what do they signify?
Yes, the PCR includes specific codes, often referenced in a supplementary sheet, which signify various elements such as the condition codes, type of service requested, and complaint categories. These codes allow for standardization in reporting and facilitate accurate data collection and analysis. Accurate coding helps in efficiently communicating the nature of the incident and the care provided.
Can medical information be shared without consent?
Under HIPAA (Health Insurance Portability and Accountability Act) regulations, medical information can generally only be shared with consent. However, there are exceptions for emergency situations where patient care is necessary. The PCR includes a section in which patients typically provide their authorization for information release, which allows providers to share critical information with other medical facilities and insurance companies.
What is the significance of the response mode to the scene?
The response mode indicates the urgency with which the EMS unit responded to the scene. It could be categorized as lights and sirens or no lights and no sirens. This aspect of the report is vital for understanding how quickly care was initiated based on the perceived severity of the incident. Documenting the response mode helps in evaluating the effectiveness of emergency response protocols.
How does the PCR support legal and administrative processes?
The PCR serves as a legal document that can be used in investigations or proceedings regarding the care that the patient received. Accurate and thorough documentation helps protect EMS providers against liability and ensures transparency in patient care processes. Administratively, analysis of PCR data can contribute to improving emergency services and healthcare protocols.
Is training required for those completing the PCR?
Yes, training is required for personnel completing the PCR. EMS providers must understand the importance of accurate documentation and the technical aspects of the form. Regular training sessions on how to properly fill out the PCR, including coding and legal considerations, ensure that all team members are competent and compliant with best practices in documentation.
Common mistakes
When filling out the Prehospital Care Report (PCR) form, accuracy is crucial for ensuring proper patient care and documentation. It is not uncommon for errors to occur, which can lead to complications down the line. Here are eight common mistakes that people make when completing this important document.
Firstly, many individuals forget to fill in the incident date and incident address. This key information allows for easy tracking of incidents and creating accurate records. Without it, the report may lack context, making it difficult for healthcare providers to understand the timeline and location of care.
Secondly, selecting the wrong incident/patient disposition can create confusion. For instance, marking "Treated & Released" when the patient was actually transported elsewhere misrepresents the care provided. It is essential to carefully evaluate and choose the correct option, as it affects future medical follow-ups and potential billing issues.
Another frequent mistake involves forgetting to document the response mode to the scene. Whether lights and sirens were used or not can significantly affect how the incident is perceived and how care is coordinated. Not capturing this information leaves gaps in communication among emergency services.
Additionally, many people overlook completing the patent medical and medication histories. Neglecting to provide this critical background information can hinder effective treatment. Medications and past medical history could influence the current diagnosis and response, so thoroughness here is vital.
It's also common for responders to miss indicating the primary payment method. This detail is indispensable for hospitals and emergency services to determine how to bill for services rendered. Without this information, there may be delays in processing claims, leading to confusion for patients regarding their responsibilities.
Another pitfall is failing to accurately document vital signs and the Glasgow Coma Scale
Furthermore, many responders make assumptions rather than documenting medication complications or procedure attempts when applicable. Even if no complications occur, it is essential to note that the medications and procedures were administered and monitored, as this assures continuity of care.
Lastly, neglecting to obtain proper patient or guardian signatures for consent can lead to serious issues. If a patient refuses treatment, their signed acknowledgment of that decision is essential to protect both the healthcare provider and the institution from liability.
In closing, careful attention to detail will ensure that the Prehospital Care Report is thorough and accurate. Each section of the form plays a critical role in facilitating effective communication and quality patient care.
Documents used along the form
The Prehospital Care Report (PCR) is a critical component of emergency medical services (EMS) documentation. It provides a detailed account of patient care during emergencies, documenting various essential elements. Along with the PCR, other forms and documents play vital roles in capturing and managing patient data, ensuring appropriate care, and facilitating communication among healthcare providers. Below is a list of the documents commonly used in conjunction with the Prehospital Care Report.
- Patient Consent Form: This document secures permission from the patient or their guardian for medical treatment and services. It outlines the nature of the treatment and any associated risks.
- Transfer of Care Form: This form is used during the handoff of patient care between EMS personnel and the receiving medical facility. It ensures that critical information is communicated effectively.
- Medication Administration Record (MAR): This record details the medications administered to the patient, including dosages and times. It helps manage medication safety and provides a clear history of treatment.
- Trauma Assessment Form: Used specifically for trauma patients, this form evaluates injuries sustained and provides critical information regarding the patient's condition at the scene.
- Vital Signs Record: This document tracks and records a patient's vital signs over time, providing essential data that can influence patient care decisions.
- Incident Report: An official summary of the emergency incident, including details about the event, response times, and actions taken. This report is vital for quality assurance and applicable for legal considerations.
- EHR (Electronic Health Record) Integration Form: When available, this form connects EMS data to electronic health records, improving continuity of care and streamlining information access across healthcare systems.
- Insurance Information Form: This document gathers necessary insurance details to facilitate billing and claims processing, ensuring that financial responsibilities are clear from the start.
- Field Treatment Guidelines or Protocols: These guidelines provide EMS personnel with essential protocols and procedures to follow during patient care, ensuring adherence to best practices and regulatory standards.
These documents, alongside the Prehospital Care Report, create a comprehensive framework that aids in the effective delivery of emergency medical services. Ensuring that all necessary forms are completed helps safeguard patient care and enhances communication among all parties involved in a patient’s treatment journey.
Similar forms
-
Emergency Medical Services (EMS) Run Report: Similar to the Prehospital Care Report, the EMS Run Report documents the details of an emergency medical call, including the patient's condition, treatments provided, and response times. Both documents serve as a comprehensive record for continuity of care and legal protection.
-
Patient Care Record (PCR): The PCR captures the clinical details of patient interactions, including assessments, treatments, and outcomes. Like the Prehospital Care Report, it emphasizes patient history and vital signs to inform receiving healthcare providers.
-
Incident Report: This document records details surrounding the incident itself, including location, time, and circumstances. Its purpose aligns with the Prehospital Care Report in providing a formal account of events for review and analysis.
-
Ambulance Service Billing Form: Used to document the services rendered and facilitate billing to insurance or the patient. Much like the Prehospital Care Report, it includes relevant patient data and service details crucial for reimbursement.
-
Transfer of Care Documentation: This form outlines the handoff process when a patient is transferred from one medical provider to another. It parallels the Prehospital Care Report by ensuring that vital patient information is communicated effectively between providers.
Dos and Don'ts
The Prehospital Care Report form is a critical document in emergency medical services. Careful attention to detail is required when filling it out. Here are five essential dos and don'ts to consider:
- Do fill out all required fields completely. Ensure that information such as incident date and patient details is accurate.
- Don't use abbreviations unless they are standard and widely recognized. This prevents confusion and misinterpretation of important data.
- Do document the service type and patient status clearly. For example, specify whether the patient was treated, transported, or refused care.
- Don't omit crucial patient information, especially regarding medications, allergies, and medical history. This information can impact treatment and outcomes.
- Do ensure that signatures are obtained where necessary, especially from the patient or guardian for consent. This protects both the service provider and the patient.
Misconceptions
Understanding the Prehospital Care Report (PCR) form is essential for ensuring efficient and accurate documentation of emergency medical services. However, several misconceptions can cloud its use. Here are ten common misconceptions about the PCR form:
- The PCR form is only for ambulance services. Many believe that only ambulance personnel use this form. In reality, various emergency medical providers and services document care using the PCR format.
- All information on the PCR form is mandatory. While certain fields are required, not all sections need to be filled out for every report. Depending on the situation, some fields may be left blank.
- The form is only used after a transport occurs. Some think that PCR forms are exclusively for incidents involving patient transport. However, they are also applicable for patients who refuse care or when no treatment is required.
- Only paramedics fill out the PCR. It’s a misconception that only paramedics are responsible for completing this form. EMTs and other trained personnel also have the authority to complete the PCR.
- The PCR does not impact patient care. Some may assume that the information on the PCR is inconsequential. In fact, this documentation is vital for continuity of care and informs other healthcare providers about the patient’s condition and treatment.
- A single PCR can accurately represent multiple patients. Many believe one PCR can cover multiple patients in a single incident. Each patient involved in an incident requires their own separate PCR for accurate documentation.
- The PCR form is filled out only at the scene. Some think that documentation is limited to the incident location. In truth, additional details can be noted en route to the hospital if needed.
- Patient privacy is not considered in the PCR. It is a common belief that personal patient information is not safeguarded. However, the PCR must comply with HIPAA regulations, which protect patient privacy.
- The PCR form is only for record-keeping. Many view the form solely as a record. However, it serves as a communication tool among healthcare providers, facilitating a shared understanding of the patient’s care history.
- The form is too complex to be completed accurately. Some think the PCR form is overly complicated. While it contains multiple sections, comprehensive training is provided to ensure accuracy and ease of use.
Key takeaways
Properly filling out the Prehospital Care Report (PCR) form is crucial for effective communication and documentation in emergency medical services (EMS). Here are key takeaways:
- Incident Details Are Essential: Begin by documenting the incident date, Oklahoma report number, and relevant EMS agency details. This provides vital context for the report.
- Accurate Patient Information: Include comprehensive patient details such as name, address, age, race, and medical history. This information facilitates continuity of care.
- Document Treatment and Disposition: Clearly indicate the patient’s disposition, such as whether they were treated, transported, or refused care. This helps establish the intervention's outcome.
- Time Tracking is Critical: Record all times associated with the response, including arrival at the scene and departure. Accurate timing can be essential for quality assurance and legal purposes.
- Assessment of Chief Complaints: Clearly document the patient's chief complaints and any symptoms reported. This forms the basis for the patient's immediate medical needs.
- Medication and Procedures Log: Include detailed information about any medications administered and procedures performed. This ensures thorough medical records and helps in preventing errors.
- Use of Reference Sheets: Make effective use of reference sheets for coding condition codes, level of service, and any specific procedures. These ensure accuracy and consistency in reporting.
- Analyze Barriers to Care: Note any barriers encountered while providing care, such as language issues or physical restraints. Understanding these can improve future responses.
- Signatures Are Mandatory: Ensure that all crew members sign the PCR form. This verifies that the report accurately reflects the care provided and fulfills legal requirements.
Thorough and accurate completion of the PCR form not only improves patient care but also provides legal protection and supports the integrity of the EMS system.
Browse Other Templates
Arkids - If assistance is needed during the application process, a Help Center is available for support.
What Taxes Does Delaware Have - Form 1089 contributes to a smoother tax filing experience in Delaware.