Fill Out Your Progress Notes Form
The Progress Notes form is a vital document in patient care, capturing essential information during a patient's treatment journey. This form is structured to include key details, ensuring that all relevant aspects of a patient's health are accurately recorded. It starts with the date of the entry, emphasizing the timeline of care provided. Patient identification is crucial, so it requires the patient's full name, grade, rank, rate, and the name of the hospital or medical facility. Each entry must be clear and concise, allowing healthcare professionals to review and understand a patient’s status quickly. The form is standardized as Form 509, which promotes uniformity in documentation practices across various facilities. This consistency not only enhances communication among medical staff but also supports the overall quality of care delivered to patients. By systematically updating the Progress Notes, healthcare providers can ensure continuity of care and address any changes in the patient's condition promptly.
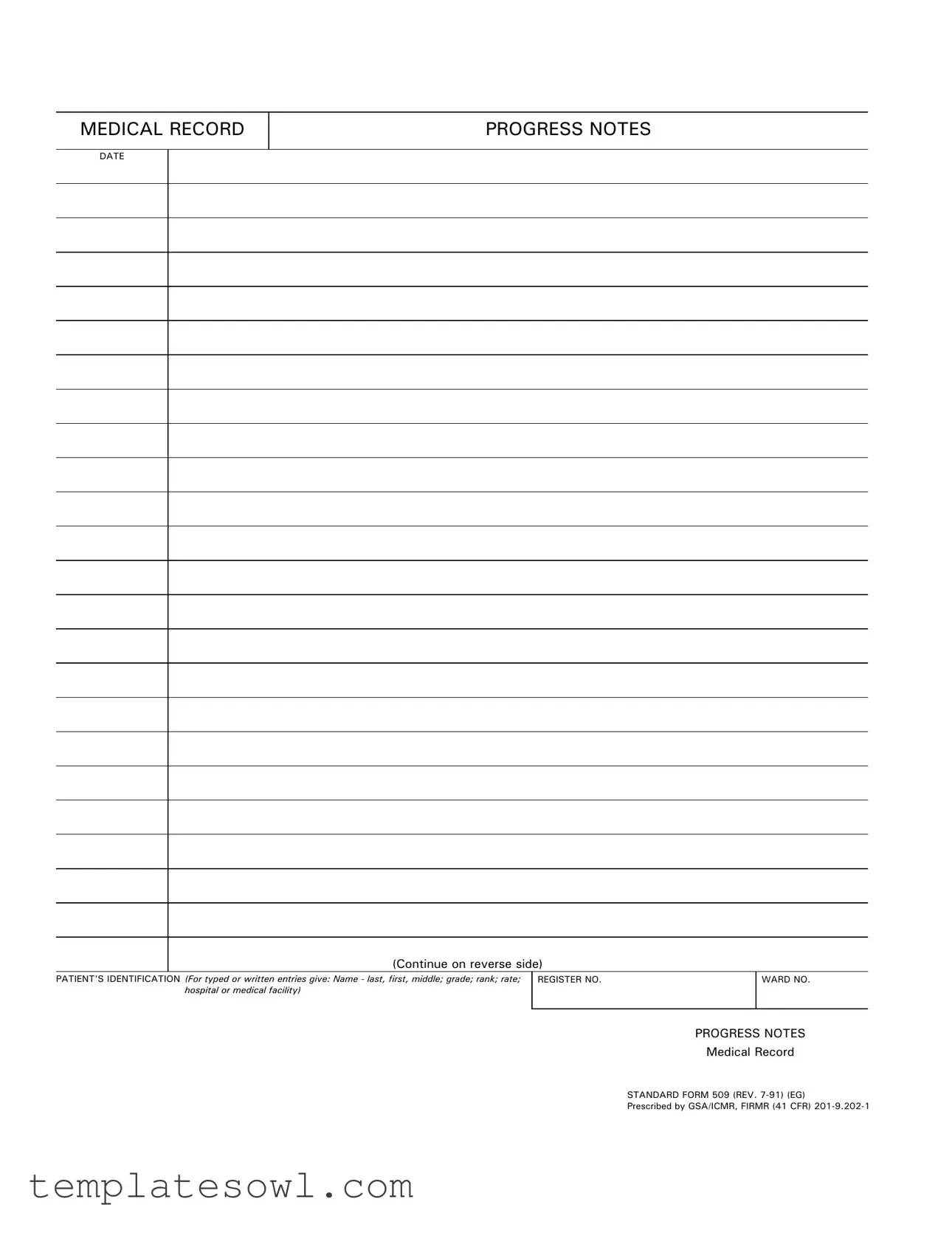
Progress Notes Example
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | The Progress Notes form is used to document patient care and medical progress in a clear and organized manner. |
| Governing Law | This form is governed by federal regulations as outlined in 41 CFR 201-9.202-1. |
| Patient Identification | It requires specific patient information, including name, grade, rank, and medical facility. |
| Standard Format | The form follows a standard format to ensure consistency across medical records. |
| Date Requirement | Each entry must include the date of documentation, aiding in chronological tracking. |
| Revision Date | The current version of the form was revised in July 1991. |
| Continuation | There is space provided on the reverse side for additional notes, if necessary. |
Guidelines on Utilizing Progress Notes
Once you have the Progress Notes form ready to fill out, it's important to provide accurate information. Each section requires specific details to ensure the record is complete and useful for future reference. Follow these steps to fill out the form correctly.
- Locate the date field at the top of the form. Write the current date.
- In the "PATIENT'S IDENTIFICATION" section, enter the patient's name. List the last name first, followed by the first name and middle initial.
- Indicate the patient's grade, rank, or rate. Make sure to include this information accurately.
- Provide the name of the hospital or medical facility where the patient is being treated.
- Fill in the "REGISTER NO." which is usually the patient's identification number assigned by the facility.
- Complete the "WARD NO." field with the appropriate ward number where the patient is located.
- In the "PROGRESS NOTES" section, write notes that describe the patient's status, any treatment given, and any recommendations. Be clear and concise.
What You Should Know About This Form
What is the purpose of the Progress Notes form?
The Progress Notes form serves as a standardized method for documenting a patient's medical history, ongoing treatment, and any significant changes in their condition. Health care providers use this form to maintain accurate records, ensuring that all team members are informed about the patient's status and care plan. It also helps facilitate continuity of care throughout the treatment process.
What information is required on the Progress Notes form?
You need to provide the patient's identification details, including their name (last, first, middle), grade, rank, rate, and the name of the medical facility or hospital. Additionally, the date of the entry is crucial, along with specific notes detailing observations, assessments, and any actions taken regarding the patient's care. This information is vital for tracking the patient's progress over time.
How do I fill out the Progress Notes form correctly?
When completing the Progress Notes form, ensure that all fields are filled out clearly and accurately. Begin with the date and the patient's identification details. When entering notes, be concise yet descriptive, including relevant observations and changes in the patient's condition. Use standardized abbreviations where appropriate, and maintain a chronological order to reflect the timeline of treatment. Review your notes for clarity before finalizing the entry.
What should I do if I make an error on the Progress Notes form?
If you notice a mistake after your notes have been recorded, do not attempt to erase or obliterate the error. Instead, strike through the incorrect entry with a single line and initial it. Then, provide the correct information nearby or in a new entry. This ensures that the record remains clear and trustworthy, which is crucial for ongoing patient care and legal compliance.
Is there a specific format or standard for writing Progress Notes?
While the Progress Notes form itself provides a structure, entries should follow a consistent and logical format. It’s often recommended to use the SOAP method (Subjective, Objective, Assessment, Plan) or similar frameworks to enhance clarity. This standardization helps others understand the notes quickly. Adopting a structured approach allows for efficient communication among healthcare providers and ultimately aids in delivering high-quality care to the patient.
Common mistakes
Filling out the Progress Notes form requires attention to detail and accuracy. One common mistake is failing to include complete patient identification. Each entry should contain the patient’s full name, including last, first, and middle names, along with relevant identifiers such as grade, rank, and rate. Incomplete information can lead to confusion or mismanagement of medical records.
Another frequent error is neglecting to use the correct date. The date of the entry is crucial for maintaining a chronological record of patient progress. Omitting the date or inaccurately placing it can hinder the ability to track treatment over time and make it difficult for healthcare providers to follow up on patient care effectively.
A third mistake involves incomplete or vague progress notes. Each entry should clearly describe the patient's condition, treatment provided, and any changes observed. Using ambiguous language or abbreviations that are not universally understood can obscure important information. Clarity is essential for ensuring that healthcare providers can effectively respond to the patient's needs.
Additionally, some individuals may overlook the necessity of proper formatting, which is critical for maintaining the integrity of medical records. Utilizing the standard format as prescribed helps ensure that all necessary fields are filled out and creates a consistent structure across all entries. Ignoring this can lead to disorganization and challenges in retrieving records when needed.
Finally, signature errors are also quite common. Each progress note must be signed by the individual completing the form, along with their title. Missing a signature can render a document incomplete and lead to questions regarding the validity of the information presented. Ensuring that all required fields, including signatures, are properly filled out preserves the integrity of the medical record.
Documents used along the form
The Progress Notes form is a crucial part of a patient's medical record. It's not used in isolation; several accompanying forms and documents provide a comprehensive picture of a patient's care. Understanding these documents is vital for both patients and healthcare providers.
- Patient Intake Form: This document collects essential information about a patient upon their first visit. It includes personal details, medical history, and insurance information, ensuring that the healthcare facility has all necessary data to provide appropriate care.
- Treatment Plan: Created by healthcare providers, the treatment plan outlines the patient's diagnosis, goals for therapy, and proposed interventions. This plan serves as a roadmap for treatment and helps to monitor the patient's progress over time.
- Consent Form: Before any medical procedure or treatment, patients must provide informed consent. This form ensures that patients understand the risks, benefits, and alternatives to the proposed treatment, thereby protecting both their rights and the healthcare provider.
- Discharge Summary: Once a patient has completed their treatment or hospital stay, the discharge summary provides a comprehensive overview of their treatment, condition at discharge, and follow-up care recommendations. This document is essential for both continuity of care and future medical visits.
- Medication Administration Record (MAR): This document tracks all medications given to a patient during their stay. It's crucial for ensuring the right dosage is administered at the right time and helps to prevent medication errors.
Each of these documents plays a vital role in ensuring that patient care is comprehensive and well-documented. Understanding their significance enhances collaboration among healthcare providers and improves patient outcomes.
Similar forms
SOAP Notes: Like Progress Notes, SOAP notes document patient interactions in a structured way using the Subjective, Objective, Assessment, and Plan format. They help healthcare professionals communicate effectively about a patient's status.
Narrative Notes: These notes provide a detailed account of patient care, similar to Progress Notes. They often capture a chronological narrative of patient events, treatments, and responses.
Clinical Notes: These documents outline observations and actions taken during patient encounters. They serve a similar purpose to Progress Notes, ensuring continuity of care.
Discharge Summaries: Discharge summaries encapsulate a patient's treatment and progress over their hospital stay. They share similarities with Progress Notes by summarizing key information for follow-up care.
Treatment Plans: Treatment Plans outline specific goals and interventions for patient care. They are similar to Progress Notes in that they track the ongoing management of a patient’s health and progress.
Dos and Don'ts
When filling out the Progress Notes form, there are specific actions to take and avoid. The following lists outline these do's and don'ts.
- Do fill in the date accurately.
- Do provide complete patient identification, including name and rank.
- Do ensure all required fields are filled out.
- Do use clear and concise language.
- Do review your entries for any errors before submission.
- Don't leave any mandatory fields blank.
- Don't use abbreviations that may not be widely understood.
- Don't alter any official formatting of the form.
- Don't include personal opinions or irrelevant information.
Misconceptions
Many people have misunderstandings regarding the Progress Notes form used in medical records. Here are ten common misconceptions, each clarified for better understanding.
- Progress Notes are not important. Some believe that progress notes are just routine paperwork. In reality, they are critical for tracking a patient's treatment and health outcomes.
- Anyone can fill out Progress Notes. It is a misconception that any staff member can complete these forms. Only qualified medical personnel should record information on Progress Notes to ensure accuracy and compliance.
- Progress Notes are only for doctors. Many think that only doctors can make entries. However, nurses and other healthcare professionals also contribute valuable observations and notes.
- Progress Notes are always lengthy. Some individuals assume that all entries must be lengthy and detailed. While thoroughness is important, brief and precise notes can also be effective.
- Progress Notes must be handwritten. It is often believed that entries can only be handwritten. Electronic health records systems allow for typed entries, enhancing clarity and efficiency.
- Progress Notes are confidential but not necessary to keep secure. Many think that the confidentiality of Progress Notes means they’re not sensitive. They should be stored securely to protect patient privacy.
- All progress notes look the same. There’s a misconception that Progress Notes have a uniform format. Different medical facilities may use varied templates and formats according to their needs.
- Progress Notes can be ignored. Some may believe that neglecting to update Progress Notes is acceptable. Failing to document can impede care and harm patient safety.
- Progress Notes are solely for legal purposes. While they can provide legal protection, the primary function is to communicate essential patient information among healthcare providers.
- Editing Progress Notes is unethical. It's often thought that once notes are written, they cannot be modified. Appropriate corrections are permissible but should be clearly indicated to maintain integrity.
Understanding these misconceptions can improve communication and care in the healthcare setting.
Key takeaways
Here are some key takeaways for filling out and using the Progress Notes form:
- Clearly enter the patient's identification details, including last name, first name, middle initial, grade, rank, and hospital or medical facility.
- Utilize the date section to accurately record when the progress notes are completed. This ensures proper tracking and historical context.
- The form is standardized under Standard Form 509, so it’s important to comply with its structure for consistency across medical records.
- Keep the notes focused and relevant to the patient's care. Include observations, treatments, and any changes in the patient's condition.
Browse Other Templates
How to Get My Llc in Nc - The L 01A serves multiple business types, such as corporations and partnerships.
Work Application Form - Candidates can list additional courses and training relevant to the position, enhancing their qualifications.
How to Get Va Disability - This form streamlines the process of obtaining important housing grants.