Fill Out Your Sbar Form
The SBAR form serves as an essential communication tool in healthcare settings, streamlining the exchange of critical information among medical professionals. By following a structured format, the SBAR approach categorizes vital details into four key sections: Situation, Background, Assessment, and Recommendation. Within the "Situation" section, healthcare providers briefly outline the patient's name, age, and the primary problem leading to their admission or procedure. The "Background" component provides context through relevant medical history and pertinent background data, allowing for a fuller understanding of the patient's health status. Moving to the "Assessment" part, professionals document current vital signs, any significant findings from nursing assessments, and relevant lab results, while noting the trends in abnormal clinical data. Finally, the "Recommendation" section offers clear suggestions for advancing the patient's plan of care based on the assessment. This structured yet flexible format promotes effective communication, ensuring that everyone involved in a patient's care remains informed and focused on the patient's needs.
Sbar Example
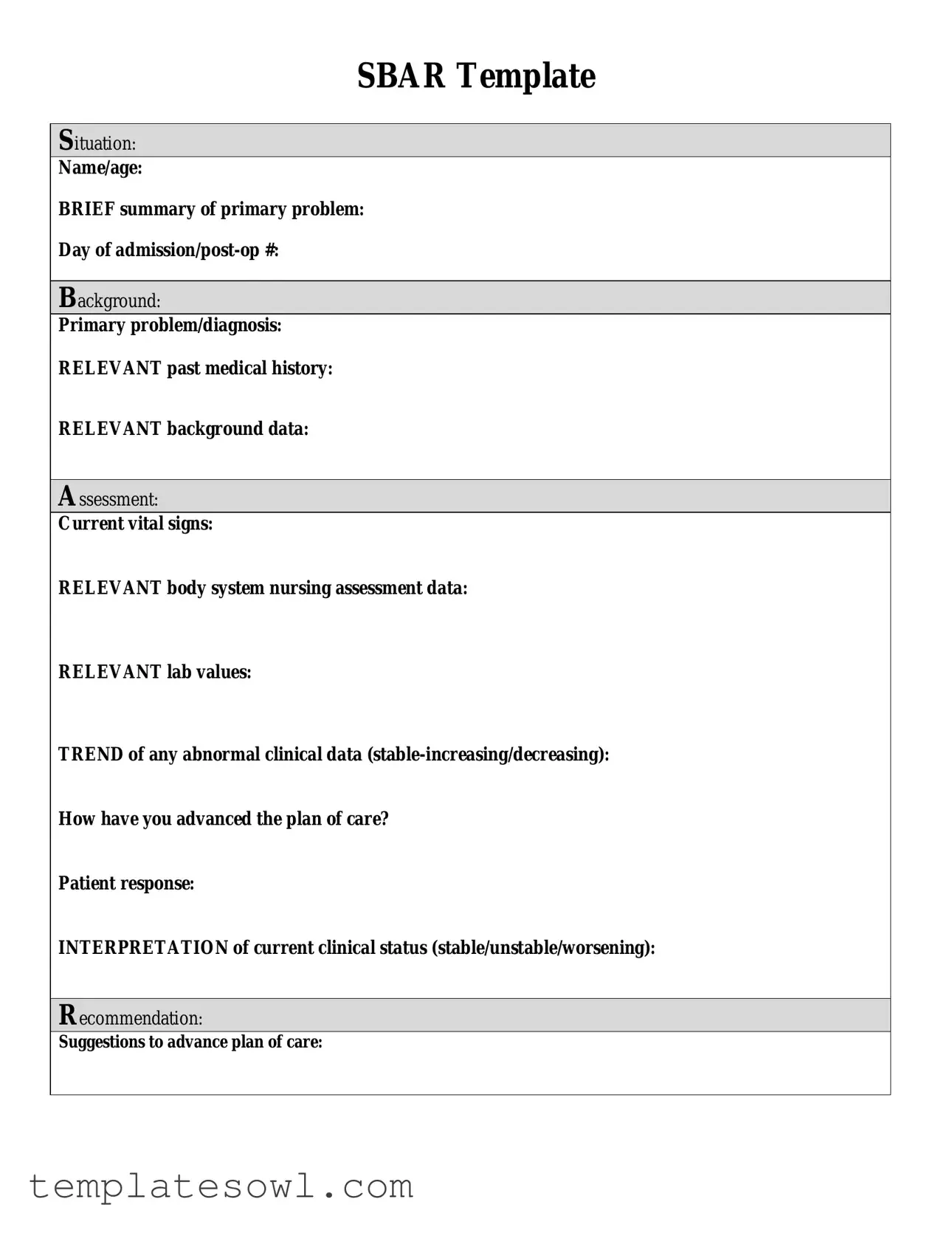
SBAR Template
Situation:
Name/age:
BRIEF summary of primary problem:
Day of
Background:
Primary problem/diagnosis:
RELEVANT past medical history:
RELEVANT background data:
Assessment:
Current vital signs:
RELEVANT body system nursing assessment data:
RELEVANT lab values:
TREND of any abnormal clinical data
How have you advanced the plan of care?
Patient response:
INTERPRETATION of current clinical status (stable/unstable/worsening):
Recommendation:
Suggestions to advance plan of care:
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The SBAR form is a communication tool designed to facilitate clear and concise exchanges of information among healthcare providers. |
| Structure | The SBAR form is structured into four key sections: Situation, Background, Assessment, and Recommendation. |
| Adaptability | Though originally created for healthcare settings, the SBAR format can be adapted for use in various professional fields to enhance communication. |
| Governing Laws | The use of SBAR may be governed by state-specific nursing regulations and practices, which can vary across states. Please consult local regulations for details. |
Guidelines on Utilizing Sbar
Completing the SBAR form is essential for effective communication in a healthcare setting. The following steps will guide you through filling out the form accurately.
- Begin with the Situation section. Fill in the patient's name and age, followed by a brief summary of the primary problem.
- Proceed to the Background section. Clearly outline the primary problem or diagnosis. Include any relevant past medical history and necessary background data that can inform others about the patient's condition.
- Move on to the Assessment section. Enter the current vital signs of the patient. Provide relevant nursing assessment data and important lab values. Indicate the trend of any abnormal clinical data, specifying whether it is stable, increasing, or decreasing.
- Document how you have advanced the plan of care, noting the patient's response to the treatment or interventions. Assess the current clinical status and label it as stable, unstable, or worsening.
- Finally, in the Recommendation section, outline your suggestions for advancing the plan of care. This can include additional tests, treatments, or consults that may be necessary.
What You Should Know About This Form
What is the SBAR form used for?
The SBAR form is a communication tool used in healthcare settings. It helps healthcare professionals convey critical information clearly and effectively. The SBAR format includes four sections: Situation, Background, Assessment, and Recommendation. This structured approach aids in quick and accurate exchanges, particularly during handoffs or emergencies.
What information should be included in the Situation section?
In the Situation section, you need to provide a brief overview of the patient. Include their name and age, along with a concise summary of their primary problem. For instance, you can state if the patient was admitted for a specific condition or if they are post-operative. This snippet of information sets the stage for what needs to be addressed.
What details are required in the Background section?
The Background section requires relevant details about the patient’s primary problem or diagnosis. Include important past medical history that may impact the current situation. Any additional background data that sheds light on the patient’s condition should also be noted. This context is essential for understanding the patient’s history and current health status.
How do I fill out the Assessment section?
In the Assessment section, document the current vital signs and relevant nursing assessment data related to the body systems. Include any pertinent lab values that have been obtained. If there are any abnormal clinical data trends, such as vital signs that are stable or changing, indicate those trends clearly. Also, mention how you have advanced the plan of care based on the patient’s response to treatment.
What should I explain in the Recommendation section?
This section is where you suggest next steps to enhance the patient’s care. Provide specific recommendations to advance the plan of care. It could include possible changes in medications, further diagnostics, or referrals to specialists. Make sure your recommendations are actionable and tailored to the patient’s needs.
Why is using the SBAR form important?
Utilizing the SBAR form is crucial because it promotes clear communication among healthcare providers. When information is transmitted effectively, it leads to better patient safety and quality of care. By following this structured format, you can ensure that essential details are not overlooked, ultimately fostering a collaborative care environment.
Common mistakes
Filling out the SBAR form is crucial for effective communication in healthcare settings. However, many individuals make mistakes that can hinder the clarity and effectiveness of the information being conveyed. The first common mistake occurs when the Situation section lacks specificity. A brief but clear summary is essential to provide immediate context about the patient. Omitting details about the primary problem, such as the day of admission or the nature of the medical condition, may leave healthcare providers with unanswered questions.
Another frequent error involves the Background portion of the form. Many people neglect to include relevant past medical history that might impact the patient's current state. This section should effectively highlight pertinent information, including chronic conditions or previous treatments. A lack of detail here can slow down decision-making processes and potentially affect patient care.
In the Assessment section, failing to provide current vital signs accurately is another mistake that can have significant consequences. Vital signs are critical indicators of a patient's health status and should be noted with precision. Just as vital, the assessment of body systems and lab values should be relevant to the patient's diagnosis. Without this information, healthcare providers may find themselves misinformed about the patient's current condition.
Additionally, individuals sometimes overlook the importance of documenting the TREND of any abnormal clinical data. Noting whether the data is stable, increasing, or decreasing helps convey urgent changes in a patient's health. This oversight can result in missed opportunities for timely intervention and monitoring.
Moving on to the Patient response aspect, some users fail to adequately describe how the patient has responded to the plan of care. Clearly documenting patient responses not only demonstrates the effectiveness of treatments but also aids in ongoing evaluation. An ambiguous or missing patient response can lead to miscommunications that jeopardize patient safety.
The INTERPRETATION section is critically important as well. When individuals fail to clearly categorize the patient’s clinical status as stable, unstable, or worsening, it may leave healthcare teams uncertain about the urgency of the situation. This lack of clarity can affect the overall management of care.
Lastly, the Recommendation segment often sees vague suggestions, which can impact future care planning. Providing specific, actionable recommendations can help ensure continuity and improvement in the patient's care pathway. A well-defined advancement of the plan can make all the difference in the outcomes achieved.
By being mindful of these common pitfalls when filling out the SBAR form, individuals can contribute to a more efficient, effective, and safe healthcare environment. Each section plays a vital role in enhancing communication and ensuring that all team members share the same understanding of a patient's condition.
Documents used along the form
The SBAR form, which stands for Situation, Background, Assessment, and Recommendation, is a vital communication tool in healthcare settings. It aids medical professionals in delivering concise and structured information about a patient, often during handoffs or critical discussions. However, it is commonly used alongside several other forms and documents that contribute to comprehensive patient care. Here’s a look at some of these essential documents.
- Patient History Form: This document collects detailed information about the patient’s medical history, including allergies, previous surgeries, and chronic conditions. It provides context for healthcare providers as they assess current health issues.
- Medication Administration Record (MAR): The MAR is a crucial document tracking all medications administered to a patient. It includes dosage, timing, and any adverse reactions, thus ensuring patient safety during treatment.
- Advance Directives: These legal documents outline a patient’s preferences regarding medical treatment and interventions in the event they cannot communicate their wishes. They empower patients and guide healthcare providers in critical situations.
- Nursing Care Plan: This plan details the specific nursing interventions tailored to address a patient's unique health needs. It serves as a guiding document for the nursing staff, ensuring all aspects of care are covered.
- Patient Consent Form: Before any medical procedure or treatment, patients must give informed consent. This form confirms that patients understand the risks, benefits, and alternatives associated with the proposed care.
- Discharge Summary: Upon a patient’s departure from a healthcare facility, this summary outlines the care provided, follow-up instructions, and any prescribed medications. It plays a vital role in continuity of care.
- Incident Report: This document is used to record any unusual or adverse events during patient care. It helps in identifying areas for improvement and ensures accountability within the healthcare system.
- Referral Form: When a patient needs specialized care, healthcare professionals use referral forms to document the reason for the referral and any relevant patient information, which assists the receiving provider in understanding the case better.
- Clinical Pathway: This is a multidisciplinary plan that outlines the expected course of treatment for specific patient populations. It helps streamline care and improve patient outcomes through standardized processes.
Together, these documents form an integral part of the healthcare communication framework. They enhance the quality of patient care and ensure all medical professionals involved are on the same page, leading to better health outcomes and patient satisfaction.
Similar forms
SOAP Notes: Similar to the SBAR form, SOAP notes are used in clinical settings for concise documentation. They categorize information into Subjective, Objective, Assessment, and Plan, providing a structured approach to patient information.
ADPIE: This acronym stands for Assessment, Diagnosis, Planning, Implementation, and Evaluation. Like SBAR, it outlines a systematic method for nursing process and patient care, emphasizing clear patient understanding.
ISBAR: An extension of SBAR, ISBAR includes Identification, enhancing communication in healthcare settings. It still maintains the focus on structured information exchange, promoting better teamwork.
Narrative Notes: While narrative notes can be less structured, they often include similar information to SBAR. Both aim to document patient status and progress effectively, although narrative notes may lack concise organization.
Clinical Pathways: These are structured multidisciplinary plans of care, outlining specific steps in patient management. They share a goal of promoting effective treatment, similar to how SBAR addresses patient assessment and recommendations.
MAR (Medication Administration Record): While focused on medication management, the MAR supports clear and concise documentation. Both MAR and SBAR emphasize accurate information for patient safety and care improvement.
Care Plans: Care plans are personalized documents that outline patient needs and treatment strategies. They resemble SBAR in their emphasis on clarity, goal setting, and evaluation of patient progress.
Patient Summary Form: This document provides a quick reference for healthcare providers, summarizing key patient information. Both forms share the objective of succinctly delivering critical data for effective care.
Transfer/Hand-off Reports: Used during patient transfers, these reports ensure continuity of care. Like SBAR, they focus on essential information that facilitates communication and protects patient safety.
Incident Reports: Though addressing different situations, incident reports, like SBAR, require concise and accurate documentation about events affecting patient care. Both strive for clarity to improve safety and outcomes.
Dos and Don'ts
When filling out the SBAR form, keeping clarity and accuracy in mind is essential. Here are four do's and don'ts to guide you.
- Do provide a brief and clear summary of the situation.
- Do include relevant past medical history for context.
- Don't use complex medical jargon that might confuse the reader.
- Don't forget to assess and interpret vital signs and relevant lab values.
Following these guidelines ensures that the information is helpful and straightforward, aiding in effective communication.
Misconceptions
The SBAR form is a standardized communication tool used in healthcare settings to enhance clarity and efficiency. However, there are several misconceptions surrounding its use. Here is a list of seven common misunderstandings:
- SBAR is only for nurses. Many believe that only nursing staff can utilize the SBAR form. In reality, it is beneficial for all healthcare professionals, including physicians, pharmacists, and therapists, to improve cross-disciplinary communication.
- SBAR is a one-time tool. Some think SBAR should be used only once per patient encounter. Instead, it should be a dynamic tool employed throughout the patient's care process, adapting to new information and evolving situations.
- The SBAR process is complex. A common belief is that the SBAR form is complicated and difficult to use. On the contrary, it is designed for simplicity and clarity, allowing users to quickly convey essential information without confusion.
- SBAR eliminates the need for face-to-face communication. Some believe that utilizing SBAR replaces the need for direct dialogue. In fact, it serves to complement verbal interactions, ensuring that crucial information is accurately conveyed during discussions.
- Providing recommendations is optional. Many users think that making recommendations on the SBAR form is not necessary. However, it is an integral part of the tool, allowing the communicator to suggest actionable steps for patient care.
- SBAR is only useful in emergencies. A misconception exists that SBAR is only relevant in urgent situations. It is equally important in routine care and assessments, enhancing communication during all patient interactions.
- The SBAR format stifles creativity. Some feel that the structured approach of SBAR restricts their communication styles. Rather, the SBAR format provides a framework that ensures all critical aspects of a patient's condition are covered while allowing for personalized input.
Understanding these misconceptions can lead to improved adoption of the SBAR form, benefiting healthcare communication and patient care overall.
Key takeaways
When utilizing the SBAR (Situation, Background, Assessment, Recommendation) form, keep these key takeaways in mind:
- Understand the Structure: The SBAR form is divided into four distinct sections. Each section serves a specific purpose, making the communication of important information clear and concise.
- Be Concise in the Situation: Start with the patient's name, age, and a brief summary of their primary problem. Avoid unnecessary details to keep it focused.
- Provide Relevant Background: Include critical information about the primary problem, the diagnosis, and any relevant past medical history to provide context.
- Gather Essential Assessment Data: This section should contain current vital signs, relevant nursing assessments, and lab values that may impact the patient’s care.
- Monitor Trends: Note any trends in abnormal clinical data, whether they are stable, increasing, or decreasing, as this information is vital for ongoing assessment.
- Keep Patient Response in Mind: Ensure that you document how the patient has responded to interventions, as this helps in evaluating the effectiveness of the care plan.
- Clarify Clinical Status: Provide an interpretation of the current clinical status, marking it as stable, unstable, or worsening. This can guide immediate clinical decisions.
- Plan Ahead with Recommendations: In the recommendation section, suggest clear, actionable steps to advance the patient’s plan of care.
- Use Clear Language: Avoid complex terminology. Fill out the SBAR form in straightforward language so that all team members can understand it quickly.
- Review Before Sharing: Always review the completed SBAR form for accuracy and completeness. This ensures that vital details are not overlooked when sharing with colleagues.
Browse Other Templates
Utrgv Gpa Calculator - The information you provide on this form helps protect your privacy under federal law.
Is Herpes a Reportable Disease - Encourages timely and accurate data submission.
501c3 Ez Form - Your organization has no current business relationships with Aflac.