Fill Out Your Provider Dispute Resolution Request Form
The Provider Dispute Resolution Request form is an essential tool for healthcare providers seeking to address discrepancies related to billing determinations made by insurance providers. This form serves to initiate a reconsideration process, allowing the provider to present their case without the added burden of billing the patient during the resolution period. It is crucial to fill out the form accurately, paying special attention to required fields marked with an asterisk, and providing a detailed description of the dispute along with the expected outcome. Providers should also offer supporting information to bolster their claims, ensuring clarity in the dispute presented. The form encompasses various aspects, including details about the provider, patient, claim information, and the type of dispute, whether it pertains to claim resolutions, medical necessity appeals, or reimbursement requests. Understanding the specific requirements helps streamline the process, preventing issues related to miscategorized disputes. Additional stipulations, such as the necessity for routine follow-up through a different form, further guide providers in navigating their concerns effectively. By adhering to these guidelines, providers can help ensure a smooth journey through the dispute resolution process.
Provider Dispute Resolution Request Example
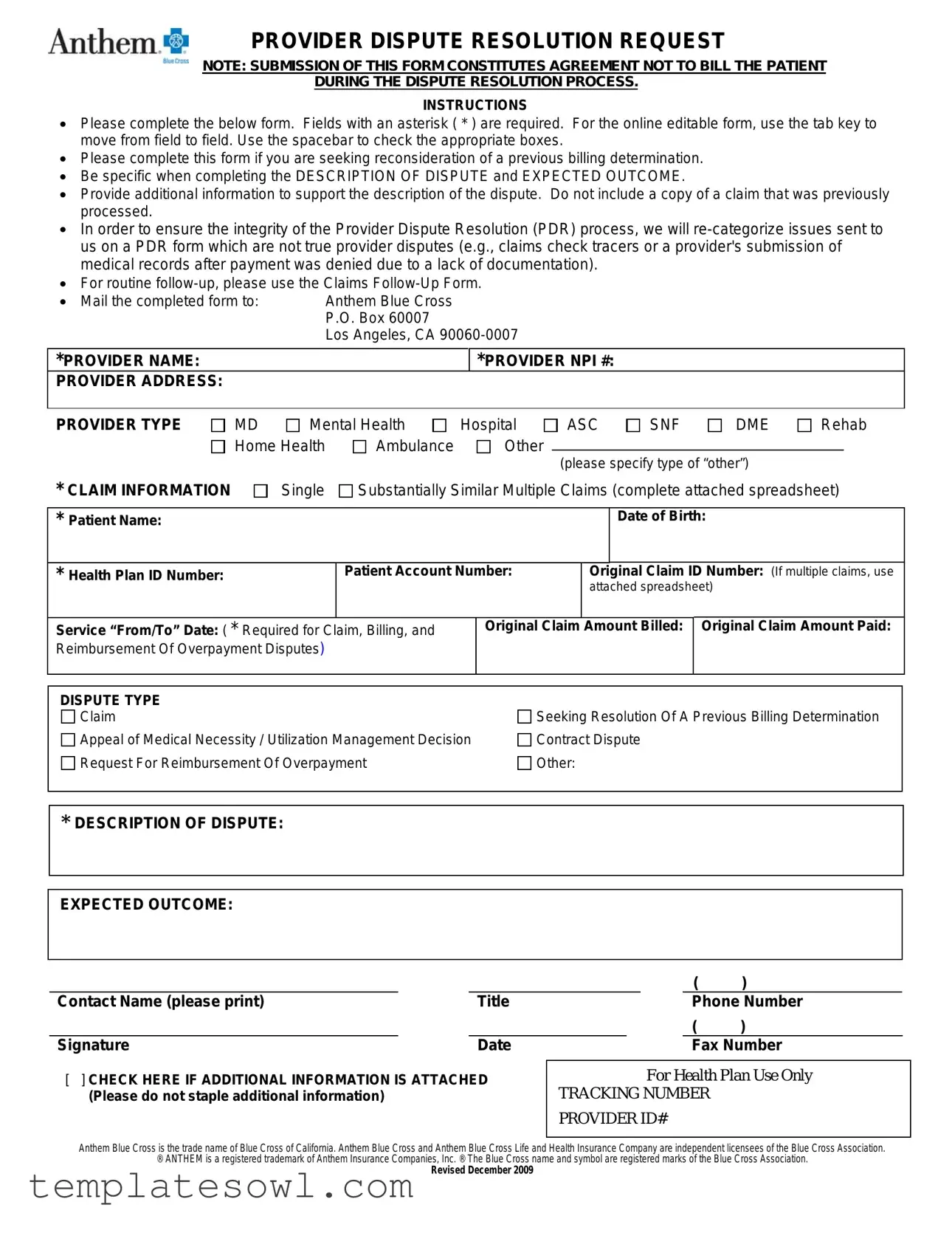
PROVIDER DISPUTE RESOLUTION REQUEST
NOTE: SUBMISSION OF THIS FORM CONSTITUTES AGREEMENT NOT TO BILL THE PATIENT
DURING THE DISPUTE RESOLUTION PROCESS.
INSTRUCTIONS
•Please complete the below form. Fields with an asterisk ( * ) are required. For the online editable form, use the tab key to move from field to field. Use the spacebar to check the appropriate boxes.
•Please complete this form if you are seeking reconsideration of a previous billing determination.
•Be specific when completing the DESCRIPTION OF DISPUTE and EXPECTED OUTCOME.
•Provide additional information to support the description of the dispute. Do not include a copy of a claim that was previously processed.
•In order to ensure the integrity of the Provider Dispute Resolution (PDR) process, we will
•For routine
• Mail the completed form to: |
Anthem Blue Cross |
|
|
P.O. Box 60007 |
|
|
Los Angeles, CA |
|
|
|
|
*PROVIDER NAME: |
|
*PROVIDER NPI #: |
PROVIDER ADDRESS: |
|
|
|
|
|
PROVIDER TYPE
MD |
Mental Health |
Hospital |
ASC |
SNF |
DME |
|
Home Health |
Ambulance |
Other |
(please specify type of “other”) |
|||
|
|
|
|
|||
Rehab
* CLAIM INFORMATION |
Single |
Substantially Similar Multiple Claims (complete attached spreadsheet) |
|
|
|
|
Date of Birth: |
* Patient Name: |
|
|
|
|
|
|
|
*Health Plan ID Number:
Patient Account Number:
Original Claim ID Number: (If multiple claims, use attached spreadsheet)
Service “From/To” Date: ( * Required for Claim, Billing, and Reimbursement Of Overpayment Disputes)
Original Claim Amount Billed: Original Claim Amount Paid:
DISPUTE TYPE |
|
Claim |
Seeking Resolution Of A Previous Billing Determination |
Appeal of Medical Necessity / Utilization Management Decision |
Contract Dispute |
Request For Reimbursement Of Overpayment |
Other: |
*DESCRIPTION OF DISPUTE:
EXPECTED OUTCOME:
|
|
|
( |
) |
|
||||
Contact Name (please print) |
|
Title |
|
|
|
|
Phone Number |
|
|
|
|
|
( |
) |
|
||||
Signature |
|
Date |
|
|
|
Fax Number |
|
||
[ ] CHECK HERE IF ADDITIONAL INFORMATION IS ATTACHED |
|
|
For Health Plan Use Only |
|
|||||
(Please do not staple additional information) |
|
|
TRACKING NUMBER |
|
|
||||
|
|
|
PROVIDER ID# |
|
|
||||
|
|
|
|
|
|
|
|
|
|
Anthem Blue Cross is the trade name of Blue Cross of California. Anthem Blue Cross and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association.
®ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. ® The Blue Cross name and symbol are registered marks of the Blue Cross Association.
Revised December 2009
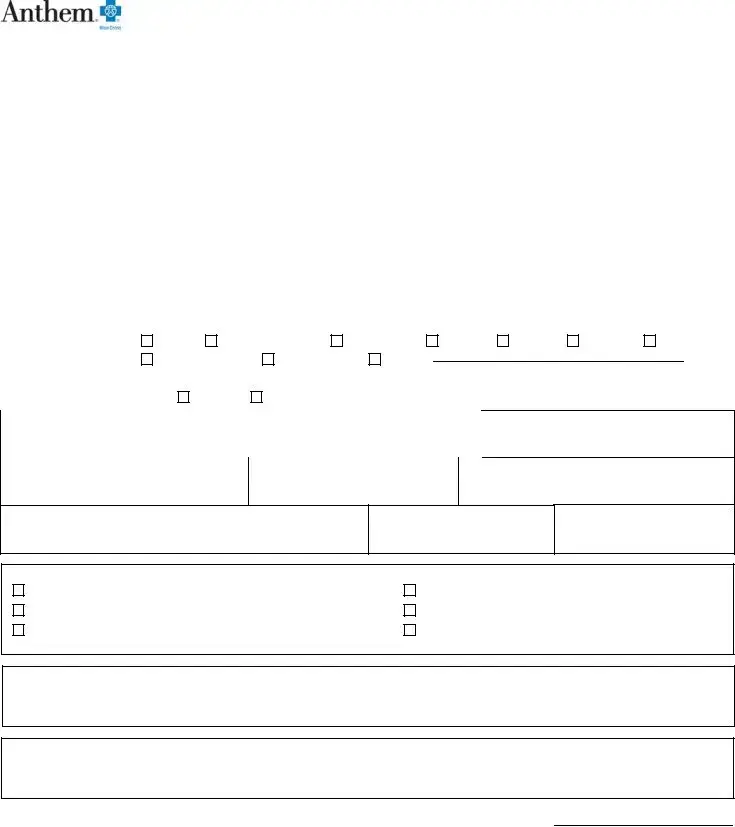
PROVIDER DISPUTE RESOLUTION REQUEST
For use with multiple “LIKE” claims (disputed for the same reason)
*PROVIDER NAME:
*PROVIDER NPI #:
|
|
* Patient Name |
|
|
|
|
|
|
|
|
* Service |
|
Original |
|
Original |
|
|
|
|
|
|
|
|
|
* Health Plan ID |
|
|
|
|
Claim |
|
|
|
||||
|
|
|
|
|
|
Date of |
|
|
Original Claim ID |
|
From/To |
|
Amount |
|
Claim |
|
|
|
Number |
|
Last |
First |
|
|
Birth |
|
Number |
|
Number |
|
Date |
|
Billed |
|
Amount Paid |
|
Expected Outcome |
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
[ ] CHECK HERE IF ADDITIONAL INFORMATION IS ATTACHED (Please do not staple additional information)
Page ______ of ______
Anthem Blue Cross is the trade name of Blue Cross of California. Anthem Blue Cross and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association.
®ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. ® The Blue Cross name and symbol are registered marks of the Blue Cross Association.
Revised April 2009
Form Characteristics
| Fact Name | Description |
|---|---|
| Submission Agreement | Filing the Provider Dispute Resolution Request indicates consent not to bill the patient while the dispute is resolved. |
| Required Fields | Specific fields are marked with an asterisk (*) and must be completed for the form to be valid. |
| Purpose of Form | This form is utilized to request a reconsideration of a previous billing determination. |
| Expected Outcome | Providers must clearly state their expected outcome within the form. |
| Additional Information | Any extra information to support the dispute description should be attached but not as processed claims. |
| Dispute Categorization | Issues that do not qualify as true provider disputes will be re-categorized, helping maintain integrity in the resolution process. |
| Claims Follow-Up | For routine follow-ups related to claims, another form specifically for Claims Follow-Up should be utilized. |
| Mailing Address | Completed forms must be sent to Anthem Blue Cross at P.O. Box 60007, Los Angeles, CA 90060-0007. |
| Version Information | The form has been revised multiple times, with the most recent updates in December 2009. |
Guidelines on Utilizing Provider Dispute Resolution Request
Completing the Provider Dispute Resolution Request form requires attention to detail and careful consideration of the information you provide. After submitting this form, you can expect to go through a dispute resolution process without billing the patient during this time. Below are the steps to follow when filling out the form.
- Begin by entering your Provider Name, making sure to include your Provider NPI #.
- Complete your Provider Address and select your Provider Type from the list provided.
- Choose the Claim Information type: Single, Substantially Similar, or Multiple Claims. If you select Multiple Claims, fill out the attached spreadsheet accordingly.
- Fill in the Patient Information fields including the Date of Birth, Patient Name, Health Plan ID Number, and Patient Account Number.
- Provide the Original Claim ID Number and the Service “From/To” Date. Remember that this information is required for specific disputes.
- Indicate the Original Claim Amount Billed and the Original Claim Amount Paid.
- Select the Dispute Type that corresponds to the nature of your request.
- Clearly write out the Description of Dispute and your Expected Outcome. Be specific to ensure clarity.
- Complete the contact information section by providing your name, title, phone number, signature, date, and fax number.
- If additional information supports your dispute, check the box indicating that additional information is attached.
- Finally, ensure that you mail the completed form to Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007.
What You Should Know About This Form
What is the Provider Dispute Resolution Request form?
The Provider Dispute Resolution Request form is used by healthcare providers to formally request a review of a previous billing decision made by an insurance company. This process allows providers to seek reconsideration without billing the patient during the resolution process.
Who should fill out this form?
This form should be completed by healthcare providers who wish to dispute a billing determination. Whether you are a doctor, mental health provider, or run a hospital, this form is relevant if you disagree with the payment decision by Anthem Blue Cross.
What information do I need to provide on the form?
You'll need to provide details about the provider, including your name, NPI number, and address. You'll also need patient information like their name, date of birth, and Health Plan ID number. The specific details about the claim and the nature of the dispute must be included as well.
What is meant by 'Description of Dispute' and 'Expected Outcome'?
The 'Description of Dispute' section is where you explain why you think the previous decision was incorrect. Be clear and specific. The 'Expected Outcome' is where you outline what resolution you are seeking, whether it's a reprocessing of the claim or an adjustment to the payment amount.
Can I include a copy of the processed claim?
No, you should not include a copy of the claim that was previously processed. Instead, provide additional supporting information that could help clarify the dispute described on the form.
What happens if I submit an issue that is not a true provider dispute?
If the issue submitted does not qualify as a true provider dispute, the request will be re-categorized. For example, claims check tracers or issues about submitting medical records may not meet the criteria for a dispute.
How do I submit the completed form?
Once you have filled out the form, send it by mail to Anthem Blue Cross at the specified address: P.O. Box 60007, Los Angeles, CA 90060-0007. Make sure to check that all required fields are completed before mailing.
What should I do if I have multiple claims to dispute?
If you have multiple claims that are similar and tied to the same dispute, you should complete an attached spreadsheet to provide all necessary details for each claim. Include the claim ID numbers and any other relevant information as required.
Is there a cost associated with submitting this form?
No, there is no cost to submit the Provider Dispute Resolution Request form. Submitting this form signals that you will not bill the patient while the dispute is being resolved, ensuring they are not financially impacted during this process.
What happens after I submit the form?
Once the form is submitted, Anthem Blue Cross will review your dispute. They will then provide a response regarding the resolution of your request. You will be notified of their decision, allowing you to take further steps if necessary.
Common mistakes
When filling out the Provider Dispute Resolution Request form, individuals often overlook essential details, leading to mistakes that can delay the resolution process. One common error is failing to provide complete or accurate contact information. Each section of the form plays a vital role in ensuring effective communication. Without a valid phone number or email, the resolution team may not be able to reach the provider for clarification, resulting in setbacks.
Another frequent mistake involves neglecting the specific fields marked with an asterisk (*). These fields are required, and skipping them could render the submission incomplete. It is crucial to ensure that every mandatory section is filled out thoroughly; otherwise, the form may be returned or disregarded entirely.
In addition, many individuals struggle with articulating the DESCRIPTION OF DISPUTE and EXPECTED OUTCOME sections. Being vague or overly general in these areas can hinder the review process. The description must clearly outline the nature of the dispute, while the expected outcome should reflect what resolution is sought. A precise presentation of these details allows the reviewing team to understand the issue better.
Submitting additional documentation is another area where individuals can err. Although the form mentions that no processed claim is needed, some providers mistakenly include copies of previously processed claims. Adhering to these instructions is critical, as irrelevant documentation can complicate the case instead of clarifying it.
Providers may also misidentify the type of dispute. Select the correct DISPUTE TYPE carefully; options include claims seeking resolution, appeals of medical necessity decisions, and requests for reimbursement. Selecting the wrong dispute type can lead to processing the request incorrectly, further delaying resolution.
Moreover, the section regarding CLAIM INFORMATION is often subject to oversight. Failing to provide accurate and complete claims data, such as the Original Claim ID or specific service dates, can create confusion. Each detail is crucial for the processing team to understand the dispute context.
In addition, individuals often forget to sign the form or include a date. This omission can result in the form being considered invalid. Ensure that every submission is signed and dated to confirm authenticity.
Another common mistake is not checking for additional information attachments. If extra documentation is included, ticking the box indicating this can prevent unnecessary delays in processing. Ignoring to confirm this may lead to miscommunication about what was submitted.
Lastly, individuals may fail to send the form to the correct mailing address. The instructions specify where to send the completed form, and sending it elsewhere can lead to processing delays. It is always prudent to double-check the mailing details to ensure the form reaches Anthem Blue Cross promptly.
Documents used along the form
When navigating the complexities of billing disputes with providers, it’s important to utilize various forms and documents to support your case effectively. Each of these documents serves a distinct purpose in the resolution process. Here’s a list of commonly used forms alongside the Provider Dispute Resolution Request form:
- Claims Follow-Up Form: This form is utilized for routine inquiries regarding the status of a claim. It's the first step to checking on claims that may not involve significant disputes.
- Medical Necessity Appeal Form: Use this form when appealing a denial based on medical necessity. It provides a structured way to submit additional evidence and rationale for reconsideration.
- Reimbursement Request Form: This document is essential when seeking reimbursement for services rendered. It details the services provided and the associated costs, ensuring all relevant information is presented for consideration.
- Consultation Report: A detailed report from a healthcare provider that outlines the medical necessity of the services rendered, current treatment protocols, and reasons for the dispute.
- Prior Authorization Request Form: This form requests approval for specific services or treatments before they take place. It's important to include it if the dispute involves a service that required prior authorization.
- Detailed Billing Statement: This document lists charges for services rendered. It breaks down each charge and can assist in clarifying discrepancies related to payment or services provided.
- Patient's Medical Records: Relevant sections of medical records may be needed to validate treatment decisions and the necessity for specific services. This helps provide context to the billing dispute.
- Contract or Agreement Documentation: Keep copies of the contracts or agreements between the provider and the insurance company. These documents can provide critical insights into covered services and billing practices.
- Proof of Timely Filing: Any documentation that confirms the claim was submitted within the required time frames. This can help establish your case if timely filing is under dispute.
- Additional Supporting Documentation: This can include any letters, emails, or communication that further explains or clarifies the dispute. Gathering all relevant information serves to bolster your request.
Each of these documents plays a critical role in ensuring a smooth and effective resolution process. By gathering and submitting the appropriate forms along with the Provider Dispute Resolution Request form, you enhance your chances for a favorable outcome.
Similar forms
The Provider Dispute Resolution Request form serves as an important tool for healthcare providers to seek reconsideration of billing determinations. However, it shares similarities with several other key documents within the healthcare and insurance landscape. Here’s a look at seven documents that are akin to the Provider Dispute Resolution Request form:
- Claims Appeal Form: Just like the Provider Dispute Resolution Request, this form is used to challenge a health insurance company's denial of a claim. It allows the provider to present their case with supporting documentation.
- Claim Check Tracer Request: This document is essential for tracking the status of a previously submitted claim. While it focuses more on inquiry rather than dispute, it requires specific details about the claim, resembling the information needed in the dispute resolution request.
- Utilization Review Appeal Form: Similar to the Provider Dispute Resolution Request, this form is utilized when a provider disagrees with a utilization management decision. It focuses on the medical necessity of services and the need for reconsideration.
- Request for Reconsideration Form: This form is often used to formally request an evaluation of a billing decision. It mirrors the process described in the Provider Dispute Resolution Request by needing specific information and outlines the provider’s expected outcomes.
- Authorization Verification Form: This document is often required to confirm that prior authorization was obtained for a service. It parallels the Provider Dispute Resolution Request form by ensuring that all necessary information is provided for processing.
- Pre-Authorization Form: When a provider seeks approval for a service before it is performed, this form is utilized. It requires comprehensive details much like the Provider Dispute Resolution Request form regarding the service being disputed.
- Billing Inquiry Form: This form is often used to seek clarification about a bill. While it may not strictly involve a dispute, it informs the insurer of potential issues with billing, akin to the purpose of the dispute resolution request.
Understanding these documents can enhance a provider's ability to navigate disputes and billing challenges in the healthcare system effectively. Each plays a unique but interconnected role in ensuring clarity and resolution in healthcare financing.
Dos and Don'ts
When filling out the Provider Dispute Resolution Request form, careful attention to detail can facilitate the process. Here are four important suggestions regarding what to do and what to avoid.
- Complete All Required Fields: Ensure that all fields marked with an asterisk (*) are filled out accurately. This includes the provider name, NPI number, and patient information.
- Be Clear and Specific: Clearly articulate the description of the dispute and the expected outcome. Specificity helps in understanding the issue at hand.
- Provide Supporting Information: Include any additional information that could bolster your dispute, but do not attach previously processed claims.
- Mail It Properly: Send the completed form to the specified address for timely processing.
- Do Not Bill the Patient: Submitting this form signifies an agreement not to bill the patient while the dispute process is underway.
- Avoid Ambiguity: Do not provide vague descriptions. Ambiguity can result in delays or denial of your dispute.
- Refrain from Submitting Non-Dispute Issues: The form is strictly for provider disputes. Issues such as claims check tracers should be directed elsewhere.
- Do Not Staple Additional Information: Any extra documentation must be included without staples to ensure proper processing.
Misconceptions
Here are some common misconceptions about the Provider Dispute Resolution Request form:
- You can still bill the patient during the dispute. Submission of this form means that providers agree not to bill the patient while the dispute is being resolved.
- Only certain types of disputes can be filed. Providers can submit disputes for various reasons, including billing determinations and utilization reviews.
- It’s not necessary to provide detailed information. Being specific in the DESCRIPTION OF DISPUTE and EXPECTED OUTCOME fields is crucial for a thorough review.
- Previous claims need to be resubmitted. You should not include copies of claims that have already been processed.
- Any issue can be addressed using this form. The form is meant specifically for provider disputes and cannot be used for matters like claims check tracers.
- If you use the form, you cannot follow up. Routine follow-ups should use the Claims Follow-Up Form, separate from disputes.
- Submission is complicated and time-consuming. The form is designed to be user-friendly; you can easily navigate it using the tab key for filling out information.
- All information must be submitted at once. You can check a box to indicate that additional information is attached without stapling any documents.
- You should only contact the health plan after the form is submitted. If you have any questions, reaching out to the health plan during the process is encouraged.
Key takeaways
Here are some key takeaways to keep in mind when filling out and using the Provider Dispute Resolution Request form:
- Do not bill the patient during the process. Submitting the form means you agree not to charge the patient while the dispute is being resolved.
- Complete all required fields. Ensure that you fill in all fields marked with an asterisk (*). Missing information may delay the resolution of your dispute.
- Be specific and detailed. When describing the dispute and expected outcome, provide as much detail as possible. This aids in the evaluation of your request and increases the likelihood of a favorable outcome.
- Avoid including processed claims. Do not send copies of previously processed claims with your request. Instead, focus on providing additional supporting information about the dispute.
- Use the appropriate follow-up form. For routine follow-ups rather than true disputes, utilize the Claims Follow-Up Form instead of the Provider Dispute Resolution Request form.
By keeping these points in mind, you can navigate the dispute resolution process more effectively and improve your chances of a favorable outcome.
Browse Other Templates
Ems Pcr - Document whether a hospital team was notified prior to arriving at the facility.
Letter to School for Absence of Child - Highlights the necessity of formal documentation for absences.
Movers Contract Template - Though care is taken, the risk of damage is acknowledged in the agreement.