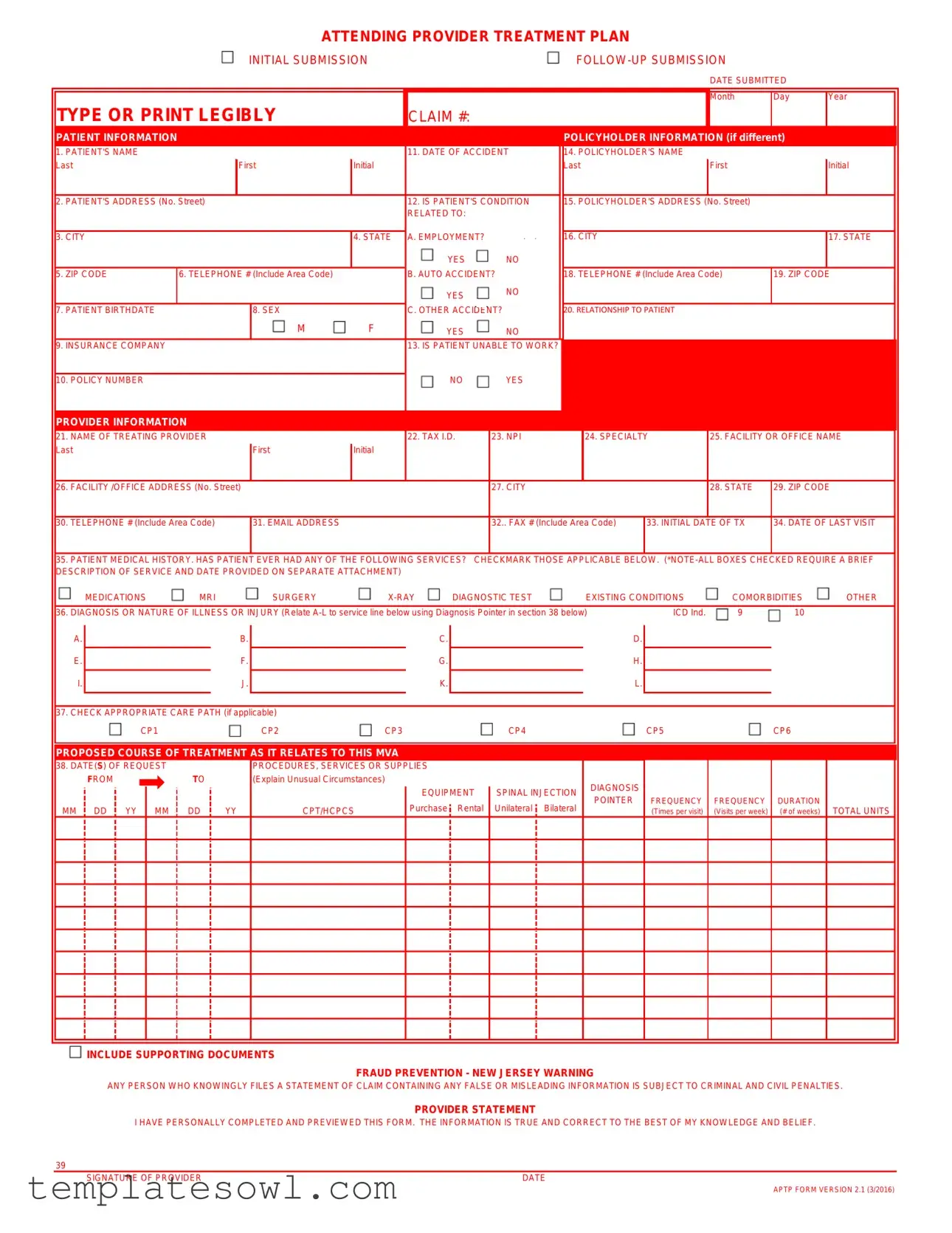
Fill Out Your Provider Treatment Plan Form
The Provider Treatment Plan form plays a critical role in documenting the care strategy for patients, particularly in relation to medical treatments following accidents. This comprehensive document collects essential patient and provider information, including patient names, addresses, and contact details, as well as insurance policyholder information when applicable. Key sections of the form address the patient’s medical history, including diagnoses, previous treatments, and any relevant services received. Providers must specify the proposed course of treatment and outline requested services along with expected treatment duration and frequency. Additionally, the form requires the provider's signature, confirming accuracy and transparency. Supporting documents such as progress notes and medical histories must accompany the form to substantiate the treatment plan and assist in fraud prevention. This structure ensures clear communication among all parties involved in the patient's care, facilitating coordinated efforts towards recovery.
Provider Treatment Plan Example
ATTENDING PROVIDER TREATMENT PLAN
INITIAL SUBMISSION |
DATE SUBMITTED
TYPE OR PRINT LEGIBLY
CLAIM #:
Month
Day
Year
PATIENT INFORMATION |
|
|
|
|
|
|
POLICYHOLDER INFORMATION (if different) |
||||||
1. PATIENT'S NAME |
|
|
|
|
11. DATE OF ACCIDENT |
14. POLICYHOLDER'S NAME |
|
|
|
|
|||
Last |
|
First |
Initial |
|
|
Last |
|
First |
|
Initial |
|||
|
|
|
|
|
|
|
|
|
|
|
|
||
2. PATIENT'S ADDRESS (No. Street) |
|
|
|
12. IS PATIENT'S CONDITION |
15. POLICYHOLDER'S ADDRESS |
(No. Street) |
|
|
|
||||
|
|
|
|
|
RELATED TO: |
|
|
|
|
|
|
|
|
|
|
|
|
|
A. EMPLOYMENT? |
|
|
|
|
|
|
|
|
3. CITY |
|
|
|
4. STATE |
|
16. CITY |
|
|
|
17. STATE |
|
||
|
|
|
|
|
YES |
NO |
|
|
|
|
|
|
|
5. ZIP CODE |
6. TELEPHONE # (Include Area Code) |
|
B. AUTO ACCIDENT? |
18. TELEPHONE # (Include Area Code) |
19. ZIP CODE |
|
|
||||||
|
|
|
|
|
YES |
NO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7. PATIENT BIRTHDATE |
|
|
8. SEX |
|
C. OTHER ACCIDENT? |
20. RELATIONSHIP TO PATIENT |
|
|
|
|
|||
|
|
|
M |
F |
YES |
NO |
|
|
|
|
|
|
|
9. INSURANCE COMPANY |
|
|
|
|
13. IS PATIENT UNABLE TO WORK? |
|
|
|
|
|
|
|
|
|
|
|
|
|
NO |
YES |
|
|
|
|
|
|
|
10. POLICY NUMBER |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PROVIDER INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
21. NAME OF TREATING PROVIDER |
|
|
|
22. TAX I.D. |
23. NPI |
|
24. SPECIALTY |
25. FACILITY OR OFFICE NAME |
|
||||
Last |
|
|
First |
Initial |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
26. FACILITY /OFFICE ADDRESS (No. Street) |
|
|
|
27. CITY |
|
|
|
28. STATE |
29. ZIP CODE |
|
|||
|
|
|
|
|
|
|
|
|
|||||
30. TELEPHONE # (Include Area Code) |
|
31. EMAIL ADDRESS |
|
|
32.. FAX # (Include Area Code) |
33. INITIAL DATE OF TX |
34. DATE OF LAST VISIT |
|
|||||
35.PATIENT MEDICAL HISTORY. HAS PATIENT EVER HAD ANY OF THE FOLLOWING SERVICES? CHECKMARK THOSE APPLICABLE BELOW.
MEDICATIONS |
MRI |
SURGERY |
DIAGNOSTIC TEST |
EXISTING CONDITIONS |
COMORBIDITIES |
OTHER |
|||
|
|
|
|
|
|||||
36. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY (Relate |
ICD Ind. |
9 |
10 |
|
|||||
A.
E.
I.
B.
F.
J.
C.
G.
K.
D.
H.
L.
37. CHECK APPROPRIATE CARE PATH (if applicable)
CP1 |
CP2 |
CP3 |
CP4 |
CP5 |
CP6 |
PROPOSED COURSE OF TREATMENT AS IT RELATES TO THIS MVA
38. DATE(S) OF REQUEST |
|
|
|
|
PROCEDURES, SERVICES OR SUPPLIES |
|
|
|
|||||||
|
|
FROM |
|
|
|
|
TO |
|
|
(Explain Unusual Circumstances) |
|
|
|
|
DIAGNOSIS |
|
|
|
|
|
|
|
|
|
|
|
EQUIPMENT |
SPINAL INJECTION |
POINTER |
||
|
|
|
|
|
|
|
|
|
|
|
|||||
MM |
|
DD |
|
YY |
MM |
|
DD |
|
YY |
CPT/HCPCS |
Purchase |
Rental |
Unilateral |
Bilateral |
|
|
|
|
|
||||||||||||
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FREQUENCY
(Times per visit)
FREQUENCY DURATION
(Visits per week) (# of weeks)
TOTAL UNITS
 INCLUDE SUPPORTING DOCUMENTS
INCLUDE SUPPORTING DOCUMENTS
FRAUD PREVENTION - NEW JERSEY WARNING
ANY PERSON WHO KNOWINGLY FILES A STATEMENT OF CLAIM CONTAINING ANY FALSE OR MISLEADING INFORMATION IS SUBJECT TO CRIMINAL AND CIVIL PENALTIES.
PROVIDER STATEMENT
I HAVE PERSONALLY COMPLETED AND PREVIEWED THIS FORM. THE INFORMATION IS TRUE AND CORRECT TO THE BEST OF MY KNOWLEDGE AND BELIEF.
39
SIGNATURE OF PROVIDER |
DATE |
APTP FORM VERSION 2.1 (3/2016)
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Provider Treatment Plan form is used for submitting treatment plans for patients, primarily in relation to auto accidents. |
| Patient Information | This section requires essential details like the patient's name, address, and insurance information. |
| Policyholder Details | If the policyholder differs from the patient, their information, including name and address, must be provided. |
| Governing Laws | In New Jersey, submissions must comply with the New Jersey Department of Banking and Insurance regulations. |
| Diagnosis Codes | The form requires the primary, secondary, and any additional diagnosis codes in the IC9 format. |
| Proposed Treatment Plan | Section 40 outlines the requested dates of treatment and the specific care paths and services needed. |
| Fraud Warning | This section warns that knowingly submitting false information can lead to legal penalties. |
Guidelines on Utilizing Provider Treatment Plan
Completing the Provider Treatment Plan form requires careful attention to detail. Make sure all necessary information is filled out accurately to avoid delays. Below are the clear steps to help you through the process.
- Begin with the top section: Specify whether this is an initial submission or a follow-up submission. Enter the claim number and the date you are submitting the form.
- Provide Patient Information: Fill in the patient's name, address, city, state, zip code, telephone number, birth date, sex, and Social Security number.
- Insurance Details: Fill in the insurance company name and policy number. Indicate if the patient is unable to work, and provide the policyholder's information if it differs from the patient.
- Indicate the Date of Accident: Specify the date of the accident and check if the patient's condition is related to employment, an auto accident, or another accident.
- Provider Information: Enter the name, tax ID number, specialty, and facility or office name for the treating provider. List the complete facility or office address along with the contact phone number, email, and fax number.
- Medical History: Provide the initial date of treatment, the date of the last visit, and complete the medical history section. Check all services previously provided and attach a brief description of any checked boxes separately.
- Diagnosis Codes: Fill in the primary, secondary, and any additional diagnosis codes.
- Course of Treatment: Outline the proposed course of treatment, including the date(s) of treatment requested. Choose the appropriate care path and detail the services requested using CPT/HCPCS/NDC codes.
- Frequency and Duration: Specify the frequency of visits per week and how many weeks of treatment are expected. Calculate and enter the total units of treatment requested.
- Check Attachments: Mark any supporting documents you are including with the form, such as progress notes and medical history.
- Provider Statement: Finally, the treating provider must sign and date the form, confirming that the information is correct.
Once completed, review the form for accuracy before submission. Ensure all attachments are included and clearly labeled for processing.
What You Should Know About This Form
What is the purpose of the Provider Treatment Plan form?
The Provider Treatment Plan form is designed to collect essential information about a patient’s treatment needs, especially in relation to medical claims due to accidents. This includes details about the patient's condition, treatment history, and proposed care paths. Submitting this form ensures that the appropriate insurance coverage is accessed for the patient's treatment plan.
Who needs to fill out the form?
The form must be completed by the treating provider. This could be a physician or other healthcare professionals involved in the patient's care. The provider ensures that all information is accurate and comprehensive, reflecting the patient's current medical status and treatment plan.
What information is required about the patient?
Several pieces of vital information about the patient are necessary, including their full name, address, date of birth, and insurance details. The form also asks about the patient's medical history, including previous treatments, primary and secondary diagnoses, and any relevant accident details. All of this information helps create a clear picture of the patient’s situation.
What are the sections of the form related to treatment?
The form includes sections where the provider specifies the proposed course of treatment and the requested dates for any treatment. There are also areas to detail the care path selected and to provide specific service request codes, which are crucial for accurate billing and insurance processing.
Are attachments required with this form?
Yes, attachments are often necessary. The form includes checkboxes for various supporting documents such as progress notes, test results, and medical history. Providers must ensure that any relevant documents are included as backup to the information provided on the form.
What happens if false information is submitted?
Submitting false or misleading information can lead to serious consequences. In New Jersey, for instance, individuals who knowingly file fraudulent claims may face both criminal and civil penalties. It’s crucial for providers to be diligent in completing the form accurately to avoid potential legal issues.
How is the form submitted?
The completed Provider Treatment Plan form should be submitted through the specified method outlined by the insurance company—this may be via mail, fax, or an electronic submission portal. Always double-check submission guidelines to ensure a smooth process and timely approval of the treatment plan.
Common mistakes
Completing the Provider Treatment Plan form accurately is essential for effective processing and approval. One common mistake people make is failing to fill out all the required fields. Incomplete information can lead to delays and misunderstandings, impacting both patient care and reimbursement processes. Ensure that all sections, especially those clearly marked, are completed fully to provide a comprehensive view of the patient's status.
Another frequent error involves the patient’s information. Some individuals neglect to double-check the accuracy of names and dates. For instance, misspelled names or incorrect policy numbers can cause considerable confusion. Verifying each entry, particularly the patient’s name, claims number, and dates, is vital to avoid unnecessary complications.
Inaccurate coding can also hinder the processing of claims. The form requires specific diagnosis codes, such as ICD-9 codes, and mistakes in these codes can lead to denial of services. It is crucial to ensure that the correct codes are used for the patient’s conditions. Additionally, providing additional diagnosis codes when necessary can help clarify the patient’s situation and support the requested treatments.
Furthermore, some people overlook the need for supporting documents. The form clearly specifies which attachments are required, such as progress notes or test results. Failing to include these documents can cause claims to be marked as incomplete. Every checkbox checked must correspond with the necessary proof to back up the treatment requests.
Another mistake occurs in the proposed course of treatment section. Not specifying exact dates or failing to detail the treatment types can result in ambiguity. It is important to provide clear and concise information about both dates and the therapeutic modalities planned for the patient.
Lastly, individuals may disregard the fraud prevention notice included on the form. Misrepresenting any information intentionally can lead to significant legal consequences. Therefore, it is important to ensure all statements are truthful and accurate. A thorough review process can prevent any inadvertent errors that may have serious implications.
Documents used along the form
The Provider Treatment Plan form is a crucial document in the healthcare process, particularly when dealing with claims related to medical treatment. It often accompanies several other forms to facilitate a comprehensive understanding of a patient's treatment needs and history. Below are some commonly used forms that are typically linked with the Provider Treatment Plan form.
- Progress Notes: These documents provide a detailed account of each patient visit. They chronicle the patient's condition, treatment provided, and any changes in the treatment plan. This ongoing documentation is essential for tracking progress and adapting treatment as necessary.
- SOAP Notes: This structured format includes sections for Subjective information, Objective findings, Assessment, and Plan of care. SOAP Notes simplify the organization of patient information, enhancing communication among healthcare providers and ensuring consistency in the patient’s care.
- Test Results: Results from diagnostic tests such as lab work, X-rays, MRIs, or other assessments are critical for making treatment decisions. These results supplement the treatment plan by providing objective data on the patient's health status.
- Medical History: This form outlines the patient's past medical conditions, surgeries, medications, and allergies. A thorough medical history helps providers make informed decisions about current treatment approaches and avoid potential risks.
- Prescriptions: Documentation of medications prescribed to the patient informs all parties of the treatment regimen. It ensures continuity in medication management and aids in monitoring possible interactions or side effects.
In conclusion, while the Provider Treatment Plan form serves as a vital framework for outlining a patient's care, these additional documents play an important role in providing a more detailed picture of the patient's health and treatment journey. Together, they enable healthcare providers to collaborate effectively and ensure optimal patient care.
Similar forms
- Medical History Form: This document collects a patient's previous medical background, treatments, and conditions, similar to the treatment plan's focus on a patient's medical history and diagnoses.
- Progress Notes: These notes provide ongoing documentation of a patient's treatment and response to care, much like the treatment plan details the proposed course and expected outcomes from the provider's perspective.
- Referral Form: A referral outlines the need for specialized treatment or assessment, similar to how the treatment plan articulates the necessity of specific services based on the patient's condition.
- Claim Submission Form: This form is used to submit billing information to insurance providers, paralleling the treatment plan’s necessity for accurate patient and treatment details to facilitate proper billing.
- Patient Consent Form: This document secures patient agreement for treatment, which complements the treatment plan by ensuring that the patient understands the proposed interventions and agrees to them.
- Follow-up Care Plan: Like the initial treatment plan, this document outlines ongoing treatment strategies after a patient's initial evaluation, helping ensure continuity of care.
- Insurance Authorization Request: This request for approval from an insurance provider is similar to the treatment plan's need for detailed treatment parameters to secure appropriate authorization for planned services.
Dos and Don'ts
Filling out the Provider Treatment Plan form requires attention to detail and accuracy. Here are four essential dos and don'ts to keep in mind:
- Do: Fill out all required fields completely. Incomplete information can delay processing and may lead to claim rejection.
- Do: Use legible handwriting or type the information. This ensures that the information is easily readable by all parties involved.
- Do: Review the completed form thoroughly before submission. Check for any errors or missing details to avoid complications later.
- Do: Attach any necessary supporting documents. This includes progress notes, test results, and medical history, if applicable.
- Don't: Use abbreviations or shorthand that may confuse the reader. Clarity is essential for accurate processing.
- Don't: Ignore the provider statement section. Failure to sign and date this section can invalidate the submission.
- Don't: Provide false or misleading information. This can result in serious legal consequences due to fraud prevention regulations.
- Don't: Forget to verify the patient information. Ensuring that all details, including names and dates, are correct is crucial for a successful claim.
Misconceptions
Understanding the Provider Treatment Plan form is crucial for both providers and patients. However, several misconceptions can cloud its purpose and functionality. Here are five common myths, along with clarifications:
- Misconception: The form is only for initial treatments.
- Misconception: Patients do not need to provide any personal information.
- Misconception: The form doesn't need supporting documents.
- Misconception: Once submitted, the form cannot be changed.
- Misconception: Only the provider needs to sign the form.
This assumption overlooks the fact that the Provider Treatment Plan can also be submitted for follow-up treatments. Both initial and subsequent submissions provide necessary updates on the patient's condition and care.
While it may seem unnecessary, providing accurate personal information is vital. This includes details like the patient's name, address, and insurance information, which play a key role in processing claims and ensuring proper care.
In fact, many sections of the form require supporting attachments. For instance, if certain services were checked, a brief description and the date provided must be included on a separate attachment, ensuring comprehensive documentation.
Although it is important to submit accurate information, corrections can be made if an error is discovered after submission. Providers have options to amend submissions, ensuring that all information remains up-to-date and accurate.
While the provider's signature is crucial, patients should also be aware of the process. Their understanding of what is being submitted on their behalf can enhance transparency and help avoid confusion regarding their treatment.
Key takeaways
Completing the Provider Treatment Plan form accurately is essential for ensuring that medical services are properly documented and billed. Below are key takeaways to assist in the process:
- Clarity is Crucial: Ensure that all information is filled out legibly. Using a typewriter or printing in block letters can help avoid confusion.
- Accurate Patient Information: Double-check the patient's name, address, and birthdate. Errors in this section can lead to significant billing issues.
- Policyholder Details: If the policyholder differs from the patient, provide complete and accurate information for them, including name and address.
- Diagnosis Codes: Include all relevant diagnosis codes. This is crucial for insurance processing and helps to justify the treatment plan.
- Proposed Treatment Plan: Clearly outline the proposed course of treatment. Indicate the dates of treatment requested and the expected frequency of visits.
- Check Appropriate Care Path: Mark the applicable care path carefully. This helps in streamlining the treatment process through the correct channels.
- Attachments Matter: Remember to check any applicable attachments such as progress notes or test results. Missing documents can delay claims approval.
- Fraud Prevention Awareness: Be mindful of the warnings regarding false information. Providing misleading information can result in severe penalties.
- Provider Statement: Ensure that the provider signs and dates the form after reviewing all information for accuracy. This endorsement is crucial for the legitimacy of the submission.
By adhering to these guidelines, submitting the Provider Treatment Plan form becomes a smoother process that benefits both the provider and the patient.
Browse Other Templates
Car Accident Release of Liability Form - By agreeing to a private settlement, you are bypassing lengthy legal processes.
Homeschool Attendance Tracker - Include the student's full name, including first, middle, and last names.
Mutual of Omaha Life Insurance Phone Number - Ensuring eligibility and entitlement is vital when filing for accidental death benefits.