Fill Out Your Psychotherapy Form
Psychotherapy serves as a vital tool for individuals seeking to navigate complex emotional landscapes and enhance their mental well-being. The Client Psychotherapy Intake Form plays a crucial role in this process, guiding both client and therapist towards a productive therapeutic relationship. By requesting personal information, health history, and past therapeutic experiences, this form establishes a comprehensive overview of the client’s current mindset and lifestyle. Key areas include general health, emotional challenges, and family mental health history, ensuring that critical factors affecting the client's mental health are addressed. Additionally, the form emphasizes confidentiality and outlines the limits of such protection, which helps instill trust between the client and therapist. As the client documents relevant experiences, from sleep habits to significant life changes, they offer insight into their unique circumstances. Ultimately, filling out this form is an integral step in preparing for meaningful dialogue and effective interventions during therapy sessions.
Psychotherapy Example
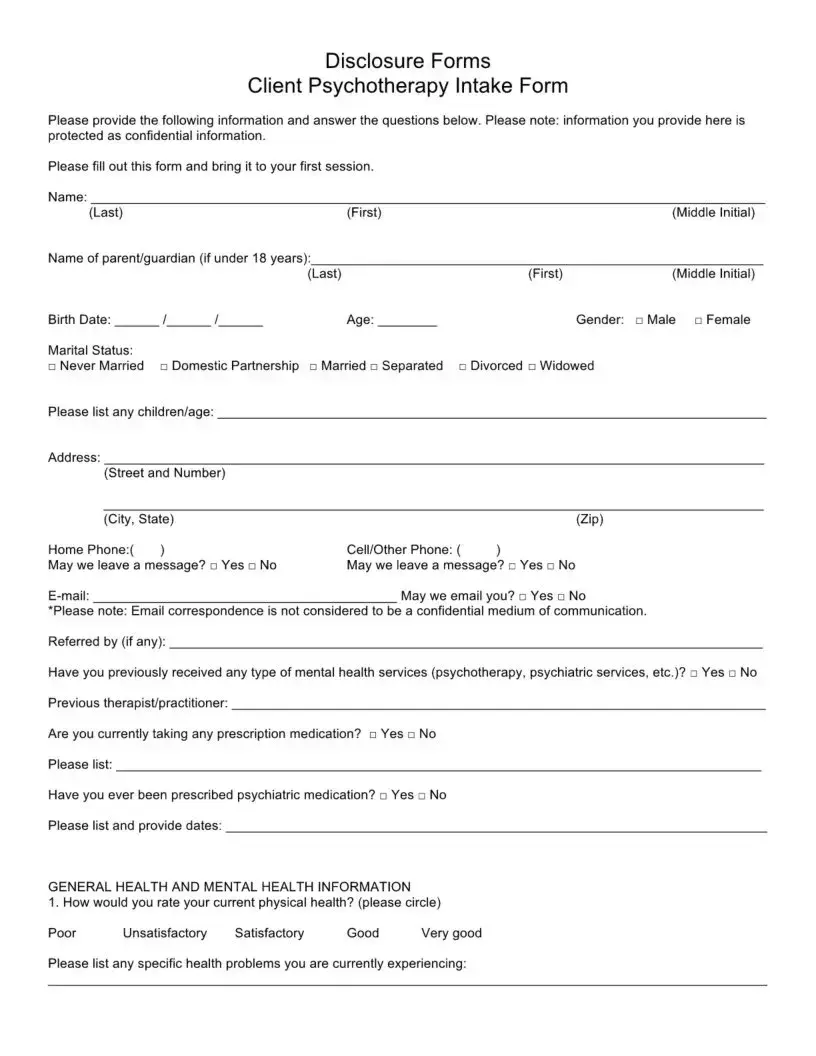
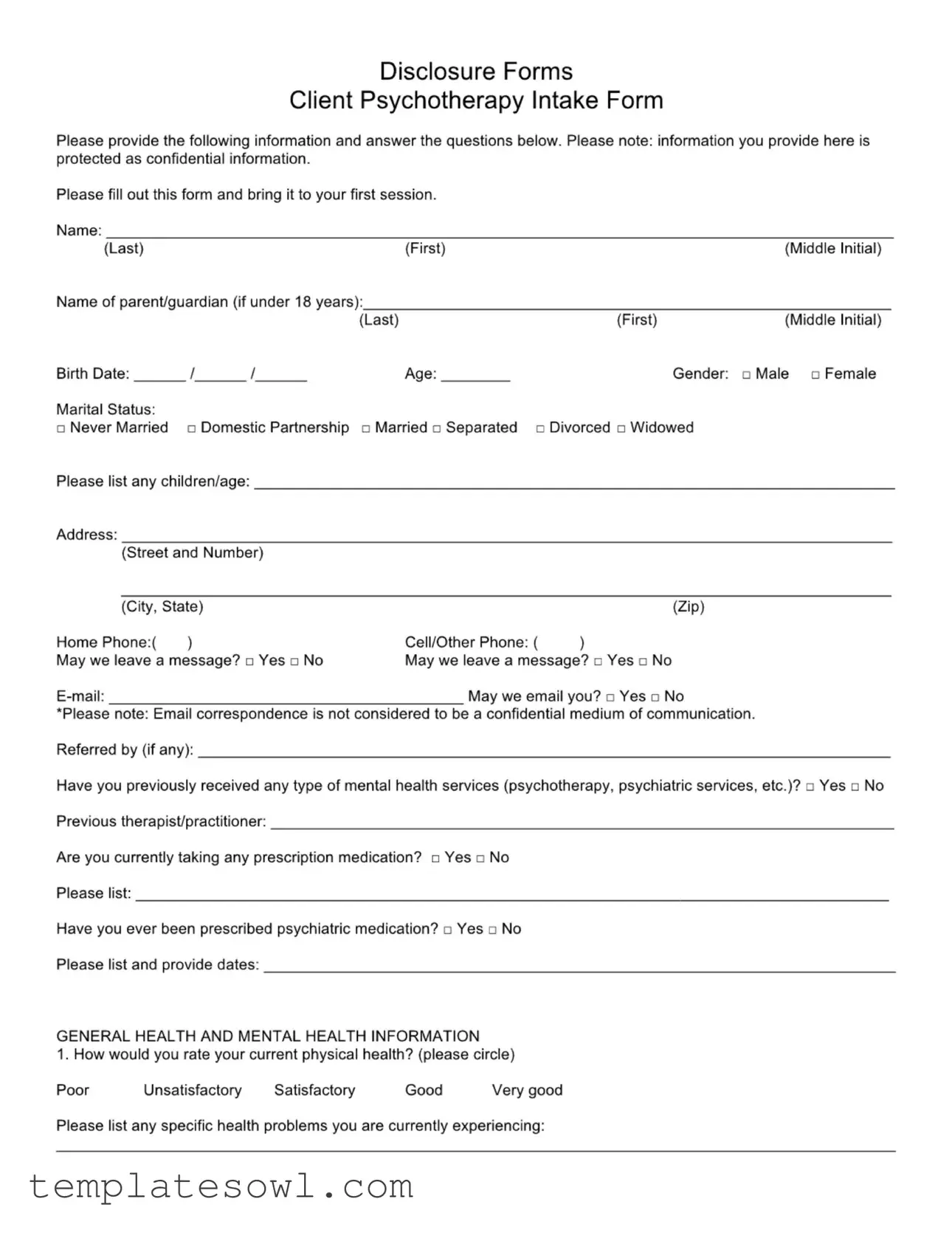
Disclosure Forms
Client Psychotherapy Intake Form
Please provide the following information and answer the questions below. Please note: information you provide here is protected as confidential information.
Please fill out this form and bring it to your first session.
Name: |
|
|
(Last) |
(First) |
(Middle Initial) |
Name of parent/guardian (if under 18 years):
|
|
|
(Last) |
(First) |
(Middle Initial) |
Birth Date: |
/ |
/ |
Age: |
Gender: |
□ Male □ Female |
Marital Status:
□Never Married □ Domestic Partnership □ Married □ Separated □ Divorced □ Widowed
Please list any children/age:
Address:
(Street and Number) |
|
|
|
(City, State) |
|
(Zip) |
|
Home Phone:( |
) |
Cell/Other Phone: ( |
) |
May we leave a message? □ Yes □ No |
May we leave a message? □ Yes □ No |
||
|
May we email you? □ Yes □ No |
||
*Please note: Email correspondence is not considered to be a confidential medium of communication.
Referred by (if any):
Have you previously received any type of mental health services (psychotherapy, psychiatric services, etc.)? □ Yes □ No
Previous therapist/practitioner:
Are you currently taking any prescription medication? □ Yes □ No
Please list:
Have you ever been prescribed psychiatric medication? □ Yes □ No
Please list and provide dates:
GENERAL HEALTH AND MENTAL HEALTH INFORMATION
1. How would you rate your current physical health? (please circle)
Poor |
Unsatisfactory |
Satisfactory |
Good |
Very good |
Please list any specific health problems you are currently experiencing:
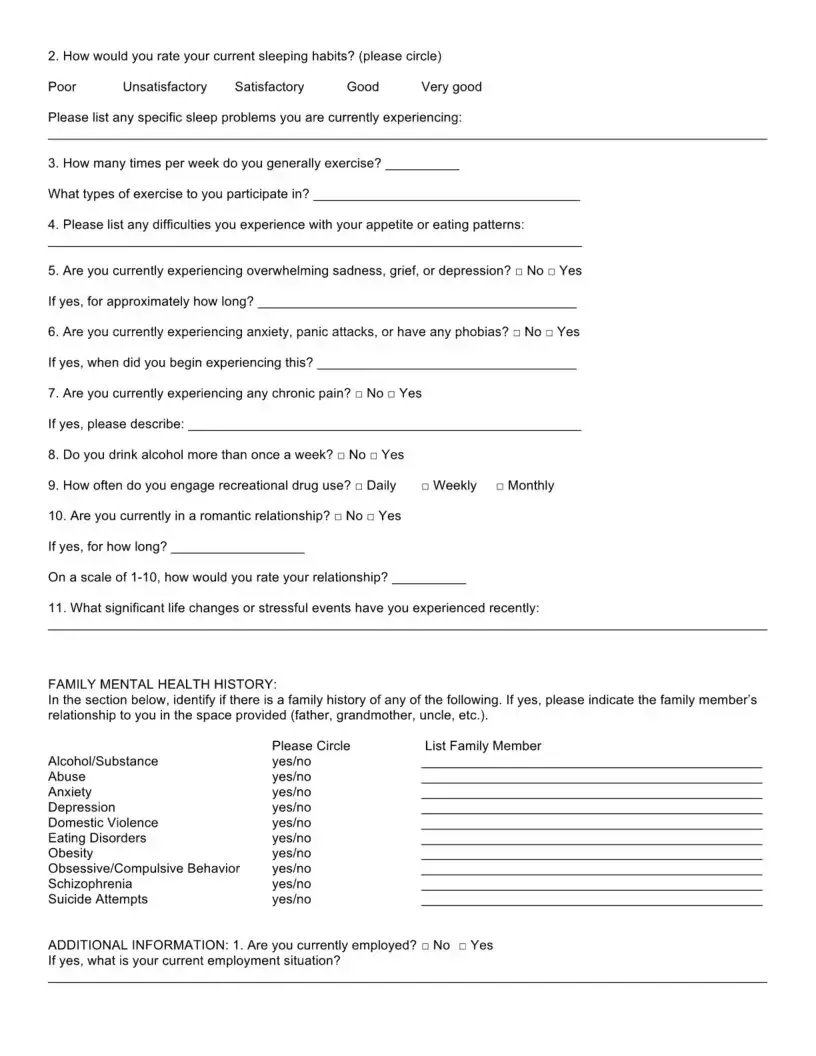
2. How would you rate your current sleeping habits? (please circle)
Poor |
Unsatisfactory |
Satisfactory |
Good |
Very good |
Please list any specific sleep problems you are currently experiencing:
3.How many times per week do you generally exercise? What types of exercise to you participate in?
4.Please list any difficulties you experience with your appetite or eating patterns:
5.Are you currently experiencing overwhelming sadness, grief, or depression? □ No □ Yes If yes, for approximately how long?
6.Are you currently experiencing anxiety, panic attacks, or have any phobias? □ No □ Yes If yes, when did you begin experiencing this?
7.Are you currently experiencing any chronic pain? □ No □ Yes
If yes, please describe:
8. Do you drink alcohol more than once a week? □ No □ Yes
9. How often do you engage recreational drug use? □ Daily |
Weekly |
Monthly |
10.Are you currently in a romantic relationship? □ No □ Yes If yes, for how long?
On a scale of
11.What significant life changes or stressful events have you experienced recently:
FAMILY MENTAL HEALTH HISTORY:
In the section below, identify if there isPlea familyse Circlehistory of any of theListfollowingFamily Member. If yes, please indicate the family member’s Alcohol/Substancerelationship to you in the space providedyes/no(father, grandmother, uncle, etc.).
Abuse |
yes/no |
Anxiety |
yes/no |
Depression |
yes/no |
Domestic Violence |
yes/no |
Eating Disorders |
yes/no |
Obesity |
yes/no |
Obsessive/Compulsive Behavior |
yes/no |
Schizophrenia |
yes/no |
Suicide Attempts |
yes/no |
ADDITIONAL INFORMATION: 1. Are you currently employed? □ No □ Yes
If yes, what is your current employment situation?
Do you enjoy your work? Is there anything stressful about your current work?
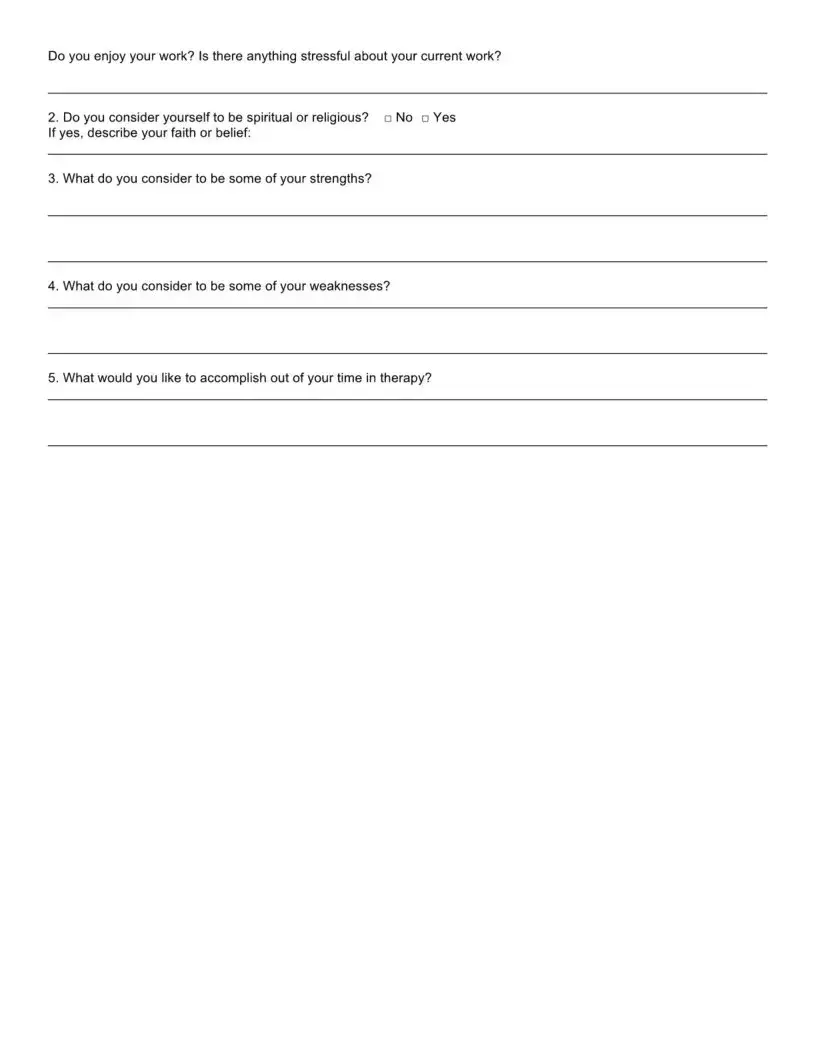
2. Do you consider yourself to be spiritual or religious? |
No Yes |
If yes, describe your faith or belief: |
|
3. What do you consider to be some of your strengths?
4.What do you consider to be some of your weaknesses?
5.What would you like to accomplish out of your time in therapy?
Disclosure Forms
Limits of Confidentiality
Contents of all therapy sessions are considered to be confidential. Both verbal information and written records about a client cannot be shared with another party without the written consent of the client or the client’s legal guardian. Noted exceptions are as follows:
Duty to Warn and Protect
When a client discloses intentions or a plan to harm another person, the mental health professional is required to warn the intended victim and report this information to legal authorities. In cases in which the client discloses or implies a plan for suicide, the health care professional is required to notify legal authorities and make reasonable attempts to notify the family of the client.
Abuse of Children and Vulnerable Adults
If a client states or suggests that he or she is abusing a child (or vulnerable adult) or has recently abused a child (or vulnerable adult), or a child (or vulnerable adult) is in danger of abuse, the mental health professional is required to report this information to the appropriate social service and/or legal authorities.
Prenatal Exposure to Controlled Substances
Mental Health care professionals are required to report admitted prenatal exposure to controlled substances that are potentially harmful.
Minors/Guardianship
Parents or legal guardians of
Insurance Providers (when applicable) Insurance companies and other
Information that may be requested includes, but is not limited to: types of service, dates/times of service, diagnosis, treatment plan, description of impairment, progress of therapy, case notes, and summaries.
I agree to the above limits of confidentiality and understand their meanings and ramifications.
Client Signature (Client’s Parent/Guardian if under 18)
Today’s Date
Disclosure Forms
Cancellation Policy
If you fail to cancel a scheduled appointment, we cannot use this time for another client and you will be billed for the entire cost of your missed appointment. A full session fee is charged for missed appointments or cancellations with less than a
Thank you for your consideration regarding this important matter.
Client Signature (Client’s Parent/Guardian if under 18)
Today’s Date
AUTHORIZATION FOR USE OR DISCLOSURE OF
PROTECTED HEALTH INFORMATION
(Page 1 of 2)
1. Client’s name:
First Name |
Middle Name |
Last Name |
2.Date of Birth: / /
3.Date authorization initiated: / /
4.Authorization initiated by:
Name (client, provider, or other)
5. Information to be released:
Authorization for Psychotherapy Notes ONLY (Important: If this authorization is for Psychotherapy Notes, you must not use it as an authorization for any other type of protected health information.)
6.Purpose of Disclosure: The reason I am authorizing release is: My request
Other (describe):
7.Person(s) Authorized to Make the Disclosure:
8.Person(s) Authorized to Receive the Disclosure:
9. This Authorization will expire on |
/ / |
or upon the happening of the following event: |
Authorization and Signature: I authorize the release of my confidential protected health information,
as described in my directions above. I understand that this authorization is voluntary, that the information to be disclosed is protected by law, and the use/disclosure is to be made to conform to my directions. The information that is used and/or disclosed pursuant to this authorization may be re disclosed by the recipient unless the recipient is covered by state laws that limit the use and/or disclosure of my confidential protected health information.
Signature of the Patient
Signature of Personal Representative Relationship to Patient if Personal Representative
Date of signature
PATIENT RIGHTS AND HIPAA AUTHORIZATIONS
(Page 2 of 2)
The following specifies your rights about this authorization under the Health Insurance Portability and Accountability Act of 1996, as amended from time to time (“HIPAA").
1.Tell your mental health professional if you don’t understand this authorization, and they will explain it to you.
2.You have the right to revoke or cancel this authorization at any time, except: (a) to the extent information has already been shared based on this authorization; or (b) this authorization was obtained as a condition of obtaining insurance coverage. To revoke or cancel this authorization, you must submit your request in writing to your mental health professional and your insurance company, if applicable.
3.You may refuse to sign this authorization. Your refusal to sign will not affect your ability to obtain treatment, make payment, or affect your eligibility for benefits. If you refuse to sign this authorization, and you are in a
4.Once the information about you leaves this office according to the terms of this authorization, this office has no control over how it will be used by the recipient. You need to be aware that at that point your information may no longer be protected by HIPAA.
5.If this office initiated this authorization, you must receive a copy of the signed authorization.
6.Special Instructions for completing this authorization for the use and disclosure of Psychotherapy Notes. HIPAA provides special protections to certain medical records known as "Psychotherapy Notes.” All Psychotherapy Notes recorded on any medium (i.e., paper, electronic) by a mental health professional (such as a psychologist or psychiatrist) must be kept by the author and filed separate from the rest of the client’s medical records to maintain a higher standard of protection. “Psychotherapy Notes” are defined under HIPAA as notes recorded by a health care provider who is a mental health professional documenting or analyzing the contents of conversation during a private counseling session or a group, joint, or family counseling session and that are separate from the rest of the individual’s medical records. Excluded from the “Psychotherapy Notes” definition are the following: (a) medication prescription and monitoring, (b) counseling session start and stop times, (c) the modalities and frequencies of treatment furnished, (d) the results of clinical tests, and (e) any summary of: diagnosis, functional status, the treatment plan, symptoms, prognosis, and progress to date.
In order for a medical provider to release “Psychotherapy Notes” to a third party, the client who is the subject of the Psychotherapy Notes must sign this authorization to specifically allow for the release of Psychotherapy Notes. Such authorization must be separate from an authorization to release other medical records.
Form Characteristics
| Fact Title | Description |
|---|---|
| Confidentiality | Client information is protected as confidential, ensuring privacy and security during therapy sessions. |
| Legal Guardian Consent | If the client is a minor, a parent or legal guardian must provide consent and may access the client’s records. |
| Limits of Confidentiality | There are notable exceptions, such as the duty to warn in cases of imminent harm or abuse. |
| Emergency Cancellation Policy | Clients will be billed for missed appointments without 24-hour notice, except in cases of illness or emergencies. |
| Previous Mental Health Services | Clients must disclose if they have previously received mental health services, which can inform current treatment. |
| Health and Wellness Assessment | A section assesses both physical and mental health to tailor therapy to individual needs. |
| Email Communication | Clients are informed that email is not considered a secure or confidential mode of communication. |
| Family Mental Health History | Understanding family mental health history helps therapists form a more complete picture of the client’s situation. |
Guidelines on Utilizing Psychotherapy
Completing the Psychotherapy form is an important step in starting your journey. To ensure the therapist has all the necessary information, fill out the form carefully and honestly. Bring the completed form with you to your first session.
- Personal Information: Fill in your name, birth date, age, and gender. If you are under 18, include your parent or guardian's name.
- Marital Status: Select your current marital status and list any children along with their ages.
- Contact Information: Provide your address, home phone number, and cell phone number. Indicate if messages can be left at either number.
- Email: Enter your email address and indicate if you would like to receive emails.
- Referral: Note who referred you to this therapy service, if applicable.
- Mental Health History: Answer whether you have received mental health services before and provide any relevant details.
- Current Medications: State if you are currently taking any prescription medications and list them if applicable.
- General Health: Rate how you feel about your physical health and sleep habits. List any specific issues you've encountered.
- Exercise and Eating Habits: Describe your exercise routine and any problems with appetite or eating patterns.
- Current Mental State: Answer questions related to sadness, anxiety, chronic pain, alcohol consumption, and drug use.
- Relationship Status: Indicate if you are in a romantic relationship and rate its quality.
- Family Mental Health History: Specify if there’s a family history of mental health issues and identify the relationship to you.
- Employment and Spirituality: State your employment status and share if you consider yourself spiritual or religious.
- Personal Assessment: Reflect on your strengths and weaknesses, and articulate what you hope to achieve through therapy.
- Signature: Sign and date the form at the end, indicating your understanding of the limits of confidentiality and cancellation policy.
What You Should Know About This Form
What is the purpose of the Psychotherapy Intake Form?
The Psychotherapy Intake Form is designed to gather important information about clients before they begin therapy. It assists therapists in understanding clients' backgrounds, mental health history, and current concerns. This information helps create a personalized treatment plan that meets the client's specific needs.
Is the information on the form confidential?
Yes, the information provided on the Psychotherapy Intake Form is considered confidential. Therapists are required to protect clients' privacy and cannot share information with others without written consent. However, there are specific exceptions where disclosure is required, such as in cases involving threats to others, child abuse, or harm to oneself.
What should I do if I have questions while filling out the form?
If you have questions while completing the Psychotherapy Intake Form, it is advisable to reach out to the therapist's office for clarification. Most offices have staff members who are available to assist you with any uncertainties regarding the questions or the information required.
Are there any specific health issues that I should disclose?
It is important to disclose any current health issues or mental health concerns you may have. This can include physical health problems, chronic pain, sleep issues, or emotional difficulties such as anxiety or depression. Providing comprehensive information allows the therapist to better understand your situation and tailor their approach accordingly.
What if I am uncomfortable sharing certain information?
If you feel uncomfortable providing certain details, it is essential to communicate this feeling to your therapist. Open dialogue can foster trust, and therapists can work with you to ensure you feel safe and respected during the process. It’s common for clients to feel apprehensive, and therapists are trained to create a supportive environment.
Will my insurance company receive information from this form?
If applicable, insurance providers may request certain information from the Psychotherapy Intake Form for billing and reimbursement purposes. This could include details about the type of service, diagnosis, treatment plan, and progress notes. Clients should be aware that sharing information with insurance providers typically requires prior consent.
What are the consequences of missing an appointment?
If you miss a scheduled appointment without canceling at least 24 hours in advance, there may be financial implications. The entire cost of the session will typically be billed to you. This policy is enacted so that therapists can manage their schedules effectively and accommodate other clients who may need appointments.
Common mistakes
When filling out the Psychotherapy Intake Form, one common mistake is providing incomplete personal information. Clients sometimes forget to include critical details such as their middle initial or contact information. Even minor omissions can hinder effective communication and may result in delays for their first appointment.
Another frequent error involves misrepresenting previous mental health treatments. Some individuals may select "No" when they have indeed received therapy or psychiatric services before. This not only affects the therapist's understanding of the client’s background but also delays the tailored treatment approach necessary for effective care.
People often struggle with the health and mental health sections of the form. They may either rate their health too optimistically or pessimistically, failing to provide an accurate picture of what they are experiencing. Clarity in these responses is vital for the mental health professional to develop an appropriate treatment plan that meets each client's needs.
Additionally, clients frequently skip questions or provide vague answers in the family mental health history section. This can lead to a misunderstanding of genetic predispositions or familial patterns that might impact their mental health. It is essential to take time to reflect on their family history to provide comprehensive information.
Finally, many individuals tend to overlook the importance of thoroughly reading the confidentiality section. Understanding what is confidential and what is not helps set realistic expectations about privacy during therapy sessions. A lack of clarity in this area may lead to discomfort or hesitation in sharing sensitive information later on.
Documents used along the form
The psychotherapy form is a critical document in the therapeutic process, serving as a foundation for a client's treatment. However, it is often accompanied by several other forms and documents that further clarify the therapeutic relationship and outline important policies. Below is a brief overview of some of these additional documents commonly utilized alongside the psychotherapy form.
- Informed Consent Form: This document details the nature of therapy, the rights and responsibilities of both therapist and client, and the potential risks and benefits of treatment. It ensures clients understand what therapy involves before they begin.
- Insurance Information Form: Designed to collect information about the client's insurance coverage, this form helps facilitate billing for services. It may include details about the insurance provider, policy number, and the client’s responsible party for payments.
- Emergency Contact Form: This form captures information about who to contact in case of an emergency. It typically includes the name, relationship, and phone number of the individual, ensuring that the therapist can reach out if there's an urgent situation.
- Progress Notes: These are internal records created by the therapist during or after sessions. They document the client’s progress, treatment plans, and any specific issues discussed, helping track the therapeutic journey and inform future sessions.
- Termination/Closure Form: When therapy ends, this document outlines the reasons for termination and any follow-up steps. It ensures clients receive closure and can transition smoothly if further services are needed.
- Client Rights and Responsibilities: This form clarifies clients' rights regarding their treatment, including confidentiality and the ability to voice concerns. It reinforces the ethical commitment of the therapist to provide respectful and competent care.
Each of these documents plays a significant role in creating a safe and structured environment for therapy. Understanding them helps clients engage more actively in their treatment and fosters a collaborative relationship between therapist and client.
Similar forms
Client Intake Form: Similar to the Psychotherapy form, this document gathers essential personal details about a client. It may ask for information such as demographics, medical history, and insurance details to create a comprehensive profile.
Medical History Form: Like the Psychotherapy form, this document aims to understand health risks and previous treatments. It covers past medical conditions, medications, and allergies, aligning with mental health considerations.
Consent to Treat Form: This document, much like the Psychotherapy form, establishes an agreement between the client and the practitioner. It explains the nature of treatment and confirms the client’s consent to receive services.
Confidentiality Agreement: Similar in its intention to the Disclosure Forms section, this document explains what information is confidential. It outlines the limitations of confidentiality, ensuring the client understands their privacy rights.
Release of Information Form: Much like the Disclosure Forms, this document allows clients to authorize the sharing of their health information with specified individuals or organizations, ensuring clients maintain control over their personal data.
Emergency Contact Form: This form is similar in that it gathers essential information about whom to contact in case of an emergency. It ensures that the mental health professional has a reliable way to reach a client’s support network when needed.
Referral Form: Like the referral section in the Psychotherapy form, this document tracks who referred the client. It can help in understanding the client’s background and their journey to seeking help.
Medication Management Form: This document aligns closely with the medication inquiries in the Psychotherapy form. It collects information about current and past medications, ensuring the practitioner has a complete view of the client’s treatment history.
Client Feedback Form: Similar to evaluating therapy sessions, this form gathers client feedback on their experiences. It aims to improve future services and helps practitioners adapt to client needs based on their input.
Discharge or Termination Form: This document, like the cancellation section, outlines the procedures when therapy concludes. It addresses any follow-up care and clarifies any remaining responsibilities for the client.
Dos and Don'ts
When filling out the Psychotherapy form, it is important to follow certain guidelines to ensure clarity and accuracy. Below are some do's and don'ts to keep in mind.
- Do: Provide accurate and truthful information to ensure effective treatment.
- Do: Complete all required sections of the form, including health history and medication details.
- Do: Use clear handwriting if filling out a paper form or ensure legible typing if filling it out electronically.
- Do: Bring the form to your first session to facilitate a smooth intake process.
- Don't: Skip questions or sections unless they are marked as optional.
- Don't: Provide vague or general answers; be specific to give the therapist a clear understanding of your situation.
- Don't: Forget to indicate if you have prior therapy experience, as this information is critical to your treatment plan.
- Don't: Wait until your first session to fill out the form; complete it beforehand to maximize your time with the therapist.
Misconceptions
Misconceptions about psychotherapy forms can lead to confusion and hinder the therapeutic process. Understanding these misconceptions is vital for anyone preparing to fill out a psychotherapy form.
- All information will be shared with others. Many individuals worry that their personal information will not remain confidential. However, psychotherapy forms often emphasize that the information is protected and will not be disclosed without consent, unless there are safety concerns.
- Filling out the form is unnecessary. Some believe that they can enter therapy without completing the required forms. In reality, these forms help therapists understand clients’ needs and backgrounds, ensuring a more effective treatment plan.
- Only severe issues require a psychotherapy form. It’s a common belief that only those with serious mental health issues need to fill out these forms. However, anyone seeking therapy, regardless of their situation, should provide this information for proper assessment.
- The form is just a formality. While it might seem like a simple paperwork task, the psychotherapy form plays a crucial role in establishing a therapeutic relationship and guiding the course of treatment.
- Info on the form is permanent and cannot be changed. Many people fear that once they submit their answers, they cannot update their information. In fact, clients can revise information during sessions as their situation evolves or new details emerge.
Understanding these points can alleviate concerns and promote a more open and productive therapeutic process.
Key takeaways
Understanding the Psychotherapy Intake Form is essential for a smooth start to your therapeutic journey. Here are some key takeaways to keep in mind:
- Confidentiality is Important: The information you provide is private. Your therapist cannot share it without your consent, except in specific situations where there is potential harm to yourself or others.
- Fill It Out Completely: Be thorough when answering questions. This information helps your therapist understand your needs and create a personalized treatment plan.
- Be Honest About Your History: Disclose any previous mental health services and medications. Your past experiences can influence your current treatment.
- Assess Your Health: Take time to rate your physical and mental health honestly. Consider how you manage your sleep, appetite, and any ongoing pain.
- Highlight Family History: If any family members have had mental health issues, note them. This can provide valuable insight into patterns and risks.
- Set Goals for Therapy: Think about what you want to achieve in therapy. Sharing your goals can help guide the therapy process effectively.
Browse Other Templates
Long Shoreman Jobs - Submitting interest in casual work is your first step toward potential employment.
26-1880 - This form is a key tool for enhancing the security of your benefit payments.
Af 910 - Previous editions of the form are now obsolete and should not be used.