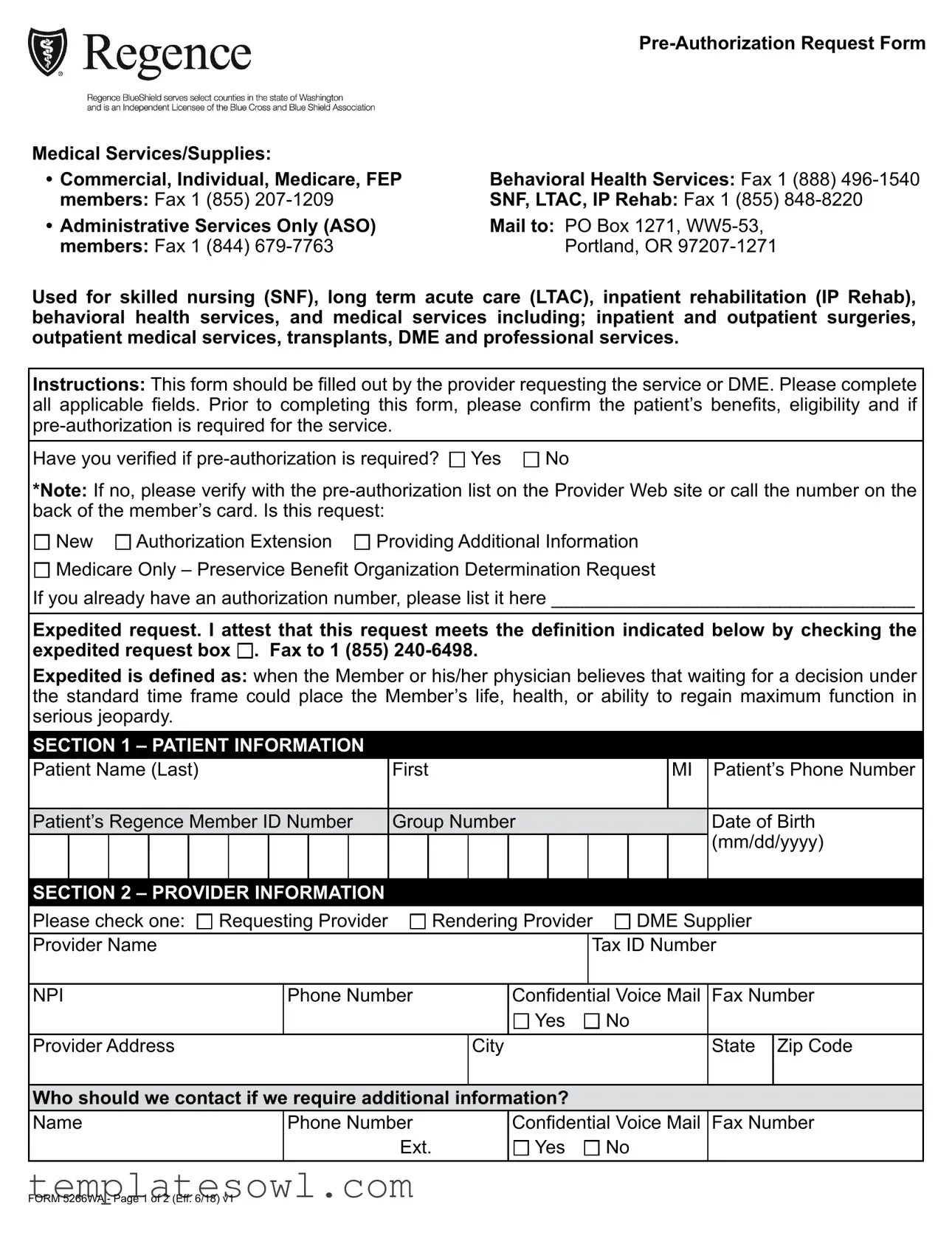
Fill Out Your Regence Blue Cross Authorization Request Form
The Regence Blue Cross Authorization Request form is a vital tool for healthcare providers seeking pre-authorization for various medical services and supplies. This form is applicable to a range of areas including skilled nursing, long-term acute care, inpatient rehabilitation, and behavioral health services, as well as both inpatient and outpatient medical procedures. Providers must accurately fill out all relevant sections, ensuring that patient benefits and eligibility are verified prior to submission. The form allows for new requests, authorization extensions, and the provision of additional information. Notably, it features a section for expedited requests, which can be crucial when a patient's life or health may be at serious risk due to waiting times for approval. Specific information such as patient details, provider information, and the nature of the requested services must be clearly indicated. Additionally, necessary clinical documentation should accompany the request to support the medical necessity criteria. With an emphasis on precise and comprehensive submissions, the Regence Blue Cross Authorization Request form facilitates a smooth approval process for necessary medical care.
Regence Blue Cross Authorization Request Example
Medical Services/Supplies: |
|
Commercial, Individual, Medicare, FEP |
Behavioral Health Services: Fax 1 (888) |
members: Fax 1 (855) |
SNF, LTAC, IP Rehab: Fax 1 (855) |
Administrative Services Only (ASO) |
Mail to: PO Box 1271, |
members: Fax 1 (844) |
Portland, OR |
Used for skilled nursing (SNF), long term acute care (LTAC), inpatient rehabilitation (IP Rehab), behavioral health services, and medical services including; inpatient and outpatient surgeries, outpatient medical services, transplants, DME and professional services.
Instructions: This form should be filled out by the provider requesting the service or DME. Please complete all applicable fields. Prior to completing this form, please confirm the patient’s benefits, eligibility and if
Have you verified if
*Note: If no, please verify with the
New Authorization Extension Providing Additional Information
Medicare Only – Preservice Benefit Organization Determination Request
If you already have an authorization number, please list it here ___________________________________
Expedited request. I attest that this request meets the definition indicated below by checking the expedited request box . Fax to 1 (855)
Expedited is defined as: when the Member or his/her physician believes that waiting for a decision under the standard time frame could place the Member’s life, health, or ability to regain maximum function in serious jeopardy.
SECTION 1 – PATIENT INFORMATION |
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||
Patient Name (Last) |
|
|
|
|
|
First |
|
|
|
|
|
|
|
MI |
Patient’s Phone Number |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient’s Regence Member ID Number |
Group Number |
|
|
|
|
Date of Birth |
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(mm/dd/yyyy) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION 2 – PROVIDER INFORMATION |
|
|
|
|
|
|
|
|
|
|
|||||||||
Please check one: Requesting Provider |
Rendering Provider DME Supplier |
||||||||||||||||||
Provider Name |
|
|
|
|
|
|
|
|
|
|
|
Tax ID Number |
|||||||
|
|
|
|
|
|
|
|
|
|||||||||||
NPI |
|
|
Phone Number |
|
|
Confidential |
Voice Mail |
Fax Number |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
No |
|
||||
Provider Address |
|
|
|
|
|
|
|
City |
|
|
|
|
|
State Zip Code |
|||||
Who should we contact if we require additional information?
Name
Phone Number
Ext.
Confidential Voice Mail
Yes No
Fax Number
FORM 5266WA - Page 1 of 2 (Eff. 6/18) v1
SECTION 3 – PREAUTHORIZATION REQUEST
Is this request:
|
Date of Service (if scheduled) __________________ (mm/dd/yyyy) |
|
|
||||||||
Please check one: Outpatient Hospital |
|
Inpatient |
ASC |
Office |
|
|
|
|
|||
|
Other____________________________________ |
|
|
|
|
||||||
Please check all that apply: Surgical |
DME Diagnostic |
Medical |
|
|
|||||||
|
|
Other____________________________________ |
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
||
Rendering or Treating Provider and Provider Specialty |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
||
Physical Address where services will occur |
City |
|
|
State |
|
Zip Code |
|||||
|
|
|
|
|
|
|
|
|
|
||
IF INPATIENT OR OUTPATIENT FACILITY |
|
|
IF |
DME |
|
|
|||||
Facility Name |
|
|
|
Company Name |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|||
Anticipated Admission |
Anticipated Length of stay |
Tax ID Number |
|
NPI |
|
|
|||||
(mm/dd/yyyy) |
|
|
|
|
|
|
|
|
|
|
|
Note: If anticipated length of stay is not indicated, no |
DME Address |
|
|
|
|
||||||
more than two days will be assigned if approved. |
|
|
|
|
|
|
|||||
|
|
|
|
|
City |
|
|
State |
|
Zip Code |
|
Note: This form does not serve as a notification of |
|
|
|
|
|
|
|||||
Signed copy of prescription attached: Yes No |
|||||||||||
admission. Please reference the Provider Web site for |
|||||||||||
instructions to notify us of an admission. |
|
|
Invoice attached: Yes No |
|
|
||||||
Please provide all diagnosis, CPT® or HCPCS codes |
and their descriptions, if available; this will help |
||||||||||
processing of your request. |
|
|
|
|
|
|
|
|
|||
Diagnosis code(s) and description(s) |
|
CPT® or HCPCS code(s) and description(s) |
DME Only Line |
||||||||
|
|
|
|
|
|
|
|
|
Item Cost |
||
Primary: |
|
|
|
|
|
|
|
$ |
|||
Second: |
|
|
|
|
|
|
|
$ |
|||
Third: |
|
|
|
|
|
|
|
$ |
|||
Please submit the following clinical documentation with this form as appropriate for this request:
History & Physical Lab/Radiology/Testing Results Current Symptoms & Functional Impairments
Treatment History and any other information such as chart notes that support medical necessity for the request.
FORM 5266WA - Page 2 of 2 (Eff. 6/18) v1
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is utilized for pre-authorization requests related to medical services and supplies, including skilled nursing and inpatient rehabilitation. |
| Eligibility | The requesting provider must ensure the patient's benefits and eligibility are verified prior to completing the form. |
| Submission Methods | Requests can be submitted via fax, with dedicated numbers for different services, or mailed to the specified address in Portland, OR. |
| Expedited Requests | Providers may check an expedited request box if waiting for a standard decision could jeopardize the member's health or recovery. |
| Required Fields | The form requires specific fields to be filled out, including patient information, provider details, and the nature of the request. |
| Required Documentation | Clinical documentation such as lab results and treatment history must accompany the request to demonstrate medical necessity. |
| Contact Information | A section for additional contact information is included, allowing the provider to specify who should be contacted for any further inquiries. |
| Governing Laws | This form is governed by Washington State laws and regulations regarding health insurance and patient care. |
| Form Updates | The version of this form is effective as of June 18, 2022, and is subject to updates as needed to comply with current regulations. |
Guidelines on Utilizing Regence Blue Cross Authorization Request
Once you have gathered the necessary information, filling out the Regence Blue Cross Authorization Request form is a straightforward process. This form is essential for requesting pre-authorization for medical services, including skilled nursing, surgeries, and behavioral health services. Below are the steps to help you complete the form efficiently.
- Confirm the patient's benefits and eligibility to ensure pre-authorization is required for the requested service.
- Indicate on the form whether the request is new, an authorization extension, providing additional information, or specifically for Medicare.
- If applicable, note the existing authorization number.
- If this is an expedited request, check the appropriate box and ensure you meet the criteria for expedited status.
- Fill in the patient's information, including their name, phone number, Regence member ID, group number, and date of birth.
- Provide your information as the provider, indicating whether you are the requesting provider, rendering provider, or DME supplier.
- List your provider name, tax ID number, NPI, phone number, and address details.
- Designate who should be contacted for additional information and provide their contact information.
- Specify whether the pre-authorization request is a pre-service or concurrent review, and note the date of service if applicable.
- Check the type of service being requested: outpatient hospital, inpatient, ASC, office, or other.
- Indicate the nature of the request by checking all relevant boxes, such as surgical, DME, diagnostic, or medical.
- Provide the rendering or treating provider's physical address where the services will occur.
- If applicable, specify details for DME, including company name, anticipated admission date, and anticipated length of stay.
- List diagnosis, CPT® or HCPCS codes, and their descriptions related to the request.
- Note the line item costs for DME, if applicable.
- Attach clinical documentation that supports the medical necessity of the request, such as history and physical, lab results, treatment history, and other relevant information.
After completing the form, it should be faxed to the appropriate number provided in the instructions based on the type of services requested. It's important to ensure all relevant attachments and documentation are included to facilitate a smooth approval process.
What You Should Know About This Form
What is the Regence Blue Cross Authorization Request form used for?
This form is used to request pre-authorization for various medical services and supplies. It covers skilled nursing facilities, long-term acute care, inpatient rehabilitation, behavioral health services, and both inpatient and outpatient surgeries. It also includes requests for outpatient medical services, transplants, durable medical equipment (DME), and professional services.
Who needs to fill out this form?
The form must be filled out by the healthcare provider requesting the service or durable medical equipment. It is important for the provider to complete all applicable fields to ensure the request is processed smoothly.
What should I do before filling out the form?
Before completing the form, you need to confirm the patient’s benefits and eligibility. It is also essential to check if pre-authorization is required for the service being requested. This can be done by checking the pre-authorization list on the Provider Web site or by calling the number found on the back of the member’s card.
What information should I include about the patient?
Include the patient's full name, phone number, Regence Member ID number, group number, and date of birth. This information is critical for identifying the patient and processing the request accurately.
What types of requests can I submit with this form?
You can submit a new pre-authorization request, request an authorization extension, or provide additional information. If it is a Medicare-only inquiry, you can also request a preservice benefit organization determination.
What is an expedited request?
An expedited request is necessary when waiting for a decision could seriously impact the member's health or ability to regain maximum function. To submit an expedited request, check the expedited request box on the form and fax it to the designated number.
What clinical documentation do I need to attach?
You should attach relevant clinical documentation that supports the medical necessity of the request. This may include the medical history and physical examination results, lab tests, current symptoms, functional impairments, and treatment history. Additional information, such as chart notes, can also be helpful.
Where should I send the completed form?
Depending on the type of request, the form should be faxed to the appropriate number listed on the form or mailed to the provided address. Always verify that you are sending it to the correct location to avoid delays.
How do I know if my request was approved?
Once you submit the request, you will need to await a response from Regence Blue Cross. They will reach out if they need any additional information or to inform you of the decision regarding your request.
Common mistakes
Filling out the Regence Blue Cross Authorization Request form can be challenging, and mistakes can lead to delays or denials in obtaining necessary services. One common error is failing to check whether pre-authorization is actually required. Many people skip this step, assuming all requests need approval. The form clearly instructs users to verify the patient’s benefits and eligibility before proceeding. Skipping this verification can result in unexpected complications.
Another frequent mistake arises from incomplete patient information. Omitting critical details like the patient's Regence Member ID number, phone number, or birth date can hinder processing. Each field plays a vital role, and missing information can lead to misunderstandings or delays. Ensuring meticulous completion of this section is key to a smooth authorization process.
A third common oversight involves the clinical documentation submitted alongside the request. Many providers forget to include necessary documentation, such as history and physical reports or lab results. Without these, the review may be delayed, as the reviewers may need to reach out for additional information. Clinical documentation supports the medical necessity of the request, so it is crucial to gather and submit all relevant records.
Finally, some individuals fail to indicate whether their request is for a new service or an extension. This detail clarifies the intent of the request and helps expedite the review process. Incorrectly marking this option can lead to confusion and unnecessary delays. Pay careful attention to this checkbox to ensure clarity and precision in the submission.
Documents used along the form
The Regence Blue Cross Authorization Request form is essential for obtaining pre-authorization for various medical services and supplies. Along with this form, several other documents may be required or recommended to ensure a complete and accurate request. Below is a list of these accompanying forms and documents, each serving its distinct purpose in the authorization process.
- Patient Consent Form: This document provides the necessary consent from the patient, allowing healthcare providers to share their medical information with the insurance company. It protects patient privacy while facilitating communication.
- Clinical Summary: A brief overview of the patient's medical history, current conditions, and treatment plan. This summary helps the insurer understand the necessity of the requested services.
- Physician's Letter of Medical Necessity: A letter from the treating physician that outlines why a specific treatment or service is necessary for the patient's health. It typically includes clinical evidence to support the request.
- Billing Statement: This document details the costs associated with the services requested. It provides transparency regarding the financial aspects of the treatment, allowing the insurer to review the charges.
- Diagnostic Results: Results from recent lab tests or imaging studies that are relevant to the request. These results offer objective evidence to support the need for the proposed services.
- Medication List: A comprehensive list of medications the patient is currently taking. This helps the insurance provider assess any potential interactions and determine the appropriateness of the requested treatment.
- Treatment History: Documentation of the patient's past treatments and responses. This information helps establish how the patient's condition has evolved and the effectiveness of previous therapies.
- Pre-Authorization Checklist: A checklist that outlines all necessary forms and information required for the authorization request. This ensures that nothing is overlooked, streamlining the submission process.
Submitting these documents alongside the Regence Blue Cross Authorization Request form can enhance the likelihood of a timely and favorable decision. Always ensure that all required information is accurate and complete to facilitate the best outcome for the patient's healthcare needs.
Similar forms
- Prior Authorization Request Form: Similar to the Regence Blue Cross Authorization Request form, this document is used to obtain approval before certain medical services are performed, ensuring that the proposed services meet the insurance company's medical necessity criteria.
- Insurance Claim Form: This document is submitted after services are provided, detailing the medical procedures and costs incurred. Like the Authorization Request, it requires clear information about the patient and provider to facilitate processing.
- Referral Form: Used when a primary care physician refers a patient to a specialist. This form, akin to the Authorization Request, often requires information about the patient's health history and the reason for the referral.
- Medical Necessity Form: This document outlines the clinical justification for specific treatments or procedures, similar in purpose to the Authorization Request. Both forms aim to substantiate that the service requested is necessary for the patient's health.
- Predetermination of Benefits Form: This is requested to determine what benefits will be covered for a proposed treatment before it is performed. It parallels the authorization request as both are proactive steps to understand coverage.
- Continuity of Care Form: Used when transitioning between providers or facilities, this ensures that the patient's care continues without interruption. Like the Authorization Request, it emphasizes the importance of documentation and communication.
- Patient Information Release Form: This document allows healthcare providers to share a patient’s medical records. It is similar as both require patient consent and relevant details for processing and approval.
- Benefit Investigation Form: This is utilized to ascertain coverage specifics for a patient’s treatment options. It's comparable to the Authorization Request in that both serve to clarify the patient's benefits and coverage limitations before services are rendered.
Dos and Don'ts
When filling out the Regence Blue Cross Authorization Request form, there are several important considerations to keep in mind. Here’s a list of recommendations to ensure a smooth submission process.
- Do verify patient benefits and eligibility before completing the form. This helps ensure that the request will be processed efficiently.
- Do complete all applicable fields. Providing incomplete information may delay the authorization process.
- Do attach all necessary clinical documentation that supports the medical necessity of the request. This includes history and physical exams, lab results, and treatment history.
- Do check for pre-authorization requirements on the provider web site or by calling the number listed on the member’s card to avoid any surprises later.
- Don’t submit the form without double-checking all information provided. Errors may lead to rejection or delays.
- Don’t forget to confirm if the request is new or an extension of a previous authorization. This distinction is essential for proper processing.
- Don’t ignore the expedited request option if there are urgent health concerns. Ensure you check the appropriate box and justify the need for urgent processing.
- Don’t assume that additional documentation is unnecessary. Always attach supplementary materials that reinforce the request's validity.
By following these guidelines, you will enhance your chances of a successful authorization request with Regence Blue Cross.
Misconceptions
Misconceptions about the Regence Blue Cross Authorization Request form can lead to confusion and potential delays in receiving necessary services. Understanding the realities surrounding the form can simplify the process for everyone involved. Here are ten common misconceptions:
- Misconception 1: Filling out the form is optional.
- Misconception 2: Only large hospitals need to use the form.
- Misconception 3: The form guarantees approval.
- Misconception 4: Pre-authorization is the same as a referral.
- Misconception 5: I can submit the form anytime.
- Misconception 6: It is enough to provide basic patient information.
- Misconception 7: The form is only for inpatient services.
- Misconception 8: You don’t need to confirm patient eligibility.
- Misconception 9: Completing the expedited request section is straightforward.
- Misconception 10: You do not need to follow up after submission.
Many believe that the authorization request form is merely a suggestion. However, submitting this form is essential for obtaining prior approval for certain medical services and supplies.
Smaller providers often think this form does not apply to them. In reality, any provider requesting pre-authorization must fill it out, regardless of practice size.
Completing the form does not guarantee that the request will be approved. Approval is contingent upon the specifics of the case and alignment with coverage policies.
There is an important distinction between a referral and pre-authorization. A referral facilitates access to a specialist, while pre-authorization is a requirement for certain services to be covered.
While the form can be submitted at any time, it is crucial to consider deadlines, especially for scheduled services. Delays in submission may lead to interferences in care.
Merely providing basic information might not suffice. Comprehensive details—including diagnosis codes, medical necessity documentation, and provider information—are vital for review.
Some individuals think this form is exclusively for inpatient services. It applies to various services, including outpatient surgeries, durable medical equipment, and behavioral health services.
Assuming eligibility is unnecessary can be problematic. Before completing the form, providers should verify the patient's benefits and eligibility to ensure a smoother process.
While checking the expedited request box may seem simple, providers must be certain that the situation meets defined criteria to avoid complications.
Many assume that submitting the form is the end of the process. Following up can be vital to ensure all required information is received and to check the status of the request.
Key takeaways
The Regence Blue Cross Authorization Request form is crucial for obtaining necessary medical services and supplies. Here are key takeaways to consider when filling out and using the form:
- Complete the Form Accurately: Ensure all applicable fields are filled out thoroughly. This includes patient information, provider details, and the specifics of the preauthorization request.
- Check Pre-Authorization Requirements: Before completing the form, confirm whether pre-authorization is required for the service. Utilize the pre-authorization list provided on the Provider Web site or contact the number on the member’s card.
- Indicate the Nature of the Request: Select whether the request is new, an authorization extension, or providing additional information. This helps in processes management.
- Use Expedited Requests Wisely: If the situation is urgent, check the expedited request box. This should only be used when waiting for a decision might jeopardize the member’s health or recovery.
- Provide Detailed Patient Information: Include complete details such as the patient’s name, Regence Member ID, date of birth, and contact number. Accurate information is essential for smooth processing.
- Attach Required Documentation: Include relevant clinical documentation like history and physical notes, lab results, treatment history, and any other supporting materials that demonstrate medical necessity.
- Avoid Delays: Ensure to submit the form and any attachments via the correct fax numbers based on the type of services requested. Correct submission can significantly reduce processing time.
Browse Other Templates
Exterior Painting Contractor - The form includes obligations from both the contractor and the client to ensure a clear understanding of responsibilities.
Cotc Transcript Request - Complete this form to access your official COTC transcripts.
Fair Rental Value Calculator 2023 - The form ensures that the final calculations reflect the family's share of rent and the PHA's contribution accurately.