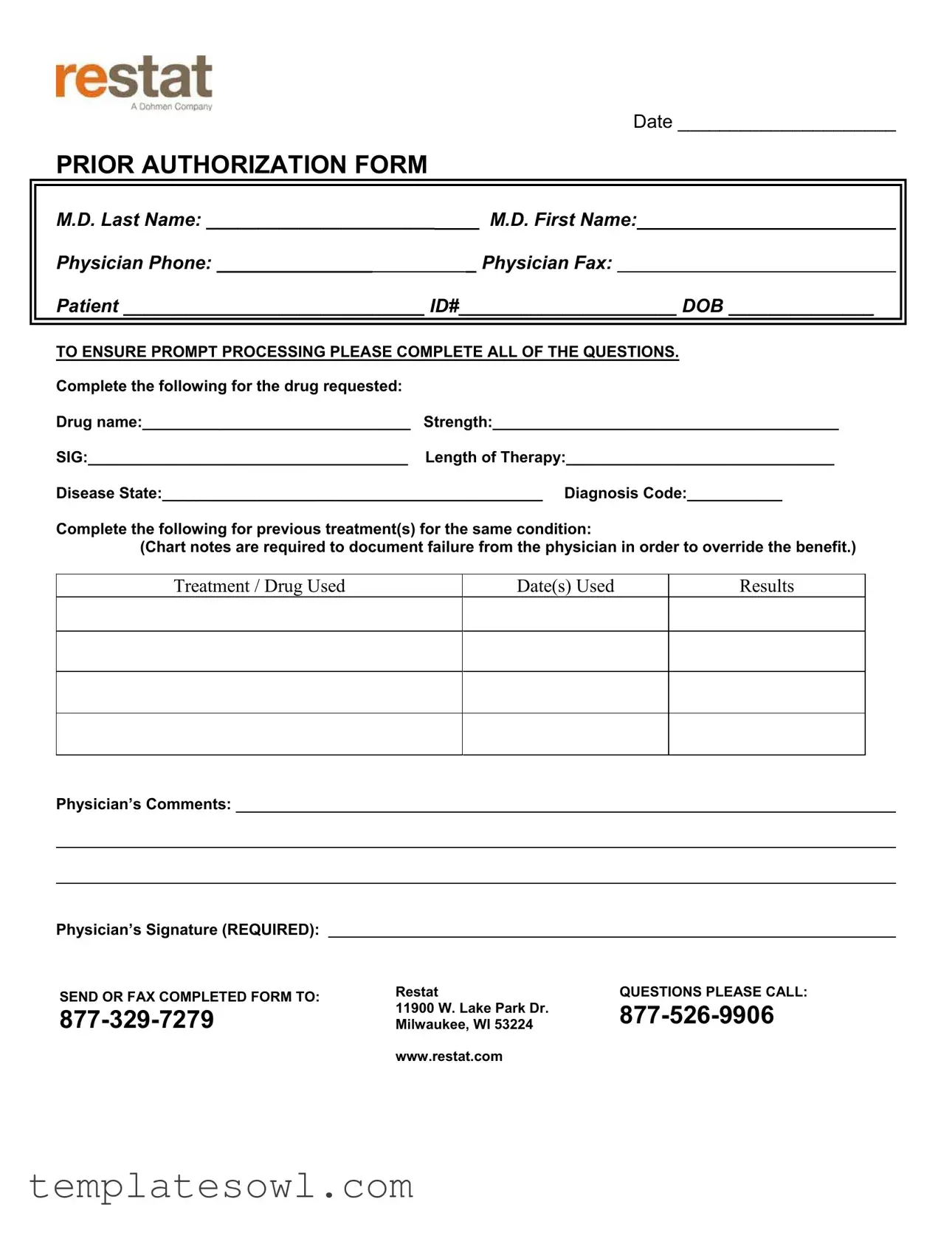
Fill Out Your Restat Prior Authorization Form
The Restat Prior Authorization form serves as a critical tool in the healthcare landscape, facilitating the approval process for specific medical treatments and medications. This comprehensive document requires detailed information from physicians to ensure that requests for prior authorization are processed efficiently. Essential elements include the physician's name, contact information, and patient details such as ID number and date of birth. The form also necessitates specifics regarding the drug being requested, including its name, strength, and length of therapy. Additionally, healthcare providers must document previous treatments, detailing any prior medications used, dates of use, and the results to justify the request. Submitting complete and accurate information is vital, as incomplete forms may delay authorization. The form must be signed by the physician, affirming the accuracy of the information provided. Once completed, it can be sent via fax or mail to the designated Restat office, where further inquiries can be directed. This process ensures that patients receive timely access to necessary treatments while maintaining compliance with insurance protocols.
Restat Prior Authorization Example
|
|
|
|
|
|
|
DATE _____________________ |
||||
|
|
PRIOR AUTHORIZATION FORM |
|
|
|
|
|
|
|
|
|
|
|
M.D. Last Name: ______________________ |
|
|
M.D. First Name: |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Physician Phone: _______________ |
|
|
_ Physician Fax: |
|
|
||||
Patient _____________________________ ID#_____________________ DOB ______________
TO ENSURE PROMPT PROCESSING PLEASE COMPLETE ALL OF THE QUESTIONS.
Complete the following for the drug requested: |
|
Drug name:_______________________________ |
Strength:________________________________________ |
SIG:_____________________________________ |
Length of Therapy:_______________________________ |
Disease State:____________________________________________ Diagnosis Code:___________
Complete the following for previous treatment(s) for the same condition:
(Chart notes are required to document failure from the physician in order to override the benefit.)
Treatment / Drug Used
Date(s) Used
Results
Physician’s Comments:
Physician’s Signature (REQUIRED):
SEND OR FAX COMPLETED FORM TO: |
Restat |
QUESTIONS PLEASE CALL: |
|
11900 W. Lake Park Dr. |
|
||
Milwaukee, WI 53224 |
|||
|
www.restat.com |
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Date Requirement | The form must include the date when it is completed to ensure proper tracking of the authorization request. |
| Physician Information | Both the last name and first name of the physician must be provided along with their phone and fax numbers to facilitate communication. |
| Patient Identification | Patient details including ID number and date of birth are essential to link the authorization request to the correct individual. |
| Drug Details | The form requires specific information about the requested drug, including name, strength, and length of therapy. |
| Previous Treatments | Documentation of prior treatments for the same condition is necessary. This includes the treatment/drug used, dates of use, and results. |
| Submission Process | The completed form must be sent via fax or mail to Restat's office in Milwaukee, WI, ensuring it reaches the proper department. |
Guidelines on Utilizing Restat Prior Authorization
After completing the Restat Prior Authorization form, it will be sent to the designated address or fax number for review. It is important to ensure that all sections are fully filled out to prevent delays in processing. Follow the steps below to accurately complete the form.
- Write the date at the top of the form.
- Fill in the physician's last name and first name.
- Enter the physician's phone number and fax number.
- Provide the patient's name, ID number, and date of birth.
- For the drug requested, fill out the following:
- Drug name
- Strength
- SIG (directions for use)
- Length of therapy
- Disease state
- Diagnosis code
- Complete the section regarding previous treatment(s):
- List the treatment/drug used
- Input the dates used
- Summarize the results
- Add physician's comments
- Have the physician sign the form in the designated area.
- Send or fax the completed form to Restat using the provided contact information.
What You Should Know About This Form
What is the Restat Prior Authorization form?
The Restat Prior Authorization form is a document that physicians use to request approval for specific medications before they are prescribed. This process helps ensure that the treatments align with the patient’s needs and health insurance guidelines.
Who needs to fill out the Restat Prior Authorization form?
The form must be completed by the physician who is prescribing the medication. It's designed to capture essential information about the drug, patient details, and previous treatments that justify the need for prior authorization.
What information is required on the form?
Physicians need to provide their names, contact information, and details about the patient, including the patient’s ID number and date of birth. Additionally, specific information about the medication requested, previous treatments, and the physician's signature are required.
Why are previous treatments documented on the form?
Documenting previous treatments is essential to show that the patient has tried other options that were not effective. Insurance providers may require this information to justify the need for a more expensive or alternative medication.
How does the prior authorization process work?
After the physician completes the Restat Prior Authorization form, it is submitted to Restat for review. The request is assessed based on insurance criteria, and once a decision is made, the physician is notified about the approval or denial.
What happens if the prior authorization is denied?
If a request is denied, the physician can appeal the decision. This may involve submitting additional documentation or providing further justification for the necessity of the treatment. Communication between the physician and insurance is critical during this process.
How can I check the status of my prior authorization?
To check the status, you can contact Restat directly at the provided phone numbers. It's helpful to have the patient's information and reference number ready when making the call for faster assistance.
Can I expedite the prior authorization process?
While there are circumstances where urgent requests may be considered, completing the form accurately and thoroughly is vital for prompt processing. It's crucial that all required fields are filled out to avoid delays.
Where do I send the completed form?
Once the form is completed, it should be sent or faxed to Restat at the address provided on the form. Ensure to double-check the contact information to avoid miscommunication.
What should I do if I have questions about the form?
If you have questions regarding the Restat Prior Authorization form or the process itself, you can call the customer service numbers listed on the form for assistance. The representatives are available to guide you through any uncertainties.
Common mistakes
When filling out the Restat Prior Authorization form, attention to detail is crucial. One common mistake is not providing complete patient information. Including each piece of required information, such as the patient’s name, ID number, and date of birth, is essential. Omitting details can delay the authorization process significantly.
Another frequent error is failing to specify the drug requested accurately. The form requires the drug name, strength, and SIG. Errors in this section can lead to confusion and potentially result in denials or delays. Be clear and precise.
Incomplete information about previous treatments is also problematic. The form asks for details on prior medications used, including dates and results. Providing vague or missing treatment history can weaken the case for prior authorization. Doctors must clearly document failures and outcomes linked to previous therapy.
Patients and physicians sometimes overlook the importance of the physician’s comments on the effectiveness of past treatments. This section holds weight in justifying the need for the new medication. By neglecting to fill this out, you risk leaving a significant void in the application.
Finally, failings can occur if the physician's signature is missing. This is a required part of the authorization process. Without it, the form is incomplete and cannot be processed. Ensure that all sections, especially the signature, are finalized before submission.
Documents used along the form
The Restat Prior Authorization form is an essential document used to manage requests for medication coverage. Alongside this form, several other documents play a crucial role in ensuring a smooth and comprehensive authorization process. Each document serves a specific purpose, contributing to the overall efficiency of handling prior authorization requests.
- Clinical Notes: These notes provide detailed information about the patient’s medical history and prior treatments. They are critical for demonstrating medical necessity and supporting the claimed need for the requested drug.
- Medication History Report: This report outlines all medications the patient has taken recently. It helps the reviewing authority see the effectiveness of previous treatments and the rationale behind requesting a new drug.
- Clearance Letter: This letter from referring specialists or previous physicians may validate the need for a new treatment. It includes professional opinions that can strengthen the authorization request.
- Formulary Exception Request: If the medication is not on the insurance company's formulary, this request outlines justifications for the necessity of using a non-formulary drug. It details why alternatives will not suffice.
- Patient Consent Form: This is necessary to confirm that the patient is aware of the prior authorization request and consents to the disclosure of their medical information to assist in the review process.
- Billing Information Form: This document ensures the correct billing practices are followed for medications. It includes insurance details and billing codes necessary for claim processing.
- Appeal Letter: If a prior authorization request is denied, this letter can be used to formalize an appeal. It should address the reasons for denial and argue for the medical necessity of the requested treatment.
Incorporating these documents into the prior authorization submission not only streamlines the review process but also enhances the chance of approval. A thorough and well-documented approach fosters better communication among healthcare providers, insurers, and patients.
Similar forms
The Restat Prior Authorization form has similarities with several other important documents used in healthcare. Each of these forms serves to facilitate communication between healthcare providers and insurance companies to ensure necessary treatments are authorized. Here’s a list of nine documents that are similar in purpose or function:
- Prior Authorization Request Form: This form is specifically used for obtaining approval from an insurance company before a treatment or medication can be covered. Much like the Restat form, it requires detailed patient and physician information.
- Medical Necessity Documentation: Physicians submit this documentation to justify the need for a treatment. Similar to Restat, it must outline the patient's condition and rationale for the prescribed therapy.
- Prescription Drug Prior Authorization Form: This document specifically requests authorization for prescription medications. It mirrors the Restat form in requiring drug details and patient diagnosis.
- Claims Appeal Form: This document is used when a claim for payment is denied. While it focuses on appealing a decision, it shares the need for comprehensive patient and treatment information, akin to Restat.
- Patient History Form: This form gathers comprehensive medical background on a patient. Like the Restat form, it collects critical details that inform treatment decisions and prior therapy attempts.
- Treatment Authorization Request: Used to gain pre-approval for a specific treatment plan, this form aligns closely with the Restat, needing similar patient and treatment information.
- Drug Utilization Review Form: This form assesses the appropriateness of prescribed medications. It is similar in that it evaluates past treatments and outcomes, enhancing patient safety.
- Clinical Evaluation Form: Often used to assess a patient’s eligibility for certain treatments, this form parallels the Restat in its emphasis on detailed evaluations and treatment histories.
- Referral Request Form: This document initiates a referral process to a specialist. While it differs slightly in intent, it involves patient details and clinical justification similarly to the Restat form.
Understanding these documents helps clarify how health services function and reinforces the importance of thorough communication in patient care.
Dos and Don'ts
When filling out the Restat Prior Authorization form, there are several key points to consider that will ensure a smoother process. Below is a compiled list of dos and don’ts to guide you:
- Do fill out the form completely, ensuring that all sections are addressed fully.
- Do provide accurate and up-to-date patient information, including the ID number and date of birth.
- Do include specific details about the drug requested, such as the drug name, strength, and dosing instructions.
- Do submit any required chart notes that demonstrate previous treatments and their results.
- Don't leave any questions or fields blank, as incomplete forms may result in delays.
- Don't forget to include the physician's signature, as it is mandatory for processing.
- Don't hesitate to reach out to Restat’s customer service for questions about the form or submission process.
Misconceptions
There are several misconceptions that often arise regarding the Restat Prior Authorization form. Understanding the truth behind these ideas can help streamline the process and ensure accurate submissions. Here are six common myths explained:
- Misconception 1: The form is optional.
- Misconception 2: Any physician can sign the form.
- Misconception 3: Previous treatments do not need to be documented.
- Misconception 4: The form can be submitted without additional patient information.
- Misconception 5: It doesn't matter how the form is submitted.
- Misconception 6: Approval is guaranteed after submission of the form.
Many believe that submitting the Restat Prior Authorization form is optional. In reality, this form is a vital part of acquiring necessary medications that may not be covered without prior authorization. Completing the form correctly is essential for the approval process.
It is crucial to note that the form must be signed by the prescribing physician managing the patient's care. Signatures from other healthcare providers may not be accepted, as they are required to ensure informed medical decisions.
Some people think that details of prior drug treatments are irrelevant. However, documenting previous treatments and their outcomes is necessary to justify the need for the requested medication. This helps in processing the request more efficiently.
Complete information is crucial for processing the prior authorization. Missing patient details, such as ID number or date of birth, can delay the approval or result in a denial of the request.
Submission methods matter greatly. While the form can be sent by fax or mail, timely submission is critical for prompt processing. Using the recommended channels ensures that the request is handled efficiently.
Submitting the Restat Prior Authorization form does not guarantee that a request will be approved. The authorization depends on medical necessity and adherence to guidelines set by the insurance provider.
Addressing these misconceptions can lead to a smoother prior authorization process and ultimately benefit patients in need of timely medication access.
Key takeaways
Filling out the Restat Prior Authorization form is an important step in ensuring patients receive the necessary medications without delays. Here are key takeaways to consider:
- Completeness is Crucial: Filling out all sections of the form is essential. Missing information can lead to processing delays. Ensure that all fields are filled, including drug details and patient information.
- Document Previous Treatments: Provide a comprehensive history of previous treatments. Include the treatment names, dates used, and the results to support the authorization request. This can aid significantly in demonstrating the need for the requested medication.
- Physician's Comments Matter: Utilize the space for the physician’s comments effectively. Clear explanations regarding the patient's condition and treatment failures can strengthen the case for prior authorization.
- Submission Methods: Once completed, send the form to Restat via mail or fax. Be aware of the contact information provided on the form for follow-up questions or clarifications.
These steps can substantially improve the chances of a successful authorization request and facilitate timely treatment for patients.
Browse Other Templates
Tarjeta Dorada Application Online - Applicants must be prepared to provide detailed information about all household members.
Cmsnet - Ensure compliance with federal, state, and local laws related to data access.
Get Title From Dmv - It is essential to maintain communication with the Motor Vehicles office throughout the FS-6T process.