Fill Out Your Samba Insurance Claim Form
The Samba Insurance Claim form is a crucial document for members seeking to navigate the claims process efficiently. It encompasses key sections that ensure all necessary information is collected for processing medical claims. You'll start by providing member information, including name, gender, date of birth, and address. Following that, patient details are required, which expand upon the relationship between the member and the patient receiving medical services. The form further includes specific questions regarding the nature of the claim, whether it pertains to an accident, and if there are other insurance coverages involved. Important instructions are provided clearly on the reverse side to facilitate the filing process, guiding users on what to include and highlight after completion. Complying with these instructions is essential to avoid delays in processing. As you navigate through this form, remember to sign off and date to authorize claims processing. Finally, the form also explains that payments can be directed either to healthcare professionals or to members themselves, depending on the circumstances laid out. Overall, the clarity and structured layout of the Samba Insurance Claim form serve to ease what can often be a daunting task.
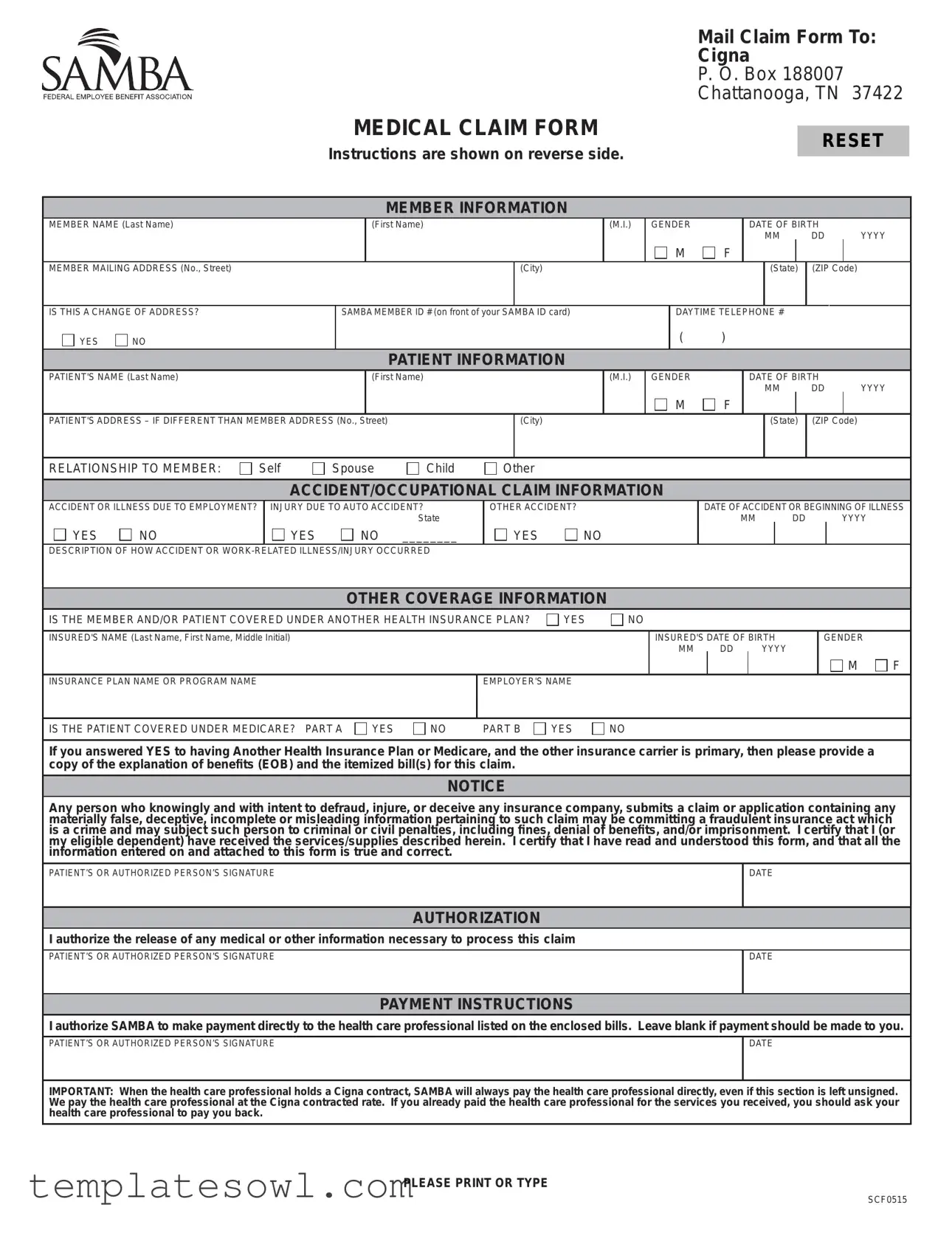
Samba Insurance Claim Example
Mail Claim Form To:
Cigna
P. O. Box 188007
Chattanooga, TN 37422
MEDICAL CLAIM FORM
RESET
Instructions are shown on reverse side.
MEMBER INFORMATION
MEMBER NAME (Last Name)
(First Name)
(M.I.) GENDER
M
F
DATE OF BIRTH
MM DD YYYY
MEMBER MAILING ADDRESS (No., Street)
(City)
(State) (ZIP Code)
IS THIS A CHANGE OF ADDRESS?
YES |
NO |
SAMBA MEMBER ID # (on front of your SAMBA ID card)
DAYTIME TELEPHONE #
( )
PATIENT INFORMATION
PATIENT'S NAME (Last Name)
(First Name)
(M.I.) GENDER
M
F
DATE OF BIRTH
MM DD YYYY
PATIENT'S ADDRESS – IF DIFFERENT THAN MEMBER ADDRESS (No., Street)
(City)
(State) (ZIP Code)
RELATIONSHIP TO MEMBER:
Self
Spouse
Child |
Other |
ACCIDENT/OCCUPATIONAL CLAIM INFORMATION
ACCIDENT OR ILLNESS DUE TO EMPLOYMENT?
YES 
 NO
NO
INJURY DUE TO AUTO ACCIDENT? State
YES |
NO ________ |
OTHER ACCIDENT?
YES |
NO |
DATE OF ACCIDENT OR BEGINNING OF ILLNESS
MM DD YYYY
DESCRIPTION OF HOW ACCIDENT OR
OTHER COVERAGE INFORMATION
IS THE MEMBER AND/OR PATIENT COVERED UNDER ANOTHER HEALTH INSURANCE PLAN?
YES
NO
INSURED'S NAME (Last Name, First Name, Middle Initial)
INSURED'S DATE OF BIRTH
MM DD YYYY
GENDER

 M
M  F
F
INSURANCE PLAN NAME OR PROGRAM NAME
EMPLOYER'S NAME
IS THE PATIENT COVERED UNDER MEDICARE? PART A
YES
NO |
PART B |
YES
NO
If you answered YES to having Another Health Insurance Plan or Medicare, and the other insurance carrier is primary, then please provide a copy of the explanation of benefits (EOB) and the itemized bill(s) for this claim.
NOTICE
Any person who knowingly and with intent to defraud, injure, or deceive any insurance company, submits a claim or application containing any materially false, deceptive, incomplete or misleading information pertaining to such claim may be committing a fraudulent insurance act which is a crime and may subject such person to criminal or civil penalties, including fines, denial of benefits, and/or imprisonment. I certify that I (or my eligible dependent) have received the services/supplies described herein. I certify that I have read and understood this form, and that all the information entered on and attached to this form is true and correct.
PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE
DATE
AUTHORIZATION
I authorize the release of any medical or other information necessary to process this claim
PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE
DATE
PAYMENT INSTRUCTIONS
I authorize SAMBA to make payment directly to the health care professional listed on the enclosed bills. Leave blank if payment should be made to you.
PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE
DATE
IMPORTANT: When the health care professional holds a Cigna contract, SAMBA will always pay the health care professional directly, even if this section is left unsigned. We pay the health care professional at the Cigna contracted rate. If you already paid the health care professional for the services you received, you should ask your health care professional to pay you back.
PLEASE PRINT OR TYPE
SCF0515
INSTRUCTIONS FOR FILING A CLAIM
IMPORTANT
1.Use this form for medical claims. You can find information on how to file Pharmacy or Dental and Vision claims at www.SambaPlans.com.
2.You only need to fill out this form if your health care professional isn't filing the claim for you. Even if not part of the Cigna PPO network
3.If you received this claim form electronically, click to the right of the each field and type in the information. Once done, remember to click on the Reset button on the bottom of page 1 after printing out the completed form.
4.If you are filling the form out by hand, use a new printed form instead of a photocopy. That way we can scan your form and process the claim with no delays. Please print clearly in black ink.
5.We must get your claim by December 31st of the year after the year you received the service.
6.Please use a separate claim form for each health care professional, and for each member of your family. You can get a new blank form by going to www.SambaPlans.com or by calling Customer Service
7.To process your claim, we need your ID number. It's on the front of your SAMBA ID card.
8.We need an itemized bill to process the claim correctly. We can't accept receipts, balance due statements and cancelled checks in place of the itemized bill.
9.Itemized bills must include (see Section 7 of the SAMBA Health Benefit Plan brochure for more information):
Member name |
Type of service/Procedure code |
Date of Service (mm/dd/yyyy) |
Charge for the service |
Patient name |
Diagnosis code (ICD format) |
|
Health care provider signature |
Health care professional name/credentials Health care professional address Health care professional Tax ID number Health care professional NPI number
10.We suggest you make a copy of your bill(s) and your completed claim form for your records.
11.Important: We pay covered claims directly to any health care professional with a Cigna contract. We only send the payment to you when:
–the health care professional doesn't have a contract with Cigna and/or
–you leave the payment instructions section blank.
We reserve the right to request other documents, such as medical records, if we need them before processing your claim.
12.If the patient has other health insurance coverage, and that other insurance is primary and SAMBA secondary, we need an Explanation of Benefits (EOB) for this service from the other insurance company when you send the completed form and itemized bill.
MAILING INSTRUCTIONS
–If you are sending one claim, please don't staple or paper clip the bills to the claim form.
–If you are sending more than one claim in the same envelope, then please use a paper clip to keep the claim form and itemized bills together.
–Send your completed claim form and itemized bills to the address listed on the front of this form.
If you have additional questions, please contact Customer Service at
EXPLANATION OF BENEFITS
Once we have processed the claim, you'll receive an Explanation of Benefits (EOB). The EOB will explain the charges applied to your deductible (the amount you pay for covered services before your plan begins to pay) and any charges you owe your health care professional. Please keep your EOB on file in case you need it in the future.
Form Characteristics
| Fact Name | Description |
|---|---|
| Mailing Address | Claims must be mailed to: Cigna, P.O. Box 188007, Chattanooga, TN 37422. |
| Deadline for Claims | Submit your claim by December 31st of the year following the year you received the service. |
| Signature Requirement | Patient's or authorized person’s signature is required to authorize claim processing. |
| Itemized Bill Requirement | Only itemized bills are acceptable. Do not submit receipts or balance statements. |
| Medicare Coverage | Indicate if the patient has Medicare coverage, including Part A and Part B. |
| Fraud Notice | Submitting false information can lead to severe penalties, including criminal charges. |
| Health Coverage Information | If there is other health insurance, provide the name and date of birth of the insured. |
| State-Specific Laws | Refer to regulations applicable in your state; laws may vary by jurisdiction. |
Guidelines on Utilizing Samba Insurance Claim
Once you have gathered the necessary documentation, filling out the Samba Insurance Claim form is a straightforward process. It is crucial to provide accurate information to ensure timely processing of your claim. By following the steps outlined below, you can complete the form with confidence and send it off correctly.
- Begin by entering your Member Information. Fill in your last name, first name, and middle initial. Indicate your gender, date of birth, and mailing address, including city, state, and ZIP code. If this is a change of address, check "YES" or "NO". Enter your SAMBA Member ID number and daytime telephone number.
- Next, complete the Patient Information. Provide the patient's name in the same format as your own, along with their gender and date of birth. If the patient’s address differs from yours, fill in the patient address section. Specify your relationship to the patient (e.g., self, spouse, child, other).
- Then, move on to the Accident/Occupational Claim Information. Indicate whether the accident or illness was work-related, involved an auto accident, or was due to another accident. Record the date of the accident or the onset of illness and include a brief description of how it occurred.
- In the Other Coverage Information section, indicate if the member or patient is covered under another health insurance plan. If so, provide the insured's name, date of birth, gender, insurance plan name, and employer's name. Also, indicate if the patient is covered under Medicare Parts A or B.
- Read and understand the Notice about fraud, then certify that the services listed are received accurately, signing and dating the section as the patient or authorized person.
- Authorize the release of any necessary medical information by signing and dating the authorization section.
- If you wish for SAMBA to make payment directly to the healthcare professional, sign and date the payment instructions section. If payment should be made to you, leave this section blank.
- Make sure to print clearly. If you filled the form in by hand, use black ink and a fresh printed form. For electronic submissions, carefully type in each field and click 'Reset' when done.
- Attach an itemized bill that meets all listed criteria, ensuring it includes details such as the patient's name, service type, charge, diagnosis code, health care professional's credentials, and contact information.
- Finally, mail your completed claim form and itemized bills to Cigna P. O. Box 188007 Chattanooga, TN 37422. Avoid stapling or clipping bills if sending one claim. Use a paper clip for multiple claims.
After submitting your claim, retain a copy of your completed form and itemized bills for your records. You will receive an Explanation of Benefits (EOB) once your claim has been processed, explaining any charges related to deductibles and your payment obligations.
What You Should Know About This Form
1. What is the purpose of the Samba Insurance Claim form?
The Samba Insurance Claim form is primarily used to request reimbursement for medical services. Members use this form when their healthcare provider does not directly file a claim on their behalf. Completing this form accurately ensures the claim is processed efficiently and payment is made either to the member or directly to the healthcare professional.
2. How should I fill out the Samba Insurance Claim form?
To complete the Samba Insurance Claim form, you need to provide detailed information about the member and the patient, including names, addresses, and date of birth. Sections on accident or occupational claim information must be filled out if applicable. Make sure to include details regarding any other health insurance coverage, including Medicare, if relevant. Using clear, black ink is recommended if filling the form out by hand. Electronic submissions can be made by typing directly into the fields.
3. What documents are required to accompany the claim form?
An itemized bill that outlines the medical services received must be submitted with the claim form. This document should include specific details such as the member's name, type of service, date of service, and the healthcare provider's credentials. If applicable, an Explanation of Benefits (EOB) from the primary insurance provider is also required if the Samba plan is secondary. Receipts or balance statements are not acceptable substitutes for an itemized bill.
4. What are the deadlines for submitting a claim?
Claims should be submitted no later than December 31 of the year following the year in which the service was provided. This deadline is crucial to ensure reimbursement. Submitting claims after this date may result in denial of the claim.
5. Where should I mail the completed claim form?
The completed Samba Insurance Claim form should be mailed to the following address: Cigna P.O. Box 188007 Chattanooga, TN 37422. It is crucial to follow mailing instructions closely to avoid delays. Claims should not be stapled, and if submitting multiple claims, a paper clip can be used to organize the documents.
6. What should I do if I have questions about the claims process?
If you have additional questions regarding the claims process, contacting Customer Service is recommended. You can reach out by calling 1-800-638-6589 for assistance. Customer Service representatives can provide guidance and clarify any uncertainties related to completing the claim form or the submission process.
Common mistakes
Filling out the Samba Insurance Claim form can be straightforward, but many people make common mistakes that can delay processing. One frequent error is not providing complete information in the MEMBER INFORMATION section. For instance, leaving out details such as the member's full name, mailing address, or the member ID number can lead to complications. Always double-check that your information matches what appears on your SAMBA ID card. Accuracy here is vital, as it helps the processing team identify your account and expedite your claim.
Another mistake often encountered is failing to correct the patient’s details when they differ from the member's information. If the patient is someone other than the member, such as a child or spouse, be sure to complete the PATIENT INFORMATION section accurately. Omitting or incorrectly stating the patient’s relationship to the member can raise questions and slow down the approval process. Take the time to verify all names and relationships to ensure everything aligns correctly.
Individuals frequently neglect to attach the required documentation. Claims processing needs an itemized bill if the health care professional is not submitting the claim on your behalf. Not only must this bill list specific details like service type, date, and provider information, but it should also be signed by the health care professional. Forgetting to include these documents can lead to delays or even denial of coverage. Always keep a copy of the bills and forms for your records.
Lastly, many people overlook the importance of submitting the claim on time. You must submit your claim by December 31 of the year following the date of service. Missing this deadline can result in expulsion from the claims process altogether. Set reminders for yourself and plan to mail your claims as early as possible. Taking these steps will help ensure that your claim is processed without unnecessary trouble and that any eligible benefits are received promptly.
Documents used along the form
When submitting a claim using the Samba Insurance Claim form, it is essential to include several other documents to facilitate the processing of your request. Below is a list of commonly required forms and documents that complement the claim form.
- Itemized Bills: These are detailed statements from your healthcare provider that outline the services rendered, along with associated costs. Ensure that these bills include all required details, such as diagnosis codes and provider information.
- Explanation of Benefits (EOB): If you have other health insurance coverage, this document is crucial. It provides details about what has been covered by your primary insurer, as well as any amounts that remain your responsibility.
- Medical Records: Depending on the nature of your claim, additional medical records may be requested to substantiate the services provided and their necessity. Keep these records readily available.
- Authorization for Release of Information: This form allows your healthcare provider to share necessary information with your insurer to process your claim. Having this form signed can speed up the process.
- Proof of Payment: If you have already paid the provider, this proof—like a receipt—should be submitted to demonstrate that expenses were incurred prior to filing the claim.
- Transfer of Benefits Form: Complete this form if you want SAMBA to pay the healthcare provider directly. This document is especially important when dealing with in-network care providers.
Gathering these additional documents will enhance the efficiency of your claim submission and ensure that all necessary information is available for review. Prompt action in preparing your documentation can lead to faster processing and resolution of your claim.
Similar forms
The Samba Insurance Claim form is a crucial document in processing insurance claims. Several other documents serve similar purposes in the realm of health insurance and claims submission. Here’s a look at eight of these documents and how they relate to the Samba Insurance Claim form:
- Health Claim Form (CMS-1500): This form is widely used by healthcare providers to bill Medicare and other insurance carriers. Like the Samba form, it requires patient and provider information, as well as details about the diagnosis and services rendered.
- Hospital Bill: A hospital bill itemizes all services provided during a patient’s stay. It serves as supporting documentation for claims, similar to the itemized bills required by the Samba form.
- Explanation of Benefits (EOB): This document details what your insurance has paid and what you owe. Just as the Samba form requires EOBs for claims involving other insurance, EOBs provide insights into how services were processed by your insurance provider.
- Medicare Claim Form (CMS-1490S): Used for filing Medicare claims, this form captures similar patient and provider information. It also asks about other insurance coverage, paralleling the Samba form’s inquiries regarding additional health plans.
- Dental Claim Form: Often used for dental services, this form outlines procedures and costs just like the Samba form. It captures member and patient data, focusing specifically on dental care.
- Vision Claim Form: Like the dental claim form, the vision claim form caters to eye care services. It requires similar information to submit and process reimbursements effectively.
- Workers’ Compensation Claim Form: Utilized for workplace injuries, this form collects information about the injury, much like the accident claims section of the Samba form. It is crucial in determining coverage for work-related incidents.
- Prior Authorization Request Form: Some treatments or services require pre-approval from your insurance provider. This form outlines necessary patient details and requested services, analogous to the preliminary information requested in the Samba form.
Understanding these similarities can ease the process of filing claims and help ensure that necessary information is submitted accurately and completely.
Dos and Don'ts
Here’s what to do and what to avoid when filling out the Samba Insurance Claim form:
- Do use a new printed form if filling out by hand.
- Do include your SAMBA member ID number from your ID card.
- Do provide an itemized bill for the claim.
- Do print clearly in black ink to ensure legibility.
- Don’t use a photocopy of the form; it may cause delays.
- Don’t forget to fill out separate claim forms for each family member.
- Don’t send receipts instead of the required itemized bill.
- Don’t staple or paper clip the bills to the claim form when submitting one claim.
Misconceptions
Understanding the Samba Insurance Claim form is crucial for efficient processing of claims. However, several misconceptions persist regarding its use. Here are eight common misunderstandings, clarified for better comprehension.
- Only health care professionals can submit a claim: Many believe that only providers can file claims on behalf of patients. In reality, patients can submit their claims using the form if their providers do not.
- The form must be submitted immediately after a service: Some think they need to file the claim right after receiving care. Claims can be submitted any time before December 31st of the year following the year the service was rendered.
- Photocopies of the claim form are acceptable: A common assumption is that it's fine to submit photocopies. However, it's specified that only original forms should be used to ensure proper scanning and processing.
- Itemized bills are optional: Individuals may believe generic receipts are sufficient. In fact, itemized bills are mandatory for processing a claim correctly.
- There is no need to include dependent's information: Some think they can submit claims without detailing their dependents. The form requires complete information about the relationship of the patient to the member.
- The payment will always go to the member: There is a misconception that payment goes directly to the member regardless of provider contracts. Payment is typically directed to health care professionals with Cigna contracts.
- Medicare coverage is irrelevant: Some individuals think their Medicare coverage doesn't matter when filing claims. It is vital to indicate whether either the member or patient is covered under Medicare, as it impacts claim processing.
- Claim forms do not require a signature: Many underestimate the importance of signing the form. A signature is required to authorize the release of information and confirm the accuracy of the provided details.
Understanding these misconceptions can help avoid delays in claim processing and ensure that members receive the benefits they are entitled to. Be proactive; carefully completing the claim form is essential for a smooth claims experience.
Key takeaways
Here are some key takeaways for filling out and using the Samba Insurance Claim form:
- Identify the relevant form: Use the specific Medical Claim Form for medical claims only. For other types such as Pharmacy or Dental, refer to the resources available online.
- Responsibility for filing: If your healthcare professional is not filing the claim on your behalf, you will need to complete this form. Out-of-network professionals can still submit the claim for you.
- Filling out the form: When filling out the form electronically, ensure you click to the right of each field to enter information. If completed by hand, utilize a blank printed form instead of a photocopy.
- Submission deadlines: Submit your claim by December 31st of the year following the service date to ensure processing.
- Separate forms required: Use a different claim form for each healthcare professional and each family member. New forms can be obtained online or via Customer Service.
- Importance of itemized bills: An itemized bill is necessary for processing. Neither receipts nor balance statements will be accepted in its place.
- Direct payment information: For professionals with a Cigna contract, payment will go directly to them unless specified otherwise on the form.
Browse Other Templates
Doctors Note Return to Work - The form aims to support the employee's successful return while considering health needs.
Top Grade Interview - Facilitated change management initiatives that positively impacted employee morale.